Antihistamines_Revie..
advertisement
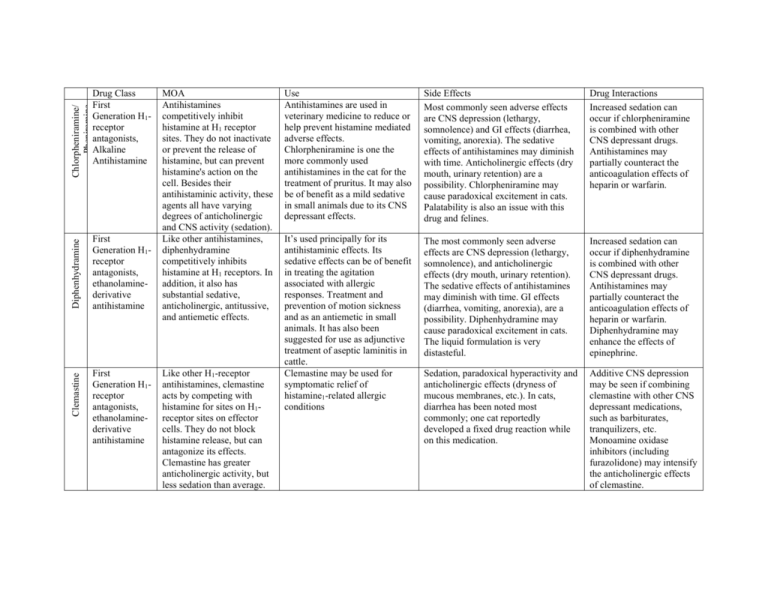
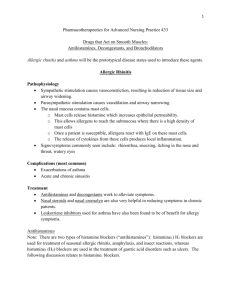
Chlorpheniramine/ Pheniramine Diphenhydramine First Generation H1receptor antagonists, ethanolaminederivative antihistamine Clemastine Drug Class First Generation H1receptor antagonists, Alkaline Antihistamine First Generation H1receptor antagonists, ethanolaminederivative antihistamine MOA Antihistamines competitively inhibit histamine at H1 receptor sites. They do not inactivate or prevent the release of histamine, but can prevent histamine's action on the cell. Besides their antihistaminic activity, these agents all have varying degrees of anticholinergic and CNS activity (sedation). Like other antihistamines, diphenhydramine competitively inhibits histamine at H1 receptors. In addition, it also has substantial sedative, anticholinergic, antitussive, and antiemetic effects. Like other H1-receptor antihistamines, clemastine acts by competing with histamine for sites on H1receptor sites on effector cells. They do not block histamine release, but can antagonize its effects. Clemastine has greater anticholinergic activity, but less sedation than average. Use Antihistamines are used in veterinary medicine to reduce or help prevent histamine mediated adverse effects. Chlorpheniramine is one the more commonly used antihistamines in the cat for the treatment of pruritus. It may also be of benefit as a mild sedative in small animals due to its CNS depressant effects. Side Effects Most commonly seen adverse effects are CNS depression (lethargy, somnolence) and GI effects (diarrhea, vomiting, anorexia). The sedative effects of antihistamines may diminish with time. Anticholinergic effects (dry mouth, urinary retention) are a possibility. Chlorpheniramine may cause paradoxical excitement in cats. Palatability is also an issue with this drug and felines. Drug Interactions Increased sedation can occur if chlorpheniramine is combined with other CNS depressant drugs. Antihistamines may partially counteract the anticoagulation effects of heparin or warfarin. It’s used principally for its antihistaminic effects. Its sedative effects can be of benefit in treating the agitation associated with allergic responses. Treatment and prevention of motion sickness and as an antiemetic in small animals. It has also been suggested for use as adjunctive treatment of aseptic laminitis in cattle. Clemastine may be used for symptomatic relief of histamine1-related allergic conditions The most commonly seen adverse effects are CNS depression (lethargy, somnolence), and anticholinergic effects (dry mouth, urinary retention). The sedative effects of antihistamines may diminish with time. GI effects (diarrhea, vomiting, anorexia), are a possibility. Diphenhydramine may cause paradoxical excitement in cats. The liquid formulation is very distasteful. Increased sedation can occur if diphenhydramine is combined with other CNS depressant drugs. Antihistamines may partially counteract the anticoagulation effects of heparin or warfarin. Diphenhydramine may enhance the effects of epinephrine. Sedation, paradoxical hyperactivity and anticholinergic effects (dryness of mucous membranes, etc.). In cats, diarrhea has been noted most commonly; one cat reportedly developed a fixed drug reaction while on this medication. Additive CNS depression may be seen if combining clemastine with other CNS depressant medications, such as barbiturates, tranquilizers, etc. Monoamine oxidase inhibitors (including furazolidone) may intensify the anticholinergic effects of clemastine. Hydroxyzine First Generation H1receptor antagonists, piperazinederivative antihistamine Hydroxyzine acts by competing with histamine for sites on H1-receptor sites on effector cells. Antihistamines do not block histamine release, but can antagonize its effects. In addition to its antihistaminic effects, hydroxyzine possesses anticholinergic, sedative, tranquilizing, antispasmodic, local anesthetic, mild bronchodilative, and antiemetic activities. Hydroxyzine is used principally for its antihistaminic, antipruritic and sedative/tranquilization qualities, often in atopic patients. The most likely adverse effect associated with hydroxyzine is sedation. In dogs, this is usually mild and transient. Occasionally antihistamines can cause a hyperexcitability reaction. Dogs have reportedly developed fine rapid tremors, whole body tremors and rarely, seizures while taking this drug. Cats may develop polydipsia, depression or behavioral changes while on this medication. Additive CNS depression may be seen if combining hydroxyzine with other CNS depressant medications, such as barbiturates, tranquilizers, etc. Additive anticholinergic effects may occur when hydroxyzine is used concomitantly with other anticholinergic agents. Hydroxyzine may inhibit or reverse the vasopressor effects of epinephrine. Use norepinephrine or metaraminol instead. Trimeprazine/ Promeprazine First Generation H1receptor antagonists, phenothiazine antihistamine Trimeprazine has antihistaminic, sedative, antitussive and antipruritic qualities. The veterinaryapproved product also has prednisolone in its formulation that provides additional antiinflammatory effects. Trimeprazine is used alone for the treatment of pruritic conditions, especially if induced by allergic conditions. For trimeprazine, possible adverse reactions include: sedation, depression, hypotension and extrapyramidal reactions (rigidity, tremors, weakness, restlessness, etc.). Other CNS depressant agents (barbiturates, narcotics, anesthetics, etc.) may cause additive CNS depression if used with phenothiazines. Quinidine when given with phenothiazines may cause additive cardiac depression. Antidiarrheal mixtures (e.g., Kaolin/pectin, bismuth subsalicylate mixtures) and antacids may cause reduced GI absorption of oral phenothiazines. Increased blood levels of both drugs may result if propranolol is administered with phenothiazines. Phenothiazines block alpha-adrenergic receptors; if epinephrine is also given, unopposed beta activity causing vasodilation and increased cardiac rate can occur. Phenytoin metabolism may be decreased if given concurrently with phenothiazines. Oxatomide Second Generation antihistamine, firstgeneration of the piperazine class. In addition to its H1 receptor antagonism, it also possesses antiserotonergic actions. Oxatomide lacks any anticholinergic effects. Astemizole second generation antihistamine Astemizole competitively binds to histamine H1receptor sites in the gastrointestinal tract, uterus, blood vessels, and bronchial muscle. This suppresses the formation of edema and pruritus (caused by histamine). Astemizole does not cross the blood-brain barrier, and H1 receptor binding is mostly in the peripheral rather than central nervous system (CNS depression is thus minimal). Astemizole may also act on histamine H3 receptors, thereby producing adverse effects. A piperazine derivative, is a sedating antihistamine that has also been reported to have mastcell stabilising properties. It is used for the symptomatic relief of allergic conditions including urticaria, rhinitis, and conjunctivitis It has anticholinergic and antipruritic effects. Acute dystonic reactions and long-lasting impaired consciousness were associated with oxatomide therapy in 6 children.1 Impaired consciousness varied from lethargy and somnolence to a clinical picture resembling encephalitis and persisted for 2 days or more in 3 patients. It has been reported that this drug might prevent much of the muscle wasting (atrophy) that occurs in immobile, bedridden patients. An experiment on a small number of mice showed that astemizole blocked the activity of a protein present in muscle that is involved in muscle atrophy. However the concerns for the drug's longterm effects on the heart preclude its routine use in humans for this indication. It has been withdrawn from the market in most countries because of rare but potentially fatal interactions with CYP3A4 enzyme inhibitors (e.g. erythromycin, grapefruit juice). Terfenadine second generation antihistamine acts on blood vessels and gastrointestinal and respiratory systems by competing with histamine for peripheral H1-receptor sites; decreases allergic response by blocking histamine formerly used for the treatment of allergic conditions. It was superseded by fexofenadine in the 1990s due to the risk of cardiac arrhythmia caused by QT interval prolongation. cardiac arrhythmia caused by QT interval prolongation. Loratidine second generation antihistamine, closely structurally related to tricyclic antidepressants such as imipramine, and distantly related to the atypical antipsychotic quetiapine Loratadine is a tricyclic antihistamine, which acts as a selective inverse agonists of peripheral histamine H1receptors It helps to relieve sneezing, runny nose, and itchy, watery eyes. This medicine is used to treat the symptoms of indoor and outdoor allergies. It is also used to treat itchy skin rash and hives. As a 'non-sedating' antihistamine, loratadine causes less sedation and psychomotor retardation than the older antihistamines because it penetrates the blood brain barrier only to a slight extent. Although drowsiness is rare at the common 10 mg dose, patients should, nevertheless, be advised that it can occur and may affect performance of skilled tasks (e.g., driving); excess alcohol should be avoided, although an interaction between alcohol and loratadine has not been shown.Other possible side-effects include headache and antimuscarinic effects such as urinary retention, dry mouth, blurred vision, and gastrointestinal disturbances. interaction with other medications such as erythromycin, or foods like grapefruit. The addition of, or dosage change in, these CYP3A4 inhibitors makes it harder for the body to metabolize and remove terfenadine. In larger plasma concentrations, terfenadine may lead to toxic effects on the heart's rhythm (e.g. ventricular tachycardia and torsades de pointes). Substances that act as inhibitors of the CYP3A4 enzyme such as ketoconazole, erythromycin, cimetidine and furanocoumarin derivates (found in grapefruit) lead to increased plasma levels of loratadine. This had no clinically significant effects in controlled trials.