Nursing Facility Transition Model for Individuals with Mental Illness:
advertisement

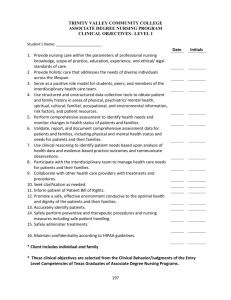
Transitioning Clients with Mental Illness from Colorado Nursing Facilities: A Best Practices Model Report June 2006 Prepared by Systems Change for Real Choices Grant Staff Real Choice Systems Change Grant #915328 from the Centers for Medicare and Medicaid Services and the Colorado Department of Health Care Policy and Financing Table of Contents Introduction ................................................................................................................................... 3 Client Criteria ................................................................................................................................. 4 Transition Time Frame ................................................................................................................... 4 Transition Steps .............................................................................................................................. 4 Transition Step 1 ........................................................................................................................... 5 IDENTIFICATION/ASSESSMENT ......................................................................................................... 5 JUSTIFICATION ................................................................................................................................. 5 PLAN FOR PROGRESS........................................................................................................................ 5 REFERRAL ........................................................................................................................................ 6 Transition Action Levels .............................................................................................................. 6 Level 1 - Referral to Transition Planning........................................................................................ 6 Level 2 - Not Ready for Transition at This Time ............................................................................ 6 Transition Step 2 ........................................................................................................................... 9 Transition Step 3 ......................................................................................................................... 10 Phases of the Transition Plan ........................................................................................................ 10 Phase 1: Preparation for discharge from the nursing facility ...................................................... 10 Phase 2: Discharge from Nursing Facility ................................................................................... 10 Phase 3: Community Stability....................................................................................................... 10 Transition Step 4 ......................................................................................................................... 12 Transition Step 5 ......................................................................................................................... 13 Appendix A: Summary and Checklist ......................................................................................... 14 Appendix B: Glossary of Terms .................................................................................................. 16 Appendix C: Transition Flow Chart ............................................................................................ 19 Appendix D: Nursing Facility Client Transition Referral and Response Form .......................... 21 Appendix E: Transition Readiness Assessment Form ................................................................. 23 Appendix F: Community Resource Assessment Form................................................................ 26 Appendix G: Client Community Living Self-Assessment .......................................................... 29 2 Introduction From February through October, 2005, a group of consumers, providers, practitioners, advocates, and experts came together from several fields, including mental health, long term care, and independent living, to form an ad hoc Mental Health Advisory Committee. This committee focused specifically on issues involved in transitioning of nursing facility Clients with mental illness out of nursing facilities and into community living arrangements. These meetings were convened by the Department of Health Care Policy and Financing (the Department), and made possible by funding and staff provided by the Systems Change for Real Choices (SCRC) Grant from the Centers for Medicare and Medicaid Services (CMS). Working collaboratively, the advisory committee participants identified the major challenges preventing people with mental illness from discharging out of nursing facilities and into less restrictive communities, such as homes, apartments, or alternative care facilities (ACFs). The advisory committee also brainstormed about the approaches, strategies, and techniques proven to support and facilitate successful transitions. The result of their work is this "Best Practices Model" report. By publishing this report, the Department aims to make available a framework for successful transition of nursing facility Clients with mental illness. The Best Practices described herein are offered as a guide for service providers, advocates, and mental health Clients themselves. The Department is not mandating any of the procedures outlined in this report. The adoption or use of these guidelines by any agency or facility is entirely voluntary. The Mental Health Advisory Committee designed this model to do the following: Assure that Clients of nursing facilities who have mental illness are assessed on a monthly basis to determine transition potential. Assure that individuals who wish to make the transition have appropriate information and support to request transition services. Establish a formalized transition process including referral, assessment, transition levels, interventions and accountability measures. Emphasize informed consumer choice and consumer responsibility. Develop efficient and effective system collaboration between consumers, family members, nursing facilities, mental health centers, independent living centers, and Single Entry Point agencies. Strengthen existing supports and customizes specific interventions to help individuals successfully transition from institutions to independent community living. Provide a continuum of interventions, from point of transition referral to successful maintenance in a community setting. 3 Client Criteria Under this model, a potential Client is an individual who meets the following criteria: Residence in a nursing facility. Mental illness diagnosis alone or dual diagnosis (such as mental illness in combination with developmental disability, physical disability, or chemical addiction). Motivation to transition to a community independent living arrangement (i.e. a small group home, own apartment, with family/friend), or to some other less restrictive setting such as an assisted living facility. Some family and/or other support system involvement. Transition Time Frame The transition period begins when the Client is referred for a transition assessment. The transition period ends when the Client is living in the community, receiving the recommended level of services needed to maintain community living, and is actively engaged in formal and/or informal community based support systems for at least three months. Transition Steps 1. The Nursing Facility Treatment Team identifies and assesses the potential Client, upon receiving a request for such assessment from the Client or another party. 2. A Transition Support Team forms, to include the Client, family, friends, advocates, nursing facility staff, mental health providers, and other community based providers. 3. The Transition Support Team develops a Transition Plan with the Client exercising maximum choice and decision-making. 4. The Transition Support Team works to locate and access funding needed for transition expenses. 5. The Transition Support Team provides post-transition follow-up support. In working with nursing facility Clients who have mental illness, providers are encouraged to plan for and complete all transition steps as described in this document. It may be helpful for transition planners, mental health providers, and nursing facility staff members to utilize the onepage summary/checklist in Appendix A. For additional clarity, a glossary is provided in Appendix B, and a Transition Flow Chart is provided in Appendix C. 4 Transition Step 1 The Nursing Facility Treatment Team identifies and assesses potential Clients, upon receiving a request for such assessment from the Client or another party. IDENTIFICATION/ASSESSMENT Each Client who has mental health issues should be assessed to identify transition potential by the Nursing Facility Treatment Team, which includes the nursing facility staff and mental health providers. This assessment should occur during regularly scheduled case review meetings. Treatment plans for Clients with mental illness should consistently include transition goals, and case review notes should include documentation addressing progress towards transition goals. This documentation should identify the Client's degree of readiness for transition, with justification for that assessment, and the plans for helping the Client to move toward transition readiness. Annually, the Client should be assessed to determine which of the following levels of readiness for transition action is most appropriate. Transition Action Level 1: The Client is ready for Referral to the Transition Planning and Transition Preparedness Program, based on the following criteria: expresses a desire to live in a less restrictive setting able to make effective use of needed support services to manage daily needs cooperative with treatment aware of mental illness and its impact on life functioning Transition Action Level 2: The Client is not ready for transition at this time, based on the following criteria: not able to make effective use of needed support services to manage daily needs not cooperative with treatment unaware of mental illness and its impact on life functioning JUSTIFICATION The Nursing Facility Treatment Team should provide thorough documentation of the objective criteria used to justify its assessment of the Client's Transition Action Level. PLAN FOR PROGRESS The Nursing Facility Treatment Team's assessment documentation shall include specific plans and objectives for the coming month to move the Client closer to the next action level or referral for a Transition Readiness Assessment. 5 REFERRAL In addition to the annual assessment during regularly scheduled case reviews, a nursing facility Client can be referred for a transition readiness assessment at any time by any of the following: the Client Nursing Facility Treatment Team family member friend advocate nursing facility staff medical staff mental health provider any interested party Referral for transition assessment occurs when a Nursing Facility Client Transition Referral and Response Form (see Appendix D) is completed and submitted to any of the following: nursing facility staff physician/nurse mental health provider The Nursing Facility Client Transition Referral and Response Form is then submitted to the mental health clinician within 5 business days of receipt. Within 10 business days of receipt of the referral form, the Nursing Facility Treatment Team meets and conducts a case review to discuss transition readiness. During this case review, using the Transition Readiness Assessment Form (see Appendix E) the Nursing Facility Treatment Team determines the Client’s appropriate Transition Action Level based on objective criteria and the Client's input. Based on the assessed Transition Action Level, the Nursing Facility Treatment Team identifies one of the transition referral response actions listed below. The mental health provider assigned to the Client's case then completes the Transition Referral Response Action within 10 business days of receipt of the referral. Transition Action Levels Level 1 - Referral to Transition Planning →Response Action: A transition assessment meeting is scheduled Level 2 - Not Ready for Transition at This Time →Response Action: A treatment goal, objective, and plan is developed and implemented to move the Client closer to Level 1 The mental health provider sends a copy of the Nursing Facility Client Transition Referral and Response Form to the Client. This form informs the client of the Nursing Facility Treatment Team’s decision concerning transition readiness. A copy of the Nursing Facility Client Transition Referral and Response Form should be included in the individual’s mental health center Client chart and in the individual's nursing facility Client chart. The Client, including his/her designated representative should be given the opportunity to ask for reconsideration 6 and/or reversal of the transition readiness decision either verbally during a Nursing Facility Treatment Team meeting or in writing to the Nursing Facility Treatment Team. The mental health provider should inform the Long term care Ombudsman of the request, and should schedule a Nursing Facility Treatment Team meeting and/or submit to the Nursing Facility Treatment Team a copy of the request from the Client and/or referral source. A copy of the Client’s written request for reconsideration and/or reversal is included in the individual's nursing facility Client chart and in the individual's mental health center Client chart. If there is no written documentation of the request for reconsideration, then documentation of a verbal discussion of the decision should be included in the nursing facility Client chart and in the mental health center Client charts. The Client should also be provided with information about other possible transition resources which he/she may choose to pursue even without the support of the transition team, as well as information about the possible risks involved in doing so. The outcome of the request for reconsideration should be documented in the individual’s mental health center Client chart and in the individual's nursing facility Client chart. Assessment of Clients Who Meet Level 1 Criteria The Transition Assessment meeting includes nursing facility staff and mental health providers. The Transition Assessment is completed during this meeting. Transition eligibility criteria considered during this assessment includes: the Client’s ability to carry out daily living skills such as cooking, cleaning, and money management, or to effectively manage support services to assist with such skills the Client’s ability to manage medication and mental illness symptoms family support financial resources available to support community living the Client's ability to be safe in the community a determination that the Client is cognitively intact availability and accessibility of the services necessary to support the Client's community living the Client's ability to maintain health and well-being outside of a skilled care facility the availability of an adequate support system, or the potential for developing such a support system during the transition planning process the treating physician’s verification that the Client's medical needs can be provided for in the community The Transition Assessment includes the following documents: Independent Living Assessment. It is recommended that a validated assessment tool be utilized to measure the Client’s living skills level and/or to identify the types and amount of in-home support services needed to support independent living. One such tool is the Independent Living Skills Survey (ILSS), a comprehensive, objective, performance- 7 focused, easy instrument for measuring the basic functional living skills of individuals with severe and persistent mental illness. Resource Assessment. The planning process considers the basic resources needed for any transition, and also the specific resources needed by the individual Client. The process should include completion of the Community Resource Assessment Form (Appendix F). In particular, any services the Client has been receiving in the nursing facility should be reviewed for the feasibility of finding equivalent services available and accessible in the community. Transitional Readiness Assessment. The planning process should carefully consider and address each of the eligibility criteria identified above, with emphasis on both objective criteria and input from the Client. Self-Assessment for Community Living. Using the form provided in Appendix G, the Nursing Facility Treatment Team works closely with the Client to develop a comprehensive self-assessment. Based on the Transition Assessment, the Nursing Facility Treatment Team assigns the Client to one of the following transition levels: Level 1: Transition Planning and Preparedness Program Level 2: Not ready at this time for transition The mental health provider then takes the following actions, depending on the assigned transition level: Client and assigned to Level 1: →Referral to Transition Planning and Preparedness Program →Request to Client’s Nursing Facility Treatment Team for assignment of a Transition Coordinator to initiate the transition process. Client assigned to Level 2: →Response Action: A treatment goal, with supporting objectives and plans, are developed and implemented to move the Client closer to Level 1. The goal, objectives, and plans are added to the nursing facility care plan and the mental health center treatment plan. A summary of the transition assessment process and justification for transition level decision is documented on the Nursing Facility Client Transition Referral and Response Form. Copies of this form are sent to the Client. The Client may also choose to allow release of the form to the person who made the referral for transition assessment, within the guidelines of the Health Insurance Portability and Accountability Act (HIPAA). Copies are also placed in the nursing facility Client chart and in the mental health center Client chart. Copies of all assessment tools used to determine transition level should be made available to the Client upon request. 8 Transition Step 2 A Transition Support Team is established. Members include the Client, a Transition Coordinator, family, friends, advocates, nursing facility staff, mental health provider, primary care physician, SEP case manager, and community based providers. The Transition Support Team appoints a Transition Coordinator, who will be responsible for carrying out the following tasks: coordinating Transition Support Team activities defining the responsibilities of each Transition Support Team member advocating for the Client ensuring the progress of the transition process and accountability for the transition plan, encouraging all Transition Support Team members to meet goals within identified time frames evaluating and documenting the transition process facilitating communication and collaboration among Transition Support Team members and with other involved parties identifying transition barriers and presenting them to the Transition Support Team to resolve monitoring, evaluating, and following up on outcomes resolving situations if systems fail accessing and monitoring transition expense funding The Transition Coordinator should organize the Transition Support Team within two weeks of receiving the referral. Other members can be included in the Transition Support Team, at the discretion of the Transition Coordinator. 9 Transition Step 3 At its first meeting, the Transition Support Team develops the Transition Plan. The Transition Coordinator is responsible for ensuring that each aspect of the Transition Plan is represented by an appropriate service provider on the Transition Support Team. The Transition Plan covers the complete transition period. The transition period begins when the Treatment Team determines that the Client meets criteria for Level 1 – Referral for Transition Planning. The transition period ends three months after discharge, when the Client is living in the community, is receiving the recommended level of services to maintain placement, and is actively engaged in formal and/or informal community based support systems. The Transition Plan should reflect the Client's progress as well as any obstacles which impede that progress. Goals, objectives, and action steps should address all barriers to community living identified during the independent living skills functional assessment. Goals, objectives, and action steps should be addressed within the allotted transition period. Phases of the Transition Plan The Transition Plan includes three phases: Phase 1: Preparation for discharge from the nursing facility During Phase 1, the Transition Support Team addresses life management skills that were identified as deficit areas on the functional assessment, by establishing goals, objectives, action steps, and time frames. Phase 2: Discharge from Nursing Facility The Transition Support Team completes the Community Resource Assessment tracking form to identify community resources needed by the Client. The Transition Support Team develops goals, objectives, action steps, and time frames to establish each community resource needed prior to discharge. The Transition Support Team develops a complete list of contact numbers of all individuals providing support services to the transitioning individual. Phase 3: Community Stability The Transition Coordinator monitors the Client closely for three months during Phase 3. The Transition Support Team meets at least monthly, or more often if needed, to review the Client’s progress. The Transition Support Team identifies goals, objectives, action steps, and time frames to establish and maintain community stability. 10 The Client is an active and equal member of the Transition Support Team and should be assigned reasonable and appropriate transition responsibilities. The Client should be involved in all Transition Support Team meetings. The Transition Plan should address the following areas on an individualized basis: social and family support systems community equivalents of all services that the Client has been receiving while in the nursing facility on-going medical and medication needs on-going mental health needs identification of relapse triggers seasonal issues that may impact stability rehabilitation and social skills transportation durable medical equipment occupational therapy and safety evaluation financial legal life management skills needed for community living The Transition Coordinator should utilize a checklist and/or guideline as a frame of reference document to track assigned responsibilities and time frames. The Transition Coordinator is responsible for documentation of the transition process including case reviews, progress reports, and the Transition Plan. All transition-related documentation will be included in the mental health center Client chart and in the nursing facility Client chart. The full Transition Support Team reviews the Transition Plan on at least a monthly basis. Changes may be made to the treatment plan as the Client moves through each phase of the transition. The Transition Coordinator may schedule additional meetings as needed to monitor these changes. The Transition Coordinator monitors progress towards transition goals on an on-going basis, by obtaining update reports from, and problem-solving with, the Client and other Transition Support Team members. 11 Transition Step 4 Funding for community living expenses is essential to the transition process. The Transition Support Team should make a best effort to access funding as needed through available formal and informal resources. Available financial resources will depend upon the Client's circumstances and eligibility. Funding sources for ongoing maintenance include any one, or a combination, of the following: Social Security Disability Income (SSDI) Supplemental Security Income (SSI) Other retirement income Veteran's benefits The Client's personal or family resources For some Clients who expect to incur initial expenses in relocating from a nursing facility into the community, funds may be available through the Community Transition Services (CTS) benefit under Colorado's Home and Community Based Services for the Elderly, Blind and Disabled (HCBS-EBD) waiver. CTS is not a benefit under the Home and Community Based Services for Persons with Mental Illness (HCBS-MI) waiver. However, a Client with mental illness may be eligible for services under HCBS-EBD, including CTS. The CTS benefit can assist Medicaid Clients in transitioning from nursing facilities to community-based residences. Under this benefit, a Transition Coordination Agency works with the Client to create a plan for a safe transition from a nursing facility to a community-based residence. CTS can also provide funds to help the Client pay for security and utility deposits, moving expenses, one time pest eradication, one time cleaning expenses, essential household furnishings, and a one time purchase of food. 12 Transition Step 5 Transition interventions continue into the community for at least three months after discharge. This period of time in the transition process is considered Phase 2, Discharge from Nursing Facility, and Phase 3, Community Stability. The Transition Support Team continues to meet as needed during these phases to develop and monitor goals, objectives, action steps, and time frames, in order to support the Client in establishing and maintaining community stability. Transition is considered complete when the Client has been living in the community for at least three months, is receiving the recommended level of services needed to maintain community living, and is actively engaged in a formal and/or informal community based support system. The Transition Support Team, with substantial input from the Client, determines when the transition has been successfully completed, based on the following criteria: 1. The Client has maintained community living for three months without using more intensive services such as a hospital step-down or hospital admission. 2. The Client is receiving the recommended level of services, including support services and medication management. 3. The Client is actively engaged in formal and/or informal community based support system. In cases when the Client cannot maintain successful community living, the Transition Support Team will work with the Client to consider other options, which may include returning to the nursing facility, placement in another nursing facility, temporary residence in a group home or halfway house. The Transition Support Team will ensure that the Client's funding source for the original nursing facility placement will again pay for the new or return placement. If that original funding source is no longer in place, for example if the Client has lost Medicaid eligibility, the Transition Support Team will assist the Client in finding alternative funding sources. If members of the Transition Support Team are no longer available when the Client's transition has failed, the Transition Coordinator and/or the local Single Entry Point case manager will take over the role of assisting the Client with funding, resource coordination, placement, and other needs. When the Client has successfully completed transition and all necessary on-going services are in place, the Transition Coordinator will end Transition Support Team activities. 13 Appendix A: Summary and Checklist 14 Nursing Facilities Transition Model for Individuals with Mental Illness Summary and Checklist _______Clients with mental illness are assessed monthly to identify transition potential, followed by submission of a completed Nursing Facility Client Transition Referral and Response Form. _______The Nursing Facility Treatment Team conducts a case review and a transition assessment which includes: o Functional Assessment o Resource Assessment o Transitional Readiness Assessment o Client Self-Assessment for Community Living _______Within two weeks, the mental health provider completes one of the following transition response actions: o Level 1: Ready for transition planning. A transition assessment meeting is scheduled. A Transition Coordinator is assigned to begin the transition process. o Level 2: Not ready for transition at this time. A treatment goal, objective, and plan is developed and implemented to move the Client closer to Level 1. _______For Clients determined to be at Level 1, a Transition Support Team is established. _______The Transition Support Team develops a Transition Plan. _______The Transition Support Team closely monitors the Transition Plan, and modifies it appropriately as the Client moves through each transition phase. _______The Transition Support Team provides post-transition follow-up support to the Client for three months after discharge from the nursing facility. _______The transition is complete when the Client has lived and remained stable in the community for three months. 15 Appendix B: Glossary of Terms 16 Glossary of Terms: Best Practices Transition Model Definitions 1. Transition Plan – A comprehensive plan that enables a Client of a nursing facility to move from the facility into a community living arrangement. 2. Client – A nursing facility Client who meets the criteria established for transition potential. 3. Transition Period – The time period from when the Client is referred for a transition assessment to the point in time when the individual is living in the community, receiving the recommended level of services needed to maintain in the community and actively engaged in formal and/or informal community based support system for at least three months. 4. Transition Steps – Five action steps that identify the goals and objectives for each phase of transition. 5. Nursing Facility Treatment Team – A team of professionals that provide services to a Client of a nursing facility including primary care physician, nurse, social worker, activities director and mental health provider. 6. Transition Support Team – A team of professionals that develops and monitors the transition plan; locates and accesses funding needed for transition expenses and provides post-transition follow up support for the transitioned individual. 7. Transition Action Level – A category of transition readiness that requires a specific response from the treatment team. There are two levels. Level 1 – Referral to Transition Planning Level 2 – Not Ready for Transition at this time. 8. Nursing Facility Transition Referral and Response Form – Form used to refer a nursing facility Client for assessment of transition readiness. 9. Mental Health Provider – Clinician, case manager or therapist employed by the community mental health center or behavioral health organization providing mental health care to the nursing facility Client. 10. Functional Assessment – A validated assessment tool that measures an individual’s living skills level and/or identifies types and amount of in-home support services needed to support independent living. 11. Resource Assessment – A questionnaire that identifies basic resources needed for any transition and specific resources needed for particular individuals in transition. 17 12. Transitional Readiness Assessment - A tool that will assess each of the identified transition eligibility criteria to determine level of skill training or resource acquisition needed to successfully transition the Client into the community. 13. Self-Assessment for Community Living – A questionnaire that will be completed by the Client to help them decide what type of support they believe they will need to live in the community. 14. Transition Coordinator – An individual who facilitates the Transition Support Team. 18 Appendix C: Transition Flow Chart 19 20 Appendix D: Nursing Facility Client Transition Referral and Response Form 21 22 Appendix E: Transition Readiness Assessment Form 23 24 25 Appendix F: Community Resource Assessment Form 26 27 28 Appendix G: Client Community Living Self-Assessment 29 30 31 32