Harrison`s Principle.. - UM Personal World Wide Web Server
advertisement
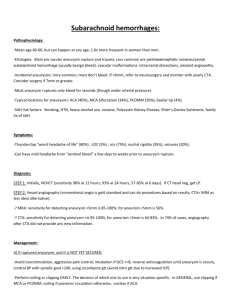
Harrison's Principles of Internal Medicine - 16th Ed. (2005) 349. CEREBROVASCULAR DISEASES - Wade S. Smith, S. Claiborne Johnston, J. Donald Easton INTRODUCTION Cerebrovascular diseases include some of the most common and devastating disorders: ischemic stroke, hemorrhagic stroke, and cerebrovascular anomalies such as intracranial aneurysms and arteriovenous malformations (AVMs). They cause ~200,000 deaths each year in the United States and are a major cause of disability. The incidence of cerebrovascular diseases increases with age, and the number of strokes is projected to increase as the elderly population grows, with a doubling in stroke deaths in the United States by 2030. Most cerebrovascular diseases are manifest by the abrupt onset of a focal neurologic deficit, as if the patient was "struck by the hand of God". A stroke, or cerebrovascular accident, is defined by this abrupt onset of a neurologic deficit that is attributable to a focal vascular cause. Thus, the definition of stroke is clinical, and laboratory studies including brain imaging are used to support the diagnosis. The clinical manifestations of stroke are highly variable because of the complex anatomy of the brain and its vasculature. Cerebral ischemia is caused by a reduction in blood flow that lasts longer than several seconds. Neurologic symptoms are manifest within seconds because neurons lack glycogen, so energy failure is rapid. When blood flow is quickly restored, brain tissue can recover fully and the patient's symptoms are only transient: this is called a transient ischemic attack (TIA). Typically the neurologic signs and symptoms of a TIA last for 5 to 15 min but, by definition, must last 24 h. If the cessation of flow lasts for more than a few minutes, infarction or death of brain tissue results. Stroke has occurred if the neurologic signs and symptoms last for 24 h. A generalized reduction in cerebral blood flow due to systemic hypotension (e.g., cardiac arrhythmia, myocardial infarction, or hemorrhagic shock) usually produces syncope (Chap. 20). If low cerebral blood flow persists for a longer duration, then infarction in the border zones between the major cerebral artery distributions may develop. In more severe instances, global hypoxiaischemia causes widespread brain injury; the constellation of cognitive sequelae that ensue is called hypoxic-ischemic encephalopathy (Chap. 258). Focal ischemia or infarction, on the other hand, is usually caused by thrombosis of the cerebral vessels themselves or by emboli from a proximal arterial source or the heart. Cerebral hemorrhage produces neurologic symptoms by producing a mass effect on neural structures or from the toxic effects of blood itself. IMAGING STUDIES (SEE ALSO CHAP. 347) Computed Tomographic Scans CT53 radiographic images identify or exclude hemorrhage as the cause of stroke, and they identify extraparenchymal hemorrhages, neoplasms, abscesses, and other conditions masquerading as stroke. Scans obtained in the first several hours after an infarction generally show no abnormality, and the infarct may not be seen reliably for 24 to 48 h. CT may fail to show small ischemic strokes in the posterior fossa because of bone artifact; small infarcts on the cortical surface may also be missed. Contrast-enhanced CT54 scans add specificity by showing contrast enhancement of subacute infarcts and allow visualization of venous structures. Coupled with newer generation scanners, CT angiography (CTA) can be performed with administration of intravenous iodinated contrast allowing visualization of the cervical and intracranial arteries. Carotid disease and intracranial vascular occlusions are readily identified with this method (Fig. 349-12). After an intravenous bolus of contrast, deficits in brain perfusion produced by vascular occlusion can also be demonstrated (Fig. 349-12 C). CT imaging is also sensitive for detecting subarachnoid hemorrhage, and CTA can readily identify intracranial aneurysms (see below). Because of its speed and wide availability, noncontrast head CT is the imaging modality of choice in patients with acute stroke (Fig. 349-1), and CTA and CT perfusion imaging may also be useful and convenient adjuncts. Magnetic Resonance Imaging (MRI) MRI2 reliably documents the extent and location of infarction in all areas of the brain, including the posterior fossa and cortical surface. It also identifies intracranial hemorrhage and other abnormalities but is less sensitive than CT55 for detecting acute blood. MRI scanners with magnets of higher field strength produce more reliable and precise images. Diffusion-weighted imaging is more sensitive for early brain infarction than standard MR56 sequences (Fig. 349-13), as is FLAIR (fluid-attenuated inversion recovery) imaging (Chap. 347). Using intravenous administration of gadolinium contrast, MR perfusion studies can be performed. Brain regions showing poor perfusion but no abnormality on diffusion are considered equivalent to the ischemic penumbra (see "Pathophysiology of Ischemic Stroke," above), and patients showing large regions of mismatch may be better candidates for acute revascularization. MR angiography is highly sensitive for stenosis of extracranial internal carotid arteries and of large intracranial vessels. With higher degrees of stenosis, MR angiography tends to overestimate the degree of stenosis when compared to conventional x-ray angiography. MRI with fat saturation is an imaging sequence used to visualize extra- or intracranial arterial dissection. This sensitive technique images clotted blood within the dissected vessel wall. MRI2 is less sensitive for acute blood products than CT57 and is more expensive and time consuming and less readily available. Claustrophobia also limits its application. Most acute stroke protocols use CT because of these limitations. However, MRI may be useful outside the acute period by more clearly defining the extent and possible source of a stroke. Cerebral Angiography Conventional x-ray cerebral angiography is the "gold standard" for identifying and quantifying atherosclerotic stenoses of the cerebral arteries and for identifying and characterizing other pathologies, including aneurysm, vasospasm, intraluminal thrombi, fibromuscular dysplasia, arteriovenous fistula, vasculitis, and collateral channels of blood flow. Endovascular techniques, which are evolving rapidly, can be used to deploy stents within delicate intracranial vessels, to perform balloon angioplasty of stenotic lesions, and to treat intracranial aneurysms by embolization. Recent studies have documented that intraarterial delivery of thrombolytic agents to patients with acute MCA58 stroke can effectively recanalize vessels and improve clinical outcomes. Although its use is investigational in many centers, cerebral angiography coupled with endovascular techniques for cerebral revascularization may become routine in the near future. Conventional angiography carries risks of arterial damage, groin hemorrhage, embolic stroke, and renal failure from contrast nephropathy, so it should be reserved for situations where less invasive means are inadequate. Ultrasound Techniques Stenosis at the origin of the internal carotid artery can be identified and quantified reliably by ultrasonography that combines a B-mode ultrasound image with a Doppler ultrasound assessment of flow velocity ("duplex" ultrasound). Transcranial Doppler (TCD) assessment of middle, anterior, and posterior cerebral artery flow and of vertebrobasilar flow is also useful. This latter technique can detect stenotic lesions in the large intracranial arteries because such lesions increase systolic flow velocity. In many cases, MR59 angiography combined with carotid and transcranial ultrasound studies eliminates the need for conventional x-ray angiography in evaluating vascular stenosis. Alternatively, CT60 angiography of the entire head and neck can be performed during the initial imaging of acute stroke. Because this images the entire arterial system relevant to stroke, with the exception of the heart, much of the clinician's stroke workup can be completed with one imaging study. Perfusion Techniques Both xenon techniques (principally xenon-CT61) and PET62 can quantify cerebral blood flow. These tools are generally used for research (Chap. 347) but can be useful for determining the significance of arterial stenosis and planning for revascularization surgery. Single photon emission tomography (SPECT), CT perfusion, and MR63 perfusion techniques report relative cerebral blood flow. Since CT imaging is used as the initial imaging modality for acute stroke, many centers now combine both CT angiography and CT perfusion imaging together with the noncontrast CT scan. CT perfusion imaging increases the sensitivity and improves accuracy in imaging ischemic brain. Alternatively, MR perfusion can be combined with MR diffusion imaging to identify the ischemic penumbra as the mismatch between these two imaging sequences (Fig. 349-13). The ability to image the ischemic penumbra allows more judicious selection of patients who may or may not benefit from acute interventions such as thrombolysis or investigational neuroprotective strategies. INTRACRANIAL HEMORRHAGE Hemorrhages are classified by their location and the underlying vascular pathology. Bleeding into subdural and epidural spaces is principally produced by trauma (Chap. 357). Intraparenchymal, intraventricular, and subarachnoid hemorrhage will be considered here. DIAGNOSIS Intracranial hemorrhage is often discovered on noncontrast CT64 imaging of the brain during the acute evaluation of stroke. Since CT is more sensitive than routine MRI2 for acute blood, CT imaging is the preferred method for acute stroke evaluation (Fig. 349-1). The location of the hemorrhage narrows the differential diagnosis to a few entities. Table 349-6 lists the causes and anatomic spaces involved in hemorrhages. EMERGENCY MANAGEMENT Close attention should be paid to airway management since a reduction in the level of consciousness is common. The initial blood pressure should be maintained until the results of the CT65 scan are reviewed. Patients with acute SAH13 should have blood pressure lowered to a normal range with nonvasodilating agents such as nicardipine, labetalol, or esmolol. Patients with cerebellar hemorrhages or with depressed mental status and radiographic evidence of hydrocephalus should undergo urgent neurosurgical evaluation. Based on the clinical examination and CT findings, further imaging studies may be necessary, including MRI2 or conventional x-ray angiography. Stuporous or comatose patients generally are treated presumptively for elevated ICP66, with tracheal intubation and hyperventilation, mannitol administration, and elevation of the head of the bed while surgical consultation is obtained (Chap. 258). SUBARACHNOID HEMORRHAGE Excluding head trauma, the most common cause of SAH13 is rupture of a saccular aneurysm. Other causes include bleeding from a vascular anomaly and extension into the subarachnoid space from a primary intracerebral hemorrhage. Some idiopathic SAHs are localized to the perimesencephalic cisterns and are benign; they probably have a venous or capillary source, and angiography is unrevealing. Saccular ("Berry") Aneurysm Autopsy and angiography studies have found that about 2% of adults harbor intracranial aneurysms, for a prevalence of 4 million persons in the United States; the aneurysm will rupture, producing SAH13, in 25,000 to 30,000 cases per year. For patients who arrive alive at hospital, the mortality rate over the next month is about 45%. Of those who survive, more than half are left with major neurologic deficits as a result of the initial hemorrhage, cerebral vasospasm with infarction, or hydrocephalus. If the patient survives but the aneurysm is not obliterated, the rate of rebleeding is about 20% in the first 2 weeks and about 3% per year afterwards. Given these alarming figures, the major therapeutic emphasis is on preventing the predictable early complications of the SAH. Unruptured, asymptomatic aneurysms are much less dangerous than a recently ruptured aneurysm. The annual risk of rupture for aneurysms 10 mm in size is ~0.1%, and for aneurysms 10 mm in size is ~0.5 to 1%; the surgical morbidity far exceeds these percentages. As more data become available, a true risk-benefit analysis for treating these aneurysms will result. Giant aneurysms, those 2.5 cm in diameter, occur at the same sites (see below) as small aneurysms and account for 5% of cases. The three most common locations are the terminal internal carotid artery, MCA67 bifurcation, and top of the basilar artery. Their risk of rupture is about 6% in the first year after identification and may remain high indefinitely. They often cause symptoms by compressing the adjacent brain or cranial nerves. Mycotic aneurysms are usually located distal to the first bifurcation of major arteries of the circle of Willis. Most result from infected emboli due to bacterial endocarditis causing septic degeneration of arteries and subsequent dilatation and rupture. Whether these lesions should be sought and repaired prior to rupture, or left to heal spontaneously, is controversial. PATHOPHYSIOLOGY Saccular aneurysms occur at the bifurcations of the large to medium-sized intracranial arteries; rupture is into the subarachnoid space in the basal cisterns and often into the parenchyma of the adjacent brain. Approximately 85% of aneurysms occur in the anterior circulation, mostly on the circle of Willis. About 20% of patients have multiple aneurysms, many at mirror sites bilaterally. As an aneurysm develops, it typically forms a neck with a dome. The length of the neck and the size of the dome vary greatly and are factors that are important in planning neurosurgical obliteration or endovascular embolization. The arterial internal elastic lamina disappears at the base of the neck. The media thins, and connective tissue replaces smooth-muscle cells. At the site of rupture (most often the dome) the wall thins, and the tear that allows bleeding is often no more than 0.5 mm long. Aneurysm size and site are important in predicting risk of rupture. Those 7 mm in diameter and those at the top of the basilar artery and at the origin of the posterior communicating artery are at greater risk of rupture. CLINICAL MANIFESTATIONS Most unruptured intracranial aneurysms are completely asymptomatic. Symptoms are usually due to rupture and resultant SAH13. At the moment of aneurysmal rupture with major SAH, the ICP68 suddenly rises. This may account for the sudden transient loss of consciousness that occurs in nearly half of patients. Sudden loss of consciousness may be preceded by a brief moment of excruciating headache, but most patients first complain of headache upon regaining consciousness. In 10% of cases, aneurysmal bleeding is severe enough to cause loss of consciousness for several days. In about 45% of cases, severe headache associated with exertion is the presenting complaint. The patient often calls the headache "the worst headache of my life." Occasionally these ruptures may present as headache of only moderate intensity or as a change in the patient's usual headache pattern. The headache is usually generalized, often with neck stiffness, and vomiting is common. Although sudden headache in the absence of focal neurologic symptoms is the hallmark of aneurysmal rupture, focal neurologic deficits may occur. Anterior communicating artery or MCA69 bifurcation aneurysms may rupture into the adjacent brain or subdural space and form a hematoma large enough to produce mass effect. The common deficits that result include hemiparesis, aphasia, and abulia. Occasionally, prodromal symptoms suggest the location of a progressively enlarging unruptured aneurysm. A third cranial nerve palsy, particularly when associated with pupillary dilatation, loss of ipsilateral (but retained contralateral) light reflex, and focal pain above or behind the eye, may occur with an expanding aneurysm at the junction of the posterior communicating artery and the internal carotid artery. A sixth nerve palsy may indicate an aneurysm in the cavernous sinus, and visual field defects can occur with an expanding supraclinoid carotid or anterior cerebral artery aneurysm. Occipital and posterior cervical pain may signal a posterior inferior cerebellar artery or anterior inferior cerebellar artery aneurysm. Pain in or behind the eye and in the low temple can occur with an expanding MCA70 aneurysm. Thunderclap headache is a variant of migraine that simulates a SAH13. Before concluding that a patient with sudden, severe headache has thunderclap migraine, a definitive workup for aneurysm or other intracranial pathology is required. Aneurysms can undergo small ruptures and leaks of blood into the subarachnoid space, so-called sentinel bleeds. Sudden unexplained headache at any location should raise suspicion of SAH13 and be investigated, because a major hemorrhage may be imminent. DELAYED NEUROLOGIC DEFICITS There are four major causes of delayed neurologic deficits: rerupture, hydrocephalus, vasospasm, and hyponatremia. 1. Rerupture. The incidence of rerupture of an untreated aneurysm in the first month following SAH13 is ~30%, with the peak in the first 7 days. Rerupture is associated with a 60% mortality and poor outcome. Early treatment eliminates this risk. 2. Hydrocephalus. Acute hydrocephalus can cause stupor and coma. More often, subacute hydrocephalus develops over a few days or weeks and causes progressive drowsiness or slowed mentation (abulia) with incontinence. Hydrocephalus is differentiated from cerebral vasospasm with a CT71 scan, TCD72 ultrasound, or conventional x-ray angiography. Hydrocephalus may clear spontaneously or require temporary ventricular drainage. Chronic hydrocephalus may develop weeks to months after SAH13 and manifest as gait difficulty, incontinence, or impaired mentation. Subtle signs may be a lack of initiative in conversation or a failure to recover independence. 3. Vasospasm. Narrowing of the arteries at the base of the brain following SAH13 causes symptomatic ischemia and infarction in ~30% of patients and is the major cause of delayed morbidity and death. Signs of ischemia appear 4 to 14 days after the hemorrhage, most often at 7 days. The severity and distribution of vasospasm determine whether infarction will occur.Delayed vasospasm is believed to result from direct effects of clotted blood and its breakdown products on the artery. In general, the more blood that surrounds the arteries, the greater the chance of symptomatic vasospasm. Spasm of major arteries produces symptoms referable to the appropriate vascular territory (see "Stroke Syndromes," above). All of these focal symptoms may present abruptly, fluctuate, or develop over a few days. In most cases, focal spasm is preceded by a decline in mental status.Vasospasm can be detected reliably with conventional x-ray angiography, but this invasive procedure is expensive and carries risk of stroke and other complications. TCD73 ultrasound is based on the principle that the velocity of blood flow within an artery will rise as the lumen diameter is narrowed. By directing the probe along the MCA74 and proximal ACA75, carotid terminus, vertebral, and basilar arteries on a daily or everyother-day basis, vasospasm can be reliably detected and treatments initiated to prevent cerebral ischemia (see below). CT76 angiography is another method that can reliably detect vasospasm.Severe cerebral edema in patients with infarction from vasospasm may increase the ICP77 enough to reduce cerebral perfusion pressure. Treatment is with mannitol and hyperventilation (Chap. 258). 4. Hyponatremia. Hyponatremia may be profound and develop quickly in the first 2 weeks following SAH13. It usually results from inappropriate secretion of vasopressin (Chap. 319) and secretion of atrial and brain natriuretic factors, which produce a natriuresis. This "cerebral salt-wasting syndrome" clears over the course of 1 to 2 weeks and, in the setting of SAH, should not be treated with free-water restriction as this may increase the risk of stroke (see below). LABORATORY EVALUATION AND IMAGING (FIG. 349-14) The hallmark of aneurysmal rupture is blood in the cerebrospinal fluid (CSF). More than 95% of cases have enough blood to be visualized on a high-quality noncontrast CT78 scan obtained within 72 h. If the scan fails to establish the diagnosis of SAH13 and no mass lesion or obstructive hydrocephalus is found, a lumbar puncture should be performed to establish the presence of subarachnoid blood. Lysis of the red blood cells and subsequent conversion of hemoglobin to bilirubin stains the spinal fluid yellow within 6 to 12 h of SAH. This xanthochromic spinal fluid peaks in intensity at 48 h and lasts for 1 to 4 weeks, depending on the amount of subarachnoid blood. The extent and location of subarachnoid blood on noncontrast CT79 scan help locate the underlying aneurysm, identify the cause of any neurologic deficit, and predict delayed vasospasm. A high incidence of symptomatic vasospasm in the MCA80 and ACA81 has been found when early CT scans show subarachnoid clots 5 3 mm in the basal cisterns or layers of blood 1 mm thick in the cerebral fissures. CT scans less reliably predict vasospasm in the vertebral, basilar, or posterior cerebral arteries. Lumbar puncture prior to an imaging procedure is indicated only if a CT82 scan is not available at the time of the suspected SAH13. Once the diagnosis of hemorrhage from a ruptured saccular aneurysm is suspected, four-vessel conventional x-ray angiography (both carotids and both vertebrals) is generally performed to localize and define the anatomic details of the aneurysm and to determine if other unruptured aneurysms exist (Fig. 349-14). CT angiography is an alternative method for locating the aneurysm and may be sufficient to plan definitive therapy. At some centers, the ruptured aneurysm can be treated using endovascular techniques at the time of the initial angiogram (see below). The ECG83 frequently shows ST-segment and T-wave changes similar to those associated with cardiac ischemia. Prolonged QRS complex, increased QT interval, and prominent "peaked" or deeply inverted symmetric T waves are usually secondary to the intracranial hemorrhage. There is evidence that structural myocardial lesions produced by circulating catecholamines may occur after SAH13, causing reversible cardiomyopathy sufficient to cause shock or congestive heart failure. Serious ventricular dysrhythmias are unusual. Close monitoring (daily or twice daily) of electrolytes is important because hyponatremia can occur precipitously during the first 2 weeks following SAH13 (see above). TREATMENT Early aneurysm repair prevents rerupture and allows the safe application of techniques to improve blood flow (e.g., induced hypertension and hypervolemia) should symptomatic vasospasm develop. An aneurysm can be "clipped" by a neurosurgeon or "coiled" by a neurointerventional radiologist. Surgical repair involves placing a metal clip across the aneurysm neck, thereby immediately eliminating the risk of rebleeding. This approach requires craniotomy and brain retraction, which is associated with neurologic morbidity. The newer endovascular technique involves placing platinum coils within the aneurysm via a catheter that is passed from the femoral artery. The aneurysm is packed tightly to enhance thrombosis and over time is walled-off from the circulation (Fig. 349-14). The only prospective randomized trial of surgery versus endovascular treatment for ruptured aneurysm, the International Study of Aneurysm Treatment (ISAT), was terminated early when 24% of patients treated with endovascular therapy were dead or dependent at 1 year compared to 31% treated with surgery, a 23% relative reduction. However, some aneurysms have a morphology that is not amenable to coiling, and only a few endovascular centers are available world-wide. Thus, surgery remains an important treatment option. The medical management of SAH13 centers on protecting the airway, managing blood pressure before and after aneurysm treatment, preventing rebleeding prior to treatment, managing vasospasm, treating hydrocephalus, treating hyponatremia, and preventing pulmonary embolus. Intracranial hypertension following aneurysmal rupture occurs secondary to subarachnoid blood, parenchymal hematoma, acute hydrocephalus, or loss of vascular autoregulation. Patients who are stuporous should undergo emergent ventriculostomy to prevent cerebral ischemia from high ICP84. Medical therapies designed to combat raised ICP (e.g., mild hyperventilation, mannitol, and sedation) can also be used as needed (Chap. 258). High ICP refractory to treatment is a poor prognostic sign. Prior to definitive treatment of the ruptured aneurysm, care is required to maintain adequate cerebral perfusion pressure while avoiding excessive elevation of arterial pressure. Occasionally an intracranial hematoma causing neurologic deterioration requires removal. Because rebleeding is common, all patients who are not candidates for early aneurysm repair are put on bed rest in a quiet room and are given stool softeners to prevent straining. If headache or neck pain is severe, mild sedation and analgesia are prescribed. Extreme sedation is avoided because it can obscure changes in neurologic status. Adequate hydration is necessary to avoid a decrease in blood volume predisposing to brain ischemia. Seizures are uncommon at the onset of aneurysmal rupture. The quivering, jerking, and extensor posturing that often accompany loss of consciousness are probably related to the sharp rise in ICP85 or, perhaps, acute generalized vasospasm. However, phenytoin is often given as prophylactic therapy since a seizure may promote rebleeding. Glucocorticoids may help reduce the head and neck ache caused by the irritative effect of the subarachnoid blood. There is no good evidence that they reduce cerebral edema, are neuroprotective, or reduce vascular injury, and their routine use therefore is not recommended. Antifibrinolytic agents are not routinely prescribed but may be considered in patients in whom aneurysm treatment cannot proceed immediately. They are associated with a reduced incidence of aneurysmal rerupture but are also associated with an increased incidence of delayed cerebral infarction and DVT86. Vasospasm remains the leading cause of morbidity and mortality following aneurysmal SAH13 and treatment of the aneurysm. Treatment with the calcium channel antagonist nimodipine (60 mg orally every 4 h) improves outcome, perhaps by preventing ischemic injury rather than reducing the risk of vasospasm. Nimodipine can cause significant hypotension in some patients, which may worsen cerebral ischemia in patients with vasospasm. Symptomatic cerebral vasospasm can also be treated by increasing the cerebral perfusion pressure by raising mean arterial pressure through plasma volume expansion and the judicious use of vasopressor agents, usually phenylephrine or dopamine. Raised perfusion pressure has been associated with clinical improvement in many patients, but high arterial pressure may promote rebleeding in unprotected aneurysms. Treatment with induced hypertension and hypervolemia generally requires monitoring of arterial and central venous pressures. Volume expansion helps prevent hypotension, augments cardiac output, and reduces blood viscosity by reducing the hematocrit. This method is called "triple-H" (hypertension, hemodilution, and hypervolemic) therapy. If symptomatic vasospasm persists despite optimal medical therapy, intraarterial vasodilators and percutaneous transluminal angioplasty are considered. Vasodilatation following angioplasty appears to be permanent, allowing triple-H therapy to be tapered sooner. The pharmacologic vasodilators (verapamil and nicardipine) do not last more than 8 to 24 h, and therefore multiple treatments may be required until the subarachnoid blood is reabsorbed. Acute hydrocephalus can cause stupor or coma. It may clear spontaneously or require temporary ventricular drainage. When chronic hydrocephalus develops, ventricular shunting is the treatment of choice. Free-water restriction is contraindicated in patients with SAH13 at risk for vasospasm because hypovolemia and hypotension may occur and precipitate cerebral ischemia. Many patients continue to experience a decline in serum sodium despite receiving parenteral fluids containing normal saline. Frequently, supplemental oral salt coupled with normal saline will mitigate hyponatremia, but often patients also require hypertonic saline. Care must be taken not to correct serum sodium too quickly in patients with marked hyponatremia of several days' duration, as central pontine myelinolysis (Chap. 258) may occur. All patients should have pneumatic compression stockings applied to prevent pulmonary embolism. Systemic heparin is contraindicated in patients with ruptured and untreated aneurysms; it is a relative contraindication following craniotomy, and it may delay thrombosis of a coiled aneurysm.