POLICIES - CoxHealth
advertisement

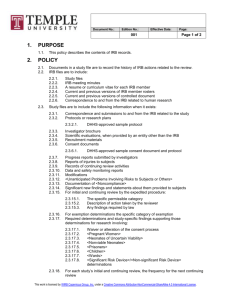
STANDARDS CoxHealth IRB Title: Noncompliance Submitted by: Cortney Freeman Effective Date: 09/09 Standard #: IRB 20 Last Reviewed: 12/11, 09/12 Last Revised: 12/11 The purpose of this standard is to create an understanding of how noncompliance issues will be handled by the IRB. When a study design and/or standards and regulations are not followed in the conducting of a study these are considered deviations and acts of noncompliance. Anyone that knows of such events should report them to the IRB office or Compliance Officer as soon as they become aware of the event. All parties involved are required to cooperate with an investigation if one is deemed necessary and/or with actions that are taken in regards to noncompliance events. I. Definitions: A. Noncompliance: any violation of any regulation or standard that governs human subject research, any deviation from the study protocol approved by the IRB (study deviation), or any violation of any conditions imposed by the IRB on the approval of the study or conduct of the research. B. Minor noncompliance: a noncompliant event that does not impact subject safety, compromise the integrity of the study/data, violate a subject’s rights or welfare or affect the subjects willingness to participate in the research. A minor noncompliant event can also include inadvertent errors or oversight of a regulation or standard that does not increase harm. An example of a minor noncompliance might be a follow-up visit that occurs outside the protocol allowance window. C. Serious noncompliance: a noncompliant event that may impact subject safety, increase risks to the subjects, affect the integrity of the data, violate a subject’s rights or welfare or affect the subject’s willingness to participate in the study. A serious noncompliant event can also include an investigator knowingly disregarding or violating regulations and/or standards applicable to the conduct of research. Examples of serious noncompliance include incorrect treatment provided to a patient or conducting research without prior IRB approval. D. Continuous noncompliance: a series of noncompliant events occurring within the conducting of one study protocol or by a single investigator. II. Information that must be submitted for noncompliance events A. As much as possible of the following information must be provided. If not available at time of notifying the IRB, then it should be submitted as soon as it is known. 1. Investigator Name 2. Study Name and Number, if the event is associated with a particular study 3. Event Date 4. Subject ID, if event patient related 5. Event description including sponsor interpretation if the event is minor or serious 6. Action taken to avoid reoccurrence 7. Date sponsor notified 8. Date IRB notified B. It is the responsibility of the Principal Investigator to make sure the study sponsor is notified of the event C. The IRB will ensure the proper authorities are notified as warranted. III. Steps once an event of noncompliance is reported A. Once the IRB office and/or Compliance Officer becomes aware of a noncompliance issue the IRB Chair will be contacted so together a decision can be made if the event is minor, serious, continuous, or not enough information is available to make a determination. B. If the event is determined to be minor, it will be reported to the IRB at its next convened meeting for determination if further action is required. C. If there is not enough information available to make a determination if the event is serious or continuous an investigation may be conducted by the IRB office, Compliance Officer, and/or the IRB Chair. D. If the event is determined to be serious or continuous by the IRB Chair or Compliance Officer, they may take the following steps: 1. Require that preliminary steps be immediately taken to further investigate and begin to correct the noncompliance a. The IRB office, Compliance Officer, and/or the IRB Chair may conduct an investigation into any reported noncompliance if such an investigation is necessary c. If none of the individuals can adequately conduct the investigation, the occurrence may be handled by the legal department 2. Require temporary suspension of the protocol and/or investigator’s involvement in the research until a Full IRB meeting can be convened, as long as no patients will be harmed by the suspension of activity. The Full IRB will then determine what further action is required. E. If deemed appropriate any reported event can be handled through the Research Misconduct standard. F. Any decision made will be communicated via letter. For unfounded noncompliance or for minor noncompliance a letter will be sent only to the principal investigator. For serious and continuous noncompliance a letter will be sent to the principal investigator, CoxHealth authority over the principal investigator, and the appropriate federal agency if the research is federally funded. IV. Actions that may be taken by the IRB A. No further action B. Suspend or terminate the protocol C. Require additional information or further investigation D. Require modifications to the protocol and/or consent E. Require subjects currently or previously on the protocol be notified of the noncompliance when such information might relate to their willingness to continue to take part in the research F. Require subjects be re-consented G. Modify the continuing review schedule to more frequent review H. Require additional education to research staff I. Require oversight of research by an authority of the investigator J. Monitor the research process including consent K. Require periodic audits L. Request situation be handled by other authorities, such as the legal department M. Any other action deemed necessary by the IRB