Treating Motor Speech Disorders: A Model
advertisement

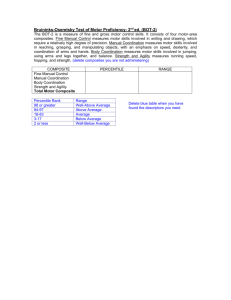
Treating Motor Speech Disorders: A Model-Driven Approach Heather M. Clark, Ph.D. CCC/SLP Foundations of Approach Address impairment, activity, and participation Impairment level treatment is based on sound neurophysiological principles Activity level treatment is based on principles of motor learning Participation level measurement and/or treatment is incorporated throughout management to validate benefits Key Issue: Assessment Effective treatment depends on accurate assessment Identification of underlying impairments Strength Tone Range Coordination Differential diagnosis Dysarthria (type), AOS, Aphasia Designing an intervention plan Functional goals Activity level targets Participation level targets Behavioral objectives Impairment level targets Activity level targets Impairment Level Targets Tone Strength Range Coordination (best addressed at activity level) Strength Training: A principled approach Issues to consider Does underlying weakness contribute to speech (and swallowing) problems? Can strength be improved by training? Will increased strength result in improved function? Physiology review: Motor Units Motor unit: motoneuron and the muscle fibers it innervates Specific motor units are recruited for any given movement Force Speed Direction Principles of strength training Goals Strength Endurance Power Overload Hypertrophy of muscle tissue Increased motor unit recruitment Specificity of training The effects of strength training are highly specific to the trained behaviors This is primarily related to motor learning and motor unit recruitment Factors subject to specificity Force Contraction velocity Duration Dynamics 1 Direction of load Kinematic chain Force Low force: Type I units High force: Type II units If exercise is completed to the point of fatigue, both Type I & II are trained Contraction velocity Power increased by Increasing resistance while maintaining contraction velocity Increasing velocity while maintaining resistance Combination of above Exercises should closely match speed of desired outcome Dynamics Isotonic: muscle changes length while maintaining tension Isometric: muscle changes tension while maintaining constant length (principles apply to length of muscle, hence “range”) Direction of Load Concentric: Resistance applied as muscle shortens Eccentric: Resistance applied as muscle lengthens Kinematic Chain Open: distal segment moves freely Closed: body moves around fixed distal segment Other issues Frequency: amount of time allowed for recovery between training sessions Progression: systematic increase of resistance, contraction velocity, and/or duration Contra-indications for strength training Hypertonia Fatigue Susceptibility Absence of weakness Issues Key descriptors in the oral system Direction of movement Force Speed Integration? Recovery No data are available regarding the optimal frequency of training sessions for oral-pharyngeal musculature Progression Increase resistance Increase repetitions or duration Increase contraction velocity Strength-training as intervention Clearly identify treatment target Strength, endurance, power Direction, duration, and range Match exercise as closely as possible to desired movement outcome Be mindful of overload and progression Be mindful of contra-indications Other Impairment-level Targets Tone Range Tone Hypertonicity Goal is to decrease tone Inhibit stretch reflex Hypotonicity 2 Goal is to increase tone Facilitate stretch reflex Oral Motor Tasks Designed to Influence Tone or Range Slow stretch Fast stretch Massage Heat Cold Vibration Electrical Stimulation Slow stretch Description May be active, passive, or assisted Movements are slow and beyond typical ROM Physiologic impact May inhibit stretch reflexes Loosens connective tissue and adhesions Indications Generally employed to reduce spasticity Contra-indications and cautions May not have same effects in orofacial system Inappropriate stretching can cause discomfort and swelling Support: none Fast stretch Description Usually passive Movements are quick and non-sustained Physiologic impact Intended to elicit stretch reflex Indications Generally employed to increase tone Contra-indications and cautions May not have same effects in orofacial system Inappropriate stretching can cause discomfort and swelling Support: none Massage Description Stroking and/or application of pressure Effleurage, petrissage, friction, tapotement Physiologic impact Loosens connective tissue adhesions, facilitate blood & lymph flow Central and peripheral relaxation Stimulate muscle spindles Indications Generally employed to reduce spasticity (deep friction), increase tone (tapping), or improve ROM related to scar tissue Contra-indications May not have same effects in orofacial system Should not be employed without thorough understanding of tissue morphology Support: Sullivan et al (1997) reported improved phonatory function Heat Description Heat applied to tissue May be deep or superficial Physiologic impact Increases pain threshold 3 Increases blood flow Indications Generally employed to reduce pain associated with ROM Contra-indications and cautions Should not be used on inflamed tissue Should not be used on patients with reduced ability to report pain Support: none (TMJ?) Cold Description Application of cold to superficial tissues Physiologic impact May reduce spasticity by decreasing conduction velocities Increases blood flow Indications Generally employed to reduce spasticity Contra-indications and cautions Should not be used on patients with reduced ability to report pain or discomfort Support: none Note: thermal stimulation affects sensation, not movement Vibration Description Low or high frequency vibratory stimulation Physiologic impact TVR: stimulates muscle spindle; facilitates agonist & inhibits antagonist Indications May be used to increase or decrease tone Contra-indications and cautions May not have same effects in orofacial system Produces heat May damage skin, particularly around the face Should not be used in cerebellar or extrapyramidal lesions Support: none Electrical stimulation Description Low voltage electrical currents applied to muscle fibers Physiologic impact Causes contractions of muscle fibers Indications Generally employed to improve strength and tone Contra-indications and cautions May not have same effects in orofacial system Recruits MU in different order than volitional contractions; limits motor learning Support: Swallowing: Park et al (1997); Freed et al (2001) Impairment Level Targets Increase tone Strength training Fast stretch* Brief cold* Electrical stimulation Vibration to agonist* *may not have same effects in oral system Decrease tone Slow stretch* Sustained cold* Vibration to antagonist* 4 Increase ROM Active or passive ROM / stretch Heat Specific Examples by Subsystem Respiration relaxation or posture adjustment to reduce tone Phonation laryngeal adduction exercises addressing vocal cord paralysis Laryngeal massage addressing spasticity and/or spastic dysphonia Resonation CPAP to train velar elevators Articulation Tongue strengthening to improve articulation Lip stretch to improve ROM Activity Level Targets: Speech Disorders Dysarthria Apraxia Articulation, Voice, Fluency Any intervention focusing on improving integrated movement patterns during speech Specific Examples by Subsystem Respiration Adequate use of available breath support Improved phrase grouping Phonation Easy onset phonation during connected speech Effortful phonation Resonation Appropriate oral/nasal resonance Articulation Exaggerated articulation of consonants and vowels during speech Intelligibility Prosody Slowed rate Principles of Motor Learning Applies to any change in movement behavior related to changes in central motor unit recruitment Relevant to the learning of any skilled movement Some definitions Acquisition Practice (therapy) When recruitment patterns are being established Specificity can be exploited Learning The game (retention and transfer) Recruitment patterns are being refined and generalized Specificity should be overcome In general… Variables that exploit specificity facilitate acquisition but deter learning Variables that confound specificity prolong acquisition but result in better learning Why? Recall and evaluation strategies play a role in motor learning Schema theory (Schmidt, 1998) Getting practice “recalling” movements and “evaluating” movements improves ultimate retention and transfer Variables impacting motor learning Pre-practice variables Practice conditions 5 Feedback Pre-practice variables Motivation Elicitation Instructions Models Practice conditions Scheduling Massed vs distributed practice Variability Constant vs variable Target, context, etc Feedback Type Knowledge of results (KR) Information about outcome Critical for learning Knowledge of performance (KP) Information about movement execution Most important to guide acquisition Temporal Locus Pre KR interval Post KR interval Frequency High frequency speeds acquisition Low frequency promotes learning Motor Learning in Intervention Acquisition: Exploit specificity Blocked practice Consistent practice Frequent, specific feedback (KP) Learning: Overcome specificity Distributed practice Variable practice Reduced feedback, focus on KR Motor Learning in Intervention Always! Treatment activities should closely match intended movement outcome TONS of practice Avoid verbose instructions & feedback When giving KP, have client attend to perceptual information (biofeedback) Additional Implications When learning strategies are integrated into practice, acquisition will slow Outcome assessment must take place outside of practice (therapy) and should incorporate activity and participation measures Case studies Flaccid dysarthria 49 year old s/p resection of medullary tumor resulting in flaccid dysarthria of CN X, XI, XII and significant oropharyngeal dysphagia Predicted impairments? Assessment strategies? Functional goals? Treatment targets? Intervention plan? Spastic dysarthria 6 27 year old man s/p viral encephalitis resulting in severe spastic quadriplegia and spastic dysarthria. Speech limited to undifferentiated vowels. He is married with 3 preschool children and he and his wife own and manage and flower distribution business Predicted impairments? Assessment strategies? Functional goals? Treatment targets? Intervention plan? Hypokinetic Dysarthria Let’s get Mikey! 40ish male with early onset Parkinsons disease. Symptoms are primarily in limbs but speech deficits are noticed in “off” cycles of meds. Professional actor by training but now focuses on public speaking events Predicted impairments? Assessment strategies? Functional goals? Treatment targets? Intervention plan? Ataxic Dysarthria 49 year old female s/p cerebellar stroke leaving her with severe ataxic dysarthria. She has 3 teenage sons. Prior to her stroke she was a community leader, serving on the school board, teaching Sunday School, and directing the local scholarship pageant Predicted impairments? Assessment strategies? Functional goals? Treatment targets? Intervention plan? 7