Investigation of neonate with fever Approximately 8.5% of infants
advertisement

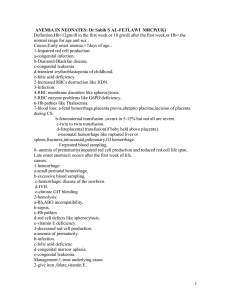
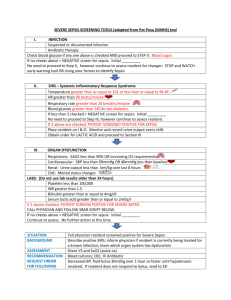
Investigation of neonate with fever Approximately 8.5% of infants who are younger than 90 days and have a temperature of ≥38˚C will have a serious bacterial infection(SBI). Neonates with fever who are aged 38 days or younger may have few clues on history and physical examination to guide therapy. Therefore, a high index of suspicion is necessary in order to detect the febrile neonate with a serious bacterial infection. Definitive identification of a serious bacterial infection requires laboratory investigation; a full sepsis evaluation; and a positive result in blood culture, cerebrospinal fluid (CSF), and/or urine. Bacterial meningitis is more common in the first month of life than at any other time. An estimated 5-10% of neonates with early onset group B streptococcal sepsis have concurrent meningitis. Typically, infections that occur in the first week of life are secondary to vertical transmission, and those infections occurring after the first week are usually community acquired or hospital acquired. Assessment History Prenatal history, maternal h/o STIs, GBS status and prophylaxis, mode of delivery, PROM and h/o maternal fever Risk factors for neonatal sepsis: o BW<2500gm o PROM o Septic or traumatic delivery o Fetal hypoxia o Maternal peripartum infection o Galactosemia o Gestational age at delivery Course since delivery Use of peripartum and antepartum antibiotics Feeding details – type, quantity, frequency and vomiting Sleep history Family and sibling h/o illness, infections H/o past deliveries and infections Symptoms s/o NS o Apnea o Bradycardia o Floppiness o Temperature instability – fever in 15% initially o Respiratory distress o Neurologic symptoms – seziures, irritability o Jaundice within 24hrs without incompatibility history o Vomiting, diarrhea and abdominal distension Examination Complete physical examination including vital signs Growth parameters and percentiles General appearance – activity level, color, tone, irritability Signs of localized infections – thorough examination of skin, mucous membrane, ear and extremities Examine umbilical stump Jaundice –prolonged Signs of serious infection o Irritability o Inconsolability o Poor perfusion o Poor tone o Decreased activity and o Lethargy A significant proportion of infants <28days may present with low risk features on history and examination in presence of SBI, and therefore full investigations are warranted Specific signs of an infected organ may pinpoint the primary site or a metastatic site. Most neonates with early-onset GBS (and many with L. monocytogenes) infection present with respiratory distress that is difficult to distinguish from hyaline membrane disease. Periumbilical erythema, discharge, or bleeding without a hemorrhagic diathesis suggests omphalitis (infection prevents obliteration of the umbilical vessels). Coma, seizures, opisthotonos, or a bulging fontanelle suggests meningitis, encephalitis, or brain abscess. Decreased spontaneous movement of an extremity and swelling, warmth, erythema, or tenderness over a joint indicates osteomyelitis or pyogenic arthritis. Unexplained abdominal distention may indicate peritonitis or necrotizing enterocolitis (particularly when accompanied by bloody diarrhea and fecal leukocytes). Cutaneous vesicles, mouth ulcers, and hepatosplenomegaly (particularly with disseminated intravascular coagulation [DIC]) can identify disseminated herpes simplex. Etiology infections that occur in the first week of life are secondary to vertical transmission Infections occurring after the first week are usually community acquired or hospital acquired. Most common o Group B Beta-hemolytic Streptococcus (Group B Strep) o Escherichia coli K1 (ECK1) o Listeria monocytogenes Other pathogens o Haemophilus Influenzae o Coagulase-negative staphylococci (Nosocomial) Investigations – There is NO specific diagnostic marker for sepsis in neonates, only determinants. A full sepsis evaluation is recommended in all febrile neonates. This includes a CBC count, blood culture, urinalysis, urine culture, and CSF analysis and culture. FBC o White cell count <5000/mm3 or >25000/mm3, may be normal in 50% of culture proven cases o Absolute neutrophil count(ANC) <1000/mm3 – only in 2/3rd of culture positive cases o Bands to total neutrophil count ratio > 0.2 (sensitivity of 60-90%) o Immature to mature neutrophil count ratio >0.2 (sensitivity of 60-90%) o Thrombocytopenia <100,000 may occur in 10-60% of cases All changes can be seen with physiological stressors and findings should be used in combination. Blood culture – positive in 5-10% of cases o Anerobic cultures more important in neonates with abscess, bowel involvement, massive hemolysis and refractory pneumonia o Generally reveal the organism of infection within 36-48hrs o Single site cultures equally effective in isolating bacteria in neonates o Blood cultures may be negative in up to 38% of culture proven meningitis Gram stain – early identification if gram-negative or gram-positive status of organism Coagulation studies o Abnormal PT, PTT, fibrinogen and d-dimer can occur in neonates with severe sepsis but not sensitive to diagnose sepsis Lumbar puncture - An estimated 5-10% of neonates with early onset group B streptococcal sepsis have concurrent meningitis. Even culture proven meningitis may not show white cell changes in CSF. o Elevated protein level (normal in 50% meningitis cases) o Decreased CSF glucose (normal in 50% of meningitis cases) o Positive culture results o CSF WBC count (normal in 29% of meningitis cases) o Follow up LP needed in 24-36hrs after antibiotic therapy to confirm sterility C-reactive protein(CRP) o Are elevated at some point in 50-90% of infants with SBI o Not recommended as a sole indicator of neonatal sepsis o May be used as serial study once noted to be elevated for determining response to antibiotics IgM concentration in serum o Helpful in determining presence of intrauterine infection. Urine culture o Low yield in early-onset sepsis o Suprapubic bladder puncture or bladder catheterization recommended in all cases of late onset sepsis o Painful procedure with low yield o >10WCC/mm3, >104 organism/ml in urine from catheterization and any organism in suprapubic collection Novel infection markers o CD11b, CD64, IL-6, IL-8 – may be helpful as adjunctive markers o Serial measurements and use of combinations of tests may improve their value o Procalcitonin may be elevated in patients with sepsis but further research is needed to establish clear role Chest X-ray – o Segmental or lobar infiltrate o More commonly diffuse, fine, reticulogranular pattern similar to RDS o Non-specific as to cause or effect of symptoms CT scanning and MRI o Needed in course of complex neonatal meningitis o To document hydrocephalus, infarctions or abscesses Cranial ultrasound in neonates o Ventriculitis, abnormal parenchymal echogenicities, extracellular fluid and chronic changes in cases of meningitis o Variable sensitivity not a diagnostic tool HSV PCR o Reserved for infants with CNS abnormalities, vesicles o Vesicles not present in 1/3rd of cases Emerging technology o PCR technology for detection of specific pathogens o No role for diagnosis but may be useful in future to target antibiotic therapy