Metabolism
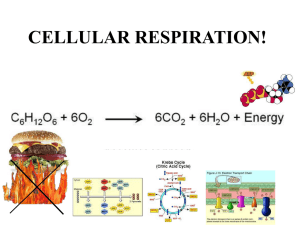
advertisement

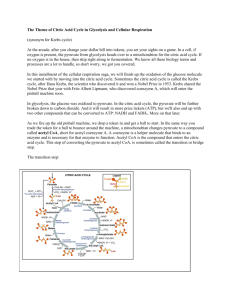
• • • • • Metabolism How do we derive energy from food, and what do we do with that energy? Catabolism Breaking down macronutrients for energy and other reasons Carb metabolism--glycogenolysis, glycolysis, TCA cycle, electron transfer chain Fatty acid beta-oxidation Protein breakdown Anabolism • • • • • • • • • • • • • • • Building up body components Requires energy Glycogenesis Gluconeogenesis Fatty acid synthesis Protein synthesis High energy compounds Adenosine triphosphate (ATP) Guanosine triphosphate (GTP) Nicotinamide adenine dinucleotide (NADH) Nicotinamide adenine dinucleotide phosphate (NADPH) – Both NADH and NADPH contain niacin Flavin adenine dinucleotide (FADH2) – Contains riboflavin Carbohydrate metabolism Glycolysis-glucose to pyruvate Pyruvate to acetyl coA Krebs/TCA/citric acid cycle Electron transport chain Glycolysis… • • • • • Is anaerobic Occurs in the cytoplasm of all cells Takes 1 molecule of glucose to 2 molecules of pyruvate Yield: 2 NADH + 4 ATP, but 2 ATP used at beginning of pathway Pyruvate Acetyl coA Occurs in mitochondria with an enzyme complex that utilizes thiamin as a • • • • • • • • • coenzyme Coenzyme A is derived from pantothenic acid 2 molecules pyruvate from 1 molecule glucose yields 2 NADH and 2 acetyl co A molecules Requires oxygen If oxygen isn’t available Pyruvate is converted to lactate Can be converted back to pyruvate when at rest, or can be converted to glucose in liver (gluconeogenesis) This can occur in muscle during strenuous exercise Citric Acid Cycle citrate Acetyl coA + oxaloacetate Produces 2 CO2 molecules Also produces 6 NADH, 2 FADH2 + 2 GTP per each original molecule of glucose (2 acetyl coA) • • • • • Electron transport chain Where NADH and FADH2 are converted to ATP 1 molecule NADH from citric acid cycle = 2.5 ATP 1 molecule FADH2 = 1.5 ATP Oxygen is required Water is produced • • • What about the NADH’s from glycolysis? Yield either 1.5 or 2.5 molecules ATP Electrons have to be shuttled into the mitochondrion So we can only give an approximate range of ATP yield • • • • The bottom line from one glucose molecule Glycolysis: 2 ATP, 3-5 ATP from NADH Pyruvate to acetyl coA: 5 ATP from NADH Citric acid cycle: 2 GTP, 3 ATP from 2 FADH, 15 ATP from 6 NADH Grand total: 30-32 ATP • • You have to spend energy to make energy Glycolysis takes 2 ATP in beginning steps The equivalent of 2 ATP is needed to start beta-oxidation of fat • • • • • • • • • • • • • Beta-oxidation of fatty acids Occurs in mitochondria, requires oxygen Fatty acids are shuttled into mitochondria by carnitine Fatty acid must be activated by coA – ATP AMP + 2P – Successive acetyl coA’s clipped off – 1 FADH2 + 1 NADH produced/clip The bottom line for beta-oxidation of stearic acid (C18:0) 20 ATP from 8 NADH 12 ATP from 12 FADH2 9 acetyl coA’s through the citric acid cycle: 9 GTP, 67.5 ATP from 27 NADH and 13.5 ATP from 9 FADH2 Minus 2 ATP to start beta oxidation: 120 ATP Fat burns in a flame of carbohydrate Carbohydrate is needed Without sufficient oxaloacetate from carb to drive the citric acid cycle, the acetyl coA from fatty acid beta-oxidation is converted to ketones ketosis Ketogenesis-Occurs in Liver Two molecules of acetyl coA combine to form acetoacetate Acetoacetate exists in equilibrium with another ketone, beta-hydroxybutyrate Acetoacetate can be used as energy source for many tissues, but not for… Ketones can be used as brain fuel in a pinch • • What about protein? Amino acids can be used for energy once amine groups are removed Some amino acid skeletons (keto acids) are converted to pyruvate or citric acid cycle intermediates--glucogenic amino acids Ketogenic amino acids are converted to acetyl coA ATP yield for amino acids is variable • Under normal conditions, protein is not metabolized for energy Only during late starvation and stress is protein used as an energy source • • • • • Gluconeogenesis Used when glucose is limited and brain/red blood cells are in need Problem: several steps in glycolysis and citric acid cycle are irreversible Solution: separate enzymes get around these blocks • Reminder You cannot make glucose from fatty acids or acetyl coA • • Lactate Glucose Conversion in liver via the Cori cycle (Gerty Cori was the first woman to win a Nobel prize in medicine for this discovery) Fatty Acid Synthesis-Lipogenesis • • • Occurs in cytosol NOT a reversal of beta-oxidation Lipogenesis utilizes energy in the form of NADPH • • • Can carbs make me fat? Yes, but not the way you think Excess carb Calories in the diet spare fat from being used for energy A small amount of carb may be converted to triglycerides Hormonal Control of Metabolism • • • • Insulin Glucagon Epinephrine-stimulates glycogenolysis during the fight or flight response Cortisol-promotes protein catabolism for gluconeogenesis in times of prolonged stress (surgery, injury) Real-Life Situations • • • • • Feasts Fasts Starvation Stress (see figs 7-22 through 7-25) • • • • Feasting Insulin rules, glucagon, epinephrine, and cortisol suppressed Anabolism--glycogen stores replenished Refill amino acid pool Excess energy stored as fat • • • • A Short-Term Fast (overnight or up to 2 days) Glucagon rules; insulin is suppressed Glycogenolysis occurs to keep brain and red blood cells fed As glycogen stores are depleted, fatty acids are burned as fuel A little gluconeogenesis from free amino acids occurs • • • Longer-term fasting (up to ~ 1 week) Insulin secretion is still suppressed Gluconeogenesis from free amino acids and glycerol Fatty acid beta-oxidation • • • Hunger-Strike Fasting (à la David Blaine) Ketones begin to supply energy to brain as free amino acids decline Body begins energy conservation measures Some brain cells are still dependent on glucose, so a little gluconeogenesis occurs from protein catabolism Late-Stage Starvation • • Fat stores depleted Protein catabolism picks up slack--muscles atrophy • • Physiological Stress Epinephrine and cortisol enter picture big time, along with glucagon Cortisol inhibits fat tissue breakdown, so energy needs are met by protein once glycogen is depleted • • Energy Balance Calories ingested - Calories expended Energy Balance If result of equation is + over time (and you’re a nonpregnant adult), you may gain weight • • • • • • • • • If result of equation is - over time, you may lose weight Calories in--control of intake physiological cues Hunger Satiation Satiety Appetite-psychological cue Control of Physiological Cues Diet composition--high fiber vs. low fiber Gut sensation of fullness Ambient temperature Hormones – Insulin suppresses synthesis of neuropeptide Y – Leptin • • • • Then we have the environmental and social influences Time of day Social situation Emotional situation Availability of food • • • Components of Energy Expenditure Resting metabolic rate Thermic effect of food Physical activity • • Resting Metabolic Rate The Calories needed for involuntary functions – Breathing – Pumping blood – Protein turnover – Neurological activity – Temperature regulation RMR is controlled by thyroid gland Thyroid hormone (thyroxine) Influences on RMR • • • • • • Age Gender Height Amount of lean body mass (muscle) Fever, infection Fasting, malnutrition • • Thermic Effect of Food Increase in metabolic rate from ingesting, digesting and absorbing food A minor contributor to total energy expenditure Physical Activity • • • • • • • • • • • The most variable component – Sedentary – Moderate activity – Heavy activity – Exceptional activity Direct measurement of energy expenditure--Calorimetry Direct--person resides in a controlled chamber Indirect--measurement of oxygen in and carbon dioxide out Doubly labeled water--expensive, but a good measurement Do the math! Convert your weight to kg (lb/2.2) If male, multiply wt x 1.0 Cal/kg/hr x 24 hr If female, wt x 0.9 Cal/kg/hr x 24 hr Adjust by physical activity (see table 8.4) – Sedentary x 1.2-1.3 Light x 1.3-1.45 – Moderate x 1.45-1.65 Heavy x 1.65-1.9 – Exceptional x 1.9-2.2 Example 1 A 35-yr-old man who works in front of a computer for 10+ hr/day; parks next to his building; physical activity consists of going from recliner to fridge to recliner on weekends Wt: 176 lb., or 80 kg (176 /2.2) 80 x 1 x 24 = 1920 x 1.2-1.3 = 2300-2500 Example 2 • 21 yr old female; physical therapy major at UW; in training for triathlons in • • • November & December; also works at gym as a trainer Wt: 125 lb. /56.8 kg Basal Calories: Activity level: • • • • How to Calculate Ideal Body Weight Males: 106 lb for 1st 5’ of ht, then 6 lb for each in over 5’ Females: 100 lb for 1st 5’ of ht, then 5 lb for each in over 5’ Add 10% for a large frame Subtract 10% for a small frame • Assessing body composition Weight--may not tell you much • • • Body mass index = wt (lb)/ht (in)2 x 704.5 [or wt (kg)/ht (m)2] Also may not tell you much What does the BMI # mean? • • • • • • • • • < 16 Too lean 16-19.9 Lean, maybe underweight 20-24.9 Desirable 25-29.9 Overweight 30-34.9 Grade I obesity 35-39.9 Grade II obesity ≥ 40 Morbidly obese Estimates of body fat distribution Waist-hip ratio-high risk numbers – > 0.8 in women – > 0.9 in men Waist circumference-preferable numbers – < 35” for women – <40” for men • • • • • • • • • • • Measuring body fat Densitometry--underwater weighing Air displacement--the Bod Pod Skinfold thickness DEXA Bioelectrical impedance MRI or CT scan Too much vs. too little body fat Both extremes can be hazardous to health Both are at high risk in hospital situation Women with too little body fat may have abnormal or absent menstrual periods, which may predispose them to early bone loss Patterns of Body Fat Gynoid (pears)--fat concentrated below waist – Seen mostly in premenopausal females Android (apples)--fat concentrated in trunk – Seen mostly in men Obesity • The plague of an affluent society Current obesity risk factors • • • • Genetics – The “thrifty gene” hypothesis Environment Age and lifestyle Gender Weight Management • • • • • Reduced intake – 1 lb fat = 3500 Calories Increased exercise Behavioral change Medication Surgery • • Eating Disorders “You can never be too rich or too thin” The Duchess of Windsor • • • Eating Disorders Psychiatric disorder with medical & nutritional implications Men can also be affected Can be related to incidents of abuse, perfectionistic parents, chaos at home • • • • • • • Eating Disorders≠Disordered Eating Eating disorders are illnesses that interferes with daily living Disordered eating is usually temporary – For example, high school and college wrestlers – However, can evolve into full-blown eating disorders Anorexia Nervosa Starving oneself to attain a certain body image Sufferers want to be in control of something Some also have obsessive-compulsive disorder Behavior Patterns in Anorexia Nervosa Restrictors-simply don’t eat enough food Restrict and purgers-may get rid of food via vomiting, laxative or diuretic (“water pill”) abuse • • Consequences of Anorexia Nervosa (*females) Fat store depletion, muscle wasting Reduced estrogen production* • • Amenorrhea Reduced bone density Male body hair pattern More consequences of AN • • • • • Hair loss, dry skin Reduced blood pressure, pulse, respiration Dehydration Electrolyte (Na, K) imbalances Death due to heart failure • • Treatment Unfortunately, relapse rate is high Requires team approach--MD’s (psychiatrist and pediatrician or internist), nurses, dietitians Patients must be refed very slowly Monitor Calories, not weight gain • • • • • • Bulimia Patient at or near ideal body weight About 1/2 of anorexics become bulimic Binging followed by purging Preoccupation with body weight Consequences--tooth damage, swollen salivary glands, electrolyte imbalance Also needs team approach to therapy • • • • • • Binge Eating Disorder A relatively new diagnosis in the manual of psychiatry Person eats massive amounts of Calories at a sitting WITHOUT purging at least 2 days a week for 6 months Binges accompanied by guilt and shame FOOD IS AN ADDICTIVE DRUG