Healthcare provision in a district hospital in rural Ethiopia: an
advertisement

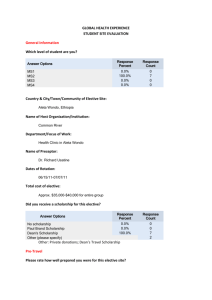
Healthcare provision in a district hospital in rural Ethiopia: an elective at Gimbie Adventist Hospital. Introduction My decision to undertake my elective in rural Ethiopia was not one taken lightly. It all started with a poster displayed in the medical school advertising Gimbie Adventist Hospital in the town of Gimbie. This was situated in the West Wollega region of Ethiopia, approximately 500km west of Addis Ababa. I had always felt that I would like to do my elective in Africa, and the poster certainly seemed to advertise everything that I had wanted – an experience of third world medicine. As soon as I saw the advertisement I knew that this was the place I had to go to. I started planning straight away, and after some discussions with the year 5 leader at the medical school, eventually the green light was given for me to go ahead with my chosen elective. I decided to raise money for the hospital I would be attending. Myself and a colleague therefore organised a Charity Fashion show, and we raised £450 each for our chosen causes. My major concern regarding my elective was the ability to finance it. Luckily, I had applied for the Yette and Boris Glass Foundation award and received a sum of £1000 which helped considerably. Had it not been for this, I might not have been able to fund this elective. With the help of the award, I was able to start organising my elective. This turned out to be relatively straightforward. I understood that I would be in very rural area, and that I would not be getting the opportunity to travel much. The hospital provided accommodation for me as part of their fee, so all I had to worry about were booking flights, organising vaccinations and anti-malarial medication, and securing a visa. Upon returning from my elective, I have to firstly state that this was the hardest thing I have ever done. About 3 weeks before I left I was starting to have moments of panic, and dreaming of such horrors as being kidnapped and held at knife point. Looking back now it seems silly, as I never once felt threatened or unsafe (except perhaps at the hands of some of the taxi drivers). The following report is an account of my elective in Ethiopia, detailing my experiences generally in the hospital and surrounding area, as well as some brief case reviews. The basic healthcare system at Gimbie Adventist Hospital is also detailed. Finally, I have made some reflection on my experiences in Ethiopia. Learning objectives My learning objectives which were decided by myself and the hospital administrator via email prior to the start of my elective were as follows: Aim: To gain experience in the management of patients in a rural healthcare setting in Ethiopia Objectives: 1. To participate in ward rounds for medical, surgical, obstetric, paediatric and infectious disease patients at Gimbie Hospital on a daily basis 2. To attend the outpatient department at Gimbie Hospital on a regular basis and, under the supervision of a physician, to assess and treat patients presenting with a variety of diseases, including infectious diseases that are uncommon in the UK 3. To attend TB and HIV outpatient clinics on a regular basis 4. To visit outreach sites for the assessment and treatment of patients. This includes joining a medical team to visit peripheral clinics affiliated with Gimbie Hospital, and joining with a community health worker to participate in village immunisation and health education outreach sessions. As can be seen from the above list, my learning objectives were very generalised, and allowed me to focus in on the things that I found most helpful and interesting. Unfortunately, due to staffing shortages, there were no outreach clinics organised during my stay. Healthcare in Ethiopia Ethiopia has a mixture of government and non government run hospitals. Gimbie Adventist Hospital is run by the Adventist Church, and so is a private hospital as such. I had expected that it would be largely run as a charitable organisation, but it is run more like a business. Patients are charged for every night they spent in hospital, and for every piece of equipment down to every last glove. After a few days, you became very aware of this and so strove to waste as little equipment as possible, only putting on two gloves if it was absolutely necessary. After every operation a form would be completed detailing exactly how much equipment had been used and the quantities of drug given, and the prices totalled to be added to the cost of the patient’s bill. This made elective surgery something for the wealthier, as often the estimated bill would be out with the realms of affordability for the local people. It was very difficult to see a patient turned away because they could not afford treatment, and on many occasions I witnessed women with grade 4 uterovaginal prolapses being sent away as the surgery would cost in the region of 1500 birr. (the average wage for an Ethiopian in Gimbie was less than 8 birr a day). There are two charity funds where patients receive free treatment: one is provided by the charity Maternity Worldwide, which provided a ‘safe birth fund’ for all expecting mothers. The other is for children admitted with malnutrition: they are treated using the ‘children’s fund’ which is provided by UNICEF. Another striking difference between the UK and Gimbie hospital is the lack of equipment and diagnostic tools. There are x-ray facilities available, but the films were of poor quality. There is one ultrasound machine, but again the images were poor and difficult to interpret. Commonly, certain blood tests could not be performed, as there was no reagent (for example you could not check haemoglobin levels, potassium levels, calcium levels etc). This meant that correct diagnosis and treatment depended heavily on the clinician’s examination skills. It was also very difficult to obtain a full history, as translators were used. Quite often the translator would not speak fluent English themselves, and so some of what the patient was reporting was lost in translation. One major problem which I found quite distressing was the inability of the hospital staff to protect a child if the parents were acting against a child’s best interests. One such example was a little boy of 7 who came in with heart failure. He was being treated with furosemide, and the physician was struggling to find a cause. The parents had no money, and so we managed to pay for his treatment using the Children’s fund. Even so, after a couple of days, the parents of the child were adamant they wanted to discharge him, despite our warnings that he would probably die without treatment. It later transpired that the reason for this was because they believed evil spirits were making him ill, and medicine could do nothing for him. I found this situation incredibly distressing. Whilst I can understand that everyone has a right to their own beliefs, to impart these onto a child like this to the detriment of his health was in my eyes unacceptable. Unfortunately there are no laws which prevent a family from acting against the child’s best interests here. The journey I began my journey at London Heathrow airport, in the process meeting the crew filming for the new BBC series of ‘Last Man Standing’. The fact that there were other young people travelling to a place such as Ethiopia made it a little less threatening. By the time I was due to get on the plane, I was more relieved at the prospect of sitting down and not lugging my heavy bags from train to train as had been the pattern of the day so far. I was travelling through the night, and the journey time was approximately 10 hours. After a sleepless flight, I landed in the capital city, Addis Ababa. I arrived in the airport at about 8.30am (2 hours ahead of the UK) and after a brief panic where I did not see any staff to greet me, I found Girmir, the hospital liaison worker. He drove me to the best hotel in Ethiopia to await Ruth, the hospital administrator. My first impressions of Addis Ababa were that it was busy, and nearly every building was covered with corrugated iron. It was a strange set-up, reasonable buildings interspersed between great expanses of slums, little sheds with iron roofs. Even stranger was the hotel, a huge grand building exuding wealth and grandeur. It would have looked in place in somewhere like London. I took a walk through the hotel grounds, and the view to be seen was the city slums. It seemed to me that such a grand building was a mockery of the surrounding poverty. The Sheraton Hotel, Addis Ababa The view of the city from the hotel We left Addis in the late afternoon, and travelled some 3 hours to Ambo. Here we stayed in one of the hotels overnight, with the intention of completing the rest of the journey the next day. As we pulled up outside the hotel we were instantly targets for beggars. One man had badly deformed arms and legs, and practically dragged himself to the kerb side to beg. I did not know what to do, I had no change on me, plus if I gave money to one man then how could I not give to all the people that had gathered to beg. I felt sick. Once I had deposited my belongings in my room, I went out to see if he was still about, but he had gone. Instead I gave my money to a blind woman. Only a few Birr was needed. The journey to the town of Gimbie was long, and took about ten hours in total. The scenery was fantastic, rolling hills with luscious green grasses and trees. The roads were not so fabulous, and I can only describe the drive like an off-road experience, the vehicle was constantly thrown off the road by the numerous massive pot holes. I found it quite exciting! The last few hours were on a dirt track, and windows had to be shut every time we passed a vehicle due to the great dust clouds created as it passed on its journey. We arrived at Gimbie at about 5pm. My first impressions were of a run down large town, with hundreds of houses extending down into the valley. Again the surrounding countryside was beautiful. I was taken to my living quarters, where I would be living alone for the majority of the time. A reasonable house, with a living room area, dining table, kitchen, three bedroom and a shower room. I was also informed I would have a maid paid for to cook, clean and shop for me. This helped a lot, as the ingredients were often different to what I was used to and the shops were merely little windows at the front of people’s houses, and you found what you were looking for merely by searching up and down the streets. my house within the hospital compound the view from the hospital compound Gimbie itself was an incredibly busy place. The town had a population of 40,000 despite not being particularly large. The roads were still dirt, although they were in the process of being converted to tarmac. The orange dust was unbelievable, and you had to cover your eyes and mouth every time a vehicle passed as the cloud that rose around you was huge. Cows, sheep and donkeys wandered everywhere. The Orthodox churches chose to deliver their daily sermons by speakerphone so that it could be clearly heard no matter where you were. People rode in the back of pick up trucks which was hardly safe, (in fact the local football team did so and the vehicle ended up in a massive pit in the road where the road layers were working – 14 people were injured and three died). the main road in Gimbie children liked to follow ‘faranjis’ (foreigners) Gimbie on market day locals selling their produce on market day The hospital Gimbie Adventist Hospital is a rural hospital containing 72 beds. There is a male/paediatric ward, a woman’s ward, two operating theatres, a labour ward, and intensive care room, and the emergency room. There is also a private corridor where patients could pay extra to stay throughout their admission. The rooms had a balcony and toilet, but were not private as such, but shared by 2-3 patients. There were various other outbuildings, including an out-patients (which saw up to 300 patients a day), the TB and HIV clinic, and the pathology laboratory. I started in the hospital the day after I arrived having braved a cold shower (it took me 2 weeks to figure out how to make the shower warm) and was shown around. The place was crowded, dirty and the smell was horrendous. The stench of urine and pus was prominent. There are 3 floors in total, the uppermost being reserved for offices. The middle floor contains the main entrance, then private rooms to the right, and the male/paediatric ward to the left. This led through to the ‘emergency room’. The biggest farce of all I felt was the ‘intensive care room’. This comprised of two dirty beds with split mattresses with various pieces of dusty and broken equipment lying about. (one of the machines actually went on fire when we tried to use it). male and paediatric ward operating theatre ‘intensive care’ laboratory and staff central out patients central out patients consulting room The remainder of the ward was filled with beds, no curtains, and often unchanged sheets. There is no play area for the children, no toys at all, they just lay in their own filth until the nurses decided to change the bedding. Downstairs is the operating theatre, the obstetrics and gynaecology out patients department, and the woman’s ward and delivery room. The main out patients department is in a separate building up some rather unsafe stairs. The woman’s ward is much the same as the male/paediatric ward, except the smell was a hundred times worse. The operating theatres are basic to say the least, there were dead flies on the window sills, and all equipment is old and temperamental. The first operation I assisted in proved to be quite a shock, all the sterile cloths and gowns were completely moth-eaten, the anaesthetist (unqualified) was questionable, and the majority of equipment seemed temperamental if not broken. It was common practice for the electricity to fail in the middle of an operation, and if it was getting dark then quite often a torch was held over the open body cavity so the surgeon could get some light. There was a hospital generator, so when the town was out of electricity for days on end, the hospital still had electricity. (unfortunately my house was powered by the town supply, so I spent many a night by candlelight.) Ward rounds were essentially in English, so most of what was going on could be understood. The pathologies which were seen were unbelievable at times; within my first week I had seen an acute case of rheumatic fever (accompanied by Sydenham’s chorea), countless cases of HIV, TB and malaria, severely malnourished children, severe vitamin D deficiency (with rickets), parasitic infections leading to acute bowel obstruction, leprosy, typhoid fever…the list is endless. My first two weeks were spent mainly concentrating on medical and surgical cases, and I was in at all hours. Typically ward round started between 7.30 and 8.30, and lasted until 11am. After this I either went to theatre with Dr Kim (he did all surgery cases with the exception of obstetrics and gynaecology) or went to outpatients with one of the physicians. Quite often I ended up back in hospital in the evenings, as it was difficult to walk through (as you did to get outside the grounds) without popping to see what was going on. The time I spent with the obstetrician and gynaecologists proved to be very rewarding. There was one permanent doctor, and throughout my stay there were two doctors who had come from the UK and Denmark as visitors through the Maternity Worldwide organisation. I witnessed many major obstetric complications. There were numerous cases of uterine rupture, which luckily ended in each case with the survival of the mother at least. I even succeeded in witnessing a case of uterine inversion due to poor management of the 3rd stage! The major reason for complications such as these was that the women were poorly educated and often came to the hospital after being in labour for perhaps 12-14 hours. By the time they made it to hospital, it was often the case that nothing could be done for their unborn child. I saw two cases of hand prolapse too, both of which ended up with horrendous wound infections after caesarean section. The process of wound cleaning was somewhat disturbing, and the doctor would just squeeze all the pus and fluid out of the gaping wound in the abdomen in the middle of the dirty ward. There was no privacy, and no anaesthesia. The women went through this ritual 3 times a day, and the sound of them screaming used to make me feel nauseated. One thing that really disturbed me was the lack of compassion for the dead babies. Having never seen a dead child before, I expected to find the whole situation really upsetting. The lack of emotional response from the parents and staff however completely normalised the whole situation. The child would be delivered, dumped on a plastic sheet and wrapped up and taken away. The woman would then end up straight back on the women’s ward (there was no recovery room) amongst those who had been fortunate enough to have a live birth. Throughout my time at the hospital I encountered many interesting cases. I have included brief descriptions of 2 cases: one obstetric and one surgical case. Obstetric case I had been very much looking forward to being involved with normal deliveries, and had spent time during my project option optimising my clinical skills so that I would be able to help in this area. I had even gone so far as to attend a perineal trauma repair course so that I would be able to suture uncomplicated perineal tears. My first midwife-led delivery was my last. I had turned up at midnight ( I had been working on my clinical audit) to be told a woman was delivering. It transpired that she was a primiparous women, had been there since 4pm and had not been assessed since then, despite being 8cm dilated. I examined her, and tried to conduct the delivery. The midwife did not seem to care at all about his patients, and often women just lay there with no analgesia or help in their delivery. Eventually he decided to deliver the baby with ventouse. Usually, only a few attempts at this are acceptable. He continued to try and use a ventouse for over an hour. Eventually the child was born, and was very hypotonic, blue, and breathing irregularly. Again, no one seemed to care, and I was left to try and resuscitate the newborn as best I could. I asked for a laryngoscope but I was told that they were locked up and could not be obtained (I later discovered that in fact the midwife was just too lazy to get one), and clean towels (again hard to come by). It really scared me the lack of care exhibited by the staff – to them it was just another neonate who was unwell at delivery, and they cared little about the outcome. Eventually the baby’s condition improved, but the degree of hypoxic brain injury obtained at delivery remains to be seen. Surgical case Whilst in the Emergency room, a small 7 year old girl was brought in by her concerned father. She appeared very lethargic and unwell, and was crying in pain. She presented with a 2 day history of right iliac fossa pain. She had no history of nausea or vomiting, but had been feverish. On examination she was tachycardic, tachypnoic with a mild pyrexia. Abdominal examination revealed tenderness in the right iliac fossa with some mild involuntary guarding but no rebound. It was thought that she might be suffering from acute appendicitis, and it was decided to manage conservatively and observe her for the time being. The next day, she became worse, and showed signs of bowel obstruction. An emergency laparotomy was organised. She was found to have an infestation of Ascaris worms in her intestines. A small incision was made and a total of 18 worms were removed. After passing a further 8 worms over the next few days, she made a complete recovery and was discharged. Clinical Audit As part of my elective, I was offered the opportunity to undertake a clinical audit of my choice. I decided to look at the management of Severe Acute Malnutrition (SAM) within the hospital over the preceding 9 months. This was compared to the guidelines set out by UNICEF. In this study I found a total of 56 patients who were admitted with SAM. Of these, I could only locate notes for 46 children. Only 40 were true cases of SAM. 29 were cases of kwashikor, and 11 were cases of marasmus. Overall, I found that the patient management in the majority of fields was very poor, with particular reference to the accurate and complete recording of information, something which is essential in monitoring the progress of the patient. This information was presented to the hospital administrator, and has highlighted those areas of clinical practice which are falling short of the guidelines. It is my hope that this audit will change current practices and that the treatment of children with SAM will improve over the coming months. child with kwashikor child with marasmus During my time at the hospital I also spent time in the community. I did this with either the External Immunisation Programme (EPI) nurse, or three catholic nuns originally from Ecuador. The EPI clinics were run two days a week, moving between the various different local villages. They provided a free immunisation programme for all babies in the area, including BCG, polio and the DTP vaccinations. We would sit under a tree on a log and give injections to the babies that were brought to us according to the immunisation card the parents brought along. We would get to the villages mainly by walking, usually about an hour in each direction. The three nuns from Ecuador were amazing women. They had been living in Gimbie for a total of 8 years, and could speak fluent Oromia (the local language). They ran a Catholic mission in the town and were often the first point of contact if someone needed help. With them I went to see villagers, give medical advice and injections, and also taught a women’s group on ‘women’s health. women’s group I really enjoyed my time with the nuns, as it gave me an opportunity to see how people lived. The majority of village houses were basically mud huts, there was no electricity or water, and no beds to speak of. typical village house The local people were all so friendly and welcoming, and quite often we would be given sugar cane to eat. The first time I was handed this I did not quite know what to do, and I found it quite strange to be tearing off pieces with my teeth, chewing them and then spitting it onto the floor. I soon got used to it, however, and realised the honour of being given sugar cane – it was the equivalent of offering expensive chocolates to a guest. I learned quickly that when I went out with the nuns, I should expect anything. A trip to church on a Sunday morning translated as an hours walk through a forest with a path riddled with ants and numerous monkeys running past you. We had attended a coffee ceremony afterwards, I was so hungry and thirsty and therefore was somewhat pleased to see they were offering round bread and coffee. It turned out the bread was full of chillies, which I felt I could cope with, until I tasted the coffee. The villagers could not afford sugar, so instead they added salt to the coffee. Not a custom I will miss. The nuns were three amazing women who had dedicated their lives wholeheartedly to helping those who needed it most, and I felt being in their presence was very inspiring. I consider myself very fortunate to have met such caring, compassionate women. Sisters Mattie, Suzie and Joannie. Conclusion At the end of my time in Gimbie, I travelled back to the capital where I spent three days. I luckily had met someone who showed me around the place and took me to the market and bars. I had been looking forward to a shower when I reached the capital (the water pump had stopped working during my stay and I had had no running water for a month – water was carried in buckets to my house either by the garner or myself) only to find that the shower in my hotel room was broken! Upon reaching the UK, I was very sad to have left Gimbie behind. I had met some wonderful people, and had some truly amazing experiences. I had found my time there to be very difficult, and going alone had certainly been a major contributor to that. I saw a lot of interesting medical and surgical cases throughout my time which I am very grateful for. I also experienced first hand the way that some people have to live, and it makes me realise how lucky I am to have been brought up in the UK. I have realised how satisfying it must be to spend time working in a developing country, and I certainly hope in my lifetime I will spend a year or two working in a place like Gimbie. We as Westerners complain at the smallest inconvenience, make a fuss over a small cut on our finger, and are obsessed with our appearance, and spend money frivolously. I was not fully aware of how some people in this world live, and though they have so many hardships they are probably happier and friendlier than the majority of us here in the UK. I feel privileged to have spent time in a developing country, and I have realised just how lucky I really am to have received a proper education, to live with electricity and water, and to live in a country where healthcare is of a high standard and free. My learning objectives were met fully (with the exception of the outreach clinics) as I spent a great deal of time in the wards, in theatre, and going out into the community. I feel that I used my time effectively, and witnessed many interesting medical cases. Overall I think my elective was a good experience, though I have to say I would like to have had the opportunity to travel. The reason I did not was due partly to the fact I went alone and partly because I was in such a remote area. For these reasons I would not recommend a student to go to Gimbie Adventist Hospital unless they are fully aware of the level of isolation they may experience. I do however recommend going to Ethiopia, it is a fantastic country to visit, and the people are so friendly and helpful.