Guidelines on the use and monitoring of Mycophenolate Mofetil
advertisement

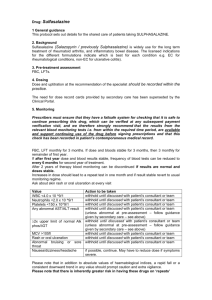
Birmingham Community Rheumatology Service Guidelines on the use and monitoring of disease modyifying anti rheumatic drugs (DMARDS) These guidelines have been produced to provide information about the use and monitoring to the most commonly used DMARDS and are based on the British Society of Rheumatology Guidelines (June 2008). They are not exhaustive and any questions or concerns about DMARDS should be referred to the Birmingham Community Rheumatology Service Telephone 0121 250 0376, Helpline 07595552782, Fax 0121 523 6163 e: rheum.lphc@nhs.net Methotrexate Azathioprine Sulfasalazine Leflunomide Ciclosporin Mycophenolate Mofetil Hydroxychloroquine Sodium Aurothiomalate Summary of monitoring requirements PAGE 1 2 3 4 5 7 8 9 10 Guidelines on the use and monitoring of Methotrexate Methotrexate is an effective treatment for inflammatory joint disease and other auto-immune diseases. Toxicity can occur, but if precautions are taken most patients tolerate oral methotrexate without serious problems. It may take 6 – 12 weeks before any benefit is seen. Patients will have received written and verbal information about the expected benefits and potential side effects of methotrexate therapy. As the tablets are available in both 2.5mg and 10mg strengths and are of similar appearance patients should be advised to check the tablet strength dispensed, patients should also be aware of their weekly dose in milligrams. It is good practice to prescribe 2.5mg tablets to avoid confusion. Methotrexate may also be given by sub-cutaneous injection (see separate protocol). Annual flu vaccination in recommended. Where appropriate patients will be given a record card or booklet on which results can be documented as per National Patient Safety Agency recommendations. Typical dose regime: 10mg once weekly initially Folic acid supplements: increase by 5mg every 2 - 6 weeks to maximum dose of Folic acid 5mg may be prescribed either once weekly or six days weekly as per the prescribers preference. Should not to be taken 25mg weekly. on same day as methotrexate. Contra-indications: Hepatic disease Precautions: Pregnancy or planned pregnancy – Methotrexate Avoid or use with extreme caution in impaired renal function – should ideally be stopped for 3 months prior to monitor renal function conception (for both men and women) Respiratory disease Breast feeding Excess alcohol and smoking should be actively discouraged in Moderate/severe renal impairment patients taking Methotrexate Avoid live vaccines Use with caution in localized or systemic infection Unexplained anaemia or cytopenia associated with Unexplained anaemia or cytopenia associated with bone marrow bone marrow failure failure Side effects : Common – mouth ulcers, nausea, vomiting, diarrhoea, sore throat Notable Drug Interactions: Trimethoprim or Co-Trimoxazole (may precipitate bone Less common - Hair loss, rash, bone marrow suppression – marrow suppression) leucopenia, thrombocytopenia, anaemia. Pneumonitis, neurological Phenytoin (antifolate effect increased) symptoms, abnormal liver function Tolbutamide (increase in serum concentration of methotrexate) Pre treatment assessment: FBC; LFT; U&E’s; Chest x-ray (unless CXR done within last 6 months) Pulmonary function tests may be indicated in patients with pre-existing pulmonary disease Blood monitoring: FBC/ WCC differential, U&E’s & LFT’s - every 2 weeks until dose and monitoring stable for 6 weeks Then monthly until stable for one year Then every 2 – 3 months based on clinical judgement and co-morbidity / dose Withhold until discussed with rheumatology department if: WBC <3.5 x 10 9/l Severe oral ulceration or rash Neutrophils <2.0 x 10 9/l Significant deterioration in renal function Platelets <150 x 10 9/l New or increasing dyspnoea or cough ALT > 3 x normal value or persistently > 2 x normal value Abnormal bruising or sore throat ( withhold until FBC Unexplained fall in Albumin (in absence of active disease) result available) If MCV >105fl serum folate and B12 should be measured In addition to absolute values for haematological indices a rapid fall or consistent downward trend in any value should prompt caution and extra vigilance. If in doubt please contact the rheumatology department. Guidelines based on British Society of Rheumatology Recommendations (June 2008) 1 Department of Rheumatology – Guidelines on the use and monitoring of Azathioprine Azathioprine (Imuran) is an immunosuppressive medication used to treat rheumatoid arthritis and other auto-immune disorders. It is also used as a steroid-sparing agent. Toxicity can occur, but if precautions are taken most patients tolerate azathioprine without serious problems. It may take 6– 12 weeks before any benefit is seen. Annual flu vaccination is recommended. Patients will have been given written and verbal information about the expected benefits and potential side effects of azathioprine. Where appropriate patients will be given a record card or booklet on which blood test results can be documented. Typical dose regime: Initially 25 – 50mg daily increasing over 4 – 6 weeks according to response blood results up to 2 – 3 mg/kg in divided doses. Thiopurine methyl transferase (TPMT) enzyme result should be available prior to dose increase. If TPMT level low discuss with discuss with rheumatologist prior to dose increase. Contra-indications: Precautions: Hepatic disease Use with caution in patients with impaired renal function and TPMT deficiency cardiac failure Immunization with live vacines Sun block and protective clothing should be encouraged to reduce Relative contra-indications: sunlight exposure Breast feeding : limited evidence – it is suggested that Use in caution in localized or systemic infection risks be discussed with the patient and advice sought Pregnancy or planned pregnancy: the risks of continuing therapy from a specialist if necessary versus discontinuation should be discussed with the patient: in patients with systemic or autoimmune disease the risks to the foetus from a flare of the disease is greater than the risk of congenital abnormalities (no increase risk observed) or of immunosupression in the foetus (very rare) Side effects: Common – Mouth ulcers, nausea, vomiting, diarrhoea, sore throat Less common – abnormal LFT’s, neutropenia, leucopenia, hepatitis, hair loss Notable Drug Interactions: Allopurinol (reduced Azathioprine dose indicated) Warfarin (inhibition of anticoagulant effects – warfarin dose may need to be increased) Phenytoin, Sodium valporate & Carbamazepime (azathioprine reduces absorption) ACE inhibitors (may precipitate anaemia - rare) Aminosalicylates and sulfasalazine (may precipitate bone marrow toxicity) Trimethoprim or Co-Trimoxazole (haemotoxicity can occur) Pre treatment assessment: FBC; LFT; U&E’s; TMPT assay Blood monitoring: FBC & LFT’s weekly for first 6 weeks then 2 weekly for further 6 weeks OR 2 weekly for first 12 weeks ( dependent upon individual patient characteristics and prescriber preference), then monthly until dose stable for 6 months. After 6 months if disease and dose stable reduce monitoring to every 2 - 3 months. (If TPMT low levels monthly monitoring should continue) If dose increase check FBC & LFT’s after 2 weeks then monthly for 6 months U&E’s and creatinine 6 - 12 monthly (more frequently if deterioration in renal function suspected) Withhold until discussed with rheumatology department if: WBC <3.5 x 10 9/l ALT > 3 x normal value or persistently > 2 x normal value Neutrophils <2.0 x 10 9/l Abnormal bruising or sore throat (withhold until FBC result available) Platelets <150 x 10 9/l Severe oral ulceration or rash If MCV>105fl investigate further - check serum B12 and folate In addition to absolute values for haematological indices a rapid fall or consistent downward trend in any value should prompt caution and extra vigilance. If in doubt please contact the rheumatology department. Guidelines based on British Society of Rheumatology Recommendations (June 2008) 2 Department of Rheumatology – Guidelines on the use and monitoring of Sulfasalazine (Salazopyrin) Sulfasalazine is used to treat rheumatoid arthritis, psoriatic arthritis and seronegative spondyloarthropathies. It has a slow onset of action 6 – 12 weeks. Enteric-coated tablets should be prescribed as they are better tolerated. Monitoring is required due to potential toxicity. It may be prescribed in combination with other disease modifying drugs or as a monotherapy. Patients will have been given written and verbal information about the expected benefits and potential side effects of Sulfasalazine. Where appropriate patients will be given a record card or booklet on which blood test results can be documented. Typical dose regime: Either: Week 1 - 500 mg daily Week 2 - 500mg twice daily Week 3 - 500mg am & 1gram pm Week 4 - 1gm twice daily OR 500mg twice daily for 2 weeks then increase to 1gm twice daily The dose may be increased to 3 gm daily if no response Contra-indications: Sulphonamide allergy Hepatic disease Severe renal impairment Side effects: Common –Nausea, rash, headache, anorexia, discolouration of urine, tears or soft contact lenses Less common – abnormal LFT’s, neutropenia, leucopenia (usually within first 6 months), hepatitis, sore throat, mouth ulcers. Oligospermia (reversible on discontinuation), photosensitivity Pre treatment assessment: FBC; LFT; U&E’s; Precautions: Moderate renal impairment May impair folate absorption Patients should be asked about rashes or oral ulceration at each visit. Has proved safe in pregnancy but risk/benefit analysis should be undertaken discussed with mother and the dose should not exceed 2 gm daily. Folic acid should be prescribed for those trying to conceive and during pregnancy Men wishing to father children should be advised that spermatogenesis might be impaired causing infertility Breast feeding acceptable as with pregnancy at maternal dose of no more than 2 gm daily Blood monitoring: FBC & LFT’s 2 – 4 weekly monthly for first 3 months (dependent upon individual patient characteristics and clinician preference) Then 3 monthly. If stable after 1-year tests can be 6 monthly for a year, then blood monitoring not strictly required. U&E’s and creatinine 6 – 12 monthly (more frequently if deterioration in renal function suspected) Withhold until discussed with rheumatology department if WBC <3.5. X 10 9/l Neutrophils <2.0 x 10 9/l Platelets <150 x 10 9/l ALT > 3 x normal value or persistently > 2 x normal value Severe oral ulceration or rash New or increasing dyspnoea or cough Nausea/headaches – may need to reduce dose Abnormal bruising or sore throat (withhold until FBC result available) Significant deterioration in renal function If MCV >105fl investigate - check serum B12 and folate In addition to absolute values for haematological indices a rapid fall or consistent downward trend in any value should prompt caution and extra vigilance. If in doubt please contact the rheumatology department. Guidelines based on British Society of Rheumatology Recommendations (June 2008) 3 Guidelines on the use and monitoring of Leflunomide (Arava) Leflunomide (Arava) is indicated for the treatment of rheumatoid and psoriatic arthritis. It has a slightly more rapid onset of action than other disease modifying drugs and therapeutic effect may be seen within 4 – 6 weeks. Monitoring is required due to potential toxicity. It may be used in conjunction with other disease modifying drugs or as a monotherapy. Annual flu vaccination is recommended. Patients will have been given written and verbal information about the expected benefits and potential side effects of Leflunomide. Where appropriate patients will be given a record card or booklet on which blood test results can be documented. Typical dose regime: 10 or 20mg once daily. If patients experience minor side effects at 20mg daily, the dose can be reduced to 10mg daily. Contra-indications: Hepatic disease/ impaired liver function Pregnancy or planned pregnancy/ breast feeding Severe immunodeficiency Moderate or severe renal impairment Severe hypoproteinaemia (nephrotic syndrome) Severe infection Impaired bone marrow function Live vaccines should be avoided Side effects: Common – Mouth ulcers, nausea, vomiting, diarrhoea, sore throat, alopecia, hypertension, skin rash Less common – abnormal LFT’s, hepatitis, bone marrow suppression - neutropenia, leucopenia thrombocytopenia, anaemia, pulmonary complications, weight loss Precautions: Patients should be advised about the use of contraception if applicable, whilst on leflunomide, and for two years after treatment. Localized or systemic infection Notable drug interactions: Phenytoin Tolbutamide Warfarin As Leflunomide has a long half-life washout procedure may be considered if side effects or if an alternative disease modifying drug to be commenced: Cholestyramine 8g TDS for 11 days or Activated charcoal 50g QDS for 11 days. For planned pregnancy the pharmaceutical company should be contacted for advice Pre treatment assessment: FBC; LFT’s; U&E’s; Blood pressure; Weight Blood monitoring: FBC & LFT’s every month for 6 months Then every 2 months Monthly blood pressure . Withhold until discussed with rheumatology department if: WBC <3.5 x 10 9/l ALAT > 3 x normal value or persistently > 2 x normal value Neutrophils <2.0 x 10 9/l Severe oral ulceration or rash Platelets <150 x 10 9/l Abnormal bruising or sore throat (withhold until FBC result available) Shortness of breath In addition to absolute values for haematological indices a rapid fall or consistent downward trend in any value should prompt caution and extra vigilance. If in doubt please contact the rheumatology department. Guidelines based on British Society of Rheumatology Recommendations (June 2008) 4 Guidelines on the use and monitoring of Ciclosporin ( Neoral) Ciclosporin (Neoral) is an immunosuppressive agent, indicated for the treatment of rheumatoid arthritis, psoriatic arthritis and SLE. It can be used as a monotherapy or in combination with methotrexate. It can take up to 12 weeks to take effect. Monitoring is required due to potential toxicity. Patients will have been given written and verbal information about the expected benefits and potential side effects of Ciclosporin. Where appropriate patients will have a record card or booklet on which results can be recorded. Typical dose regime: 2.5mg/kg/day in two divided doses, increasing if indicated after four weeks by 25mg increments to maximum dose of 4mg/kg/day Contra-indications: Precautions: Uncontrolled hypertension Grapefruit juice or grapefruit should not be ingested for one Renal impairment hour prior to Ciclosporin as it may decrease absorption. Avoid live vaccines PUVA therapy in psoriatic arthritis (discuss with dermatology Severe hepatic disease dept.) Severe hyperkalemia Suspected systemic infection Side effects: (Often dose dependent and responsive to dose reduction) Relative contra-indications Common – Hypertension, impaired renal function, Past or current malignancy hypertrichosis, headaches, tremor, fatigue, gingival Pregnancy/planned pregnancy or breast feeding hypertrophy, gastrointestinal disturbances (abdominal pain, (there is experience in the transplant literature but nausea, anorexia, diarrhoea, vomiting), burning sensation of risk/benefit ratio needs careful evaluation in individual hands and feet. cases by an expert in this field) Less common – Hepatic dysfunction, pancreatitis, weight increase, oedema, neuropathy, cramps, muscle weakness, paresthesia, confusion, Notable drug interactions hyperuricaemia, hyperkalaemia, leucopenia, reversible There are multiple drug interactions – detailed below dysmenorrhoea or amenorrhoea Pre treatment assessment: U&E’s; Creatinine X 2 normal prior to commencement 2 weeks apart (mean creatinine value required), FBC, fasting lipids, LFT’s blood pressure x 2 normal 2 weeks apart Monitoring: U & E; s and serum creatinine every 2 weeks until dose and trend stable for 3 months then monthly. FBC, LFT’s monthly until dose and trend stable for 3 months, then 3 monthly. Fasting lipids 6 – 12 monthly Blood pressure at each visit Withhold until discussed with rheumatology department if: Platelets <150 x 10 9/l Abnormal bruising Potassium increase above normal value ALT or alkaline phosphates > 3 x normal value or persistently > 2 x normal value Significant rise in fasting lipds Creatinine rise >30% from baseline ( dose adjustment may be required) Uncontrolled hypertension :If increase in mean diastolic blood pressure >95mmHg – 110mmHg on 2 consecutive occasions commence anti-hypertensive treatment with medication that does not interfere with pharmacokinetics In addition to absolute values for haematological indices a rapid fall or consistent downward trend in any value should prompt caution and extra vigilance. If in doubt please contact the rheumatology department. Guidelines based on British Society of Rheumatology Recommendations (June 2008) 5 Ciclosporin cont……… DRUG INTERACTIONS WITH CICLOSPORIN NEPHROTOXIC AGENTS: NSAID’s Aminoglycosides Amphotericin B Ciprofloxaxin Trimethoprim ACE inhibitors DRUGS WHICH INCREASE CYCLOSPORIN LEVELS Antibiotics: Erythromycin, Clarithromycin, Doxycycline, Antifungals:Fluconazole, Ketoconazole, Itraconazloe, Calcium channel blockers: Nicardipine, Amlodipine, Diltiazem, Verapamil Others: Oral contraceptives, Colchicine, H2 antagonists EFFECTS OF CYCLOSPORIN ON DRUG METABOLISM HMG CoA Reductase inhibitors: Simvastatin, Lovastatin, Atrovastatin Digoxin Prednisolone Nifedipine Colchicine Potassium sparing diuretics/potassium supplements Avoid or reduce dose when practically possible. Monitor renal function DRUGS WHICH DECREASE CYCLOSPORIN LEVELS Anti epileptics: Phenytoin, Carbamazepine, Primdione, Antibiotics: Rifampicin, Trimethoprim, Sulphonamides May increase levels and risk of rhabdomyolysis. (Does not interact with Pravastatin and Fluvastatin May increase levels Reduces clearance Increase rates of gingival hyperplasia noted Reports of muscular toxicity Avoid if risk of hyperkalaeima. Guidelines based on British Society of Rheumatology Recommendations (June 2008) 6 Guidelines on the use and monitoring of Mycophenolate Mofetil (MMF / Cellcept) Mycophenolate Mofetil (MMF) is an immunosuppressant drug originally used as an anti-rejection agent following organ transplantation. MMF is a potent reversible selective inhibitor of purine synthesis, which has been shown to inhibit T cell proliferation and antibody production by B cells. It is used in SLE, Systemic Sclerosis, Vasculitis and other autoimmune disorders. Patients will be given written and verbal information about the medication and potential side effects and where appropriate provided with a record card or booklet on which blood tests can be recorded. Annual flu vaccination is recommended. Typical dose regime: 500mg twice daily for two weeks, then increase if tolerated to 1gm twice daily. Sometimes 2 grams daily (especially Afro-Caribbeans) Contra-indications: Precautions: Severe Hepatic disease Localized or systemic infection Severe renal impairment Suspected lymphoproliferative disorder or unexplained Pregnancy or planned pregnancy thrombocytopenia, leucopenia or anaemia Breast feeding Avoid live vaccines Side effects: Common – nausea, vomiting, diarrhoea, abdominal pain, leucopenia, increased risk of infection, abnormal bruising, Notable Drug interactions: Avoid co administration of antacids with aluminium hydroxide or magnesium, and cholestyramine as absorption may be reduced Acyclovir levels of MMF or acyclovir may be increased Probenecid (increase in plasma concentration of MMF) Less common- Weight loss, Tremors, flushing, lymphadenopathy, rash, visual disturbances, myalgia, dysuria Pre treatment assessment: FBC; LFT; U&E’s; Chest x-ray Blood monitoring: FBC / WCC differential weekly until dose stable for 4 weeks Then 2 weekly for 2 months Then monthly for as long as patient takes drug Withhold until discussed with rheumatology department if: WBC <3.5 x 10 9/l Severe oral ulceration or rash 9 Neutrophils <2.0 x 10 /l Significant deterioration in renal function Platelets <150 x 10 9/l Gastro intestinal disturbances – withhold until settles then re-introduce at lower dose Abnormal bruising or sore throat (withhold until FBC result available) In addition to absolute values for haematological indices a rapid fall or consistent downward trend in any value should prompt caution and extra vigilance. If in doubt please contact the rheumatology department. Guidelines based on British Society of Rheumatology Recommendations (June 2008) 7 Guidelines on the use and monitoring of Hydroxychloroquine (Plaquenil) Hydroxychloroquine (Plaquenil) is used for treatment of rheumatoid arthritis, SLE and discoid lupus. It is make take 12-14 weeks before benefit is noted. Blood monitoring is not required but monitoring of visual acuity should be carried out. Patients will have been given written and verbal information about the expected benefits and potential side effects of hydroxychloroquine. Typical dose regime: 200mg – 400mg daily. Dose should not exceed 6.5mg/kg/day Contra-indications: Severe to moderate renal impairment - reduced dose may be indicated Pre-existing maculopathy Precautions: May be continued during pregnancy/breast feeding Avoid antacids within 4 hrs of dose Epilepsy – threshold for convulsions may be reduced May exacerbate psoriasis Side effects: Common - Rash, nausea, abdominal pain, headache Notable drug interactions: Digoxin - (plasma concentration of digoxin may be increased) Ciclosporin (plasma concentration of ciclosporin may be increased) Amiodorone, moxifloxacin, quinine and mefloquine should not be used concomitantly Less common – Pigmentary skin changes, muscle weakness, Retinopathy Pre treatment assessment: FBC; LFT; U&E’s *Ask about visual impairment (which is not corrected by glasses) Record near visual acuity of each eye (with glasses where appropriate) using reading chart and assess fundi. If visual impairment is present an assessment by an optometrist is advised. If there is any baseline abnormality in the fundi, refer to an ophthalmologist Monitoring: No blood monitoring required Visual Acuity: *Yearly monitoring of visual acuity using the reading chart and enquiring about visual symptoms is recommended –if deterioration from baseline consider referral to optometrist. *Ocular Toxicity and Hydroxychloroquine: Guidelines for Screening 2004 Guidelines based on British Society of Rheumatology Recommendations (June 2008) 8 Guidelines on the use and monitoring of Intra Muscular Gold Inections ( Myocrisin, Sodium Aurothiomalate) Intramuscular gold is used in treatment of rheumatoid arthritis. The benefit may not be noted for 3 – 6 months. Monitoring is required due to potential toxicity even with long-term use. Patients will have been given written and verbal information explaining the expected benefits and potential side effects of gold injections. Typical dose regime: Deep intramuscular to thigh or buttock. Initially a 10mg test dose is given (usually in clinic) 30 minute observation afterwards Followed by weekly injection of 50mg until significant response or until 1000mg given (if no response after total dose 1000mg given treatment should be stopped). Dose interval progressively increased aiming for maintenance dose of 50mg monthly Contra-indications: Severe to moderate renal impairment, Hepatic disease Breast feeding History of blood dyscrasia or exfoliative dermatitis Significant pulmonary fibrosis Systemic Lupus erythematosus Porphyria Avoid live vaccinations Precautions: Mild renal or hepatic impairment Urticaria or eczema Usually contraception during use is advised but may be used at low dose or monthly in pregnancy after discussion of risks/benefits Side effects: Common - Rash, loss of taste or metallic taste, mouth ulcers, nausea, diarrhoea, dizziness, facial flushing Less common – Bone marrow suppression – leucopenia, thrombocytopenia, proteinuria, pneumonitis Pre treatment assessment: U&E’s; Creatinine; FBC;; LFT’s Urinalysis Monitoring: FBC and urinalysis at time of each injection. (The results of the FBC must be available before the next injection (i.e. it is permissible to work one FBC in arrears) Ask about oral ulceration or rash at each visit Withhold until discussed with rheumatology department if WBC <3.5. x 10 9/l >1+ haematuria on> 1 occasion Neutrophils <2.0 x 10 9/l Severe oral ulceration or rash 9 latelets <150 x 10 /l Abnormal bruising or sore throat (withhold until FBC result available) Eosinophillia >0.5 x 10 9/l >2+ proteinuria on > 1 occasion (MSU to exclude infection) In addition to absolute values for haematological indices a rapid fall or consistent downward trend in any value should prompt caution and extra vigilance. If in doubt please contact the rheumatology department. Guidelines based on British Society of Rheumatology Recommendations (June 2008) 9 SUMMARY OF UPDATED DMARD MONITORING GUIDELINES ( Sept 2008) METHOTREXATE: FBC/ WCC differential, U&E’s & LFT’s - every 2 weeks until dose and monitoring stable for 6 weeks Then monthly until stable for one year Then every 2 – 3 months based on clinical judgement and co-morbidity / dose AZATHIOPRINE: FBC & LFT’s weekly for the first 6 weeks then 2 weekly for further 6 weeks OR 2 weekly for first 12 weeks (dependent upon individual patient characteristics and clinician preference) then monthly until dose stable for 6 months. After 6 months if disease and dose stable reduce monitoring to every 2 - 3 months. (If TPMT low levels monthly monitoring should continue) If dose increase check FBC & LFT’s after 2 weeks then monthly for 6 months U&E’s and creatinine 6 - 12 monthly (more frequently if deterioration in renal function suspected) SULFASALAZINE: FBC & LFT’s 2 – 4 weekly monthly for first 3 months (dependent upon individual patient characteristics and clinician preference). Then 3 monthly If stable after 1-year tests can be 6 monthly for a year, then blood monitoring not strictly required. U&E’s and creatinine 6 – 12 monthly (more frequently if deterioration in renal function suspected LEFLUNOMIDE: FBC & LFT’s every month for 6 months Then every 2 months Monthly blood pressure CICLOSPORIN: U & E; s and serum creatinine every 2 weeks until dose and trend stable for 3 months then monthly. FBC, LFT’s every 2 weeks until dose and trend stable for 3 months then 3 monthly Fasting lipids 6 – 12 monthly Blood pressure at each visit MYCOPHENOLATE MOFETIL: FBC / WCC differential weekly until dose stable for 4 weeks Then 2 weekly for 2 months Then monthly for as long as patient takes drug HYDROXYCHLOROQUINE: No blood monitoring required Visual Acuity: *Yearly monitoring of visual acuity using the reading chart and enquiring about visual symptoms is recommended – if deterioration from baseline consider referral to optometrist. SODIUM AUROTHIOMALATE: FBC and urinalysis at time of each injection. (The results of the FBC must be available before the next injection (i.e. it is permissible to work one FBC in arrears) Ask about oral ulceration or rash at each visit Guidelines based on British Society of Rheumatology Recommendations (June 2008) 10