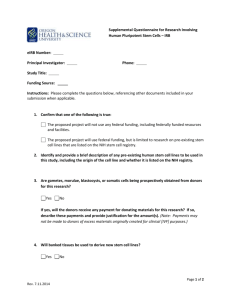
PBSC 8.27.12

GUIDELINES FOR PERIPHERAL BLOOD STEM CELL MOBILIZATION
Grading system for ranking recommendations in clinical guidelines:
(Kish MA. Guide to Development of Practice Guidelines. Clin Infectious Disease. 2001; 32: 851-4)
Strength of Recommendations
A Good evidence to support a recommendation for use
B
C
D
E
Moderate evidence to support a recommendation for use
Poor evidence to support a recommendation
Moderate evidence to support a recommendation against use
Good evidence to support a recommendation against use
Quality of Evidence
Type I
Type II
Evidence from ≥ 1 properly randomized, controlled trial
Evidence from ≥ 1 well-designed clinical trial, without randomization; from cohort or case-controlled analytic studies (preferably from > 1 center); from multiple time-series;
Type III or from dramatic results from uncontrolled experiments
Evidence from opinions of respected authorities, based on clinical experience, descriptive studies, or reports of expert committees
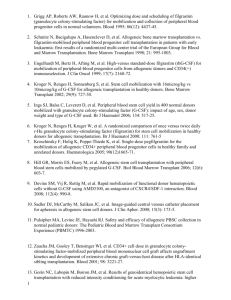
Table 1. Allogeneic Donors
Recommendation References
What is the best myeloid growth factor and dose schedule for mobilization?
What are the target
CD34
+
doses for collection?
Filgastrim 10µg/kg/day, as a single dose, or 5µg/kg twice daily, with leukapheresis beginning on the 5 th day
Pegfilgrastim 6-12mg/day as a single dose
Plerixafor 240µg/kg as single agent
For matched sibling transplants:
Optimal ≥ 4 x 10 6
CD34+ cells/kg
Maximum 8 x 10
6
CD34+ cells/kg
For matched unrelated donor transplants:
Optimal ≥ 4.5 x 10 6
CD34+ cells/kg
For haploidentical transplants:
Minimum > 5 x 10
6
CD34+ cells/kg
Maximum 10 x 10 6 CD34+ cells/kg
Strength of
Recommendation
A
C
B
A
A
B
Quality of
Evidence
I
II
II
II
II
III
1-5
6
7
8
9,10
11,12
Can plerixafor be used for normal donors?
What type of venous access is acceptable for normal donors?
Current data does not support use
Table 2. Autologous Donors
For adult donors:
Peripheral catheters are preferred, but central catheters are acceptable
For pediatric donors:
Either peripheral catheters or central catheters place under general anesthesia
Recommendation
What is the optimal myeloid growth factor and dose schedule for mobilization?
What type of chemotherapy and dose?
For growth factor only stem cell mobilization:
Filgrastim 10µg/kg/day, as a single dose, with leukapheresis beginning on the 5 th
day
Pegfilgrastim 12mg, as a single dose
For chemotherapy combined with growth factor for stem cell mobilization:
Filgrastim 5-10µg/kg/day, as a single dose, beginning > 2 days after chemotherapy administration with leukapheresis initiated when peripheral blood stem cell count or white blood cell count adequate
Pegfilgrastim 6-12mg/day, as a single dose
Disease-specific chemotherapy
Cytoxan 1.5-4g/m2
Etoposide 375mg/m2 for two days or 2g/m2 as single dose
C
B
B
Strength of
Recommendation
A
B
A
A
A
A
II
III
III
Quality of
Evidence
I
II
I
I
II
II
13
14
15
References
4
5,6
7
2
3
1
What are the target goals for collection?
When should plerixafor be used?
When should you begin monitoring peripheral
CD34+ counts?
When should you initiate leukapheresis?
Minimum of 2 x 10
6
CD34
+ cells/kg. Optimal number 5 x
10
6
CD34
+
cells/kg
Higher number of cells have been associated with improved outcomes
In patients with multiple myeloma previously receiving
>4 cycles of lenalidomide
Upfront in lymphoma or myeloma patients at high risk of stem cell mobilization failure
On re-mobilization attempts
For growth factors alone:
Beginning on the 3 rd
or 4 th
day of G-CSF
For growth factors and chemotherapy:
Beginning after hematopoetic recovery and the WBC>1000
For growth factors and plerixafor:
Beginning on the following day of plerixafor administration
For growth factors alone:
On the 4 th or 5 th day of G-CSF administration, if peripheral
CD34
+
cell count >20
For growth factors and chemotherapy:
Peripheral CD34+ cell count>20 or if peripheral CD34+ cell count not available, consider when WBC > 5K and platelet count >75K
A
A
A
B
B
B
A
II
III
III
III
I
II
11,12
13
8, 9
10
Table 3. Stem Cell Processing Guidelines
What is the optimal An International method for CD34+ cell enumeration?
Society of
Hematotherapy and
Graft Engineering
(ISHAGE) double or single-platform protocol should be used.
What is the optimal blood volume to be processed?
A large volume (3-4 times blood volume) leukapheresis should be performed, except for in pediatric patients.
A
A
I 1,2
II 3-5
References:
Allogeneic Donors
1.
Anderlini P, Donato M, Lauppe MJ, et al. A comparative study of once-daily versus twice-daily filgrastim administration for the mobilization and colletion of CD34+ peripheral blood progenitor cells in normal donors. Br J Haematol. 2000; 109:770-772.
2.
Martinez C, Urbano-Ispizua A, Marin P, et al. Efficacy and toxicity of a high-dose G-CSF schedule for peripheral blood progenitor cell mobilization in healthy donors. Bone Marrow Transplant. 1999; 24(12):
1273-8.
3.
Engelhardt M, Bertz H, Afting M, et al. High-versus standard-dose filgrastim (rhG-CSF) for mobilization of peripheral-blood progenitor cells from allogeneic donors and CD34(+) immunoselection. J Clin Oncol. 1999; 17(7): 2160-72.
4.
Ings SJ, Balsa C, Leverett D, et al. Peripheral blood stem cell yield in 400 normal donors mobilized with granulocyte colony-stimulating factor (G-CSF): impact of age, sex, donor weight and type of G-
CSF used. Br J Haematol 2006; 134: 517-25.
5.
Kroger N, Renges H, Kruger W, et al. A randomized comparison of once versus twice daily r-Hu granulocyte colony-stimulating factor (filgrastim) for stem cell mobilziation in healthy donors for allogeneic transplantation. Br J Haematol 2000; 111:761-5.
6.
Kroschinsky F, Holig K, Poppe-Thiede K, et al. Single-dose pegfilgrastim for the mobilization of allogeneic CD34+ peripheral blood progenitor cells in healthy family and unrelated donors.
Haematologica. 2005; 90(12):1665-71.
7.
Devine SM, Vij R, Rettig M, et al. Rapid mobilization of functional donor hematopoeitic cells without
G-CSF using AMD3100, an antagonist of the CXCR4/SDF-1 interaction. Blood. 2008; 112(4):990-8.
8.
Zaucha JM, Gooley T, Bensinger WI, et al. CD34 cell dose in granulocyte colony-stimulating factormobilized peripheral blood mononuclear cell grafts affects engraftment kinetics and development of extensive chronic graft-versus-host disease after human leukocyte antigen-identical sibling transplantation. Blood. 2001; 98(12):3221-7.
9.
Pulsipher MA, Chitphakdithai P, Logan BR, et al. Donor, recipient and transplant characteristics as risk factors after unrelated donor PBSC transplantation: beneficial effects of higher CD34+ cell dose. Blood
2009; 114:2606-16.
10.
Nakamura R, Auayporn N, Smith DD, et al. Impact of graft cell dose on transplant outcomes following unrelated donor allogeneic peripheral blood stem cell transplantation: higher CD34+ cell doses are associated with decreased relapse rates. Biol Blood Marrow Transplant. 2008; 14(4): 449-57.
11.
Champlin R, Hesdorffer C, Lowenberg, et al. Haploidentical “megadose” stem cell transplantation in acute leukemia: recommendations for a protocol agreed upon at the Perugia and Chicago meetings.
Leukemia 2002; 16: 427-7.
12.
Koh LP, Rizzieri DA, Chao NJ. Allogeneic hematopoietic stem cell transplant using mismatched
/haploidentical donors. Biol Blood Marrow Transplant 2007; 13: 1249-67.
13.
Devine SM, Vij R, Rettig M, et al. Rapid mobilization of functional donor hematopoietic cells without
G-CSF using AMD3100, an antagonist of CXCR4/SDF-1 interaction. Blood 2008; 112(4): 990-8.
14.
Pulsipher MA, Chitphakdithai P, Miller JP, et al. Adverse events among 2408 unrelated donors of peripheral blood stem cells: results of a prospective trial from the National Marrow Donor Program.
Blood 2009; 113:3604-3611.
15.
Pulsipher MA, Levine JE, Hayashi RJ, et al. Safety and efficacy of allogeneic PBSC collection in normal pediatric donors: the pediatric blood and marrow transplant consortium experience (PBMTC)
1996-2003. Bone Marrow Transplant 2005; 35(4): 361-7.
Autologous Donors:
1.
Carrion R, Serrano D, Gomez-Pineda A, et al. A randomized study of 10microg/kg/day (single dose) vs
2 x 5microg/kg/day (split dose) G-CSF as stem cell mobilziation regimen in high-risk breast cancer patients. Bone Marrow Transplantation; 2003: 32: 563-567.
2.
Hosing C, Qazilbash MH, Kebriaei P, et al. Fixed-dose single agent pegfilgrastim for peripheral blood progenitor cell mobilization in patients with multiple myeloma. Br J Haematol; 2006: 133(5):533-7.
3.
Andre M, Baudoux E, Bron D, et al. Phase III randomized study comparing 5 or 10 µg per kg per day of filgrastim for mobilization of peripheral blood progenitor cells with chemotherapy, followed by intensification and autologous transplantation in patients with nonmyeloid malignancies. Transfusion.
2003; (43): 50-57.
4.
Russel N, Mesters R, Schubert J, et al. A phase 2 pilot study of pegfilgrastim and filgrastim for mobilizatin peripheral blood progenitor cells in patients with non-Hodgkin’s lymphoam receiving chemotherapy. Haematologica. 2008; 93: 405-412.
5.
Fitoussi O, Perreau V, Boiron JM, et al. A comparison of toxicity following two different dose of cyclophosphamide for mobilization of peripheral blood progenitor cells in 116 multiple myeloam patients. Bone Marrow Transplantation. 2001; 27: 837-842.
6.
Hamadani M, Kochuparambil ST, Osman S, et al. Intermediate-dose versus low-dose cyclophosphamide and granulocyte colony-stimulating factor for peripheral blood stem cell mobilization in patients with multiple myeloma treated with novel induction therapies. Biol Blood Marrow Transplant. 2012; 18(7):
1128-35.
7.
Mahindra A, Bolwell BJ, Rybicki L, et al. Etoposide plus G-CSF priming compared with G-CSF alone in patients with lymphoma improves mobilization without an increased risk of secondary myelodysplasia and leukemia. Bone Marrow Transplantation. 2012; 47:231-235.
8.
Weaver CH, Hazelton B, Birch R, et al. An analysis of engraftment kinetics as a function of the CD34 content of peripheral blood progenitor cell collections in 692 patients after the administration of myeloablative chemotherpay. Blood. 1995; 86: 3961-3969.
9.
Bensinger W, Appelbaum F, Rowley S, et al. Factors taht influence collection and engraftment of autologous peripheral blood-stem cells. J Clin Oncol. 1995; 13: 2547-2555.
10.
Giralt SS, Stadtmaure EA, Harousseau JL, et al. International myeloma working group (IMWG) consensus statement and guidelines regarding the current status of sem cell collection and high-dose therapy for multiple myeloma and the role of plerixafor (AMD 3100). Leukemia. 2009; 23: 1904-1912.
11.
DiPersio JF, Micallef IN, Stiff PJ, et al. Phase III prospective randomized double-blind placebocontrolled trial of plerixafor plus granulocyte colony-stimulating factor compared with placebo plus granulocyte colon-stimulating factor for autologous stem-cell mobilization and transplantation for patients with non-Hodgkin’s lymphoma. J Clin Oncol 2009; 27: 4767-73.
12.
DiPersio JF, Stadtmaur EA, Nademanee A, et al. Plerixafor and G-CSF versus placebo and G-CSF to mobilize hematopoetic stem cells for autologous stem cell transplantation in patients with multiple myeloma. Blood 2009; 113: 5720-6.
13.
Humpe A, Riggert J, Meineke I, et al. A cell-kinetic model of CD34+ cell mobilization and harvest: development of a predictive algorithm for CD34+ cell yeild in PBPC collections. Transfusion. 2000; 40:
1363-70.
Stem Cell Processing Guidelines
1.
Sutherland DR, Anderson L, Keeney M, et al. The ISHAGE guidelines for CD34+ cell determination by flow cytometry. Journal of Hematotherapy 1996; 5: 213-226.
2.
Chapple P, Prince HM, Wall D, et al. Comparison of three methods of CD34+ cell enumeration in peripheral blood: dual-platform ISHAGE protocol versus single-platform microvolume fluorimetry.
Cytotherapy 2000; 2:371-6.
3.
Gasova Z, Marinov I, Vodvarkova S, et al. PBPC collection techniques: standard versus large volume leukapheresis (LVL) in donors and patients. Trans Apher Sci 2005; 32:167-76.
4.
Majado MJ, Minguela A, Gonzalez-Garcia C, et al. Large-volume-apheresis facilitates autologous transplantation of hematopoeitic progenitors in poor mobilizer patients. J Clin Apher 2009; 24(1):12-17.
5.
Bojanic I, Dubravcic K, Batinic D, et al. Large volume leukapheresis: efficacy and safety of processing patient’s total blood volume six times. Transfus Apher Sci 2011; 44(2):139-47.