Pharmacology Objectives 6 - U
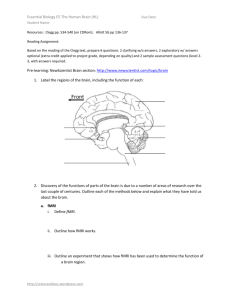
advertisement

Pharmacology Lecture 6 Autonomic Pharmacology 1) Describe the anatomical organization of the sympathetic and parasympathetic divisions of the autonomic nervous system (ANS). Sympathetic division – sympathetic nerves arise from the thoracic and lumbar divisions (thoracolumbar) of the spinal cord. Preganglionic sympathetic fibers originate from neurons in the intermediolateral columns of the spinal cord, are carried over the ventral roots to paravertebral and prevertebral ganglia, and synapse with postganglionic fibers in the sympathetic chain (paravertebral) and abdominal organs (prevertebral). Collateral fibers connect preganglionic fibers with ganglion cells for mass discharge Adrenal medulla – Chromaffin cells, ganglion cells that have not differentiated into neurons, receive innervation from sympathetic preganglionic fibers through the greater splanchnic nerve. Parasympathetic division – parasympathetic nerves arise from cranial nerves (III, VII, IX, and X) and from the sacrum (craniosacral) and synapse with ganglion cells located in the effector organ. Enteric division – consists of an intrinsic intramural collection of myenteric and submucosal plexuses located in the GI tract and modulated by extrinsic sympathetic and parasympathetic fibers. 2) Describe the sympathetic nervous system response to “fight or flight” situations. General discharge of the sympathetic nerves and adrenal medulla in response to stress is termed the “fight or flight response.” The following are sympathetic responses: Pupil – dilation Salivary gland – Bronchial smooth secretion muscle – relaxation Heart – acceleration GI smooth muscle – Spleen capsule Most arterioles – relaxation constriction constriction 3) Describe how single innervation of the arterioles by the sympathetic division can lead to both constriction and dilation of these blood vessels. Arterioles are distensible tubes filled with a liquid under pressure. Vasoconstriction is achieved through sympathetic activation, which causes smooth muscle contraction and vessel narrowing. Vasodilation occurs when sympathic stimulation ceases. This allows the vessels to dilate passively due to the distending force produced by the blood pressure. 4) List the three major transmitters of the autonomic nervous system. Acetylcholine, epinephrine, and norepinephrine. 5) List the five steps of neurotransmission. 1. Synthesis of the transmitter chemical. 2. Storage of transmitter molecules in vesicles transported by microtubules. 3. Release of transmitter in response to a nerve action potential and diffusion of transmitter from its site of release from the pre-junctional neuron to its 4. Interaction with the effector membrane on the postjunctional effector cell and 5. Termination of action of the neurotransmitter by enzymatic degradation, reuptake into the terminal, or diffusion away from the site of action. 6) Describe the sites in the ANS where acetylcholine is the neurotransmitter. Acetylcholine is the neurotransmitter at sympathetic ganglia, parasympathetic ganglia, adrenal medulla, parasympathetic post-ganglionic nerve terminal, and neuromuscular junction of somatic nerves and skeletal muscle. 7) Describe the major mechanism by which acetylcholine is inactivated, by which norepinephrine is inactivated. Acetylcholine’s actions are terminated rapidly by acetylcholinesterase, which hydrolyzes acetylcholine into acetate and choline. Choline can then be transported back to be used in acetylcholine synthesis. Norepinephrine’s actions are terminated by (1) reuptake into the terminal, (2) oxidative deamination by monamine oxidase in mitochondria, (3) 0-methylation by catechol-0-methyltransferase, and (4) diffusion away from the synapse. 8) Identify the sites in the ANS where neurotransmission is mediated by nicotinic or muscarinic acetylcholine receptors. Nicotinic cholinergic receptors are located on: (1) all autonomic sympathetic and parasympathetic ganglia (including the adrenal medulla) and (2) the neuromuscular junction of somatic nerves and skeletal muscle. Muscarinic cholinergic receptors are located on: postganglionic parasympathetic neuroeffector cells. 9) Describe the sites in the ANS where norepinephrine is used as the neurotransmitter. Norepinephrine is the neurotransmitter for most sympathetic postganglionic neuroeffector junctions. The one exception is innervation of thermoregulatory sweat glands, which uses acetylcholine, although the palms still use norepinephrine (clammy hands when stressed). 10) List the two general types of adrenergic receptors. Alpha (α) and beta (β). Alpha stimulation is usually excitatory (except in the gut). Beta stimulation is usually inhibitory (except in the heart). In the GI tract both relax smooth muscle while in the heart beta simulation increases rate and contractility. 11) Describe the origin of epinephrine and its site of release. Origin: The amino acid tyrosine is hydroxylated by tyrosine hydroylase to form dihydroxyphenylalanine (DOPA) and is then decarboxylated by DOPA decarboxylase to form dopamine. Dopamine is hydroxylated in vesicles on the β carbon of the ethylamine side-chain by dopamine β-hydroxylase to form norepinephrine. In certain areas of the brain and the adrenal medulla, norepinephrine is methylated on the amine group by phenylethanolamine-N-methyltransferase to form epinephrine. Site of release: Epinephrine is release from the adrenal medulla into the blood stream, think of it like a neurohormone. 12) Describe the sympathetic/parasympathetic neurotransmitters and their receptors for increasing or decreasing heart rate. Sympathetic (thoracolumbar) Acetylcholine (preganglionic) Norepinephrine (postganglionic) Parasympathetic (craniosacral) Acetylcholine (vagal preganglionic) Acetylcholine (postganglionic in heart) Nicotinic cholinergic receptor Beta-adrenergic (β1) receptor Nicotinic cholinergic receptor Muscarinic (AV and SA nodes) ↑HR and contractility resulting in increased cardiac output ↓HR and contractility resulting in ↓CO 13) Describe the effects of sympathetic/parasympathetic activation on pupil size and lens accommodation. Sympathetic (Dark) Acetylcholine (preganglionic) Norepinephrine (postganglionic) Parasympathetic (Light) Acetylcholine (preganglionic) Acetylcholine (postganglionic in eye) Nicotinic cholinergic Alpha-adrenergic (α1) Nicotinic cholinergic Muscarinic (constrictor muscle) Pupil dilation (mydriasis) – dialator pupillae muscle Pupil contraction (miosis) – constrictor papillae muscle 14) Describe the mechanisms by which adrenergic agonists and muscarinic antagonists both produce mydriasis. Adrenergic agonists stimulate the alphaadrenergic receptors (α1), which normally occurs due to norepinephrine released from the postganglionic fibers to the dilator pupillae muscle, resulting in mydriasis. Muscarinic antagonists prevent parasympathetic stimulation of the constrictor papillae muscle by acetylcholine causing it to relax, which results in mydriasis. 15) Describe what is meant by denervation supersensitivity. When the nervous supply of a muscle or gland is interrupted, the effector organ slowly becomes increasingly sensitive to the neurotransmitter of which it is deprived. This occurs because of upregulation of receptors after one to two weeks. 16) List the common side effects seen with the use of cholinergic antagonists. Muscarinic receptor antagonists: dry mouth, constipation, decreased sweating, mydriasis (dilation of pupil), urinary retention (especially in elderly males with benign prostatic hypertrophy), tachycardia, decreased lacrimation, precipitation of glaucoma, and decreased respiratory secretions (increased susceptibility to respiratory infections. Nicotinic receptor antagonists (sympathetic and parasympathetic ganglionic blockers): constellation of severe side effects – constipation (blocking enteric ganglia), atony of the bladder, cycloplegia, decreased sweating, postural hypotension, and tachycardia (SA node dominated by parasympathetics). 17) Contrast the therapeutic advantage of pilocarpine to acetylcholine. Pilocarpine exhibits primarily muscarinic receptor agonist actions and it is not degraded by cholinesterases thus it has a 2-3 hour duration. It can be given orally. Acetylcholine however, is a non-selective agonist of both muscarinic and nicotinic receptors and its duration is very brief because it is rapidly hydrolyzed by plasma cholinesterases. It cannot be given orally. 18) Describe the differences between a direct and indirect acting cholinergic drug. Direct acting agonists bind to the cholinergic receptor and mimic the effects of the natural receptor ligand acetylcholine. Indirect acting agonists inhibit the destruction of acetylcholine by acetylcholinesterase, thereby increasing the synaptic concentration of acetylcholine which then acts on the cholinergic receptor. 19) Identify the major advantage for using quaternary cholinesterase inhibitors. Quaternary cholinesterase inhibitors, neostigmine and edrophonium, do not significantly cross the blood-brain barrier, and therefore, they are useful for treating peripheral disorders like intestinal and bladder atony and for the management of myasthenia gravis. 20) Describe the drug of choice for reactivating cholinesterase shortly after organophosphate poisoning. The treatment of choice for severe intoxication with centrally acting cholinesterase inhibitors is atropine, given in large doses to combat the central manifestations (confusion, ataxia, convulsions, coma, and respiratory paralysis) and the peripheral signs (bronchial secretions, hypotension, and involuntary twitching leading to paralysis) resulting from overstimulation of muscarinic receptors. Atropine is a muscarinic receptor antagonist, a tertiary amine capable of penetrating into the CNS and blocking all subtypes of muscarinic receptors. 21) Describe the major symptoms of a cholinergic crisis. The common signs of “cholinergic crisis” are salivation, lacrimation, urination, defecation, emesis (“SLUDE” syndrome). 22) Describe the therapeutic uses of muscarinic agonists. Glaucoma – carbachol acts on the muscarinic receptors of the constrictor papillae muscle to produce miosis, thereby opening the canals of Schlemm to facilitate outflow of aqueous humor and decrease intraocular pressure. Diagnosis of achalasia & bronchial airway hyperreactivity – methacholine is used to diagnostically test the response of the lower esophageal sphincter in suspected cases of esophageal achalasia. When inhaled in a NaCl solution it can be used to diagnose bronchial airway hyperreactivity in patients whose asthma is not clinically apparent. Gastrointesinal and urinary bladder atony – bethanechol can be used to increase tone and contractions of the intestine and bladder in patients with postpartum or postsurgical ileus and urinary retention. 23) Describe the mechanism by which muscarinic agonists produce vasodilation. Vasodilation is brought about by activation of muscarinic receptors (M3 type) on endothelial cells which promote the release of nitric oxide (endothelium relaxing factor) that diffuses into the vascular smooth muscle and produces relaxation. 24) Describe the therapeutic uses of cholinesterase inhibitors. Treat glaucoma – phyostigmine given topically in the eye causes stimulation of the constrictor papillae through activation of muscarinic receptors by acetylcholine. Reverse atropine toxicity – phyostigmine is a tertiary amine that penetrates into the CNS and is therefore capable of reversing the effects of atropine poisoning. Reverse neuromuscular blockers – pyridostigmine reverses the effects of curariform toxicity and other neuromusclular blockers. Treat myasthenia gravis – neostigmine does not cross the blood-brain barrier and therefore works in the periphery to increase muscle strength. 25) Describe the uses for alpha and beta adrenergic receptor blockers. Objective 31. 26) Describe the homeostatic reflex changes in blood pressure and heart rate in the presence of norepinephrine, in the presence of epinephrine. Norepinephrine – activates alpha-1, alpha-2, and beta-1 receptors. Vascular alpha-1 receptors cause vasoconstriction, an increase in TPR and diastolic pressure. Beta-1 receptors cause an increase in heart rate and contractility. This is countered by activation of the baroreceptor reflex causing vagal stimulation and slowed HR such that the net effect is increased mean pulse pressure. Epinephrine – activates alpha-1, alpha-2, beta-1, and beta-2 receptors. Alpha-1 activation causes vasoconstriction, increased TPR and diastolic pressure. Vascular beta-2 actions induce vasodilation that partly offsets the alpha-1-induced increase in diastolic pressure such that the effect is less than that of norepinephrine. Due to these counteracting effects, dose is important in epinephrine’s effects. Renal and cutaneous vessels have more alpha-1 than beta-2 receptors thus the overall effect is constriction. Skeletal muscle vessels have more beta-2 than alpha-1 receptors and are dilated by low doses or slightly constricted by high doses. Therefore, with low doses diastolic pressure falls (beta-2 predominates) but with high doses it rises (alpha-1 predominates). The beta-1 effect on contractility increases mean pulse pressure, so systolic pressure is increased more than diastolic pressure. 27) Give the rationale for inclusion of epinephrine in local anesthetics. Epinephrine causes constriction of cutaneous vessels such that the blood flow is reduced and the anesthetic is cleared more slowly. Therefore the anesthetic acts longer at the site. 28) Contrast the effects of dobutamine to isoproterenol. Dobutamine – a beta-1 agonist used primarily to stimulate the heart in cases of cardiogenic shock resulting from an MI. It is also used in cardiac decompensation due to depressed myocardial contractility. Isoproterenol – is a beta-1 and beta-2 agonist used by inhalation as a bronchial dilator, but it also induces tachycardia due to its beta-1 action. This action is useful in cases of transient heart block or cardiac arrest until cardioversion is performed. 29) Describe how clonidine is thought to exert its antihypertensive effects. Clonidine is a selective alpha-2 receptor agonist acting at presynaptic receptors to inhibit the release of norepinephrine. Its antihypertensive effects are due to activation of alpha-2 receptors in the CNS resulting in decreased sympathetic outflow to the heart and blood vessels. 30) Contrast the effects of phentolamine and prazosin blockade on the release of norepinephrine, and understand the mechanism responsible for these differences. Phentolamine is a competitive antagonist of both alpha-1 and alpha-2 receptors. Inhibition of alpha-2 receptors causes excess norepinephrine secretion from cardiac adrenergic neurons with consequent tachycardia. Prozosin is a selective alpha-1 receptor antagonist used in the treatment of hypertension. Blocking alpha-1 receptors inhibits the vasoconstrictor effects of norepinephrine. The lack of alpha-2 effects prevents excess norepinephrine release. Remember that alpha-2 receptors are mainly on presynaptic membranes and alpha-1 receptors are on postsynaptic membranes. 31) List the common effects of beta and alpha blockers on cardiovascular function. Agent Beta Blockers Alpha Blockers Effects Bradycardia Bronchial Constriction Hypotension Vasodilation Lower BP Orthostatic hypotension Tachycardia Uses Hypertension, Arrhythmias, Angina pectoris, Glaucoma, Migraine headaches, Stage fright, Prophylaxis after MI Hypertension, Raynaud’s disease, Sequelae of frostbite, Pheochromocytoma, Shock 32) Describe the mechanism by which beta-blockers (eg. timolol) lower intraocular pressure. Timolol is a beta-1 and beta-2 blocker used in the eye for the management of glaucoma. The thought is that beta receptors promote formation of aqueous humor, so by blocking them, the rate of aqueous production and thus intraocular pressure is ↓. 33) Describe therapeutic uses for alpha-adrenergic receptor blockers. Raynaud’s disease – phentolamine prevents vasospasm related to this disease. Pheochromocytoma – phentolamine prevents the HTN and tachycardia. Erectile dysfunction – phentolamine can be combined with papaverine and a prostaglandin for corpus cavernosum injections. Hypertension – prazosin interferes with the vasoconstrictor effects of norepinephrine thus allowing vasodilation and decreasing TPR. Urinary retention due to benign postatic hyperplasia – prazosin, terazosin, and doxazosin relax bladder neck and prostate. 34) Describe dopamine’s mechanism of action. Dopamine exerts agonist effects on adrenergic as well as on dopaminergic receptors. Dopamine D1 receptors are especially prominent in the renal and mesenteric vascular beds and their activation causes dilation of the blood vessels. Dopamine D2 autoreceptors are important in the modulation of neurotransmitter release. In low doses its preferential action is to stimulate dopamine receptors producing relaxation of vascular smooth muscle in the renal blood vessels, thereby improving renal flow which is compromised in shock. Moderate doses stimulate beta-1 receptors in the heart to increase CO. higher doses recruit the actions of alpha-1 adrenergic receptors to produce vasoconstriction, increased BP, and less vasoconstriction in renal vessels than elsewhere. 35) Describe the mechanism of action of indirectly acting sympathomimetics. The main action of these compounds is not through the stimulation of adrenergic receptors, but rather through the release of norepinephrine or blockade of its inactivation by preventing its reuptake. Ephedrine causes the release of norepinephrine in the CNS (stimulation) and specifically on beta-2 receptors (bronchodilation and vasodilation). Pseudoephedrine has less CNS and beta-2 effects but is used because of its vasoconstrictive properties. Amphetamine causes norepinephrine release resulting in stimulation, increased BP and heart rate. Cocaine blocks norepinephrine reuptake causing euphoria, but it may also be used in surgery for its vasoconstrictive and anesthetic properties.