the Campsfield contingency plan
advertisement

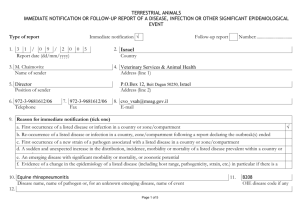
Campsfield House I.R.C. Healthcare Policy No. 7.2 Campsfield House I.R.C. Healthcare Policy No. 7.2 CONTINGENCY PLAN FOR AN OUTBREAK OF FOOD POISONING OR OTHER COMMUNICABLE DISEASE 1 Campsfield House I.R.C. Healthcare Policy No. 7.2 CONTENTS PAGE Objectives 3 Relevant definitions 3 Recognition of outbreak 4 Phase One: Reporting cases of suspected food poisoning or other reportable disease. 4 Phase Two: Institution of Formal Outbreak Control Team. 5 Functions of the Outbreak Control Team 6 Phase Three: At the end of the outbreak 6 Appendices 1b. Universal Infection Control Procedures 7 2. List of Notifiable diseases 9 3. Outbreak Diary of Events 10 2 Campsfield House I.R.C. Healthcare Policy No. 7.2 Many infectious diseases have the capacity to spread within residential establishments where large numbers of people, some of whom may be more susceptible to infection, share eating and living accommodation. The use of Universal Infection Control Procedures can minimise the spread of infection and protect the health of both detainees and staff within the Centre. Guidelines relating to general infection control procedures are included as Appendix 1. More detailed information and guidance are available from on site healthcare staff. During establishment of the healthcare service at the Campsfield House IRC will have established clear and effective communication channels with the local Public Health Department. As part of this communication the Health Centre will have been provided with a reference document relating to infectious diseases which outlines general practical management measures for specific conditions. More specific information will be provided by Public Health at the time they are notified of an incident. This ensures that the management of the situation is based on the most up to date guidelines OBJECTIVES The objectives of this plan are to: 1. Establish procedures to permit the prompt recognition, investigation and control of outbreaks of communicable disease. 2. Reduce the chance of person to person spread. 3. Notify the relevant authorities and prevent a contaminated food source gaining a wider distribution. 4. Comply with the relevant legislation. 5. Formulate action to reduce the risk of similar outbreaks. RELEVANT DEFINITIONS Infectious disease: Any disease caused by growth of pathogenic organisms. It may or may not be communicable. Food borne illness (food poisoning): Any disease of infectious or toxic nature caused by, or thought to be caused, by the consumption of food or water. Water borne illness is defined in similar terms An outbreak: when the observed number of cases exceeds the expected numbers (Generally TWO or more cases.) If any of the above baselines are met there is a need to investigate the incident to establish whether there is an outbreak of food poisoning, communicable or reportable disease in the Centre population. 3 Campsfield House I.R.C. Healthcare Policy No. 7.2 RECOGNITION OF AN OUTBREAK 1. Laboratory surveillance of microbiology reports may indicate an increase in the number of isolates of a single species. 2. Healthcare staff may notice an increased incidence of a specific infection. 3. Residential staff may report an increased incidence of a specific infection to Healthcare. PHASE ONE REPORTING CASE(S) OF SUSPECTED FOOD POISONING OR REPORTABLE DISEASE 1. If any detainee reports sick with symptoms of diarrhoea and/or vomiting or reportable disease (see Appendix 2-List of Notifiable Diseases) this should be reported promptly to the Healthcare Manager and the doctor. 2. Any incidences of staff reporting sick with complaints of diarrhoea and/or vomiting or other reportable disease (see Appendix 2) should be promptly reported to the Centre Manager who will inform the Healthcare Manager/doctor. 3. The Healthcare Manager and the doctor will investigate promptly the reports received by him/her and will: Inform the Centre Director (or Designated Deputy) of the potential problem and the action being taken. Consider the need for isolation of detainees either in the main living accommodation or Healthcare Centre as appropriate. Inform and seek advice from the Environmental Health Officers and Consultant in Communicable Disease Control. Liaise with the microbiology Laboratory Dept re: Arrangements for collection and transport of specimens to the Laboratory for examination. Liaise with the Microbiologist/Public Health Laboratory for receiving urgent reports by telephone or fax. Decide from information available, after due consultations with Consultant in Communicable Disease Control and Environmental Health Officer, whether there is an outbreak of food poisoning or reportable disease in the Centre and advise the Centre Director accordingly. Complete the Certificate of Notification of Infectious Disease or Food 4 Campsfield House I.R.C. Healthcare Policy No. 7.2 Poisoning and forward to the appropriate authorities. Liaise with local hospitals regarding admission of detainees requiring clinical interventions/isolation. PHASE TWO INSTITUTION OF A FORMAL OUTBREAK INVESTIGATION TEAM If there is the potential for a minor and or major outbreak of food poisoning or any other reportable disease the Centre Director will convene an Outbreak Control Team Meeting (OCT) in consultation with The Healthcare Manager, the Consultant in Communicable Disease Control and the Environmental Health Office Representative. In the event of an either a minor or major incident/outbreak it is urgent to convene the first meeting of the Outbreak Control Team as soon as possible after the incident is reported. OUTBREAK CONTROL TEAM (OCT) The core membership of the Outbreak Control Team will be as follows: The Team Chairman will be the Consultant in Communicable Diseases Control, having the power to co-opt other members as required depending on the nature of the outbreak. Centre Manager Consultant in Communicable. Disease Control Public Health Nurse Health Care Manager Centre doctor Immigration Service representative Principal Environmental Health Officer Catering Manager 5 Campsfield House I.R.C. Healthcare Policy No. 7.2 FUNCTIONS OF THE OUTBREAK CONTROL TEAM To define cases of infection, identify and record number of cases, develop a hypothesis concerning mode of spread and causative organism. Suggested documentation included as Appendices 3, 4 and 5. To take the necessary steps for the continuing clinical care of detainees during the outbreak. To identify the resource implications of the outbreak and its management and ensure that these are available. To agree and co-ordinate policy decisions on the investigation and control of the outbreak and ensure that they are implemented. To implement control measures. To monitor the effectiveness of the control measures. To consider the need for outside assistance. To provide clear instructions and / or information to GEO and Drummonds staff. To ensure communication with relevant outside agencies, relatives and media. To review the progress of the outbreak. To define the end of the outbreak. To prepare written reports as necessary. To lead a 'Critical Incident Debrief at the conclusion of the outbreak identifying and communicating lessons learnt. PHASE THREE AT THE END OF THE OUTBREAK The Outbreak Control Team should Review the experience of the participants involved in the management of the incident. To identify shortfalls and particular difficulties. To revise the plan in light of the above. To make recommendations which may reduce the chance of recurrence of the outbreak. 6 Campsfield House I.R.C. Healthcare Policy No. 7.2 Reference should also be made to other policies in this section and also The Practice infection control policies. GEO also have a contingency which dovetails with this one, this may be found on the common drive in the staff information sheet and a hard copy is also attached to this policy for reference. This policy is also written in conjunction with Health Protection Legislation (England) Guidance 2010, a copy of which follows this policy. APPENDIX 1 UNIVERSAL INFECTION CONTROL PROCEDURES Gloves and Aprons Disposable powder free latex or vinyl gloves should be worn for direct contact with blood or body fluid and for direct contact with non intact skin or mucous membranes. Gloves should be discarded after each procedure into yellow bags for incineration. The use of gloves does not preclude the need for thorough hand washing between procedures. Disposable plastic aprons should be worn whenever contamination of clothing with blood or body fluids is anticipated. Hand washing Hands should be washed before all procedures. If the skin is contaminated with blood or body fluid, this should be washed off immediately with soap and water ensuring hands are dried sufficiently with paper towels. Broken Skin Cuts and abrasions in any area of exposed skin, particularly the hands and forearms should be covered with a waterproof dressing. Sharps Extreme care must be exercised during the use and disposal of sharps. Needles, syringes, blades and other sharp instruments should be placed into a rigid sharps container (British Standard). Never resheath, bend or break needles. Discard needle and syringe as one unit. Never overfill the bin and ensure that it is securely closed before disposal. 7 Campsfield House I.R.C. Healthcare Policy No. 7.2 Excreta and Waste Excreta should be disposed of directly into the toilet or sluice. All waste contaminated with blood or body fluid should be discarded into yellow bags for incineration, ensuring no fluid leaks from the bag. Spillages Spills of blood or body fluid should be treated with chlorine granules and left for two minutes, then wearing gloves and aprons, the granules should be removed using paper towels and discarded as clinical waste, the area being washed over with detergent and water. All equipment necessary for the removal of body fluid incidents is contained in the yellow spill packs available throughout the centre. Urine spillages need only be cleaned with soap and water. Every detainee and member of staff should be regarded as a potential risk, therefore, it is essential that good, safe practice is routine. Failure to comply with infection control practices can have severe consequences. It will be the responsibility of the manager to provide the right equipment to maintain good infection control practices. 8 Campsfield House I.R.C. Healthcare Policy No. 7.2 Appendix 2. Diseases notifiable (to Local Authority Proper Officers) under the Health Protection (Notification) Regulations 2010: Acute encephalitis Acute meningitis Acute poliomyelitis Acute infectious hepatitis Anthrax Botulism Brucellosis Cholera Diphtheria Enteric fever (typhoid or paratyphoid fever) Food poisoning Haemolytic uraemic syndrome (HUS) Infectious bloody diarrhoea Invasive group A streptococcal disease and scarlet fever Legionnaires’ Disease Leprosy Malaria Measles Meningococcal septicaemia Mumps Plague Rabies Rubella SARS Smallpox Tetanus Tuberculosis Typhus Viral haemorrhagic fever (VHF) Whooping cough Yellow fever As of April 2010, it is no longer a requirement to notify the following diseases: dysentery, ophthalmia neonatorum, leptospirosis, and relapsing fever. 9 Appendix 3 OUTBREAK DIARY OF EVENTS OUTBREAK CONFIRMED AS……………………………………………. Signature of Centre Doctor…………………………………………………. Action Date Time Healthcare Manager Informed Doctor Informed Centre Manager Informed Consultant in Communicable Disease Informed Environmental Health Officer Informed Outbreak Control Team Convened Interim Report Completed Outbreak confirmed as over Debrief Meeting Final Report Completed 10 Date / Time Action Log of Outbreak Signature - 11 OUTBREAK LOG OF STAFF POSITION NAME STAFF GROUP REPORTED SICK DATE RETURNED COMMENTS 12 OUTBREAK LOG OF DETAINEES NAME ROOM NO. REPORTED SICK H/C OR HOSPITAL ADMISSION DATE CONFIRMED FIT COMMENTS 13 Appendix 4. Public Health Pathways and Contacts Outbreak of Infectious or notifiable Disease; Phone Thames Valley Health Protection Unit Thames Valley Health Protection Unit John Eccles house Robert Robinson Avenue Oxford Science Park OX4 4GP Tel: 0845 2799879 Fax: 0845 2799881 Health Protection Practitioner: Vanessa Baugh Public Health Consultant: Dr Noel McCarthy Author: Date Policy Reviewed: Person Reviewing: Job title: Next Review Date: Drummonds Medical Limited September 2010 Lisa Duff Healthcare Manager April 2013 . 14 15