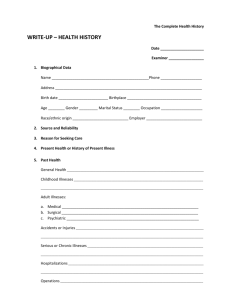
Jarvis Health History Form
advertisement

WRITE – UP HEALTH HISTORY Date__________________________ Examiner _____________________ I. BIOGRAPHICAL DATA Name ________________________________ Phone ____________________________________ Address _________________________________________________________________________ Birth date __________________________________Birthplace ____________________________ Age ________ Gender ________ Marital Status_________ Occupation _____________________ Race/Ethnic Origin ____________________ Employer ___________________________________ II. SOURCE AND RELIABILITY III. REASON FOR SEEKING CARE (CC): Main reason for consulting health professional. State briefly in client’s own words (when possible). State onset and duration briefly. IV. PRESENT HEALTH OF HISTORY OF PRESENT ILLNESS: Needs to be well organized and sequentially developed. Clear, chronological account of problem for which client is seeking care. Should include: O. Onset: Exactly when did it start? When did you first notice it? P. Provocative or Palliative: What brings it on? What where you doing when you first noticed it? What makes it better? Worse? Q. Quality or Quantity: How does it look, feel, or sound? How intense/severe is it? R. Region or Radiation: Where is it? Does it spread anywhere? S. Severity Scale: How bad is it (on a scale of 1 to 10)? Is it getting better, worse, staying the same? T. Timing: Is it constant or does it come or go? Duration- How long did it last? Frequency- How often does it occur? U. Understanding patients perception of the problem What do you think it means? ADD. Associated Factors, Significant negatives: Is this primary symptom associated with any 1 CK/REV. PAK/Feb. 2014 others? Review ROS r/t this symptom, Medication regimen (including alcohol and tobacco use). V. PAST HEALTH Describe General Health ___________________________________________________________ Childhood Illnesses ________________________________________________________________ Accidents or Injuries (include age) ___________________________________________________ Serious or Chronic Illnesses (include age) _____________________________________________ Hospitalizations (what for? Location) ________________________________________________ Operations (name, procedure, age) ___________________________________________________ Obstetric Hx: Gravida (# Pregnancies) _____Term (# Term Pregnancies) ______Preterm (# preterm pregnancies)___________ Ab/Incomplete (#Abortions/Miscarriages) ________Children Living __________________ Course of Pregnancy ______________________________________________________________ (date of delivery, length of pregnancy, length of labor, baby's weight and sex, vaginal delivery/cesarean section, complications, baby's condition). Immunizations __________________________________________________________________ Last Examination date ___________________________________________________________ Allergies ____________________________ Reaction __________________________________ Current Medications: (List all prescribed and non-prescribed drugs including Name, Dose, Route, Frequency) ___________________________________________________________________________________ ___________________________________________________________________________________ ___________________________________________________________________________________ ___________________________________________________________________________________ VI. FAMILY HISTORY – Specific Heart Disease___________________________ Allergies __________________________ High Blood Pressure _____________________ Asthma ___________________________ Stroke _________________________________ Obesity ___________________________ Diabetes ________________________________ Alcoholism or drug addiction __________ 2 CK/REV. PAK/Feb. 2014 Blood Disorders _________________________ Mental Illness ________________________ Breast/Ovarian/Colon Cancer ________________ Suicide ______________________________ Cancer (other) ____________________________ Seizure Disorder ______________________ Sickle Cell _______________________________ Kidney Disease _______________________ Arthritis _________________________________ Tuberculosis __________________________ Construct Genogram Below VII. REVIEW OF SYSTEMS (Document both past health problems that have been resolved and current problems including date of onset.) :Describe positive (P/S or P/C or P/R) items. List all pertinent negative items, e.g., P/D any unusually frequent or severe headache, any head injury, syncope, or vertigo under HEAD. 1. General Overall Health State: Present weight (gain or loss, period of time, by diet or other factors), fatigue, weakness or malaise, fever, chills, sweats or night sweats. 2. Skin: History of skin disease (eczema, psoriasis, hives), pigment or color change, change in mole, excessive dryness or moisture, pruritus, excessive bruising, rash, or lesion. 3. Hair: Recent loss, change in texture. 4. Nails: Change in shape, color, or brittleness. Health Promotion: Amount of sun exposure, method of self-care for skin and hair. 5. Head: Any unusually frequent or severe headache, any head injury, dizziness (syncope), or vertigo. 6. Eyes: Difficulty with vision (decreased acuity, blurring, blind spots) eye pain, diplopia (double vision), redness or swelling, watering or discharge, glaucoma or cataracts. Health Promotion: Wears glasses or contacts; last vision check or glaucoma test; how coping 3 CK/REV. PAK/Feb. 2014 with loss of vision if any. 7. Ears: Earaches, infections, discharge and its characteristics, tinnitus, or vertigo. Health Promotion: Hearing loss, hearing aid use, how loss affects daily life, any exposure to environmental noise, method of cleaning ears. 8. Nose and Sinuses: Discharge and its characteristics, any unusually frequent or severe colds, sinus pain, nasal obstruction, nosebleeds, allergies or hay fever, or change in sense of smell. 9. Mouth and Throat: Mouth pain, frequent sore throat, bleeding gums, toothache, lesion in mouth or tongue, dysphagia, hoarseness or voice change, tonsillectomy, altered taste. Health Promotion: Pattern of daily dental care, use of prostheses, (dentures, bridge), and last dental checkups. 10. Neck: Pain, limitation of motion, lumps or swelling, enlarged or tender nodes, goiter. 11. Breast: Pain, lump, nipple discharge, rash, history of breast disease, any surgery on breasts. Axilla: Tenderness, lump or swelling, rash. Health Promotion: Performs breast self-examination, including its frequency and method used, last mammogram and results. 12. Respiratory System: History of lung disease (asthma, emphysema, bronchitis, pneumonia, tuberculosis), chest pain with breathing, wheezing or noisy breathing, shortness of breath, how much activity produces shortness of breath, cough, sputum (color, amount), hemoptysis, toxin or pollution exposure. Health Promotion: Last chest x-ray examination. 13. Cardiovascular System: Precordial or retrosternal pain, palpitation, cyanosis, dyspnea on exertion (specify amount of exertion it takes to produce dyspnea), orthopnea, paroxysmal nocturnal dyspnea, nocturia, edema, history of heart murmur, hypertension, coronary artery disease, anemia. Health Promotion: Date of last ECG or other heart tests and results. 14. Peripheral Vascular System: Coldness, numbness and tingling, swelling of legs (time of day, activity), discoloration in hands or feet (bluish red, pallor, mottling, associated with position, especially around feet and ankles), varicose veins or complications, intermittent claudication, thrombophlebitis ulcers. Health Promotion: If work involves long-term sitting or standing, avoid crossing legs at the knees, wear support hose. 15. Gastrointestinal System: Appetite, food intolerance, dysphagia, heartburn, indigestion, pain, (associated with eating), other abdominal pain, pyrosis (esophageal and stomach burning sensation with sour eructation), nausea and vomiting (character), vomiting blood, history of abdominal disease (ulcer, liver or gallbladder, jaundice, appendicitis, colitis), flatulence, frequency of bowel movement, any 4 CK/REV. PAK/Feb. 2014 recent change, stool characteristics, constipation or diarrhea, black stools, rectal bleeding, rectal conditions, hemorrhoids, fistula). Health Promotion: Use of antacids or laxatives. 16. Urinary System: Frequency, urgency, nocturia (the number of times the person awakens at night to urinate, recent change), dysuria, polyuria or oliguria, hesitancy or straining, narrowed stream, urine color (cloudy or presence of hematuria), incontinence, history of urinary disease (kidney disease, kidney stones, urinary tract infections, prostrate); pain in flank, groin, suprapubic region, or low back. Health Promotion: Measures to avoid or treat urinary tract infections; Kegel exercises after childbirth. 17. Male Genital System: Penis or testicular pain, sores or lesions, penile discharge, lumps, hernia. Health Promotion: Perform testicular self-examination? How frequently? 18. Female Genital System: Menstrual history (age at menarche, last menstrual period, cycle and duration, any amenorrhea or menorrhagia, premenstrual pain or dysmenorrhea, inter-menstrual spotting), vaginal itching, discharge and its characteristics, age at menopause, menopausal signs or symptoms, post- menopausal bleeding. Health Promotion: Last gynecologic checkup, last Pap smear and results. 19. Sexual Health: Presently in a relationship involving intercourse? Are aspects of sex satisfactory to you and partner, any dyspareunia (for female), any changes in erection or ejaculation (for male), use of contraceptives, is contraceptive method satisfactory? Use of condoms, how frequently? Aware of any contact with partner who has sexually transmitted infection (gonorrhea, herpes, chlamydia, venereal warts, HIV/AIDS, syphilis)? Health Promotion: Prevention of STI’s? STI checkup as needed? 20. Musculoskeletal System: History of arthritis or gout. In the joints: pain, stiffness, swelling (location, migratory nature), deformity, limitation of motion, noise with joint motion. In the muscles: any pain, cramps, weakness, gait problems or problems with coordinated activities. In the back: any pain (location and radiation to extremities), stiffness, limitation of motion, or history of back pain or disk disease. Health Promotion: How much walking per day? What is the effect of limited range of motion on daily activities, such as on grooming, feeding, toileting, dressing? Any mobility aids used? 21. Neurologic System: History of seizure disorder, stroke, fainting, blackouts. In motor function: weakness, tic or tremor, paralysis, coordination problems. In sensory function: numbness and tingling (paresthesia). In cognitive function: memory disorder (recent or distant, disorientation). In mental status: any nervousness, mood change, depression, or any history of mental health dysfunction or hallucinations. 22. Hematologic System: Bleeding tendency of skin or mucous membranes, excessive bruising, lymph 5 CK/REV. PAK/Feb. 2014 node swelling, exposure to toxic agents or radiation, blood transfusion and reactions. 23. Endocrine System: History of diabetes or diabetic symptoms (polyuria, polydipsia, polyphagia), history of thyroid disease, intolerance to heat or cold, change in skin pigmentation or texture, excessive sweating, relationship between appetite and weight, abnormal hair distribution, nervousness, tremors, need for hormone therapy. FUNCTIONAL ASSESSMENT (Including Activities of Daily Living) Self-Esteem, Self-Concept: Education: (last grade completed, other significant training) ___________ ___________________________________________________________________________________ Financial Status: (income adequate for lifestyle and/or health concerns) ___________________________________________________________________________________ Value-Belief System (religious practices and perception of personal strengths) ___________________________________________________________________________________ ___________________________________________________________________________________ Self-Care Behaviors:__________________________________________________________________ Activity/Exercise: Daily profile, usual pattern of a typical day ___________________________________________________________________________________ ___________________________________________________________________________________ Independent or needs assistance with ADL’s, feeding, bathing, hygiene, dressing, toileting, bed-to-chair transfer, walking, standing, climbing stairs ___________________________________________________________________________________ Leisure Activities ____________________________________________________________________ Exercise Pattern: (type, amount per day or week, method of warm-up session, method of monitoring body’s response to exercise ___________________________________________________________________________________ Other Self Care Behaviors:_____________________________________________________________ 6 CK/REV. PAK/Feb. 2014 Sleep/Rest: Sleep patterns, daytime naps, any sleep aids used: ___________________________________________________________________________________ ___________________________________________________________________________________ Other self-care behaviors:______________________________________________________________ Nutrition/Elimination: Record 24 hour diet recall ___________________________________________________________________________________ ___________________________________________________________________________________ Is this menu pattern typical of most days? _________________________________________________ Who buys food? _____________________________Who prepares food?________________________ Finances adequate for food? ___________________________________________________________ Who is present at mealtimes? __________________________________________________________ Other self-care behaviors _____________________________________________________________ Interpersonal Relationships/Resources: Describe own role in family__________________________ How is getting along with family, friends, co-workers, classmates ____________________________ Get support with a problem from _______________________________________________________ How much daily time spent alone? ______________________________________________________ Is this pleasurable or isolating? _________________________________________________________ Other self-care behaviors _____________________________________________________________ Coping and Stress Management: Describe stresses in life now_______________________________ __________________________________________________________________________________ Change in past year__________________________________________________________________ Methods used to relieve stress __________________________________________________________ Are these methods helpful? ____________________________________________________________ 7 CK/REV. PAK/Feb. 2014 Personal Habits: Daily intake caffeine (coffee, tea, colas) ___________________________________ Smoke cigarettes? _____________________________Number packs per day____________________ Daily use for how many years ____________________Age started ____________________________ Ever tried to quit? _____________________________ How did it go? _________________________ Drink alcohol? _______________________________ Date last alcohol use _____________________ Amount of alcohol during that episode____________________________________________________ Out of last 30 days, on how many days had alcohol? ________________________________________ Ever had a drinking problem? __________________________________________________________ Any use of street drugs? _______________________________________________________________ Marijuana? _____________________________________Cocaine? ____________________________ Crack cocaine? __________________________________Amphetamines? ______________________ Barbiturates? __________________________________ LSD? _______________________________ Heroin? _______________________________________ Other?_______________________________ Ever been in treatment for drugs or alcohol? _______________________________________________ Environment/Hazards: Housing and neighborhood (type of structure, live alone, know neighbors) ___ ___________________________________________________________________________________ Safety of area _______________________________________________________________________ Adequate heat and utilities _____________________________________________________________ Access to transportation _______________________________________________________________ Involvement in community services _____________________________________________________ Hazards at workplace or home__________________________________________________________| Use of seatbelts______________________________________________________________________ Travel to or residence in other countries __________________________________________________ Military service in other countries ______________________________________________________ 8 CK/REV. PAK/Feb. 2014 Self-care behaviors___________________________________________________________________ Intimate Partner Violence: How are things at home? Do you feel safe? ________________________ ___________________________________________________________________________________ Ever been emotionally or physically abused by your partner or someone important to you? __________ ___________________________________________________________________________________ Ever been hit, slapped, kicked, pushed, or shoved or otherwise physically hurt by your partner or expartner? ____________________________________________________________________________ Partner ever force you into having sex? ___________________________________________________ Are you afraid of your partner or ex-partner? ______________________________________________ Occupational Health: Please describe your job? ___________________________________________ Work with any health hazards (e.g. asbestos, inhalants, chemicals, repetitive motion)? ___________________________________________________________________________________ Any equipment at work designed to reduce your exposure? ___________________________________ Are work programs designed to monitor your exposure? _____________________________________ Any health problems that you think are related to your job? ___________________________________ What do you like or dislike about your job? _______________________________________________ Perception of Own Health: How do you define health? _____________________________________ View of own health now______________________________________________________________ What are your concerns? ______________________________________________________________ What do you expect will happen to your health in future? ____________________________________ ___________________________________________________________________________________ Your health goals?___________________________________________________________________ Your expectations of nurses, physicians? _______________________________________________________________________________ 9 CK/REV. PAK/Feb. 2014