Pharmacy Advisor
advertisement

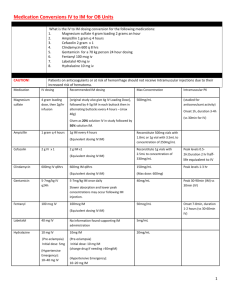
THE PHARMACY ADVISOR A Publication of the Beth Israel Deaconess Medical Center Department of Pharmacy and Pharmacy & Therapeutics Committee Volume 1, Issue 2 August/September 2002 Renal Dosage Guidelines: The 2002 update of the BIDMC Renal Dosage Guidelines is currently available from the Department of Pharmacy. This concise pocket card features general dosage and administration recommendations for common medications that require adjustment in patients with renal dysfunction or renal insufficiency. The guidelines are based on published data from several sources referenced on the pocket card. The renal dose guidelines listed in the pocket card correspond to dose recommendations for renal adjustment in POE. In both cases, it is important to note that while the guidelines serve as a useful reference tool for the majority of patients, patient-specific conditions and clinical circumstances may require dose modification to meet individual patient care needs. Please consult with a unit-based pharmacist to discuss patient-specific medication dosing. Other information found within the Pocket Card includes: Extended-Interval Aminoglycoside Guidelines, useful formulas for calculating Creatinine Clearance; Ideal, Adjusted and Dosing weights for patients; and recommendations for converting select medications from IV to PO. The estimated cost savings for each IV to PO interchange is provided. For copies of the 2002 Renal Dosage Guidelines, contact a unit-based pharmacist or page the clinical pharmacy pager at ext 31195 INSIDE THIS ISSUE 1 2 Renal Dosage Guidelines: Updated 2002 Pocket Card is available from the Department of Pharmacy Formulary Update: Meropenem (Merrem™); Aspirin/Extended-Release Dipyridamole (Aggrenox); Tramadol; Dorzolamide Hydrochloride 2% (Trusopt™); Dorzolamide 2% and timolol 0.5% (Cosopt™); Latanoprost 0.005% ( Xalatan™) 3 Medication Safety: Updated IV Administration Guidelines for Potassium Chloride 5 Kinetics Corner: Phenytoin Medication Use Evaluation: Liposomal Amphotericin (Ambisome™) The Pharmacy Advisor is a publication of the Department Of Pharmacy and the Pharmacy & Therapeutics Committee at the Beth Israel Deaconess Medical Center, Boston, MA 02215 Writing/Editorial Board: Katherine Giampietro, PharmD Christopher McCoy, PharmD Lisa Saubermann, PharmD Diane Soulliard, PharmD Bruce Bistrian, MD, Co-Chair P&T James Heffernan, MD, Co-Chair P&T Francis P. Mitrano, M.S., RPh 6 P&T Formulary Update Meropenem (Merrem) is selected as the preferred carbapenem on the BIDMC Formulary Overview: Meropenem is one of three commercially available carbapenem antibiotics (imipenem-cilastatin, meropenem and ertapenem) available in the United States. Meropenem, like the other agents in this class, is a bactericidal compound that acts primarily by binding to penicillin binding proteins. Meropenem has a very broad spectrum of activity that encompasses Gram negative, Gram positive and anaerobic bacteria. Furthermore, meropenem is impervious to many β-lactamase enzymes. Compared with imipenem-cilastatin, it is somewhat more active against Gram-negative organisms and slightly less active against Gram-positive bacteria. Indications: In addition to it’s FDA-approved indications for intrabdominal infections and bacterial meningitis in patients aged 3 months and older, meropenem’s favorable clinical and microbiologic activity make this agent valuable in the treatment of other infections including: respiratory tract infections, skin and skin-structure infections, urinary tract infections, obstetric and gynecologic infections, septicemia and febrile neutropenia. Meropenem’s primary place in therapy at BIDMC will be in the treatment of suspected or documented serious polymicrobial infections and those caused by multi-drug resistant (particularly Gram-negative) bacteria that are susceptible to meropenem. Dosing: The usual dosage of meropenem in adults is 1 g every 8 hours, administered as an intravenous infusion over 15 to 30 minutes. Dose adjustments are required in patients with renal insufficiency. Please refer to the BIDMC Renal Dosage Guidelines for specific recommendations. Side Effects/Precautions: Carbapenems share a lactam ring with beta-lactam antibiotics and should be avoided or used with caution in patients with hypersensitivity reactions to other beta-lactams. Seizures and other CNS adverse events have been reported during carbapenem therapy. Meropenem is generally considered to be somewhat less epileptogenic than imipenem/cilastatin, though some of these data are based on doses of imipenem/cilastatin that are higher than those currently used. Either carbapenem should be used with caution in patients with a history of or at increased risk of seizures. Dose adjustment is recommended in patients with advanced age and/or reduced renal function especially in patients with known factors that predispose to convulsive activity. Conclusion: Meropenem will be utilized at BIDMC as the preferred carbapenem on formulary. Favorable contract pricing in addition to proven clinical efficacy support this formulary decision. Imipenem/cilastatin will be remain on formulary as an alternate agent. Both carbapenems will continue to require ID approval. The Pharmacy Advisor 1 Medication Safety IV Administration Guidelines for Potassium Chloride Updated The medical literature is replete with citations related to dangers associated with the parenteral administration of potassium. The Institute of Medication Safety (ISMP) places injectable potassium in a category of medications termed as “high-alert medications.” Highalert medications are those that have the highest risk of causing injury and/or adverse patient outcomes when administered improperly. The top five high-alert medications identified by the ISMP are insulin; opiates and narcotics; injectable potassium chloride (or phosphate) concentrate; intravenous anticoagulants (heparin); and sodium chloride solutions above 0.9 percent. The Joint Commission on Accreditation of Healthcare Organizations (JCAHO), recently announced that their National Patient Safety Goals for 2003 would include initiatives to improve the safety of using high-alert medications. Pertinent to the use of parenteral potassium, JCAHO recommends the removal of concentrated electrolytes from patient care units and the standardization and limitation of the number of drug concentrations available in health care facilities. JCAHO further recommends that health care facilities develop special procedures for high-alert drugs using a multi-disciplinary approach. Such procedures would include written guidelines, checklists, pre-printed orders, double-checks, special packaging, special labeling, and education. The BIDMC has established ongoing initiatives to address medication safety, including the use of “high-alert medications.” Past initiatives have included removing concentrated injectable potassium from patient-care areas and more recently a multi-disciplinary committee was convened to review the aforementioned medication safety concerns with the administration of parenteral potassium. Specific goals of the committee were to review the standard concentrations of potassium infusions available within the medical center and to update the BIDMC IV administration guideline for potassium. Key medication safety points from the updated IV guideline are highlighted here. Please refer to the full text IV guideline located on the BIDMC intranet site in the IV Administration Guideline section on the Pharmacy intranet page or in the Medications and IV Administration section of The Manual of Nursing practice. The IV Administration Guidelines for Potassium contains information to assist in the utilization and dosing of parenteral potassium administration. Included in the guidelines are suggested rates for intravenous potassium infusions for patients in both ICU and non-ICU settings. The guidelines are not intended to replace clinical judgment where individual patient characteristics may require modification of the recommendations. Dose: The dose and rate of administration of parenteral potassium is based upon the patient’s clinical condition and serum potassium levels (normal range: 3.5 - 5.0 mEq/L) The maximum daily dose generally recommended is 120 mEq/ 24 hours. Certain patients, due to their clinical condition or concomitant medications, will require potassium supplementation beyond general replacement needs. A total (oral and parenteral) daily dose of potassium ranging up to 240 mEq/ 24 hours may be required in select patients. For example: patients with serious hypokalemia (serum potassium less than 3.0 mEq/L); patients on amphotericin or high dose steroid therapy; patients receiving acute leukemia induction therapy, and others. IV Administration Potassium Chloride concentrate for injection must be diluted with a compatible IV solution prior to administration. Infusion Pump Required: Potassium containing solutions must be administered via an infusion pump. Intravenous Cardiac Monitor Required for potassium infusion rates > 10 mEq/hour in ICU and non-ICU areas. Infusions of potassium in excessive amounts or at an excessive rate can produce adverse effects on the cardiac conduction system. IV administration at controlled rates, via an infusion pump is aimed at minimizing such adverse effects. IV access: Concentration dependent (see specifics below for peripheral and central administration) Potassium chloride injection is a vesicant and pain, venous irritation and/or phlebitis can occur during IV administration of potassium. Limiting the peripheral concentration of potassium will assist in minimizing this adverse effect. Peripheral Administration: Maximum rate: 10 mEq/hr Maximum concentration: 60 mEq/1000 mL Acceptable products: 10 mEq/100 ml bag* 20 mEq - 60 mEq per 1000 mL bag 40 mEq/500 mL ** *10 mEq/100 ml may be hung peripherally and will be stocked in pyxis in inpatient areas. The concentration of this product exceeds general recommendations for peripheral administration of potassium; therefore the number of doses of this particular product should not exceed two in 12 hours. **40 mEq/500 ml is available per MD request for fluid restricted patients with a peripheral line, in which the concentrated 20 mEq/50 ml product is prohibited. Central Administration: Maximum rate: 20 mEq/hr Maximum concentration: 60 mEq/1000 mL Acceptable products: 20 mEq/50 ml bag ¶ 20 mEq - 60 mEq per 1000 mL bag 40 mEq/500 mL ** ¶ 20 mEq/50 ml bags are reserved for patients with a central line who require rapid replacement of potassium for severe hypokalemia. This product is stocked in ICU areas only. The pharmacy will send this product to non-ICU areas for specific patients only. Use in non-ICU areas must be in patients with a central line and cardiac monitoring. The Pharmacy Advisor 2 Kinetics Corner: Phenytoin Formulary Update continued: Phenytoin is a commonly prescribed anticonvulsant agent. Individualization of dosage is aimed at achieving target therapeutic drug concentrations to optimize seizure control while minimizing any potential for adverse effects. Optimal dosing is challenging in some patients and may be related to phenytoin’s unique pharmacokinetic profile. Phenytoin metabolism is dose dependent and elimination kinetics are non-linear. Phenytoin follows first-order kinetics at low concentrations where the amount metabolized is proportional to concentration. At higher concentrations, elimination follows zero-order kinetics, where a fixed amount is metabolized in a given time. This kinetic change reflects a saturation of metabolic pathways. Thus, very small changes in dosage may result in disproportionate increases in serum levels (possibly 3 to 4 fold). The combined pharmacodynamic effect results in considerable inter- and intra- patient variability. Additionally, phenytoin is highly protein bound and changes in albumin or in the binding affinity of phenytoin to albumin (i.e. resulting from concomitant drug therapy or addition of tube feeding) can affect phenytoin serum concentrations. As a consequence of these variables, it is difficult to make predictions regarding optimal therapeutic dosing regimens in some hospitalized patients, especially those who are critically ill or have significant end-organ dysfunction. Several key points relating to phenytoin kinetics are provided here to assist in phenytoin dosing and monitoring. The following medications have recently been approved for addition to the BIDMC formulary Dosing: Phenytoin is available in both parenteral and oral dosage forms and different bioavailability exists for each formulation. Phenytoin chewable tablets and suspension (both 100% phenytoin acid) are immediate-release medications. Both products should be administered in divided daily doses. Phenytoin sodium capsules (92% phenytoin acid) are extended release and can be administered in divided daily doses or as a once-daily regimen. Oral administration of phenytoin is preferred in non-emergent situations. A typical oral loading dose is in the range of 15-20 mg/kg administered in 3 divided doses. The doses are given every 2-4 hours to decrease GI adverse effects and to ensure complete oral absorption. The loading dose is typically followed by a maintenance regimen of 300 mg per day. Adjustments to the daily maintenance regimen should be made in small increments (30-100mg maximum). Monitor serum levels 7-10 days following each dosage FDA Approved change to assess the trend. Steady state is usually achieved after 10-14 days; however, it may be much longer than this in some patients (range 5-30 days.) When rapid parenteral administration of phenytoin is required, IV phenytoin is available. Caution is required with IV phenytoin due to potential cardiac toxicities associated with rapid IV administration including: hypotension, bradycardia, atrial and ventricular conduction abnormalities, and ventricular fibrillation. Additionally, phenytoin injection is highly alkaline and significant venous irritation can occur when administered peripherally via a small vein. The IV loading dose is 15-20 mg/kg administered at a maximal rate of 50 mg per minute. IV maintenance is generally initiated at 100mg IV q8H and further adjusted based on drug levels and seizure activity. Therapeutic Drug Monitoring (TDM): Since phenytoin has a low therapeutic index and exhibits saturation kinetics (i.e. small increases in dose result in large increases in serum drug concentrations), TDM serves as a useful guide to dosage adjustment. It is important to note that blood levels of phenytoin reflect total serum concentrations (bound and unbound drug), however only free, unbound phenytoin, has biological activity. The goal therapeutic concentration during maintenance therapy is 10-20 mcg/ml (total phenytoin) or 1–2 mcg/ml (free phenytoin). Examples of situations when TDM would be appropriate include: during initial therapy to achieve therapeutic serum concentrations; when seizures recur after a period of control; when there is concurrent illness or a change in physiological state exists (pregnancy, hypoalbuminemia, renal failure...) or if drug toxicity is suspected. Protein Binding: Phenytoin is greater than 90% bound to serum albumin, therefore patients with renal or hepatic dysfunction and other disease states associated with hypoalbuminemia may have a higher free fraction of phenytoin circulating in the serum. Free phenytoin levels may be a more reliable means of monitoring phenytoin therapy in such patients. If a free phenytoin level is not available, a corrected phenytoin level can be calculated using the below equation to adjust total phenytoin concentrations for hypoalbuminemia. Corrected Phenytoin = Phenytoin Level (Observed)_______ Level (α x Patient’s Albumin) + 0.1 Where α is: 0.2 for Creatinine Clearance > 30 ml/minute 0.15 for Creatinine Clearance 10- 30 ml/minute 0.1 for Creatinine Clearance < 10 ml/minute Aspirin 25mg / extended release-dipyridamole 200mg capsules (Aggrenox™): is a combination antiplatelet agent intended for oral administration. FDA Approved Indications: Aggrenox™ is indicated to reduce the risk of stroke in patients who have had transient ischemia of the brain or completed ischemic stroke due to thrombosis. Dosing: The recommended dose of Aggrenox ™ is one capsule given orally twice daily, one in the morning and one in the evening. The capsules should be swallowed whole without chewing and may be given with or without food. Aggrenox ™ is not interchangeable with the individual components of aspirin and dipyridamole tablets. ___________________________________________________________ Tramadol: Tramadol is a centrally acting analgesic with dual opioid and nonopioid mechanisms. FDA Approved Indications: Tramadol is indicated for the treatment of moderate to moderately severe pain. Dosing: Adults: Moderate to severe chronic pain: 50-100 mg every 4-6 hours, not to exceed 400 mg/day. For patients not requiring rapid onset of effect, tolerability may be improved with a starting dose of 25 mg/day and increasing the dose by 25 mg every 3 days, until reaching 25 mg 4 times/day. The dose may then be increased by 50 mg every 3 days as tolerated, to reach a dose of 50 mg 4 times/day. Elderly: >75 years: 50-100 mg Q4-6H (not to exceed 300 mg/ day Dosing adjustment in renal impairment: Clcr<30 mL/ min: Administer 50-100 mg dose Q12H (max: 200 mg/day) Dosing adjustment in hepatic impairment: Cirrhosis: Recommended dose: 50 mg every 12 hours BIDMC Restrictions: Tramadol has been approved for addition to the BIDMC formulary without restriction. The combination product (tramadol 37.5mg/acetaminophen 325mg) [Ultracet™] was not approved for formulary status. Prescribers must write separate tramadol and acetaminophen orders when both products are required for patient care. Please note that the tramadol component of Ultracet™ is not commercially available in this dosage strength (37.5mg) and should not be requested as such. Please write tramadol orders in increments of the 50mg tablet as appropriate. ___________________________________________________________ Ophthalmic Class Review: As part of ongoing formulary review process the following products were moved to formulary status: Dorzolamide Hydrochloride 2% (5ml) Trusopt™ Dorzolamide 2% and timolol 0.5% (5 mL) Cosopt™ Latanoprost 0.005% (2.5 mL) Xalatan™ ___________________________________________________________ ___________ The Pharmacy Advisor 3 Medication Utilization Evaluation: Liposomal Amphotericin B Amphotericin B, an intravenous antifungal agent with activity against multiple fungal isolates including fluconazole resistant aspergillus and select candidal species, is uniquely manufactured in four different delivery systems. The newer lipid formulations were developed in the 1990’s in an attempt to reduce the predictable side effects of amphotericin B deoxycholate. In September 2000, the Pharmacy & Therapeutics (P&T) committee approved liposomal amphotericin B (Ambisome) for treatment of fungal infections in patients who are refractory to or intolerant of conventional amphotericin B deoxycholate with associated guidelines for use based on the Infectious Disease Society of America (IDSA) guidelines from the year 2000. Direct cost differences between liposomal amphotericin B and amphotericin B deoxycholate are remarkable. Therapy with liposomal amphotericin B (Ambisome) is approximately $500 per day at a dose of 5mg/kg in a 70 kg patient. A comparative dose of amphotericin B deoxycholate (1mg/kg/day) in this same patient costs $9 per day. A follow up medication utilization evaluation (MUE) was conducted and presented to the P& T committee in July 2002. This evaluation, a retrospective and concurrent chart review, was performed to compare prescribing trends at BIDMC for liposomal amphotericin B (Ambisome) to the evidence based criteria developed by the P& T Anti-infective Subcommittee (see insert). All adult inpatients treated with Ambisome were evaluated for the study period of November 2001 through March 2002 with no exclusion criteria. Sixteen patients were identified and medical records were reviewed for the following indicators: Indication for use Fungal isolates identified Previous therapy with amphotericin b deoxycholate Documented intolerance or history of intolerance to amphotericin B deoxycholate Documented treatment failure with amphotericin B deoxycholate Serum creatinine prior to liposomal amphotericin B therapy Creatinine clearance prior to liposomal amphotericin B therapy Recent rise in serum creatinine of >0.5 mg/dl Initial dose of liposomal amphotericin B therapy The indicators were compared with the approved criteria for use and dosing recommendations to determine congruence. Results of the study demonstrated that the majority of cases were empiric therapy of fever of unknown origin in neutropenic patients (38%) followed by documented Candidemia (19%), Cryptococcemia (12%) and empiric therapy for fever or unknown origin in patients post Bone Marrow Transplant, nonneutropenic. Fungal isolates were identified in 50% of the patients treated. The remaining patients either had no cultures performed or no growth identified. A large majority (87%) were patients who had not been prechallenged with amphotericin B deoxycholate. Of the patients treated previously with amphotericin B deoxycholate (13%), one had a documented previous history of intolerance and none had been classified as a treatment failure. Renal dysfunction, defined as serum creatinine >2.5mg/dL and creatinine clearance <40mL/min was identified respectively in 13% and 50% of those initiated on the liposomal therapy. Recent rises in serum creatinine (>0.5mg/dL) were noted in 25% of patients prior to therapy. Dosing regimens ranged from 2 to 6 mg/kg per day. An analysis of these results revealed the following important summary points. Ten of the sixteen patients (63%) met at least one of the criteria for appropriate use of the liposomal product but six (37%) did not meet any. Guideline based dosing was observed in 75% of those treated and 25% of patients were found to be dosed above these recommended doses. It should be noted, that limitations to this descriptive study may lie in the method of data collection, i.e. by simultaneous retrospective and concurrent chart review, the lack of formal statistical analysis and the small number of patients. It is the recommendation of the P&T committee that prescribers carefully review the BIDMC guidelines prior to initiating therapy with liposomal amphotericin B. Initial trials of amphotericin B deoxycholate with appropriate infusion parameters, premedication and fluid loading are strongly encouraged. Liposomal amphotericin B remains a restricted drug product, subject to approval by an Infectious Disease specialist. Cost consideration for the liposomal product dictate that all doses should be rounded to the nearest 50 mg to maximize unit of use (e.g, 285 mg: round to 300 mg, or 312 mg: round to 300 mg). BETH ISRAEL DEACONESS MEDICAL CENTER PHARMACY & THERAPEUTICS ANTIBIOTIC SUBCOMMITTEE (May 2002) LIPOSOMAL AMPHOTERICIN-B (AMBISOME) GUIDELINES (Note: liposomal amphotericin will be released ONLY with ID approval) CRITERIA FOR USE: Liposomal amphotericin B is indicated for patients with systemic mycoses, who are intolerant of, or refractory to conventional amphotericin B* Amphotericin B intolerance should be defined by: A minimum trial of conventional amphotericin B deoxycholate (example: 0.6mg/kg/day x 5 doses) with An increase of >1.5mg/dl in serum creatinine compared to the baseline prior to amphotericin B therapy, OR Severe or persistent infusion-related adverse events despite premedication or comedication regimens (example: pre and post-dose hydration with saline, acetaminophen, diphenhydramine, meperidine, etc.) Refractory treatment to conventional amphotericin B should be defined by: Disease progression after > 500mg or 7mg/kg total dose amphotericin B (example: 1mg/kg daily dose x 7 doses =7mg/kg total dose) Liposomal amphotericin B without challenge of conventional amphotericin B is reserved for the following patients: Patients with a baseline serum creatinine of >2.5mg/dl; OR Patients with a baseline CrCl of 40ml/min, OR Patients with a rise in serum creatinine > 0.5mg/dL in the absence of rapidly reversible causes (i.e. recent contrast, dehydration, etc.) despite adequate hydration and discontinuation of other nephrotoxins, OR Patients with a history of severe and/or persistent adverse infusion related reactions with conventional amphotericin B, OR Bone Marrow Transplant Patients with febrile neutropenia and/or documented fungal infections DOSING: Liposomal amphotericin B should be dosed by indication as follows: INDICATIONS DOSE(mg/kg/day) Empiric Therapy 3 Systemic fungal infections: 3-5 Aspergillus; Candida; Cryptococcus Visceral Leishmaniasis (immunocompromised patient) 4 (days 1-5) and 4 on days 10,17,24,31,38 empiric therapy for presumed fungal infection in febrile(38C) neutropenic patients Dosage in Renal Failure (SrCr >2.5 mg/dl): (similar to conventional Amphotericin-B) CrCl >10ml/hr dose q24h CrCl < 10ml/hr dose q 24-36h PREMEDICATIONS: Liposomal amphotericin-B does NOT require use of pre-medications, nor pre and posthydration Liposomal amphotericin B does NOT require the use of a test dose MONITORING GUIDELINES: Daily monitoring of plasma K+ , Mg, BUN, creatinine levels, and signs of nephrotoxicity *Practice guidelines for the treatment of fungal infections, Clinical Infectious Diseases, 2000:30; 652-718 http://www.journals.uchicago.edu/CID/journal/issues/v30n4/990664/990664.html This guideline has been designed to assist the clinician in the utilization and dosing of liposomal amphotericin. It is not Intended to replace clinical judgment where individual patient characteristics may require modification of the recommendations. The Pharmacy Advisor 4 The Pharmacy Advisor 5