Paraplegia: Spastic Paraplegia Causes, Symptoms & Management
advertisement
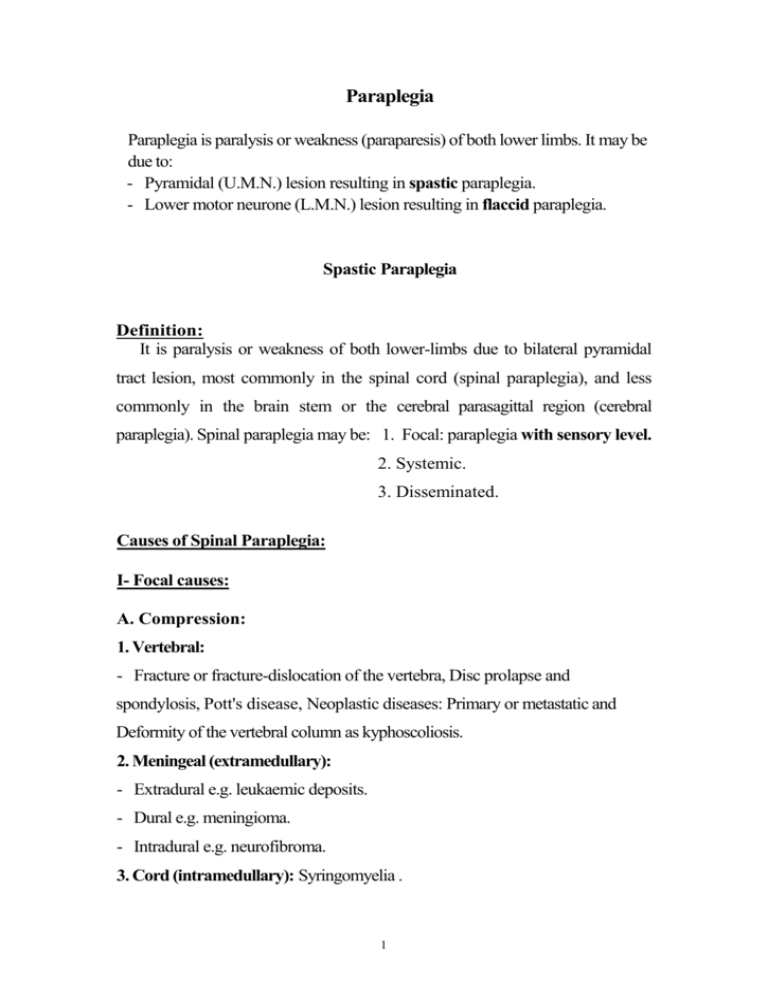
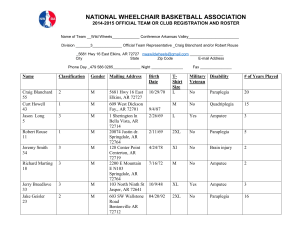
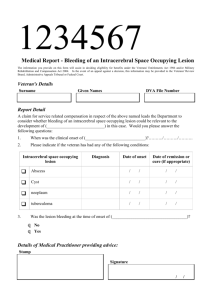
Paraplegia Paraplegia is paralysis or weakness (paraparesis) of both lower limbs. It may be due to: - Pyramidal (U.M.N.) lesion resulting in spastic paraplegia. - Lower motor neurone (L.M.N.) lesion resulting in flaccid paraplegia. Spastic Paraplegia Definition: It is paralysis or weakness of both lower-limbs due to bilateral pyramidal tract lesion, most commonly in the spinal cord (spinal paraplegia), and less commonly in the brain stem or the cerebral parasagittal region (cerebral paraplegia). Spinal paraplegia may be: 1. Focal: paraplegia with sensory level. 2. Systemic. 3. Disseminated. Causes of Spinal Paraplegia: I- Focal causes: A. Compression: 1. Vertebral: - Fracture or fracture-dislocation of the vertebra, Disc prolapse and spondylosis, Pott's disease, Neoplastic diseases: Primary or metastatic and Deformity of the vertebral column as kyphoscoliosis. 2. Meningeal (extramedullary): - Extradural e.g. leukaemic deposits. - Dural e.g. meningioma. - Intradural e.g. neurofibroma. 3. Cord (intramedullary): Syringomyelia . 1 B. Inflammatory: Transverse myelitis - Myelomeningitis - Myeloradiculitis. C. Vascular: Anterior spinal artery occlusion. II. Systemic causes: A systemic disease in neurology is a disease which affects one or more systems selectively and is usually bilateral and symmetrical. When a systemic disease affects the pyramidal tracts, either alone or with other tracts, paraplegia will result. A. Heridofamilial: 1. Hereditary spastic paraplegia. 2. Hereditary ataxias e.g. Friedreich's or Marie's ataxia. B. Symptomatic: 1. Pellagral lateral sclerosis. 2. Subacute combined degeneration. C. Idiopathic: motor neurone disease. III. Disseminated cause: Disseminated Sclerosis (D.S.) Causes of Cerebral Paraplegia: A. Causes in the Parasagittal Region: (area of cortical presentation of L.L.) 1. Traumatic e.g. depressed fracture of the vault of the skull, Subdural haematoma. 2. Vascular e.g. superior sagittal sinus thrombosis. 3. Inflammatory e.g. encephalitis, meningio-encephalitis. 4. Neoplastic e.g. parasagittal meningioma. 5. Degenerative e.g. cerebral palsy. B. Causes in the Brain Stem: Syringobulbia and midline tumors. These lesions arise in the midline and involve the innermost fibers which are those of the lower limbs. 2 Clinical Picture of Focal Paraplegia A. At the level of the lesion: 1. Vertebral manifestations: only present if the cause is vertebral. - Localized pain or tenderness. - Localized deformity or swelling. 2. Radicular manifestations: only present in extra-medullary causes. a) Posterior root affection: - Early pain in the back referred to the distribution of the affected root and described as girdle pain; it is exaggerated by coughing, sneezing and straining. - Later, there is hypoesthesia or anesthesia in the dermatome supplied by the affected root. b) Anterior root affection: localized L.M.N. weakness in the muscles supplied by the affected root. N.B: As the lesion in paraplegia is below the cervical segments (which supply the muscles of the arm), the L.M.N. affection at the level of the lesion is not clinically evident; this is due to the difficulty in eliciting wasting and the difficulty of testing for tone and deep reflexes in the trunk and abdominal muscles. If the lesion involves the cervical segments, there is quadriplegia with evident signs of L.M.N.L. in the upper limbs. B. Below the level of the lesion: (cord manifestations): 1. Motor Manifestations: They depend on whether the cause of the lesion is acute or gradual. a) If the cause is acute (inflammation, vascular or traumatic), the paraplegia passes through 2 stages: • Stage of flaccidity due to neuronal shock: Immediately following the lesion, there is sudden paralysis of the lower 3 limbs, associated with complete loss of tone and absence of reflexes. This stage lasts from 2 to 6 weeks. • Stage of spasticity due to recovery from the neuronal shock: On recovery from the shock stage, the full picture of U.M.N.L. will be established including: hypertonia, hyper-reflexia, positive Babinski sign & may be clonus. b) If the cause is gradual (e.g. neoplastic): atoryThe shock stage is absent and there will be gradual progressive weakness of LL with hypertonia and hyper-reflexia. - The weakness affects distal more than the proximal muscles and the flexor more than the extensors. - The hypertonia and hyper-reflexia affect the extensor group of muscles (antigravity) more than the flexor group (progravity). The paraplegia in this stage is described as (paraplegia in extension) - With further progression of the lesion, the extrapyramidal fibers in the cord will be affected. The hypertonia and hyper-reflexia will be more in the flexor group of muscles than in the extensors. In this stage the paraplegia is described as (paraplegia in flexion). This last stage may be associated with the mass reflex where there is spontaneous urination, defecation and sweating on scratching the skin over the medial side of the thigh. N.B: Piere Marie Foix test is done by firm passive plantar flexing of the toes and foot. This will result in spontaneous "withdrawal reflex" i.e. spontaneous flexion of the hip, knee and dorsiflexion of the ankle if the paraplegia is passing from extension to flexion. 4 1. Cause 2. Hypertonia 3. Position of L.L. 4. Deep reflexes 5. Clonus 6. Mass reflex 7. Bladder Paraplegia in extension Paraplegia in flexion Pyramidal lesion More in extensors Extended Exaggerated Extended Present Absent Precipitancy Pyramidal and extrapyramidal More in flexors Flexed Less exaggerated Absent May be present Automatic bladder 2. Sensory of Manifestations: a) If the cause of the lesion is extramedullary, encroachment on the ascending tracts at the site of lesion results in sensory level below which, all types of sensations are diminished. There is early loss of sensation in the saddle area (S 3, 4, 5), as the sacral fibres lie in the outermost part of the spinothalamic tracts in the cord. b) If the cause of the lesion is intramedullary, there will be a jacket sensory loss (hyposthetic area with normal sensations above and below it). The sensory loss is of a dissociated nature i.e. pain and temperature sensations are lost but touch and deep sensations are preserved; this is due to the interruption of the crossing fibers carrying pain and temperature by the midline lesion, while touch and deep sensation fibers ascend in the posterior column without decussation. The sensations over the saddle area are preserved (sacral spare), as the sacral fibers lie far from the midline lesion. Arrangement of fibers within the spinothalamic tract 5 3. Sphincteric Manifestations: a. In acute lesions: There is retention of urine in the shock stage, followed by precipitancy of micturition. b. In gradual lesions: There is precipitancy of micturition which may terminate in automatic bladder when complete transaction of the cord occurs. * These changes start late in extramedullary lesions and early in intramedullary lesions as the pyramidal fibres controlling the bladder centre lie medially in the cord. Management of Paraplegia I. General: - Frequent change of the patient's posture to guard against bedsores. - Care of the skin by frequent washing with alcohol followed by talc powder. In case of urinary incontinence, frequent change of bed-sheets. - Care of the bladder: If there is retention, use parasympathomimetic drugs. If this fails, use a catheter to evacuate the bladder. II. Physiotherapy III. Symptomatic Treatment: Analgesics and sedatives for pain, Muscle relaxants for the spasticity, Vitamins and tonics. 6 IV. Specific Treatment: (treatment of the cause) 1. Antituberculous drugs in Pott's disease. 2. Deep X—ray in case of intramedullary tumors. 3. Surgical eradication in case of extramedullary tumors. Differentiation between extramedullary & intramedullary lesions Extramedullary Intramedullary 1.Duration Long Short 2.Onset Painful due to posterior Painless History root irritation 3.Bladder Absent or late Early 1. Motor Usually asymmetrical Usually symmetrical 2. Sensory - Sensory level. - All types of sensations are diminished below the level including pain, temp, and touch. - Early loss of sensation in the saddle area. - Jacket sensory loss. - Dissociated sensory loss i.e. loss of pain and temp, with preservation of touch. Possible vertebral lesion Normal disturbance Clinical Picture Plain x-Ray - Late loss of sensation in the saddle area (sacral spare) Modified from: Elwan H: Principles of Neurology.University book center, Cairo, Egypt, 2007. 7