Presenting a Difficult PICU Patient Practice Case
advertisement

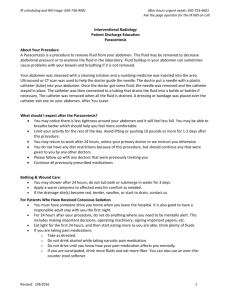
Presenting a Difficult PICU Patient Practice Case Using the resident's guide to presenting patients during PICU morning rounds, the following is an example of presenting a difficult PICU patient on morning rounds. Chart Summary HD 1 14-year-old male admitted from the OR to PICU. Rectal pull through procedure performed under general anesthetic. Extubated and breathing easy in room air with 02 Sats of 93%, awake with good perfusion. Monitored in PICU because of continuous epidural for pain relief. Claforan periop. Family request no blood products for religious reasons. HD 2 Continuous epidural discontinued. Hemoglobin 12.7, BUN 5, Creatinine 1.3. Transferred to general pediatric area. HD 3 Tmax 38.5. Abdominal tenderness. Pain meds adjusted. Ceftriaxone. HD 4 Tmax 39.3. WBC 17,200. Right sided abdominal pain. Upright Chest X-ray shows free air in the abdomen. HD 5 Tmax 39.5. Peritoneal signs. Exploratory Lap, drainage of intra-abdominal feces, excision of rectal mucosa, repair of anastomotic leak, descending colostomy with Hartman's pouch, placement of left subclavian catheter. JP drains. Thirteen liters of fluid required in the OR. Returned to the PICU intubated; ventilated with need for increasing tidal volumes and PEEP; requiring 9 liters of fluid post op and amrinone 10 mcg/kg/min, dopamine 10 mcg/kg/min to maintain a mean blood pressure of 58. Metabolic acidosis, hypocalcium and hypomagnesmia corrected. Vancomycin, cefotaxime and flagyl IV. Zantac IV prophylaxis. Fentanyl and vecuronium infusions. HD 6 High frequency oscillator required for hypoxemia. Bilateral loss of lung volumes as well as pleural effusions. Bilateral 8.5F pigtail chest tubes placed. Persistent metabolic acidosis requiring frequent sodium bicarbonate and THAM supplements. Septic shock, Acute Lung Disease, myocardial dysfunction, oliguric renal failure, disseminated intravascular coagulation, liver failure. Echocardiogram shows poor filling secondary to decreased intravascular volume despite continued fluid resuscitation. Continues on amrinone 10 mcg/kg/min, dopamine 10 mcg/kg/min and now epinephrine 0.1 mcg/kg/min. Fentanyl, versed and atracurium infusions. Vancomycin and timentin now for antibiotic coverage. NPO. Receiving central dextrose 5gm/kg/day, amino acids 1.2 gm/kg/day and 20% intralipd at 0.5 gm/kg/day. H/H 8/24. Request to give blood products denied. Erythropoetin begun. Platelets 163,000,PT 27,PTT 59. Creatinine rising from 1.7 to 2.9. Albumin 0.9, lactate 3.7, SGOT 297. Weight 70.7 kg Increasing abdominal distention leads to exploratory lap, debridement of intra-abdominal pus and silastic patch closure of abdominal wall. Femoral venous and arterial catheters placed and Continuous Arterial Venous Hemofiltration (CAVH) begun without heparinization. Additional femoral artery catheter placed for blood pressure monitoring. HD 7 Switched from oscillator to conventional ventilation because of improved compliance and oxygenation. CAVH continues, now requiring active heparinization. BUN 56, Creatinine 5.1. SGOT 4274, LDH 3974. Gram negative rods from blood and peritoneal cultures. Vancomycin, timentin, gentamycin. Continued metabolic acidosis. Insulin added to TPN solution. HD 8 WBC 38,800. Hematocrit 15. Exploratory lap to drain abscess. Pulmonary artery catheter placed for better monitoring. Blood products refused. HD 9 This morning CAVH changed to Continuous Arterial Venous Hemofiltration with Dialysis. Ultrafiltrate replaced cc per cc with replacement fluid without potassium. Dialysate running at 1000 cc/hour with KCL and NaPhosphate. GI and chest tube drainage replaced. TPN adjusted up. The following is available today at 0630 for more detailed review of the patient's status as you prepare for morning rounds. Clinical exam Chest X-ray Pediatric Intensive Care Daily Flow Sheet Patient Care Kardex Continuous infusion worksheets Respiratory Care Ventilator Flow Sheet Hemodynamic calculations Lab results Emergency Drug Sheet Example of Presenting this Patient during PICU Morning Rounds This is the 9th PICU day for John DOE, a 14 yr old 74.3 kg male remains in the PICU for ongoing support of multiorgan dysfunction after an abdominal abscess complicated his initial repair of newly diagnosed Hirshbrung disease. Post op day # 8 for Rectal pull through procedure Post op day # 4 for Exploratory lap, drainage of intra-abdominal abscess, excision of rectal mucosa, repair of anastomotic leak, descending colostomy with Hartman's pouch, placement of left subclavian catheter Post op day #5 for Exploratory lap, debridement of intra-abdominal pus and silastic patch closure of abdominal wall Post op day #1 for Exploratory lap, drainage of abscess His main problems are: 1. Gram negative peritonitis and sepsis 2. Acute Lung Injury (ARDS) 3. Bilateral pleural effusions 4. Septic shock 5. Severe Anemia, Hbg 4.4 gms/dl 6. Disseminated Intravascular Coagulation 7. Oliguric Renal Failure 8. Gastrointestinal and Liver dysfunction 9. Nutritional compromise 10. Hypo-ionizedcalcemia 11. Hypoalbuminemia 12. Hyperglycemia 13. Hyperphosphatemia 14. Technical difficulties with PA Catheter (low light indicator; CVP reading high when cordis infusing with solutions). System Review: Airway 7.5 cuffed oral endotracheal tube, taped at 22 cm, secure, patent with minimal leak and appropriately positioned on CXR exam. Thick green-tan secretions are present on day 11 of intubation. Plan: Maintain endotracheal tube patency, suction frequently Oxygenation/Ventilation This is day 6 of ventilatory support, 3 of which required high frequency oscillator support for hypoxemia. Presently, while still paralyzed and sedated, a volume controlled velor hamilton is providing adequate oxygenation (Pa02 160mmHG and Sa02 100%) and ventilation (PaC02 36, pH 7.49) on non-toxic Fi02 of 40%, PEEP 5 with some concern about low grade on-going barovolutrauma (PIP 44, TV 11ml/kg). Pleural effusions have resolved with bilateral 8.5F pigtail chest tubes, day #10. 200-500ml /shift chest tube drainage with no air leaks. Plan: Maintain ventilator support, attempt to decrease TV to 6ml/kg and PIP < 35, as long as pH > 7.2 (with or without NaHC03 or THAM) and this doesn't interfere with cardiovascular or neurologic function Maintain chest tubes CPT q4hr Cardiovascular Ongoing septic shock with poor oxygen delivery and oxygen consumption. Plan: - Volume expansion (NSS. Refuses blood and albumin) - Resume dobutamine 10 mck/kg/min - May need mild vasopressor after fluid expanded - PRBC to raise Hbg to 40-45 (refuses blood products) - Replace calcium, 10% calcium chloride 10-20mg/kg slow push over 1 hour, increase calcium in fluid - Continue sedation/paralyzation to minimize oxygen consumption Continue PA catheter monitoring, following oxygen delivery/consumption and Sv02 as make therapeutic changes to maximize oxygen delivery to meet the metabolic needs of the patient. Change oximetric PA catheter - technical problems Check for availability and efficacy of blood substitutes to improve oxygen delivery Appropriate Emergency Drug Sheet at bedside Hematologic Increasing anemia, ongoing caogulopathy and systemic heparinization for CRRT with evidence of ongoing blood loss: - Serosanguinous drainage chest tubes - Serosnaguinous drainage JP drains - Gelatinous red/dark brown drainage from rectal penrose drain Plan: - PRBC (refused) or blood substitute if available - Continue erythropoietin (day 10 (8000u daily IV, 113u/kg/day)) - Iron Dextran - Vitamin K - FFP(refused) - Use just enough heparin to avoid the CRRT filter from clotting(Presently,11u/Kg/hr) - Avoid blood draws if possible Neurologic Suspect borderline cerebral perfusion and oxygen delivery Because he requires continued paralyzation and sedation with atracurium 15 mcg/kg/min, fentanyl .03 mcg/kg/min and ativan .05 mg every 4 hours IV to support cardiopulmonary systems, unable to fully evaluate for ICP, focal neurologic problems or seizures Plan: - Continue efforts to improve global perfusion pressure and oxygen delivery - Peripheral nerve stimulator to titrate parylytic to minimum needs (allow synchronization with vent and decrease oxygen consumption) - If clinically safe, stop paralytic to grossly evaluate neuro status more clearly. - Adjust fentanyl and ativan to pain/sedation needs - appears adequate at present - Lacrilube opthalmic ointment Gastrointestinal Continued peritonitis, gastrointestinal and mild liver dysfunction with continued increased fluid loss from abdominal dressing and colostomy. Plan: - It is not felt safe to begin trophic feeds today. - Carafate 1000mg q6hr NG (56 mg/kg/day) - Aluminum hydroxide and Magnesium hydroxide 30 ml via NG for gastric pH <5.0 - Ranitidine 1mg/kg/day in TPN. - Discuss replacement of colostomy and abdominal dressing losses with surgery and nephrology - Surgery continues to monitor peritonitis and continued surgical needs Example of Presenting this Patient during PICU Morning Rounds (continued) Infectious/Immune Continued systemic inflammatory response syndrome from gram negative sepsis and peritonitis Plan: - Maintain antibiotics (renal failure doses but may need adjustment since on CRRT) - Clavulanate-ticarcillin 3.1G q12h (88 mg/kg/d) - Ciproflaxin 400 mg IV daily (5.6mg/kg/d) - Metronidazole 500 mg MG q6h (7mg/kg/d) - Fluconazole 100 mg IV daily (1.4mg/kg/d) - Sulfadiazine cream to abdominal wound QID with dressing changes - Peritoneal cultures pending from last operation, adjust as needed. - CRRT may be removing "unwanted" cytokines but may also be removing "good" cytokines. However, consider increasing ultrafiltrate rate since there is some evidence of improvement in systemic inflammatory symptoms with increased ultrafiltration rates - Consider blood, tracheal aspirate, urine cultures today- monitoring for nosocomial infections - Monitor for recurrent abscess collection intra-abdominally - Investigate if there are any systemic anticytokines, free radical scavengers, monoclonal antibodies to endotoxin, etc. that are available to assist in subduing the SIRS. Orthopedic/dermatologic Stable Plan: Ostomy care - While paralyzed and heavily sedated - Passive range of motion to extremities - OT/PT - Sneakers to feet to avoid foot drop - Dynamic air bed (rotates/CPT every 2 hours) Renal, Fluid/Electrolytes/Endocrine (*Maintenance IV rate for weight would be 104ml/hr, 2496ml/day) - Continued oliguric renal failure with total body overload but suspected decreased intravascular volume - Mild hyperglycemia (252) - Hypoalbuminemia(3.0) - Hypochloridemia (97) - Hypertriglceridemia (283) - Hyperuricemia (7.5) - CRRT day 4 using an - Amicon 20 Filter, intact - Femoral Arteriovenous CAVH (9 days), CAVH-D (day 1) - Dianeal Impersol 1.5% Dextrose at 1000 ml/hr for dialysis - Ultrafiltrate replacement fluid of 0.45 NACL with 60 mEq/l NaHC03 and 3.5 mEq KCL/L, replace ultrafiltrate cc/cc every hour, post filter (average 500-600ml/hr) - Ultrafiltrate collection bag 18 inches below filter, adjusting height to maintain ultrafiltration rate, averaging 400-600 ml/hr - Heparin 25,000 u/25ml, 800u/hr pre-filter. - Total Ultrafiltrate Replacement Fluid= 9225ml TPN = 2175ml Lipids = 414ml Atracurium infusion = 172ml Fentanyl infusion = 38ml Aline = 71ml PAP = 70ml CVP = 71ml Heparin = 134ml Flushes/meds = 996ml (4141ml/day above maintenance) (Total input without replacement = 172ml/hr) Total In = 13,366 - Total Ultrafiltrate = 9700ml U.O. = 292ml Colostomy = 1840ml Abdominal dressing = 1320 - NG = 450 JP = 28ml Chest tubes = 1021ml Peritoneal = 28ml (total patient output = 207ml/hr) Total out = 14,679 Net negative 1313 ml/24 hr Plan: After feel intravascular replete today, in order to assist with oxygen delivery, will adjust ultrafiltrate replacement fluid to allow slow daily negative balance that helps to reduce total body overload slowly but maintains adequate filling pressures for oxygen delivery needs. Adjust dialysis solution and rate with nephrology input to allow optimal nutrition while kidneys have time to heal Hourly adjustment of ultrafiltrate replacement depending on clinical status with above plans Monitor electrolytes, glucose, PO4, Mg.ionized Ca, BUN, Cr BID Adjust UF replacement fluid as needed to maintain above. Adjust medications because of renal failure and CRRT; ask pharmacology for assistance Nutrition Nutritionally compromised Presently NPO with central nutritional support of Novamine 3.5gm% with 20% Dextrose and 20% Intralipid Received: 36 ml/kg/day (1.03 x maintenance) 37 cal/kg/day 32 NPC/kg/day Total calories 2611: 56% carbohydrate, 32% fat, 11.6% protein. NPC:N ration 190:1 CHO 6.16 gram/kg/day, 4.27mg/kg/min Fat 1.17 gm/kg/day Protein 1.07gm/kg/day Na 4.3 mEq/kg/day K 0.6 mEq/kg/day Mg .07 mEq/kg/day Ca 0.6 mEq/kg/day Acetate 3 mEq/kg/day Cl 1 mEq/kg/day PO4 0.6 mMol/kg/day ZnCl 90 mcg/kg/day MTE-4 .06ml/kg/day MVI-12 0.14 ml/kg/day Ranitidine 1mg/kg/day Iron Dextran 0.7 mg/kg/day Vitamin K 0.14 mg/kg/day Insulin,human 1.2u/kg/day (.05u/kg/hr) Receiving 1u insulin/hr for every 5 grams of glucose an hour Plan: Goals: Metabolic Cart from yesterday suggested 4800 R.E.E. Maximize central TPN calories to come as close as possible to 4800 cal/day, help with tissue repair, assist immune system, improve renal recovery using - Maximum Glucose concentration of 20% to avoid clots, but increase glucose load to 15-20gm/kg/day, keeping glucose calories around 50% of total IV calories. May need to titrate insulin (1u insulin/hr per 5 grams of glucose/hr) to avoid hyperglycemia but this is common with sepsis (glucose intolerance). Watch for evidence of C02 overload from glucose load as try to wean ventilator. - Maximum lipids 3-4gm/kg/day over 24 hours, keeping fat calories at 40% total IV calories, although some believe you need to limit the amount of IV lipids during sepsis. Triglycerides are moderately elevated, common in sepsis. Monitor. - Maximize protein to 2-2.5gm/kg/day, total protein calories about 10% total IV calories and NPC:N ratio 150:1 or better. CRRT will minimize BUN rise. - May need more fluids to deliver this caloric goal but CRRT can be used to adjust total fluid balance. - Increase Cl, decrease PO4, increase insulin in TPN ( 1u insulin/hr for every 5 gram glucose /hr) - If use 20% Dextrose, 3.5% AA solution at 147 ml/h and 20% lipid at 40ml/hr x 24 hours, this will provide: 63ml/kg/day fluid 4813 cal/day (68 cal/kg/day) 61 NPC/kg/day CHO 50%,Fat 40%,Protein 10% calories NPC:N 217:1 CHO 9.98 gm/kg/day, 6.9mg/kg/min Fat 2.7 gm/kg/day Prot 1.75 gm/kg/day Adjust electrolytes,trace minerals, insulin for new rate. Medication Review Type Dose/kg/day Duration of medication Needed? Clavulanate-ticarcillin Metronidazole Ciprofloxacin Sulfadiazine cream to wound Fluconazole Lacrilube to eyes Fentanyl Atracurium Lorazepam Sucralfate Ranitidine Aluminum hydroxide & magnesium hydroxide Heparin Erythropoietin Iron Dextran Vitamin K Insulin, human Patient comfort/pain management/withdrawal support measures in place? Yes Lines, catheters Type Location Duration Needed? 7.5 cuffed oral endotracheal tube NG 7.5 F oximetric PA catheter, left subclavian Bilateral 8.5F pigtail chest tubes Peritoneal catheter JP drains x 2 Colostomy Foley Penrose drain, rectum Femoral arterial line, bilaterally ( one for BP monitoring, one for CRRT) Right femoral venous line Monitoring Type Adequate? Cardiac monitor Continuous arterial pressure Continuous CVP, PAP Intermittent CI, PCWP, O2 delivery, O2 consumption Oximeter Sv02 monitor End tidal C02 monitor Leonardo respiratory mechanics monitor Adding: Peripheral nerve stimulator Changing: Oximetric PA catheter to new one Radiology and lab standing orders Needed? Daily CXR Labs as per system plans Primary caregivers Parents have been updated on clinical care Blood products discussed. Social service and pastoral support in place Discharge planning and teaching is on hold because of seriousness of illness Parents updated on clinical course Referring physician updated? Referring physician will be called today. She called yesterday for update.

![Lymphatic problems in Noonan syndrome Q[...]](http://s3.studylib.net/store/data/006913457_1-60bd539d3597312e3d11abf0a582d069-300x300.png)