UCMC Hypothermia after Cardiac Arrest Protocol
advertisement
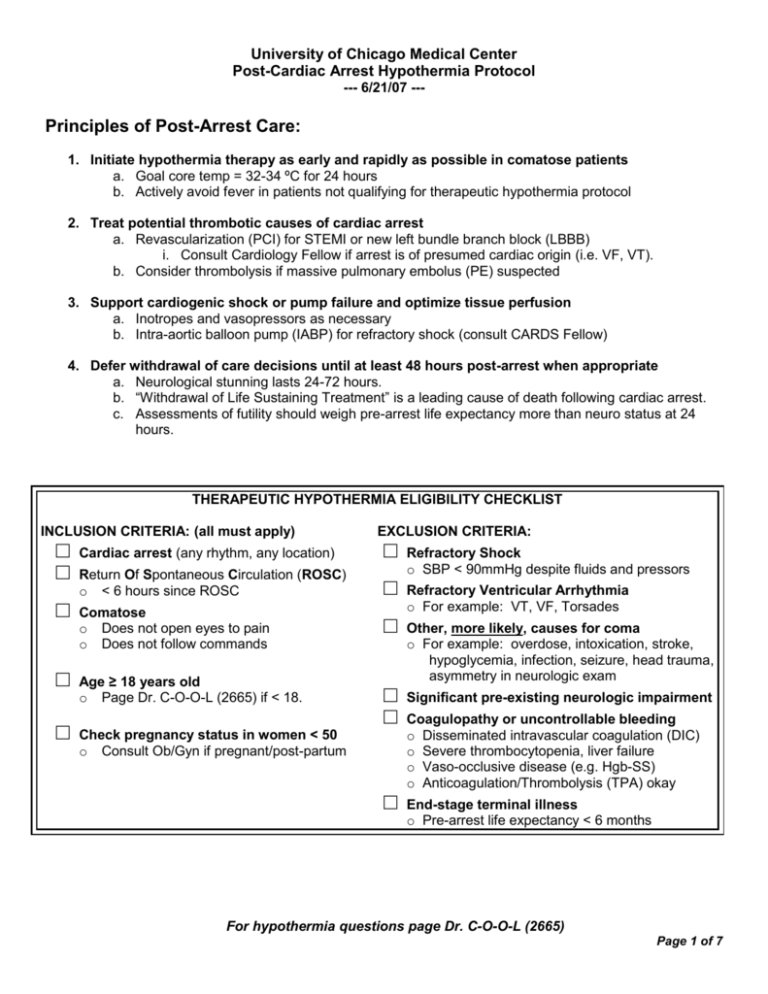
University of Chicago Medical Center Post-Cardiac Arrest Hypothermia Protocol --- 6/21/07 --- Principles of Post-Arrest Care: 1. Initiate hypothermia therapy as early and rapidly as possible in comatose patients a. Goal core temp = 32-34 ºC for 24 hours b. Actively avoid fever in patients not qualifying for therapeutic hypothermia protocol 2. Treat potential thrombotic causes of cardiac arrest a. Revascularization (PCI) for STEMI or new left bundle branch block (LBBB) i. Consult Cardiology Fellow if arrest is of presumed cardiac origin (i.e. VF, VT). b. Consider thrombolysis if massive pulmonary embolus (PE) suspected 3. Support cardiogenic shock or pump failure and optimize tissue perfusion a. Inotropes and vasopressors as necessary b. Intra-aortic balloon pump (IABP) for refractory shock (consult CARDS Fellow) 4. Defer withdrawal of care decisions until at least 48 hours post-arrest when appropriate a. Neurological stunning lasts 24-72 hours. b. “Withdrawal of Life Sustaining Treatment” is a leading cause of death following cardiac arrest. c. Assessments of futility should weigh pre-arrest life expectancy more than neuro status at 24 hours. THERAPEUTIC HYPOTHERMIA ELIGIBILITY CHECKLIST INCLUSION CRITERIA: (all must apply) □ □ □ □ □ EXCLUSION CRITERIA: Cardiac arrest (any rhythm, any location) □ Return Of Spontaneous Circulation (ROSC) o < 6 hours since ROSC □ Comatose o Does not open eyes to pain o Does not follow commands □ Age ≥ 18 years old o Page Dr. C-O-O-L (2665) if < 18. □ □ Check pregnancy status in women < 50 o Consult Ob/Gyn if pregnant/post-partum □ Refractory Shock o SBP < 90mmHg despite fluids and pressors Refractory Ventricular Arrhythmia o For example: VT, VF, Torsades Other, more likely, causes for coma o For example: overdose, intoxication, stroke, hypoglycemia, infection, seizure, head trauma, asymmetry in neurologic exam Significant pre-existing neurologic impairment Coagulopathy or uncontrollable bleeding o Disseminated intravascular coagulation (DIC) o Severe thrombocytopenia, liver failure o Vaso-occlusive disease (e.g. Hgb-SS) o Anticoagulation/Thrombolysis (TPA) okay End-stage terminal illness o Pre-arrest life expectancy < 6 months For hypothermia questions page Dr. C-O-O-L (2665) Page 1 of 7 University of Chicago Medical Center Post-Cardiac Arrest Hypothermia Protocol --- 6/21/07 --- Pre-Cooling Physician Checklist: □ Consult Inclusion/Exclusion Criteria □ Complete Therapeutic Hypothermia Post-Cardiac Arrest Order Set □ Document Initial Neurologic Status o o o Glasgow Coma Scale (best eye, verbal and motor response) If asymmetry found on neurologic exam, then order CT brain Brainstem reflexes (corneal, pupillary, occulocephalic, spontaneous respiratory effort) Spinal reflexes (rectal tone, extensor plantar “Babinski’s”) □ Record Initial Tympanic Temperature □ Send Initial Post-ROSC Labs (listed on standardized order set) □ Consult Cardiology Fellow to discuss the need for: o o o Echocardiogram within 12 hours. PTCI (in arrest cases of presumed cardiac origin) Intra-Aortic Balloon Pump (IABP) placement for refractory cardiogenic shock Hypothermia Practical Guidelines and Pitfalls: 1. Sedation/Shivering a. Shivering is primarily observed during the induction of hypothermia and usually subsides during the maintenance period. It should be treated aggressively as it increases metabolic heat production/demand and thus can make cooling difficult. b. Deeply sedate patients using standard anesthetic and opiod agents. i. NOTE: hypothermia increases half-life, decreases dose requirements and prolongs awakening time. ii. Use Richmond Agitation Sedation Scale (RASS = -4, see attached) to monitor sedation. c. Non-depolarizing paralytic agents may be used in patients with refractory shivering. i. Anticipate additional temperature drop when paralyzing a patient who is already hypothermic. ii. If paralytics are used, initiate on-going ‘train of four monitoring (TOF) with a goal of 1/4. 2. Anticipate Electrolyte Disturbances a. Overview: i. Induction of hypothermia can induce a temperature-dependent diuresis leading to both electrolyte (notably K, Mg, P and Ca) losses and intracellular shifts which have the potential for inducing cardiac arrhythmias. The literature on managing such disturbances following cardiac arrest is sparse. Accordingly, we recommend the following (primarily common sense) approach to electrolyte management: b. Potassium: i. Anticipate hypokalemia during early induction/maintenance phase of cooling. Slow/conservative repletion of K+ < 2.5 mEq/dl to low normal levels during the hypothermia maintenance phase is reasonable (adjust for urine output and renal function). NEVER REPLETE K+ DURING OR IMMEDIATELY PRIOR TO REWARMING! ii. Re-warming can induce hyperkalemia. Accordingly, be sure to check a venous K+ and discontinue all intravenous K+ repletion prior to re-warming. For hypothermia questions page Dr. C-O-O-L (2665) Page 2 of 7 University of Chicago Medical Center Post-Cardiac Arrest Hypothermia Protocol --- 6/21/07 --- c. Mg/Phos: i. Several studies have suggested that Mg may play a neuro/cardio-protective role in critically-ill patients. Repletion of Mg/Phos to high-normal levels during hypothermia is reasonable. 3. Other metabolic effects a. Hyperglycemia 1. Hypothermia decreases insulin sensitivity, insulin secretion and is associated with hyperglycemia. 2. Tight glucose control is a reasonable (though unproven) approach. 3. If an insulin drip is started, be sure to check glucose frequently during re-warming phase to avoid hypoglycemia. b. Metabolic acidosis 1. Hypothermia can also induce a mild acidosis through various mechanisms including increased production of lactate. c. Decreased drug metabolism 1. Propofol plasma levels can be ~ 30% higher at 33ºC. Titrate sedation accordingly. 4. Cardiovascular/hemodynamic effects a. MAP: Attempts should be made to maintain the Mean Arterial Pressure between 75 – 100 mmHg for the first 24-48 hours using fluids, inotropes and pressors as indicated. i. Consider intra-aortic balloon pump (IABP) placement for refractory shock. b. Heart Rate: Mild hypothermia can induce an initial tachycardia (adrenergic) followed by bradycardia. c. Arrhythmias: The risk of arrhythmias increases significantly as temperature drops below 30 ºC. As temperatures drop, the initial arrhythmia is often atrial fibrillation. Avoid over-cooling your patient. d. Cardiac Output: Can decrease by 25% due to hypothermia. e. Volume status: Hypovolemia due to cold-induced diuresis can contribute to hypotension and poor perfusion. f. Peripheral vascular resistance: Increases during hypothermia (decreases during warming – re-warm slowly). Thus aggressive warming can lead to hypotension. 5. Neurologic Assessment a. Post-arrest seizures are common and should be managed aggressively. b. If patient is receiving paralytics for excessive shivering, it will not be possible to detect status epilepticus. Be sure to consult Neurology and monitor with EEG. For hypothermia questions page Dr. C-O-O-L (2665) Page 3 of 7 University of Chicago Medical Center Post-Cardiac Arrest Hypothermia Protocol --- 6/21/07 --APPENDIX A: MEDI-THERM III Quick Reference Machine Set-Up Fill water reservoir with distilled water until green line is exposed. Connect and clamp 2 sets of gray hoses to unit (Fig. A). Connect vest wrap to one gray hose set (make sure machine is off first). Connect leg wraps in “series” using one tube from each wrap (Fig. B). Connect the remaining leg wrap tubes to the second gray hose set. Un-clamp gray hoses and wrap tubes. Turn machine ON (Machine will default to STANDBY mode). Figure A: Figure B: Hypothermia Induction Select “AUTO” mode (Figure C). Select CONTROL OPTION “Rapid”. Adjust Set Point to 34 ºC Hypothermia Maintenance (Patient Temperature ≤ 34 ºC) Change CONTROL OPTION “Gradual” Change Set Point to 33 ºC Maintain patient temperature at 33 ºC for 24 hours Figure C: Re-warming Phase Goal: T = 36.5 ºC Duration: ~ 8 hours Increase Set Point by 0.5°C/h 33 Note: When two gray hose sets are in use the Check Water Flow alarm will only sound if the flow through BOTH gray hose sets is occluded Trouble-Shooting Check the flow through the chest/leg wraps: o Confirm that gray hoses are cold, unclamped and not kinked o Confirm that Vest/Leg wrap tubes are cold, unclamped and not kinked o Disconnect one gray hose set from machine connection. If flow path is patent, alarm will not sound. o Reconnect hose to machine. o Disconnect second gray hose set from machine connection. If flow path is patent, alarm will not sound. o Reconnect hose to machine. Unable to induce cooling: o Is machine in “AUTO” (not “MANUAL” ) mode (Figure C)? o Check flow through chest/leg wraps (see above) For hypothermia questions page Dr. C-O-O-L (2665) Page 4 of 7 University of Chicago Medical Center Post-Cardiac Arrest Hypothermia Protocol --- 6/21/07 --- Foley temperature probe does not correlate with tympanic temperature: o If low-urine output or ESRD Then switch to esophageal probe Large fluctuations in patient temperature once goal is reached: o Is CONTROL OPTION set to “Gradual”? o Is patient shivering? Patient temperature is persistently > 34 ºC: o If blanket temperature 4-6 ºC and machine in “AUTO”… Then check flow through chest/leg wraps (see above) o Else order replacement unit or lower room temperature. Patient temperature is persistently < 32 ºC: o If blanket temperature at least 38-40 ºC and machine in “AUTO”... Then apply “Bair Hugger” blanket over wraps until T > 33 ºC o Else order replacement unit from Equipment Distribution. For hypothermia questions page Dr. C-O-O-L (2665) Page 5 of 7 University of Chicago Medical Center Post-Cardiac Arrest Hypothermia Protocol --- 6/21/07 --APPENDIX B: Physiological Effects of Hypothermia (Tables adapted from: Polderman, K. H. (2004). "Application of therapeutic hypothermia in the intensive care unit. Opportunities and pitfalls of a promising treatment modality--Part 2: Practical aspects and side effects." Intensive Care Med 30(5): 757-69.) For hypothermia questions page Dr. C-O-O-L (2665) Page 6 of 7 University of Chicago Medical Center Post-Cardiac Arrest Hypothermia Protocol --- 6/21/07 --- For hypothermia questions page Dr. C-O-O-L (2665) Page 7 of 7