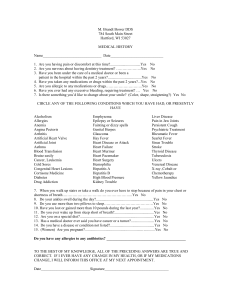
EASTPOINTE FAMILY PHYSICIANS
advertisement
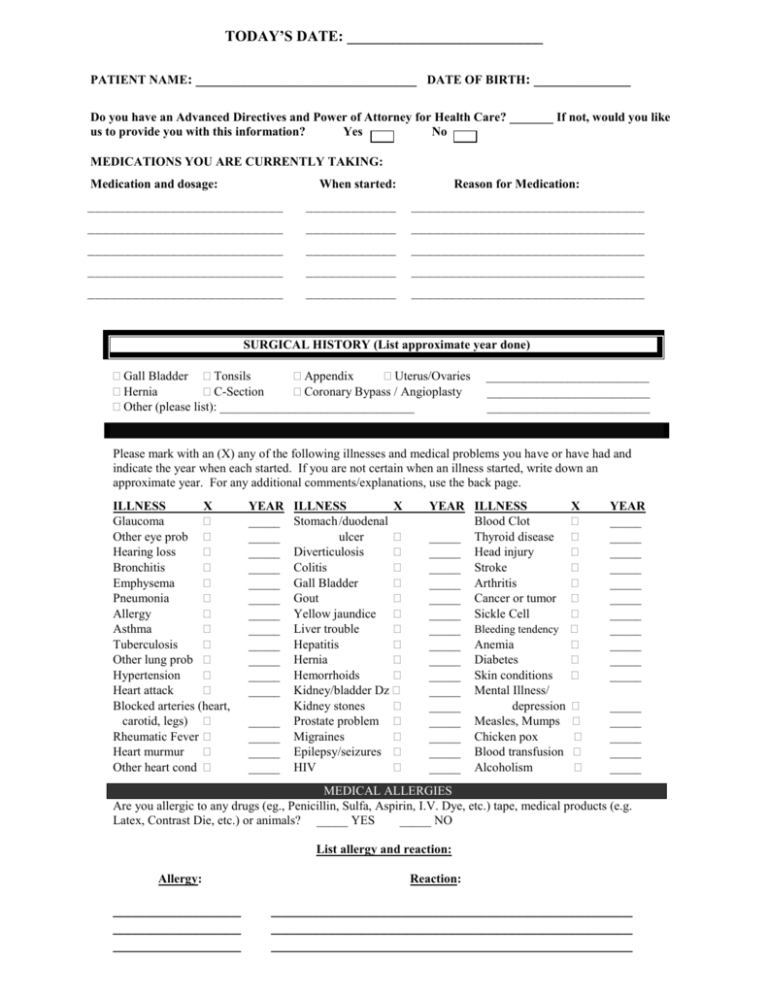
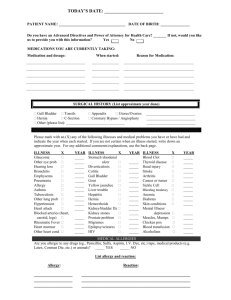
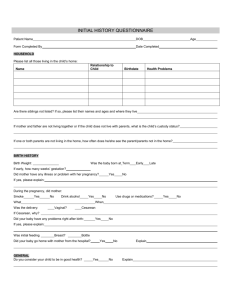
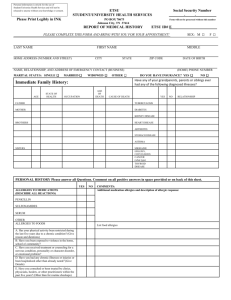
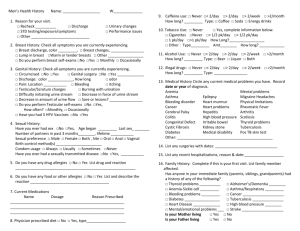
TODAY’S DATE: __________________________ PATIENT NAME: ________________________________ DATE OF BIRTH: ______________ Do you have an Advanced Directives and Power of Attorney for Health Care? _______ If not, would you like us to provide you with this information? Yes No MEDICATIONS YOU ARE CURRENTLY TAKING: Medication and dosage: When started: Reason for Medication: __________________________ ____________ _______________________________ __________________________ ____________ _______________________________ __________________________ ____________ _______________________________ __________________________ ____________ _______________________________ __________________________ ____________ _______________________________ SURGICAL HISTORY (List approximate year done) Gall Bladder Tonsils Appendix Uterus/Ovaries Hernia C-Section Coronary Bypass / Angioplasty Other (please list): _______________________________ __________________________ __________________________ __________________________ Please mark with an (X) any of the following illnesses and medical problems you have or have had and indicate the year when each started. If you are not certain when an illness started, write down an approximate year. For any additional comments/explanations, use the back page. ILLNESS X Glaucoma Other eye prob Hearing loss Bronchitis Emphysema Pneumonia Allergy Asthma Tuberculosis Other lung prob Hypertension Heart attack Blocked arteries (heart, carotid, legs) Rheumatic Fever Heart murmur Other heart cond YEAR _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ ILLNESS X Stomach /duodenal ulcer Diverticulosis Colitis Gall Bladder Gout Yellow jaundice Liver trouble Hepatitis Hernia Hemorrhoids Kidney/bladder Dz Kidney stones Prostate problem Migraines Epilepsy/seizures HIV YEAR ILLNESS Blood Clot _____ Thyroid disease _____ Head injury _____ Stroke _____ Arthritis _____ Cancer or tumor _____ Sickle Cell _____ Bleeding tendency _____ Anemia _____ Diabetes _____ Skin conditions _____ Mental Illness/ _____ depression _____ Measles, Mumps _____ Chicken pox _____ Blood transfusion _____ Alcoholism X YEAR _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ MEDICAL ALLERGIES Are you allergic to any drugs (eg., Penicillin, Sulfa, Aspirin, I.V. Dye, etc.) tape, medical products (e.g. Latex, Contrast Die, etc.) or animals? _____ YES _____ NO List allergy and reaction: Allergy: _________________ _________________ _________________ Reaction: ________________________________________________ ________________________________________________ ________________________________________________ Patient Name: ___________________________________ Date: ______________________ Place an "X" next to the test you have had done and list when and where: When done: Where test was performed: Colonoscopy EKG Chest X-ray Echocardiogram Stress Test Arterial Doppler Venous Doppler Carotid Doppler Other Habits Do you currently smoke? ____Yes ____No How many years?__________________ Do you chew tobacco? ____Yes If yes, how much per day?___________________ Are you a former smoker?___________________ ____No Consumption of Alcoholic Beverages? ____Yes ____No Amount: _________oz #______ of drinks per week / month / year Do you currently use drugs: ____Yes ____No Type:_________________________ Frequency:_____________________ Have you ever used drugs: ____Yes ____No Type:_________________________ Frequency:_____________________ Coffee / Tea? ____Regular ____Decafinated ____None Do you exercise regularly? ____Yes ____No Number of cups per day:____________________ How often:________________ Type of exercise:_____________________ Are there any health resks involved in your job, home environment, or activities? ____Yes ____No If yes, please explain:______________________________________________________________________________________________ Sexual History (The purpose of these questions is to determine your risk factors) Are you currently sexually active? _____ Yes _____ No Do you currently have more than 1 partner? _____ Yes _____ No Any history of sexually transmitted disease? _____ Yes _____ No Are you now or have ever been tested for: _____ HIV _____ Hepatitis C _______ I would rather discuss this with the doctor in person. Family Health History Have any family relatives (mother, father brother, sister, grandfather, grandmother, aunt, uncle, cousin, nephew, niece, son, daughter) suffered any of the following? Please list the people relative to their relationship to you: Condition Cancer Relationship to you Condition Nerve/Muscle diseases Obesity (overweight) Seizures (fits, epilepsy) Heart trouble Stroke Asthma or hayfever Allergies Diabetes (sugar) Ulcers Stomach or bowel problems Gout Kidney disease Arthritis Anemia (low blook) Bleeding problems Rheumatic fever Alcoholism Mental Illness Physical deformity Blind/deaf Congenitally Impaired (Mental Retardation): Other: Relationship to you Patient Name: _____________________________________ Date: ________________________ Place a mark in the box for each item that you have now or have had in the past and where applicable, please fill in additional information. GENERAL/ weakness chills change in weight or appetite CONSTITUTIONAL fatigue night sweats fevers change in sleeping habits SKIN itching rash change in color easy bruising new or changing moles or other growths on skin headache NERVOUS double vision dizziness numbness/tingling SYSTEM muscle weakness tremor/handshaking loss of coordination CARDIOVASC. chest pain trouble breathing at night easy fatigue SYSTEM palpitations (heart pounding) trouble climbing stairs RESPIRATORY SYSTEM blood clots/phlebitis ankle swelling wheezing frequent or chronic cough frequent bronchitis shortness of breath, with minimal exertion GASTROINTESTINAL stomach pain/abdominal pain indigestion/heart burn black, tarry stools URINARY urgency pain with urination previous infections blood in urine frequent urination loss of control of bladder EYES glasses/contacts eye pain EARS loss of/or decreased hearing excessive tearing blurring or spots NOSE/THROAT/ SINUSES taste or smell changes frequent sore throats JOINTS & BACK pain MUSCLES pain ENDOCRINE excessively hot always hungry HORMONE/ easy bruising difficulty swallowing vomiting/nausea diarrhea/constipation changes in bowel habits blood in stools loss of control of bowels difficult starting stream weak stream leaking urine last eye exam date: __________ double vision ringing in ears drainage hoarseness sinus problems neck swelling last dental exam: __________ swelling stiffness deformity weakness twitching cramping always thirsty excessively cold easy bleeding swollen glands LYMPH ALLERGIES/ hives hay fever drug allergies: ____________________________________ IMMUNE other allergies: _________________________________________________________ PSYCHOLOGICAL nervousness depression unable to sleep nightmares memory loss anorexia/bulimia mood swings/anxiety IMMUNIZATIONS Tetanus date: ___________ Influenza date: __________ Chicken Pox date: __________ German Measles date: __________ Pneumococcal date: __________ Hepatitis B Series date: ___________ MALES hernia pain in testicles sexual difficulties discharge from penis SIGNS, SYMPTOMS AND DISEASES NOT COVERED ABOVE (additional space on back) ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ PLEASE COMPLETE THE FOLLOWING QUESTIONS: MENSTRAL How often are your periods? Every ______days Age at onset of menses: ___________ How long do they last ______days First day of last menstrual period: _____________ Any menstrual problems? None Irregular Cramps Heavy Other: _____________ Any menopause symptoms? Irregular periods Hot flashes Vaginal dryness Insomnia If in menopause, age of onset: __________ Other:________ PREGNANCY How many times have you been pregnant? #Deliveries _____ #Miscarriages _____ #Abortions________ Any complications of pregnancy? None High blood pressure Diabetes Other _________ SEXUAL HISTORY Current method of contraception: ________________________ None Age at onset of sexual activity: ______________ Any problems with intercourse? None Pain Bleeding Other _________________ Any problems with vaginal: Burning Itching Discharge Abnormal odor OSTEOPORESIS Ever had a Bone Density Scan (DEXA) Yes No Date of last scan: ________________ Any family history of osteoporosis Yes No Do you ingest 1500 mg of Calcium per day? Yes No Not sure Do you ingest 800 IU of Vitamin D per day? Yes No Not sure Do you take any of the following? Hormone replacement: (name) ___________________________ Evista Fosamax or Actonel or Miacalcin Calcium Supplement Vitamin D Supplement CANCER SCREENING When was your last PAP Smear? _____________ Any abnormal PAP Smears in the past? ___________ Ever have gynecological procedure/surgery? Yes No What type Leep/Colposcopy/Cryotherapy Other:_____________ When was your last mammogram? ___________ Normal Abnormal Never had one Do you do self breast exam? Every month Occasionally Never Don’t know how Do you have any history of breast problems? None Fibrocystic Breast surgery Other Any family history of: Breast cancer Cervical cancer Uterine cancer Ovarian cancer ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ______ SIGNATURES Patient Signature: __________________________________________________ Date: ______________ D.O. /M.D./P.A. Signature: __________________________________________ Date: ______________