breaks - My ICO News

BHS 116.3: Physiology III
Notetaker: Stephanie Cullen
Skin Pathologies
Date: 4/29/13
Page: 1
Disorders affecting the skin are extremely common and range from innocuous viral warts (benign skin lesions) to malignant melanoma (serious skin lesions)
Many skin lesions are external manifestations of systemic disease
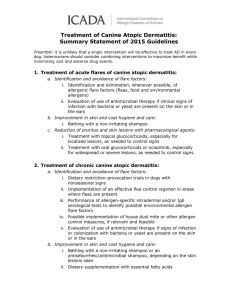
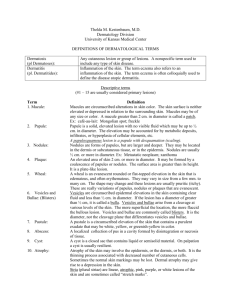
Terms used for Skin Pathologies –NOT TESTED!!!!
Macroscopic terms o Macule: flat area of any size distinguished by coloration o Papule: elevated solid area 5mm or less across o Nodule: elevated solid area > 5 mm across o Bulla: fluid-filled raised area > 5 mm across
Vesicle < 5 mm o Blister: common term used for vesicle or bulla o Pustule: discrete, pus-filled raised area o Scale: dry, plate-like excrescence (outgrowth) o Excoriation: traumatic lesion involving breakage of epidermis
Microscopic terms o Hyperkeratosis: hyperplasia of the stratum corneum (SC) o Parakeratosis: keratinization w/ retention of the nuclei in SC o Acanthosis: epidermal hyperplasia involving stratum spinosum o Dyskeratosis: keratinization below the stratum granulosum
Acute Inflammatory Dermatoses (Skin Disorders)
Urticaria (Hives) o Characterized by localized IgE-dependent mast cell degranulation and resultant dermal microvascular hyperpermeability o Formation of pruritc edematous plaques
Itchy, fluid (raised), skin lesions that are scaly to some extent o Histologically, there is superficial dermal edema and dilated lymphatic and blood filled vascular spaces in the dermis
Fluid buildup is what can cause the hives o Type I Hypersensitivity (b/c it is Ig-E mediated)
Stem from a number of allergens that people typically have a reaction to
Acute Eczematous Dermatitis (Eczema) o Encompasses a number of pathogenetically different conditions
But all have the same type of skin lesions when you look at them o 5 categories of eczematous dermatitis:
Allergic contact dermatitis (most common form)
Atopic dermatitis
Drug-related eczematous dermatitis
Photoeczematous dermatitis
Primary irritant dermatitis o All are characterized by red, papulovesicular , oozing, and crusted lesions at an early stage developing into raised, scaling plaques
BHS 116.3: Physiology III
Notetaker: Stephanie Cullen
Acute Eczematous Dermatitis
Most obvious and common form is acute allergic contact dermatitis in response to topical antigens like poison ivy or even laundry detergent (or other benign things)
Histologically, intercellular edema produces wide spaces w/in the epidermis o Results in small, fluid-filled intraepidermal vesicles (raised lesions)
Type IV hypersensitivity (b/c it is T cell mediated)
Resolves to normal when the trigger is removed (acute)
Date: 4/29/13
Page: 2
Chronic Inflammatory Dermatoses
Focuses on those persistent inflammatory dermatoses that exhibit their most characteristic clinical and histologic features over many months to years
The skin surfaces in some chronic inflammatory dermatoses is roughened as a result of excessive or abnormal scale formation and shedding (desquamation)
Psoriasis o Most frequently effects the skin of the elbows, knees, scalp, and lumbosacral areas b/c they don’t have as thick of skin on them o The most typical lesion is a well demarcated pink to salmon-colored plaque covered by loosely adherent silver-white scales o T-cell mediated disease that involves increased keratinocyte proliferation along w/ inflammation and angiogenesis
Bringing more inflammatory cells to the site o Overproduction of keratinocytes gives rise to the silver-white scales characteristic of psoriasis
Overproduced then flake off = scaling process o Type IV hypersensitivity (b/c it is T cell mediated)
Blistering (Bullous) Diseases
Groups of disorders in which blisters are the primary and most distinctive features (NO scales) o Fluid filled pustules on the surface of the skin
Blisters can occur at multiple levels w/in the skin o Subcorneal: build up under the corneal layer of the epidermis o Suprabasal: accumulates right above the basal layer of the epidermis o Subepidermal: fluid accumulation right b/t the epidermis and dermis (right below the basal layer)
Assessment of these levels is critical to forming an accurate histological diagnosis
Pemphigous – general category of diseases that fall w/in the category of blistering diseases o Rare autoimmune blistering disorder resulting from loss of the integrity of normal intercellular attachments w/in the epidermis and mucosal epithelium
Disrupt normal adhesion of these layers
Fluid builds up beneath the layer where the disruption occurs o Most individuals who develop this disease are middle aged or older men and women
BHS 116.3: Physiology III Date: 4/29/13
Notetaker: Stephanie Cullen o 4 clinical pathological variants
Pemphigous vulgaris
Pemphigous vegetans
Pemphigous foliaceus
Pemphigous erythematosus
Page: 3
Pemphigous Vulgaris o Most common type of pemphigous (80% of cases) o Primary lesions are very superficial vesicles and bullae (suprabasal) that rupture easily and leave shallow erosions covered w/ dried serum and crust
Fluid accumulates above the basal layer in the epidermis
Expose the basal layer when the blisters rupture
High susceptibility for infection o Affected people produce autoantibodies for Desmoglein-1 & 3
Components of the desmosomes that anchor keratinocytes together
Prominent adherens proteins o Adhere the various cells together, especially b/t the various layers
High density of Desmoglein-3 in the basal layer
Highest density of Desmoglein-1 at the upper layers of the epidermis
Equal amount in the suprabasal region o Attach the stratum spinosum to the stratum basale o Where the autoimmune reaction occurs o Where separation of the layers happens and fluid builds up
When there are antibodies against the desmogleins, it triggers an autoimmune reactions and breaks up their connections and fluid can build up
Type II hypersensitivity reaction (b/c it is antigens against a specific tissue) o Can be fatal if left untreated
Bullous Pemphigoid o Generally effects the elderly
People who are bed-ridden or sedentary o Lesions are tense bullae filled w/ clear fluid on normal erythamatous skin
Tighter- thicker skin on the surface o Bullae do not rupture as easily as those seen in pemphigous and can heal w/o scarring o Caused by an autoantibody directed against proteins at the dermal-epidermal junction, specifically hemidesmosomes in the basal cell basement membrane
Attachment of basal cells at the dermal level is disrupted o The antigens have been named bullous pemphigoid antigens 1 & 2
Abs bind to the Ags and cause the separation of the basal layer from the dermis
Where fluid buildup occurs (underneath the basal layer)
Tighter blister b/c it involves all layers of the epidermis forming the skin of the blister o Tissue injury is most likely due to the recruitment of neutrophils and eosinophils to the area w/ subsequent degraulation
Type II hypersensitivity reaction (b/c it is antigens against a specific tissue)
BHS 116.3: Physiology III
Notetaker: Stephanie Cullen
Disorders of Pigmentation
These disorders can render individuals more susceptible to UV rays of the sun
Vitiligo : common disorder characterized by partial or complete loss of pigmentproducing melanocytes w/in the epidermis
Lesions are most visible in darkly pigmented individuals
Date: 4/29/13
Page: 4
Benign and Premalignant Epithelial Lesions
Common and usually biologically inconsequential
Most likely derived from primitive stem cells residing in the epidermis and hair follicles
The overwhelming majority of these lesions do NOT undergo malignant transformation o Some can but most don’t
Verrucae (warts) o Common lesions of children and adolescents
Can be encountered at any age o Caused by the human papilloma virus (HPV) o Verruca vulgaris is the most common type of wart and consist of gray-white to tan, flat to convex (a little raised), but not big- 0.1-1.0 cm papules w/ a rough, pebble-like surface o Frequently appear on the hands
Actinic keratosis o Dysplasia in the skin (due to excess sun exposure) associated w/ focal build-up of excess keratin
Not a vast region of excess keratin sloughing off like in psoriasis o Lesions are usually < 1 cm in diameter, are brown-tan, red, or skin color, and have a rough, sand paper consistency o Some lesions develop a cutaneous horn
From keratin building up on the skin o Many of these lesions become malignant so early detection and removal are important
Considered pre-malignant
Most are still benign
Malignant Epidermal Tumors
Basal cell carcinoma o #1 tumor associated w/ sun exposure o Common, slow growing tumors that rarely metastasize
Might locally invade the tissue nearby but don’t spread through blood or lymph to other tissues o Tend to occur in areas most exposed to sunlight and in lightly pigmented people
Face, hands, arms o Incidence rises in immunosuppressed people o Tumors present as pearly papules, often containing prominent, dilated subepidermal blood vessels (telangiectasia)
Looks like a shiny, raised, highly vascularized region o Advanced lesions may ulcerate and extensive local invasion into the facial sinuses can occur o Histologically, the tumor cells resemble those in the normal basal cell layer of the epidermis b/c they arise from there o Tumors exhibit multifocal growths or nodular lesions which grow downward into the dermis as chords or islands of cells
BHS 116.3: Physiology III
Notetaker: Stephanie Cullen
Squamous cell carcinoma o 2 nd most common tumor arising on sun-exposed skin o Higher incidence in men than in women o Individuals who are immunosuppressed are at increased risk o Non-invasive tumors appear as sharply defined, red, scaling plaques o Invasive lesions (malignant) are nodular (bumpy regions), show variable degrees of hyperkeratosis , and may ulcerate
May look a little like those actinic keratosis (not quite to the extent of the cutaneous horn but get the keratin buildup on the surface)
Invasive cells exhibit variable differentiation – see all kinds of different cell types
Unlike basal cell carcinomas where all of the cells look like basal cells o < 5% of invasive tumors have metastasized by the time they are discovered o Both types can be found on the eyes (eyes are commonly exposed to sun)
Non-invasive: red, scaly regions
Invasive nodules are larger w/ varying degrees of raised regions and more commonly ulcerate (bottom 2 pictures)
Date: 4/29/13
Page: 5
Tumors and Tumor-like Lesions of Melanocytes
Melanocytic nevus (pigmented mole) o Nevus is any congenital lesion of the skin (birthmark, mole) o Melanocytic nevus is any congenital
(pigmented mole you’re born with) or acquired
(develops after birth) neoplasm of melanocytes o These nevi are usually uniform: tan to brown, uniformly pigmented, small (< 6mm across), solid regions of relatively flat to elevated skin w/ well-defined, rounded borders o Junctional type
Lesions are small, relatively flat , symmetric and uniform
Histologically, junctional nevi have rounded nests of nevus cells at the tips of rete ridges along the dermoepidermal junction o Compound type
Lesions are uniform and symmetrical but are more raised and dome shaped
Histologically, compound nevi have features of junctional nevi , but also nests and cords of nevus cells in the dermis
Push on the skin to give the raised appearance
Dysplastic nevi – combination of the 2 o Inherited forms are considered precursors of malignant melanoma while sporadic forms rarely turn malignant o They are larger than most acquired nevi (> 5mm) and may occur as hundreds of lesions across the body surface
Often get a number clustered together o Flat to slightly raised w/ a “pebbly” surface o May appear target-like w/ a darker raised center and irregular (lighter) flat periphery
BHS 116.3: Physiology III
Notetaker: Stephanie Cullen o Histologically, they have both a compound and junctional nevus component, in addition to linear or lamellar fibrosis
Nests from junctionaly type
Cords from compound type
Fibrosis is unique to the dysplastic nevi
Bands of fibrotic tissue are developing in lamellae
Date: 4/29/13
Page: 6
Malignant Melanoma
Malignant melanoma is a relatively common neoplasm that up until recently was almost uniformly deadly o By the time they were caught they were in the advanced stages and spreading
B/c of increased public awareness of the earliest signs of these tumors, most are cured surgically
Most lesions arise on the skin , but there are other sites of origin including the eye
Predisposing Factors: o Sunlight (major) o Preexisting dysplastic nevus
Especially if it is inherited o Hereditary factors o Exposure to certain carcinogens
Majority of lesions are > 10mm in diameter
Most important clinical signs are the change in color, size, and shape of a pigmented lesion o Unlike benign nevi, melanomas exhibit striking variations in pigmentation (appear in black, brown, red, dark blue, and gray)
Multi-colored o Borders are irregular and often “notched”
Regions of flat and raised
Initially the lesion will undergo radial growth which is horizontal growth w/in the epidermal and superficial dermal layers for a prolonged period of time o During this time, melanoma cells do NOT have the ability to metastasize
(will not spread) and there is no evidence of angiogenesis o Want to catch it during this phase
W/ time, the pattern of growth becomes vertical growth and the melanoma now grows downward into the deep dermal layers o Correlates w/ the metastatic potential of the melanoma cells and the probability of metastasis can be predicted by measuring the depth of invasion of the vertical growth below the granular cell layer of the epidermis (Breslow’s Depth)
Deeper below = greater metastasis o Metastases primarily involve the regional lymph nodes, liver, lungs, and brain
Clinical warning signs: o Enlargement of a preexisting mole
Moles you’re born w/ shouldn’t grow much over time o Itching or pain in a preexisting mole o Development of a new pigmented lesion during adult life
Typically you’re born w/ most the pigmented lesions o Irregularity of the borders of a pigmented lesion o Variation of color w/in a pigmented lesion
BHS 116.3: Physiology III
Notetaker: Stephanie Cullen
Melanoma of the Eye
Date: 4/29/13
Page: 7
Conjunctival melanoma o Only about 2% of all eye melanomas
Melanoma of the eyes is about 1/20 th as common as melanoma of the skin
Most intraocular melanomas arise in the melanocytes of the uvea (iris, CB, and choroid) but they can also originate in the pigmented epithelium of the retina
Composed of 2 cell types (spindle and epithelioid) o Spindle cell dominant lesions are of low aggressiveness
Do NOT tend to metastasize (75% 15 year survivability) o Epithelioid dominant lesions DO metastasize late in their development (35% 15 year survivability)
Uveal melanoma w/ a relatively flat pigmented lesion of the choroid (A) that a few years later has grown and ruptured Bruch’s membrane (B)