Clinical Orientation to St. Catherine`s Hospital
advertisement
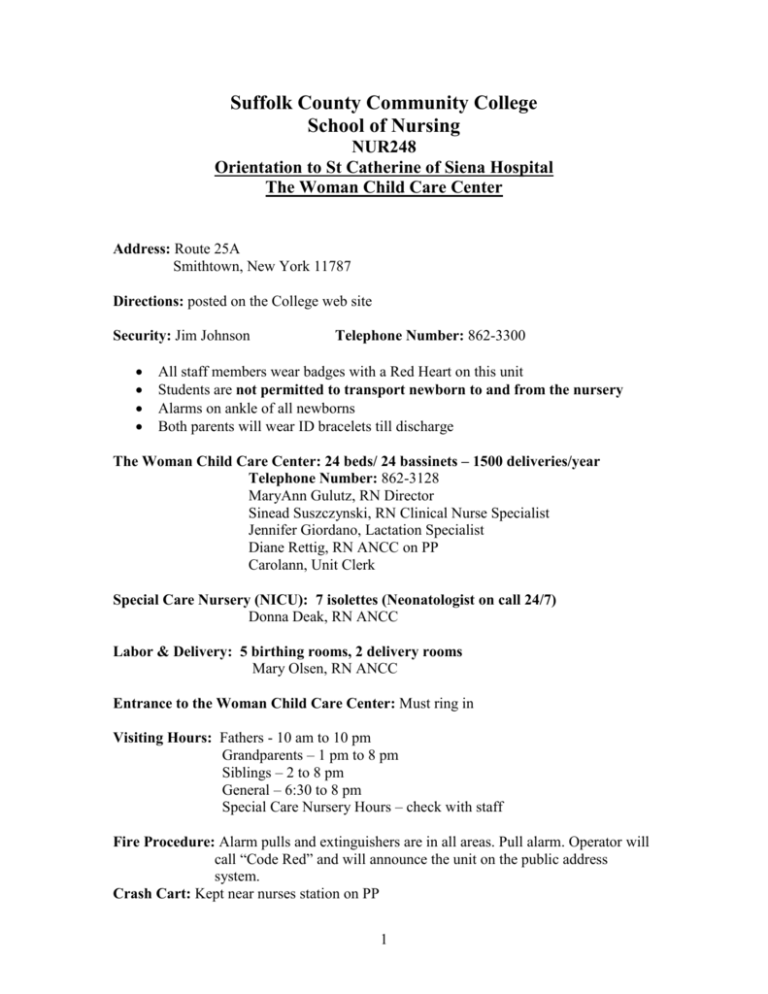
Suffolk County Community College School of Nursing NUR248 Orientation to St Catherine of Siena Hospital The Woman Child Care Center Address: Route 25A Smithtown, New York 11787 Directions: posted on the College web site Security: Jim Johnson Telephone Number: 862-3300 All staff members wear badges with a Red Heart on this unit Students are not permitted to transport newborn to and from the nursery Alarms on ankle of all newborns Both parents will wear ID bracelets till discharge The Woman Child Care Center: 24 beds/ 24 bassinets – 1500 deliveries/year Telephone Number: 862-3128 MaryAnn Gulutz, RN Director Sinead Suszczynski, RN Clinical Nurse Specialist Jennifer Giordano, Lactation Specialist Diane Rettig, RN ANCC on PP Carolann, Unit Clerk Special Care Nursery (NICU): 7 isolettes (Neonatologist on call 24/7) Donna Deak, RN ANCC Labor & Delivery: 5 birthing rooms, 2 delivery rooms Mary Olsen, RN ANCC Entrance to the Woman Child Care Center: Must ring in Visiting Hours: Fathers - 10 am to 10 pm Grandparents – 1 pm to 8 pm Siblings – 2 to 8 pm General – 6:30 to 8 pm Special Care Nursery Hours – check with staff Fire Procedure: Alarm pulls and extinguishers are in all areas. Pull alarm. Operator will call “Code Red” and will announce the unit on the public address system. Crash Cart: Kept near nurses station on PP 1 Other Important Information: Pre-conferences – report to the staff cafeteria by 8:00 am If absent or late: please call my cell # 948-7416 the night before 10 pm, or in the morning call the obstetric unit by 6:45 am at 862-3128. Leave me a message with the reason for absence or lateness. Please keep your phone chain handy as you will be responsible to notify your designated classmate if you are called for school closing or late start. There are no lockers. Do not bring valuables to clinical Eat breakfast before clinical. Your body needs it. Charting and signing of the charts: use black ink only. Please show us your notes before putting them in the patient’s chart. I must co-sign all notes and medication sheets. SCCC/SN should follow your full first and last name Dress Code: As per school policy, wear SCCC photo ID Change into scrubs (will be provided for you)when assigned to L&D Charting: I&O sheets are to be filled every hour we are here (located outside rooms) Clinical Pathways are specific for Vaginal delivery, C/S delivery, Vaginal Newborn Care and C/S Newborn Care Pain Management (pink sticker on Progress sheet) and I&O sheet can be found in the Medication section of the chart Focus charting will be done when necessary Medication System: MAR (Medication Administration Record) in separate book Medications are prepared in the med room then carried into the patient’s room IVPB schedule is 12 am/ 6 am/ 12 pm/ 6 pm IV site, tubing and dressing are changed q72h, if not done document why it was not done IV tubing 15gtts/cc (Horizon Pumps only for C/S and certain meds) SASS method used for saline lock – 1cc saline flush, administer medication, and then follow with 3cc saline flush. Every shift a 2cc saline flush is administered if NO medication is given. (Hospital has pre-filled syringes) Special Med sheet kept on clip board at nurse’s station if patient received epidurals – evaluated q4h and all info charted Remember to chart all IVPB medications on the I&O sheet Post Partum and Newborn Protocol MD’s Orders are pre-stamped on orders sheet All Parents must view “Shaken Baby Video” prior to discharge Supplies: 2 Found in clean utility room Each infant is given its own individual equipment and supplies – obtain from newborn nursery Isolation Room: Room 103 Handwashing: Must do 3 minute scrub in Newborn nursery before starting care unit with special soap (red dispenser next to sink in newborn nursery) Leave jewelry at home May wear wedding band Absolutely no acrylic nails Nail polish permitted if light colors are used Bathing: Vaginal deliveries shower as soon as stable or 4 hours after delivery C/S complete bed bath on admission, shower next AM Newborns bathed only when temperature stabilizes above 98O F Perineal Care: Void or catherize q6h for distension Peri-bottle using warm water after each void or BM Pat dry with tissues then apply sanitary pad Dermaplast/ Nupercanial ointment/ Tucks pads Sitz baths if ordered C/S Patients: VS every 15 min. x 4, then every 30 min. x 4, then every 1 hr. x 2, then every 4 hrs. times 24 hrs. and as indicated Mefoxin 2 gm. IVPB at cord clamping IV Lactated Ringer’s with Pitocin PCA Fentanyl for 24/48 hours (Demerol and Morphine alternative choice) Surgical dressing generally removed by MD, may be removed by nurse with MD order Foley catheter removed 24 hours following procedure OOB to chair ASAP Labs: H&H on 1st PP day Rhogam if eligible Rubella vaccine if titer 1:10 or less (May be giving MMR) Flu vaccine/ TDap vaccine Additional labs as ordered PKU (newborn metabolic screening) heel stick is done before discharge Cord blood is taken from all infants at time of delivery for type, Coomb’s if needed 3 Possible bilirubin workup – phototherapy isolette with bili-lights, cover eyes, keep uncovered except for diaper, rectal temps taken q4h All newborns should be placed on their backs at all times NICU (You will be an observer in this area unless the RN is willing to mentor you) Vital signs: Newborn done every ½ hour x 2 hrs. after birth, then once a shift Rectal temp done at admission on all newborns then axillary temps q4h Head and chest circumference with complete newborn assessment done at admission to nursery Pulse Ox taken on day of discharge on all newborns, must be <95% before discharge Newborn Weights: Done initially in L&D for then every night till discharge Blood glucose testing: Will not be done by students, ask RN for results and use this information is patient (mother) needs to be given insulin coverage Done at admission on all newborns (heel stick) Should be between 45-90 Hypoglycemic protocol (review hospital policy) may be initiated for newborn – keep infant warm and feed frequently Newborn Feedings: NPO for 4 hours, then sips of water followed by formula q3-4h Advance Similac 20 calories/ fluid ounce If Breast feeding, may begin in L&D – on demand schedule Record Intake Cord Care: On admission count vessels No other cleaning necessary while in hospital Keep exposed to air and dry Most MD’s instruct their patient’s to use alcohol to cleanse area when at home Circumcision Care: Circumcision usually done on day shift “Time Out Right Patient” MD gets consent signed Lots of A&D ointment on day of circ to avoid sticking to diaper Must void before being discharged Elimination: 4 Observe and record first stool and all subsequent stools for color, amount, and frequency Record first void and all subsequent voids Notify staff if no output (check every two hours) Drugs: Hepatitis B vaccine (IM) You are responsible for: The mother and/or newborn Identification of mother and newborn Helping parents with feeding, diapering, general care Charting intake and output for both mother and infant Observing the parent/infant interaction Answering questions, ongoing education Parents viewing “Shaken Baby” video before discharge – view with parents if possible Assessment of infant or mother, charting findings Reporting abnormalities to staff ASAP & instructor Discharging mother or infant Hepatitis Birth Dose given before discharge to newborn – need consent L&D Protocol (You will be an observer in this area unless the RN is willing to mentor you) Obtain history and assessment Urine sample tested for U/A, protein NPO, ice chips or clear fluids as per MD order IV’s started as per MD order Fetal monitoring applied for baseline strip for 15 minutes, then encourage walking if ordered or continuous monitoring if in active labor as per MD order Vaginal exam sterile to assess station, effacement, and dilation, to AROM (rupture artificially membranes) Medications most frequently used : Pitocin, Fentanyl, Bupivacaine, Bicitra, Demerol, Phenergan, MgSo4, Terbutaline, Toradol, and Cervidil Medications given to Newborn after delivery: Vitamin K (IM) and Erythromycin ointment (to eyes) Weight of newborn/ APGAR score of newborn 4th stage of labor (first hour after delivery) 5 6