TIA Pathway Analysis
advertisement
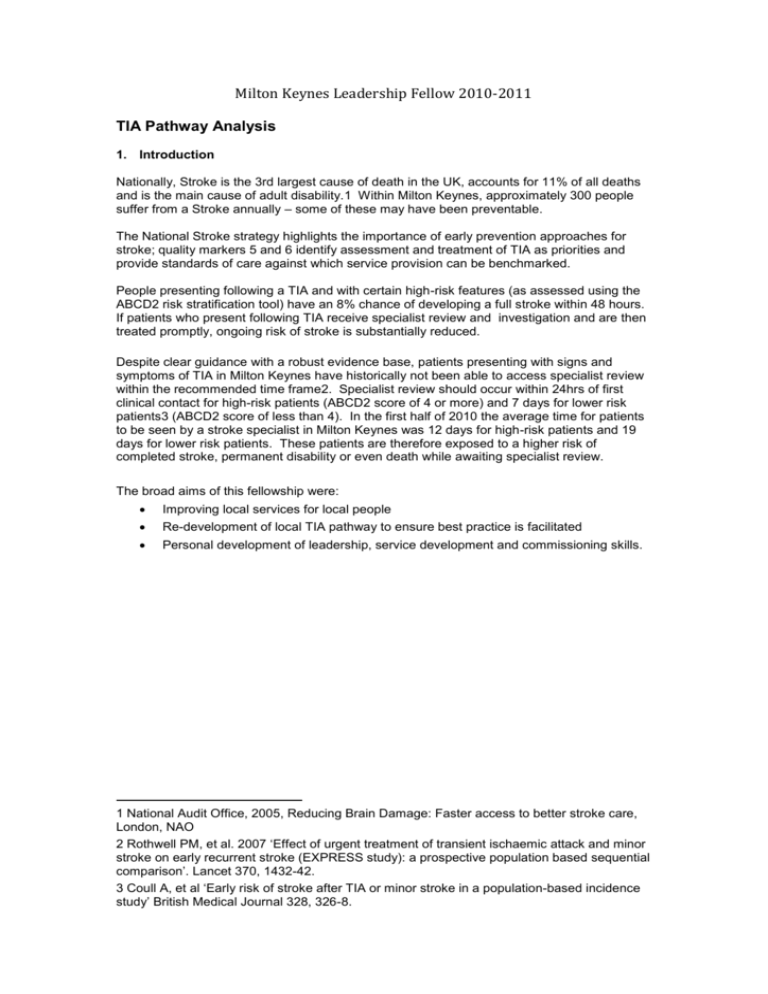
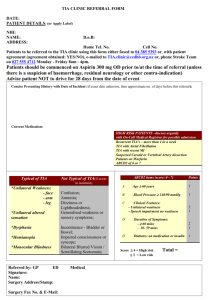
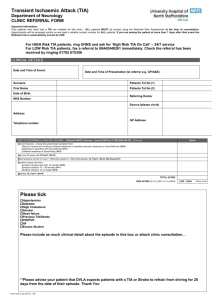
Milton Keynes Leadership Fellow 2010-2011 TIA Pathway Analysis 1. Introduction Nationally, Stroke is the 3rd largest cause of death in the UK, accounts for 11% of all deaths and is the main cause of adult disability.1 Within Milton Keynes, approximately 300 people suffer from a Stroke annually – some of these may have been preventable. The National Stroke strategy highlights the importance of early prevention approaches for stroke; quality markers 5 and 6 identify assessment and treatment of TIA as priorities and provide standards of care against which service provision can be benchmarked. People presenting following a TIA and with certain high-risk features (as assessed using the ABCD2 risk stratification tool) have an 8% chance of developing a full stroke within 48 hours. If patients who present following TIA receive specialist review and investigation and are then treated promptly, ongoing risk of stroke is substantially reduced. Despite clear guidance with a robust evidence base, patients presenting with signs and symptoms of TIA in Milton Keynes have historically not been able to access specialist review within the recommended time frame2. Specialist review should occur within 24hrs of first clinical contact for high-risk patients (ABCD2 score of 4 or more) and 7 days for lower risk patients3 (ABCD2 score of less than 4). In the first half of 2010 the average time for patients to be seen by a stroke specialist in Milton Keynes was 12 days for high-risk patients and 19 days for lower risk patients. These patients are therefore exposed to a higher risk of completed stroke, permanent disability or even death while awaiting specialist review. The broad aims of this fellowship were: Improving local services for local people Re-development of local TIA pathway to ensure best practice is facilitated Personal development of leadership, service development and commissioning skills. 1 National Audit Office, 2005, Reducing Brain Damage: Faster access to better stroke care, London, NAO 2 Rothwell PM, et al. 2007 ‘Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population based sequential comparison’. Lancet 370, 1432-42. 3 Coull A, et al ‘Early risk of stroke after TIA or minor stroke in a population-based incidence study’ British Medical Journal 328, 326-8. 2. SWOT ANALYSIS Early in the project it became clear that despite a lot of good work from many individuals, it would be difficult to deliver the gold standard treatment for patients within the current service structure at Milton Keynes Hospital. There were a number of obstacles that had habitually prevented this from happening. A SWOT analysis of the existing pathway was performed at the beginning of the project. The results are summarized below and illustrate some of the opportunities that were exploited as well as threats to success. Strengths Theme Local services for local people High Quality of care delivered by skilled and experienced stroke team Evidence Following diagnosis of suspected TIA, patients are advised they should not drive. Milton Keynes Foundation Hospital provides a local service for local people which is easily accessible by one bus from most boroughs in Milton Keynes Using data from September 2010 of the 4 high-risk patients seen in TIA clinic, 3 out of 4 (75%) received all of the recommended investigations and treatments on the same day. Although patients were not able to access clinics in a timely fashion, when they were seen, the care they received was of a high standard. Most patients received all of their investigations on the day of their clinic attendance. Single site operation The clinic is always held in the same place, meaning there is no potential for confusion about location for referrers of patients Referral proforma The existing referral proforma is short and has built-in risk stratification scoring which enables patients to be triaged appropriately to high and low risk groups. Only basic information is required on the proforma – this ensures ease of use and encourages timely delivery. Milton Keynes Foundation Trust has the necessary ‘ingredients’ for success. It reported a commitment to engagement in service re-design and development and the provision of high quality care for all. A skilled and experienced Stroke team means that once patients access the service, quality of care is excellent and delivered in a timely fashion. Currently it is free from the complexities of split-site working. Weaknesses Theme Current level of service provision/ lack of clinic availability Evidence Current operational restraints mean that Milton Keynes is currently unable to provide the service seven days a week. Lack of clinic availability means that (even based on a five day week) service patients referred within normal working hours are not meeting the vital sign targets. By way of example, it is not possible to consistently review high-risk patients within 24 hours using this clinic format – if a high-risk patient presents at 5pm on a Friday evening, the earliest they could be seen would be 9am Monday morning - a minimum wait of 64 hours. Data from September 2010 supports this, showing a total of 4 high-risk TIA referrals, none of which were seen within the recommended 24 hour timeframe. Referral pathway/form Clinic Appointments Operational Leadership The number of stages in the current referral pathway means an increased number of opportunities for delays to occur. In addition there is a lack of clinical information on the referral form – this makes it almost impossible to identify inappropriate referrals or mimics prior to actual patient contact. The TIA service operates a 5 day a week clinic model. However, it is important to note that with average waiting times of 12 and 19 days for high and low risk patients respectively, even within the 5 day structure, patients were not being reviewed in the recommended time frame Mon-Fri. Clinic appointments were not always embargoed for new TIA patients and on occasions patients presenting with TIA were not able to be seen in clinic because slots were filled with follow ups. Despite clear guidelines in the form of the national Stroke Strategy 2007 and support from the Stroke Improvement Team, in the 18 months preceding this project, there had been no significant reduction in referral to review times. This despite TIA being recognized as both a national and local priority. Additional focus is needed to ensure a hospital specialist sees patients urgently. To address this, the hospital needs to create ‘Emergency Access Clinics’. Increased emphasis must be placed on referrer’s responsibility to take immediate action to confirm an appointment the same or next day, ideally whilst the patient is with them. For example if a GP confirms the TIA clinic appointment while the patient is with them (rather than “discharge” the patient to be contacted by the hospital) the risk of the hospital being unable to contact the patient and offer an appointment is significantly reduced. Similar models of appointment booking are in place and work for services like early pregnancy scanning within the trust. Opportunities Theme Service redevelopment Multi-agency working Evidence There is an opportunity to look at where the road-blocks are occurring, what is causing delay in service delivery and to redesign the service to avoid these. In particular, to focus on the provision of a seven-day service and embargoed clinic slots for the sole use of the review of new TIA referrals. For the duration of the fellowship, there is capacity to provide dedicated project support, operational leadership and multi-agency working. This focused upon: Development and inclusion of a patient information leaflet to be included in the referral process to highlight the importance of patients attending clinics and reducing DNAs. The targeting of practices that are not risk-stratifying patients or using the TIA proforma to refer patients in a timely fashion Working with local consortia to see if can get TIA referral and risk stratification on the performance management agenda Liaison with OOH providers to look at getting an alert/reminder linked to a coding of TIA encounter Ongoing education projects with the completion of the TIA practice education pack and getting TIA on the programme for the next local GP refresher course. Local Vocational Training scheme teaching to be provided to ensure the future wave of local GPs are well equipped to effectively manage and refer patients presenting with TIA. Increased clinic frequency to 7 days a week would help to address the lack of clinic availability. However, work carried out by the National Stroke Network has found that it is only economically viable to provide a single center 7 day service if you are serving a population of more than 600,000. In order to provide a sustainable service Milton Keynes needs to consider partnering with another provider. There is an opportunity to improve the education to the referrers (GP, Ambulance, A&E etc) to reduce the number of TIA mimics being referred in order to release clinic capacity. Further work is required to ensure the information provided to patients in the community to ensure they understand what a TIA is and ensure they make themselves available to attend an urgent appointment. Public health initiatives have a key role around this. Threats Theme Ageing population Inappropriate referrals/mimics Requirements for patients to be reviewed by specialist Competition from alternative providers Incentives Evidence Milton Keynes has a younger-than-UK-average population. Its unique population demographics mean that it is likely to see an increased demand for the services of its aging population. Evidence from clinic data (based upon figures for September 2010) suggest that in any given month there are more referrals received for a TIA mimic than a true TIA. This has the potential to overwhelm the service and jeopardise the quality of care for patients with true TIA. Emphasis must be on referrer education and the encouragement of alternative referral pathways where symptoms suggest TIA is unlikely. Increased levels of sub-specialisation within the traditional classification of secondary care services means that with the low numbers of actual TIAs seen by the service, non-specialist physicians are unlikely to be exposed to enough patients to keep their skills and knowledge up to date. The provision of a 7 day a week TIA service covered only by stoke specialists will stretch existing resources. With the new white paper and increased market forces new local providers may emerge as competition to existing services. Under its current contractual responsibility, the secondary care provider received a flat tariff for review of the patient – thus it is likely to cost money to provide extra clinics /staff and a weekend service but providing the same standard of care will incur no increased costs. There are numerous threats related to continuing to provide the same level of service not least of which is exposing high-risk TIA patients to enduring stroke risk while they await specialist review. If the current provider of the TIA pathway does not meet the requirements of its commissioners, there is a real threat that notice to terminate the contract may be given. This would mean an alternative provider of services would have to be sought. This may mean far greater travelling distances for the local population. Outcomes The outcomes described were achieved through collaborative working with operations managers, project leads, secondary care organisations, clinicians, Public health physicians, GPs, The Stroke Improvement Programme, Local Stroke Implementation Team, Patient representatives, and The Stroke Network. The outcomes of this fellowship will be presented in terms of the patient, the system and my personal development. Figure 1 Patient: Clinic data from February 2011 (figure 1) confirms that the majority of patients are now seen within the recommended timescales. The data for February shows that 100% of high-risk patients were seen within 24 hours. In addition the lower risk patients are now seen well within the seven-day recommended window. This means that the patients in Milton Keynes are no longer exposed to an unnecessarily high risk of completed stroke while waiting for their specialist review. System: As the local secondary care provider, Milton Keynes Hospital is now partnering with Northampton Hospital Trust to provide a seven day service. They have a definitive TIA pathway with fewer steps that facilitates ease of use (Appendix A). As a result of these changes, for the first time patients are now accessing services within the recommended time scales. A new proforma is in place with a dedicated number for direct clinic bookings 7 days a week. (Appendix B) All practices in Milton Keynes will shortly receive a TIA education pack (Appendix C). This will re-iterate the importance of immediate referral, highlight best practice and also contain patient information leaflets. The patient information leaflets provide general information about stroke prevention, lifestyle measures, the importance of attending clinic appointment as well as a guide on what to expect when they attend clinic. Personally: The fellowship programme provided me with the opportunity to further develop my leadership skills though learning sets, the lead or be led course, LeAD learning modules as well as practical experience leading a project. I was able to gain first hand experience of service development, contracts and the commissioning of services. It taught me that not everybody will share your enthusiasm and vision and I quickly learnt to navigate the barriers and road blocks that striving for change inevitably bring. As a result of the Leadership fellow programme, I have been able to influence national strategy through events with the Department of Health and have become involved in an implementation project for educational needs analysis tool. The tool will be used in GP practices in Milton Keynes to identify knowledge and service gaps relating to the care of patients and with dementia and their carers. The wider implications of this include the use of an educational tool to map local service and influence commissioning intentions. Patient presents to GP/Out-of-Hours/ED with TIA No No Has patient had TIA event within the last 7 days? Perform ABCD2 score assessment URGENT ACTIONS: - Complete TIA referral form - In hours (Mon-Thu. 8am till 8pm and Fri. 8am till 12noon) call IMMEDIATELY Appointment Bureau on 01908 243889 to book urgent appointment - Out of hours (Mon-Thu 8pm till 8am and week-end fax referral to TIA referral line 01908 826750 Yes Yes Perform ABCD2 score assessment Score < 4 Score ≥ 4 URGENT ACTIONS: - Complete TIA referral form - In hours (Mon-Thu. 8am till 8pm and Fri. 8am till 12noon) call IMMEDIATELY Appointment Bureau on 01908 243889 to book urgent appointment - Out of hours (Mon-Thu 8pm till 8am and week-end) fax referral to TIA referral line 01908 826750 Yes - Start Aspirin unless C/I Advise - Lifestyle management - Not to drive - Give Fast leaflet Patient seen by Consultant and investigate within 24 hours (1) Appendix A MK TIA Pathway Has the patient suffered crescendo TIA? (two or more TIAs in the last 7 days) No No Perform: - ECG - Bloods (FBC, ESR, Lipids) - Glucose - Start Aspirin unless C/I Advice: - Lifestyle management - Not to drive - Give FAST leaflet Patient seen by consultant and investigated within 7 days (1) APPENDIX C – Page one of the interactive TIA pack for distribution to all GP practices in Milton Keynes TIA Clinical Guidelines and protocols IMPROVING THE TIA PATHWAY FOR HIGH AND LOW RISK PATIENTS IN MILTON KEYNES – THE NEW TIA REFERRAL FORMS Background 150,000 people have a stroke in England each year, around a third of whom die. Stroke is the largest single cause of adult disability and there are around 300,000 people living with moderate to severe disabilities as a result of a stroke. Approximately 20% of patients with a completed stroke have previously had a mini stroke, otherwise known as a transient ischaemic attack (TIA), often only a few days before the stroke. Early initiation of treatment for TIAs can reduce the number of these patients going on to have a stroke by 80%. In order to improve the TIA patient pathway, Milton Keynes Hospital is partnering with Northampton General Hospital. New TIA referral forms have been created. These incorporate the key information you need regarding referral protocols, diagnosis and out of hours service arrangements for patients in Milton Keynes. Stroke Risk following a TIA is greatest in the first 7-14 days QUICK LINKS THE REFERRAL FORM CLINICAL FEATURES PATIENT INFORMATION APPOINTMENT CARD ABCD2 SCORE