Availability of Donor Sperm
advertisement

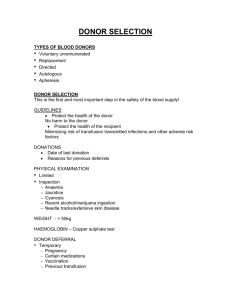
Patient Information: Use of donor sperm SOUTH WEST CENTRE FOR REPRODUCTIVE MEDICINE OCEAN SUITE - LEVEL 6 Derriford Hospital Plymouth PL6 8DH Tel. (01752) 432621 : Fax (01752) 763641 e-mail: plh-tr.ivfinfo@nhs.net - www.plymouthhospitals.nhs.uk USE OF DONOR SPERM Information Sheet Introduction Approximately one in 25 men are unable to father children. This might be for several reasons such as the result of a serious illness such as cancer, or they might be a carrier of a genetically inherited condition. For some men there is no apparent cause at all. Once it has been diagnosed that the male partner is unlikely to be fertile the couple have three choices. One is not to have children and to concentrate on developing their own lives and interests. Secondly, the couple can aim to adopt a child. Unfortunately this is fairly difficult as there are few children for adoption and waiting lists are very long. Also they do not have the shared experience of pregnancy and labour, nor are they able to make any contribution to the genetic make-up of the child. The third choice is to use donor sperm. This has the advantage that the couple can share many of the experiences that a spontaneous pregnancy brings, and half the genetic makeup comes from the mother. More and more patients are also approaching our clinic for DI treatment as a single person or as part of a same sex relationship. Approximately 800 babies are born each year in the UK using donor sperm, eggs or embryos. The experience of people who have had donor conceived children shows that this can be a very positive way to create a family. Availability of Donor Sperm Due to the law change surrounding the loss of anonymity of sperm donors in 2005, there has been a shortage in sperm donors in the UK. This has led us to formulate a waiting list at our clinic for those patients that require donor sperm. To tackle the shortage we have started to recruit our own sperm donors in the South West to build up our own donor sperm bank to enable us to treat patients locally. PI 2.1 – Use of Donor Sperm-V:5 June14r Page 1 of 5 Patient Information: Use of donor sperm Currently are several options available to you: Join the waiting list at Ocean Suite and wait for donor sperm to become available from our own donor sperm bank. This is an ongoing process. There are numerous patients already in treatment that are being offered priority treatment. If you are a new patient, it is most likely that you will need to import from abroad. Import donor sperm from abroad e.g. Denmark. This will enable you to be treated faster, avoiding waiting lists but is a more expensive option. This usually requires a payment for a ‘pregnancy slot’, and then there are the costs of the sperm samples and courier fees to pay on top. Costs can run into the £1000 - £2000 range. If importing from abroad we can only import from certified and accredited laboratories that meet the HFEA’s required standards and EU Tissue Directive standards. Clinics we have imported from include the European Sperm Bank (Nordic Cryobank) and Cryos, both based in Denmark and both with websites. Go to another clinic with an active sperm bank for treatment e.g. Cardiff, London. If you do not want to wait for treatment another option would be to go for treatment at a different UK clinic such as Cardiff or London (e.g. LWC, Bridge) who have their own donor sperm banks. Purchase donor sperm from other UK clinics. Clinics such as the Bridge (London) run donor share schemes. Costs will be similar to that of importing from abroad. Find your own known donor for your own treatment and bring them to the clinic for assessment of suitability. You may know someone who will volunteer to be a sperm donor for you. We would need to assess the potential donor for their suitability. This would involve the same processes that we use when we recruit our own donors such as blood tests, STD testing, and a basic semen analysis. Please note - no payments should be made to the donor for their donations apart from reimbursements for travel and loss of earnings in line with legal requirements as set out by the HFEA. Donor selection & recruitment The recruitment of donors is very carefully controlled by our unit and other licensed centres from whom we may obtain supplies. Particular attention is paid to the health and potential fertility of the donor. A detailed family history of the donor is also taken and the donor is excluded where there is a possible hereditary (genetic) illness. In accordance with Government guidelines, all donors are tested for HIV, Hepatitis B and C and they are screened for sexually transmitted diseases. We also check their karyotype (the chromosomal makeup of the donor) and make sure they do not carry the gene for cystic fibrosis. Donors are tested before they start donating and then again after 180 days, which is the quarantine period. We cannot give an absolute guarantee that no infection will be acquired through donor insemination but the likelihood of this happening is small and to date we do not know of any case where this has happened using the current screening techniques. PI 2.1 – Use of Donor Sperm-V:5 June14r Page 2 of 5 Patient Information: Use of donor sperm Chances of Conception There are several different treatment options available to you, and some maybe more suitable for you than others. This will be discussed at your doctor’s consultation. The different types of treatment include: Donor Insemination – is where thawed sperm is placed onto the woman’s cervix Donor Intra Uterine Insemination – is where prepared thawed sperm is placed inside the woman’s uterus (with or without mild drug stimulation) Donor IVF – is where a woman’s own eggs are inseminated with donor sperm in vitro and embryo(s) are replaced into the uterus. Each treatment type carries a different success rate and a different financial cost. Once conception has been confirmed, the pregnancy should follow a normal course. There is no lower or higher risk of miscarriage, tubal pregnancy or of congenital abnormality than when conception occurs naturally. Regulations A statutory body called the Human Fertilisation and Embryology Authority (HFEA) strictly regulates the whole field of infertility. The law on anonymity changed from 1st April 2005, so that people donating sperm eggs or embryos would do so on the understanding that they would be identifiable to any person conceived as a result of their donation. Once the donor-conceived person reaches the age of 16, they can access information about the number, gender and year of birth of any half or full siblings and non-identifying information about the donor. They can do this either via the clinic or by contacting the HFEA. At 18, all details, both identifying and non-identifying, will be available to the relevant donor-conceived person making a request. They can also find out identifying information about any genetically related siblings if both parties have consented (via the Voluntary Sibling Contact Register VSCR). As parents of a donor conceived child you are allowed to request non-identifying information about the donor and any genetically related siblings your child might have. This includes the pen portrait and good will message the donors are asked to write (as long as these do not contain any identifying information). The donor has no responsibilities or financial obligations to a child resulting from treatment. They can only find out non-identifying information about how many children have been born as a result of their donation, their sex and year of birth. Legal Parentage Regulations In April 2009 new laws about legal parenthood came into force. For married couples, the law will remain unchanged. The husband will be the legal father of any child born as a result of his wife’s treatment, unless it is shown that he did not consent to treatment with his wife. PI 2.1 – Use of Donor Sperm-V:5 June14r Page 3 of 5 Patient Information: Use of donor sperm For unmarried couples, both partners must consent to the male partner being the father in order for him to be legally recognised and named on the child’s birth certificate. For same-sex couples, for lesbian civil partners, the partner who does not give birth will be recognised as the legal second parent and named on the child’s birth certificate unless she did not consent to her partner’s treatment. For those not in a civil partnership, both women must consent to the partner who does not give birth being named as the second legal parent. Unmarried couples should note that even by having the name on the birth certificate does not automatically give him/her full parental responsibility. The couple need to make a parental responsibility agreement or obtain a parental responsibility order under the Children Act of 1989. This applies to any unmarried couple’s child and you are advised to seek your Solicitor’s advice. Counselling You and your partner will be given detailed information about the process. The implications of this treatment for yourselves, your family and any other children will be discussed. The welfare of the child will be an important issue. If you feel you need further discussion or support, please ask, and it will be arranged, free of charge. Coming to terms with infertility can be very difficult and it is essential that treatment by DI is very carefully considered and your decision is not hurried. As far as possible you should try to anticipate your own reaction to the treatment and also to the subsequent pregnancy and the baby, if the treatment is successful. Please do not hurry yourselves into the treatment because you feel that time is passing. Please discuss any uncertainties or anxieties that you may have with the medical or nursing staff. Independent counselling is available if you wish, and our medical or nursing staff will be able to give you more details. Consent You and your partner (if applicable) must consent in writing to the procedure and legal parentage (where appropriate). Telling Your Child? Centres are now required by law to give patients undergoing treatment using donor gametes/embryos information about the importance of telling any resulting child at an early age that they are donor conceived. Whether or not you choose to tell your child about his/her origin by DI is a very personal decision which you, or as a couple must make. More people are deciding to tell their children and there are now individuals and agencies available to help you in this process. The Donor Conception Network (DCN) has a series of booklets called ‘Telling and Talking’ offering parents advice about how to discuss these issues with their children and they are aimed at different age groups. We would like to remind you again, that upon reaching the age of 18, your child will now have the right to submit an application to the Human Fertilisation and Embryology Authority to find out about his/her genetic origin and identifying information about the donor may be made available to the child at this time. PI 2.1 – Use of Donor Sperm-V:5 June14r Page 4 of 5 Patient Information: Use of donor sperm Further Information Listed below are some websites, which you may wish to consult for further information about the use of donor sperm and wider issues. The Human Fertilisation and Embryology Authority website - www.hfea.gov.uk National Gamete Donation Trust website - www.ngdt.co.uk The Donor Conception Network (DCN) – www.donor-conception-network.org PI 2.1 – Use of Donor Sperm-V:5 June14r Page 5 of 5