SUPPLEMENTAL MATERIAL ONLINE: Lorius et al
advertisement
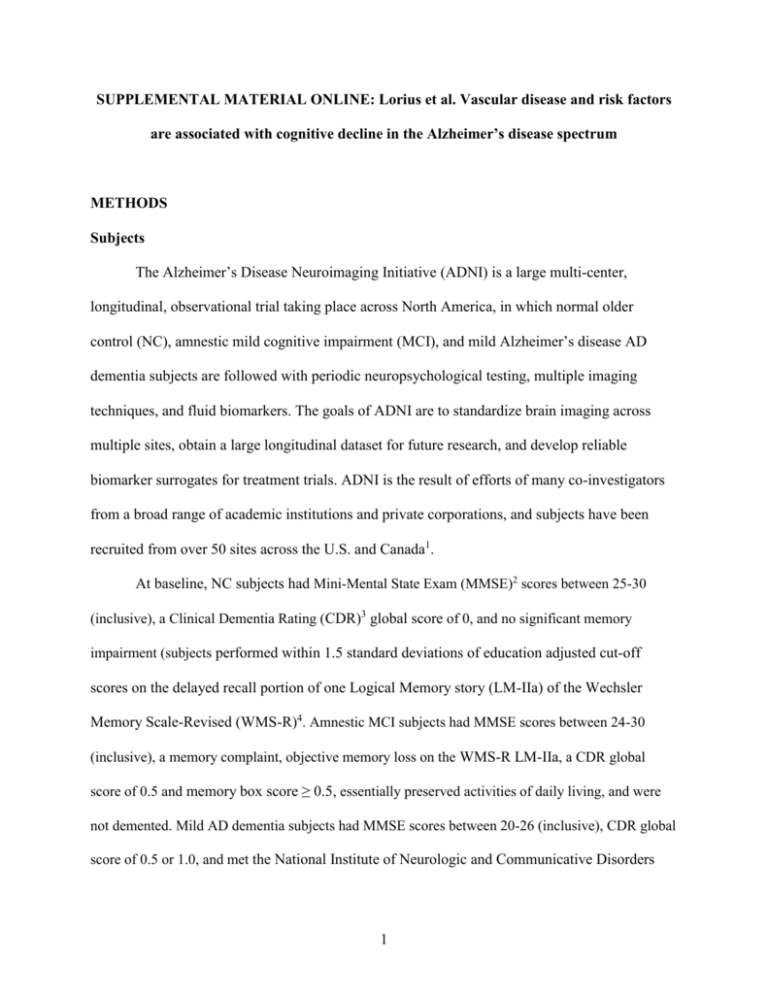
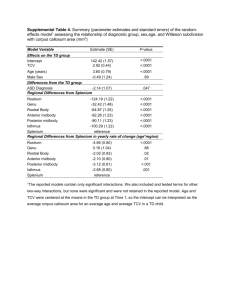
SUPPLEMENTAL MATERIAL ONLINE: Lorius et al. Vascular disease and risk factors are associated with cognitive decline in the Alzheimer’s disease spectrum METHODS Subjects The Alzheimer’s Disease Neuroimaging Initiative (ADNI) is a large multi-center, longitudinal, observational trial taking place across North America, in which normal older control (NC), amnestic mild cognitive impairment (MCI), and mild Alzheimer’s disease AD dementia subjects are followed with periodic neuropsychological testing, multiple imaging techniques, and fluid biomarkers. The goals of ADNI are to standardize brain imaging across multiple sites, obtain a large longitudinal dataset for future research, and develop reliable biomarker surrogates for treatment trials. ADNI is the result of efforts of many co-investigators from a broad range of academic institutions and private corporations, and subjects have been recruited from over 50 sites across the U.S. and Canada1. At baseline, NC subjects had Mini-Mental State Exam (MMSE)2 scores between 25-30 (inclusive), a Clinical Dementia Rating (CDR)3 global score of 0, and no significant memory impairment (subjects performed within 1.5 standard deviations of education adjusted cut-off scores on the delayed recall portion of one Logical Memory story (LM-IIa) of the Wechsler Memory Scale-Revised (WMS-R)4. Amnestic MCI subjects had MMSE scores between 24-30 (inclusive), a memory complaint, objective memory loss on the WMS-R LM-IIa, a CDR global score of 0.5 and memory box score ≥ 0.5, essentially preserved activities of daily living, and were not demented. Mild AD dementia subjects had MMSE scores between 20-26 (inclusive), CDR global score of 0.5 or 1.0, and met the National Institute of Neurologic and Communicative Disorders 1 and Stroke and the AD and Related Disorders Association Work Group (NINCDS/ADRDA) criteria for probable AD5 . Clinical assessments There are some differences between the vascular index score we used in the current study and the Framingham Study Stroke Risk profile6. The Framingham profile includes a measure of systolic blood pressure rather a history of hypertension; it includes left ventricular hypertrophy, which our index does not include; it includes age and use of antihypertensive medications, which we included separately as covariates in our analyses as described below; on the other hand our index includes hyperlipidemia and stroke, which the Framingham profile does not include. Missing values data for key predictors and dependent variables were less than 4% with the exception of white matter hyperintensity (WMH) volume. 811 of the 812 subjects had Digit Symbol scores; 812 had Rey Auditory Verbal Learning Test (RAVLT) Total Learning scores; 804 had Alzheimer Disease Assessment Scale Cognitive Subscale (ADAS-Cog) scores; 812 had Vascular index scores; 810 had systolic blood pressure values; 784 had serum glucose values; 787 had serum total cholesterol values; 810 had Body Mass Index (BMI); 812 had Apolipoprotein E ε4 (APOE4) carrier status; 632 had WMH volume values; and 808 had plasma homocysteine level values. Statistical Analyses Cross-sectional analyses: The inclusion of the interaction of vascular disease and risk factors with diagnosis allowed us to test for any differential relation of any given vascular variable to a given cognitive measure across diagnostic groups. Should the interaction be significant, a test of the same 2 relation could be followed up separately within each group, with these multiple p values “protected” by the required significant preliminary omnibus interaction. On the other hand, if the interaction was not significant, a homogeneous within group relation of the vascular variable to the dependent variable, pooling strength from the data within each of the diagnostic groups, could be performed. Longitudinal analyses: Cox Proportional Hazards Models The overwhelming majority of subjects who progressed from MCI to dementia had AD dementia. The few subjects who progressed to non-AD dementia were included with the subjects who progressed to AD dementia in the current analyses. A p<0.01 cut-off was employed in the backward elimination algorithm for the crosssectional analyses rather than p<0.05 in order to protect against multiple test chance effects owing to the sequence of significance tests performed in the backward elimination. A more liberal cut-off of p<0.05 was used in the longitudinal backward elimination algorithms because there were fewer number of terms in the initial predictor pool for the longitudinal analyses, as well as our desire to be sensitive to important effects that may be missed in these less powerful analyses. RESULTS As noted in Table 1, there was a greater proportion of males among MCI subjects compared to NC and AD dementia subjects. AD dementia subjects had less years of education compared to NC and MCI subjects. The American National Adult Reading Test (AMNART IQ), CDR sum of boxes, MMSE, ADAS-Cog, Digit Symbol, RAVLT Total Learning, and APOE4 3 carrier status were different among all three diagnostic groups in the expected directions. BMI was greater in NC subjects compared to AD dementia subjects. WMH volume was greater in AD dementia subjects compared to MCI subjects. Homocysteine level was lower in NC subjects compared to MCI and AD dementia subjects. Longitudinal Analyses: Cox Proportional Hazards Models MCI to AD dementia progression: Post hoc Tukey tests indicated that having one or two APOE4 alleles significantly (p<0.01) increased the hazard rate over having none, whereas there was no significant difference when comparing having one vs. two APOE4 alleles. ACKNOWLEDGEMENTS Data collection and sharing for this project was funded by the Alzheimer's Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: Abbott; Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Amorfix Life Sciences Ltd.; AstraZeneca; Bayer HealthCare; BioClinica, Inc.; Biogen Idec Inc.; Bristol-Myers Squibb Company; Eisai Inc.; Elan Pharmaceuticals Inc.; Eli Lilly and Company; F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc.; GE Healthcare; Innogenetics, N.V.; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Medpace, Inc.; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Servier; Synarc Inc.; and Takeda Pharmaceutical Company. The Canadian Institutes of Health Research is providing funds 4 to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer's Disease Cooperative Study at the University of California, San Diego. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of California, Los Angeles. This research was also supported by NIH grants P30 AG010129 and K01 AG030514. 5 REFERENCES 1. Weiner MW, Veitch DP, Aisen PS et al. The Alzheimer's Disease Neuroimaging Initiative: a review of papers published since its inception. Alzheimers Dement. 2012;8:S1-68. 2. Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-198. 3. Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993;43:2412-2414. 4. Wechsler D. WMS-R Wechsler Memory Scale Revised Manual. New York: The Psychological Corporation, Harcourt Brace Jovanovich, Inc, 1987. 5. McKhann G, Drachman D, Folstein M et al. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939-944. 6. D'Agostino RB, Wolf PA, Belanger AJ et al. Stroke risk profile: adjustment for antihypertensive medication. The Framingham Study. Stroke. 1994;25:40-43. 6 Figure e-1. Predicted values from fixed effects of best fitting longitudinal model of RAVLT Total Learning score across time in the study by Serum Total Cholesterol at selected baselines by diagnostic group. APOE4 alleles was set to equal presence of 1 allele. NC (Top), MCI (Middle), and AD dementia (Bottom). AD (Alzheimer’s disease), APOE4 (Apolipoprotein E 4), MCI (mild cognitive impairment), NC (normal older control), RAVLT (Rey Auditory Verbal Learning Test), SD (standard deviation). 7 Figure e-1. Lorius et al. Serum Total Cholesterol: -----: mean ___: 1 SD < mean RAVLT Total Learning score ….. : 1 SD > mean 8 Table e-1. Cross-sectional general linear model of association of vascular disease and risk factors and Digit Symbol score, displaying predictors retained in the final model. Model without WMH volume: R2=0.29, p<0.0001 Model with WMH volume: R2=0.32, p<0.0001 β Predictor 95% CI for β p % Variance Accounted for Total Partial Intercept 23.14 14.66, 31.62 <0.0001 Homocysteine -0.33 -0.59, -0.06 0.02 0.4 0.6 WMH volume -0.71 -1.00, -0.42 <0.0001 2.4 3.4 Diagnosis* AD 27.2 0.83 <0.0001 20.8 22.7 MCI 37.01 0.57 NC 45.04 0.75 0.19 0.11, 0.25 <0.0001 2.3 3.1 level AMNART IQ AD (Alzheimer’s disease), AMNART IQ (American National Adult Reading Test intelligence quotient), β (partial unstandardized regression coefficient estimate), CI (confidence interval), MCI (mild cognitive impairment), NC (normal older control), WMH (white matter hyperintensity). “%Variance Total” represents percent of total variance of Digit Symbol uniquely associated with the indicated predictor (unbiased population estimate). “%Variance Partial” represents percent of variance of Digit Symbol with portion associated with other predictors pre-removed, which is uniquely associated with the indicated predictor (unbiased population estimate). 9 * For Diagnosis and sex, covariate adjusted means and standard errors were reported instead of β and 95% CI for β, respectively. 10 Table e-2. Cross-sectional general linear model of association of vascular disease and risk factors and RAVLT Total Learning, displaying predictors retained in the final model. Model: R2=0.45, p<0.0001 β Predictor 95% CI for β p % Variance Accounted for Total Partial Intercept 35.89 26.88, 44.91 <0.0001 Vascular Index score -0.86 0.007 0.4 0.8 Diagnosis* AD 23.81 0.63 <0.0001 33.7 37.8 MCI 31.21 0.44 NC 42.59 0.57 <0.0001 1.4 2.4 Sex* -1.48, -0.24 Female 33.95 0.47 Male 31.12 0.42 Age -0.13 -0.22, -0.04 0.004 0.5 0.9 AMNART IQ 0.14 0.09, 0.19 <0.0001 1.8 3.2 AD (Alzheimer’s disease), AMNART IQ (American National Adult Reading Test intelligence quotient), β (partial unstandardized regression coefficient estimate), CI (confidence interval), MCI (mild cognitive impairment), NC (normal older control), RAVLT (Rey Auditory Verbal Learning Test). “%Variance Total” represents percent of total variance of RAVLT Total Learning uniquely associated with the indicated predictor (unbiased population estimate). “%Variance Partial” represents percent of variance of RAVLT Total Learning with portion associated with other 11 predictors pre-removed, which is uniquely associated with the indicated predictor (unbiased population estimate). * For Diagnosis and sex, covariate adjusted means and standard errors were reported instead of β and 95% CI for β, respectively. 12 Table e-3. Cross-sectional general linear model of association of vascular disease and risk factors and ADAS-Cog score, displaying predictors retained in the final model. Model: R2=0.59, p<0.0001 β Predictor 95% CI for β p % Variance Accounted for Total Partial Intercept 19.96 15.43, 24.49 <0.0001 APOE4 0.89 0.25, 1.54 0.007 0.3 0.8 AD 26.75 0.67 <0.0001 22.0 34.8 MCI 18.96 0.33 NC 10.62 0.43 0.67 0.32, 1.02 0.0002 0.7 1.6 -0.09 -0.13, -0.05 <0.0001 1.1 2.6 Diagnosis* AD dementia symptom duration (years) AMNART IQ AD (Alzheimer’s disease), ADAS-Cog (Alzheimer Disease Assessment Scale Cognitive Subscale), AMNART IQ (American National Adult Reading Test intelligence quotient), APOE4 (Apolipoprotein E 4), β (partial unstandardized regression coefficient estimate), CI (confidence interval), MCI (mild cognitive impairment), NC (normal older control). “%Variance Total” represents percent of total variance of ADAS-Cog uniquely associated with the indicated predictor (unbiased population estimate). “%Variance Partial” represents percent of variance of ADAS-Cog with portion associated with other predictors pre-removed, which is uniquely associated with the indicated predictor (unbiased population estimate). 13 * For Diagnosis, covariate adjusted means and standard errors were reported instead of β and 95% CI for β, respectively. 14 Table e-4. Longitudinal mixed effects model of association of baseline vascular disease and risk factors and Digit Symbol score over time, displaying predictors retained in the final model. Model: R2=0.76 for fixed effects, p<0.0001; R2=0.92 including random terms, p<0.0001 Predictor β 95% CI for β p Intercept 5.02 2.83, 7.20 <0.0001 Time 0.13 -0.52, 0.77 <0.0001 APOE4 -0.003 -0.80, 0.80 0.99 APOE4 x Time -0.84 -1.35, -0.34 0.001 WMH volume 0.10 -0.08, 0.28 0.26 WMH volume x Time -0.10 -0.21, 0.004 0.06 AD -2.24 -4.00, -0.48 0.03 MCI -0.45 -1.72, 0.82 NC 0 AD -3.65 -4.74, -2.56 MCI -1.58 -2.31, -0.86 NC 0 Baseline Diagnosis Baseline Diagnosis x Time 0.91 Baseline Digit Symbol 0.88, 0.95 <0.0001 <0.0001 AD (Alzheimer’s disease), APOE4 (Apolipoprotein E 4), β (partial regression coefficient estimate), CI (confidence interval), MCI (mild cognitive impairment), NC (normal older control), WMH (white matter hyperintensity). x indicates an interaction. 15 Table e-5. Longitudinal mixed effects model of association of baseline vascular disease and risk factors and RAVLT Total Learning score over time, displaying predictors retained in the final model. Model: R2=0.69 for fixed effects, p<0.0001; R2=0.90 including random terms, p<0.0001 Predictor β 95% CI for β p Intercept 7.53 4.52, 10.54 <0.0001 Time 0.61 -0.72, 1.94 0.55 Serum Total Cholesterol 0.01 -0.0003, 0.02 0.06 Serum Total Cholesterol x Time -0.006 -0.01, 0.0002 0.06 APOE4 -0.72 -1.37, -0.08 0.03 RAVLT Total Learning 0.78 0.73, 0.83 <0.0001 AD -5.30 -7.06, -3.54 <0.0001 MCI -3.35 -4.64, -2.06 NC 0 AD -2.21 -3.10, -1.31 MCI -0.82 -1.42, -0.22 NC 0 Baseline Diagnosis Baseline Diagnosis x Time <0.0001 AD (Alzheimer’s disease), APOE4 (Apolipoprotein E 4), β (partial unstandardized regression coefficient estimate), CI (confidence interval), MCI (mild cognitive impairment), NC (normal older control), RAVLT (Rey Auditory Verbal Learning Test). x indicates an interaction. 16 Table e-6. Longitudinal mixed effects model of association of baseline vascular disease and risk factors and ADAS-Cog score over time, displaying predictors retained in the final model. Model: R2=0.75 for fixed effects, p<0.0001; R2=0.95 including random terms, p<0.0001 Predictor β 95% CI for β P Intercept -3.40 -8.12, 1.31 0.16 Time -2.92 -4.23, -1.60 0.02 APOE4 -0.22 -0.81, 0.37 0.47 APOE4 x Time 0.65 0.24, 1.06 0.002 Serum Total Cholesterol 0.006 -0.002, 0.01 0.14 Serum Total Cholesterol x Time 0.007 0.001, 0.01 0.02 Baseline ADAS-Cog 0.79 0.72, 0.85 <0.0001 Baseline ADAS-Cog x Time 0.15 0.10, 0.20 <0.0001 AD 3.62 1.95, 5.30 0.0001 MCI 1.55 0.50, 2.60 NC 0 AD 2.68 1.47, 3.89 MCI 0.84 0.13, 1.55 NC 0 Baseline Diagnosis Baseline Diagnosis x Time <0.0001 Baseline WMH volume 0.12 -0.004, 0.25 0.06 Serum Glucose -0.01 -0.03, -0.00002 0.05 Baseline Age 0.07 0.01, 0.12 0.02 17 AD (Alzheimer’s disease), ADAS-Cog (Alzheimer Disease Assessment Scale Cognitive Subscale), APOE4 (Apolipoprotein E 4), β (partial regression coefficient estimate), CI (confidence interval), MCI (mild cognitive impairment), NC (normal older control), WMH (white matter hyperintensity). x indicates an interaction. 18