Colon, Rectum & Anus
advertisement

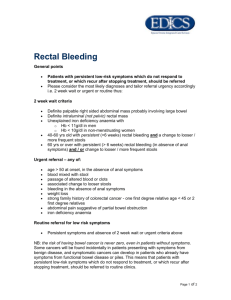
Nem’s Notes… Phase 2 Year 2 GASTROENTEROLOGY 4 (page 1 of 5) Colon, Rectum & Anus Diverticular Disease Diverticulosis Diverticulitis Diverticular disease Diverticula Epidemiology Found more commonly in populations with low intake of dietary fibre. This may be due to small volume stools which require higher intraabdominal pressure for propulsion and may lead to herniation of mucosa. Female preponderance. (Diverticular Disease) Pathology (Diverticular Disease) Clinical Features (Diverticular Disease) Complications (Diverticular Disease) Investigation (Diverticular Disease) Treatment (Diverticular Disease) Presence of diverticula Inflammation of the diverticula General term for disease involving diverticula Protrusions of gut mucosa covered by peritoneum and present in 50% of patients over 50 (a) Protrusions of mucosa covered by peritoneum (b) Hypertrophy of circular muscle (c) Inflammation can result from impaction of faecaliths (d) Repeated inflammation leads to narrowing or obstruction of the lumen (a) Usually asymptomatic (90% cases) (b) May be associated with constipation or spasm (c) Colicky pain in left iliac fossa (d) Can produce rectal bleeding (e) Acute cases present with severe pain and fever (a) Perforation leading to generalised peritonitis (b) Fistula formation into bladder or vagina (c) Intestinal obstruction (a) Blood test may show PMN leucocytosis (b) Spiral CT (c) Ultrasound (d) Flexible sigmoidoscopy (a) Asymptomatic cases require no treatment (b) Acute cases treated with cephalosporin & metronidazole as outpatient (c) Emergent cases may require surgery and bowel resection Colonic Polyps Colonic polyps are protrusions above the colon epithelium and may be epithelial or mesenchymal. Histology (Colonic Polyps) Harmartomatous Polyps Inflammatory Polyps Neoplastic Polyps Hyperplastic Polyps Lymphoid Polyps Large, stalked. Involve granulation due to excess regeneration during inflammatory bowel disease. Can be either tubular or villous. Tubular polyps are small (<10mm diameter), have numerous crypts, mucoussecreting epithelium and are stalked. Villous polyps have elongated villi with columnar epithelium. Elongated crypts without dysplasia and a ‘serrated’ upper surface to the crypts. ? more online at http://homepage.virgin.net/nemonique.sam/noteindx.htm page 1 of 5 Nem’s Notes… Phase 2 Year 2 GASTROENTEROLOGY 4 (page 2 of 5) Colon, Rectum & Anus Clinical Features Most polyps are asymptomatic and found when patients are investigated for other GI tract disorders, such as pain, altered bowel habit, bleeding haemorrhoids etc. (Colonic Polyps) Extraintestinal Features (a) Subcutaneous epidermoid cysts (b) Lipomas (c) Benign osteomas (esp skull and angle of mandible) (d) Desmoid tumours (e) Dental abnormalities (f) Congenital hypertrophy of retinal pigment epithelium (CHRPE) (Colonic Polyps) Risk Factors for Malignancy (a) Large size (>2cm) (b) Multiple polyps (c) Villous architecture (d) Dysphasia (Colonic Polyps) Adenoma-Carcinoma Sequence (a) Activation of Oncogenes (b) Loss or mutation of tumour suppressor genes (c) Defective genes of the DNA repair pathway (d) Genomic instability Colorectal Carcinoma Epidemiology (Colorectal Carcinoma) Risk Factors (Colorectal Carcinoma) Pathology (Colorectal Carcinoma) (a) Rare in the underdeveloped world (b) Common in Western populations (60 per 100,000 UK) (c) Increasing incidence with increasing age (esp >50) Non-Dietary Factors (a) Colorectal adenomas (b) Chronic extensive ulcerative colitis (c) Acromegaly (d) Pelvic radiotherapy (e) Obesity and sedentary lifestyle (f) Alcohol and tobacco use Dietary Factors (a) High red meat & saturated fat (b) Low fibre intake (c) Low fruit/veg intake (d) Low calcium/folic acid intake (a) Arise from an adenomatous polyp (b) >50% in rectosigmoid region (c) Lymphatic invasion common at presentation (d) Metatases to liver through systemic/portal circulation Duke’s Staging (Colorectal Carcinoma) Stage Description % of Cases 5 yr Survival Rate A Tumour confined to bowel wall 10% 90-100% B Beyond bowel wall but no metatases 35% 65-75% C Involving lymph nodes 30% 30-40% D Distant metatases or residual disease following surgery 25% <5% more online at http://homepage.virgin.net/nemonique.sam/noteindx.htm page 2 of 5 Nem’s Notes… Phase 2 Year 2 GASTROENTEROLOGY 4 (page 3 of 5) Colon, Rectum & Anus Clinical Features (Colorectal Carcinoma) Management (Colorectal Carcinoma) Prevention & Screening (Colorectal Carcinoma) (a) Altered bowel habit (b) Rectal bleeding (c) Iron deficiency anaemia (d) Bowel obstruction (e) Weight loss (a) Surgical removal of tumour by resection (b) Adjuvant chemotherapy for stage C colon cancer patients (c) Combination radiotherapy for stage C rectal cancer patients (a) Healthcare agencies advocate low-fat, high-fibre diet (b) Endoscopic screening with polyp removal for families with FAP (Familial Adenomous Polyposis) and HNPCC (Hereditary Non Polyposis Colon Cancer) (c) Possible flexible sigmoidoscopy at age 55 Ischaemic Colitis Caused by insufficient or blocked blood supply to the mesenteric arteries or veins Pathology (Ischaemic Colitis) (a) Anoxic or hypoxic injury depending on adequacy of collateral supply (b) Cell death due to calcium ion movement through damaged membranes (c) Free radical damage on reperfusion with oxygen (in non-occlusive cases) Causes (a) Occlusive (Ischaemic Colitis) (b) Non-occlusive Clinical Features (Ischaemic Colitis) Investigation (Ischaemic Colitis) Complications (Ischaemic Colitis) Treatment (Ischaemic Colitis) (i) Superior mesenteric embolus/thrombosis (ii) Mesenteric vein thrombosis (i) Systemic hypotension (ii) Vasoconstriction (iii) Viscosity disturbances (iv) Arterial narrowing (v) Pharmacological effects (eg digitalis, cocaine) (a) Sudden Abdominal pain (b) Passage of bright red blood with or without diarrhoea (c) Distended abdomen (d) Signs of shock (e) Signs of cardiovascular disease (a) Sigmoidoscopy to rule out bleeding from diverticular disease or ulcerative colitis (b) Barium enema to see characteristic ‘thumb-printing’ on colon wall (a) May develop strictures (b) May develop gangrene (a) Treatment of cardiovascular problems (b) Surgery if required to resect bowel more online at http://homepage.virgin.net/nemonique.sam/noteindx.htm page 3 of 5 Nem’s Notes… Phase 2 Year 2 GASTROENTEROLOGY 4 (page 4 of 5) Colon, Rectum & Anus Megacolon & Megacolon refers to a number of different congenital and acquired conditions where Hirschsprung’s the colon is dilated. Disease Presents in first years of life when an aganglionic segment of the rectum gives rise to constipation and subacute obstruction. Anticholinesterase is increased. Failure of relaxation of the internal sphincter can be treated successfully with surgery. Treatment of megacolon is similar to constipation, but saline wash-outs and manual removal of faeces is sometimes required. Solitary Rectal Ulcer Features (a) Bowel Irregularity (b) Rectal bleeding with the passage of mucous (c) Mainly due to excess straining at stool Management (a) Rectal exam (b) Sigmoidoscopy reveals redness/ulcer 10com from rectal margin (c) Histology is diagnostic – non-specific inflammatory changes (d) Treatment is unsatisfactory. Local steroids may help Melanosis Coli &Pigmentation of mucosa (melanosis coli) caused by surreptitious laxative ingestion Laxative Abuse Commonly seen in young females with anorexia or bulemia. (a) Diarrhoea of high volumes (1 litre per day) (b) Pigmented mucosa (c) Histological rectal biopsy shows pigment-laden macrophages (d) Phenolphthalein laxatives detected by NaOH poured onto stools Faecal Impaction Pruritis Ani Requires manual removal of faeces and care to prevent recurrence Causes Management Haemorrhoids Anal Fissures (a) Soiling of perianal skin (b) Local anal lesions eg infection of haemorrhoids (c) Hydrocortisone creams (a) Hygiene – weak local steroids mixed with antiseptic eg timodine Haemorrhoids are varicosities resulting from the dilatation of internal haemorrhoidal venous plexus and require no treatment if minor. Otherwise treated with topical emollients and high fibre diet. Classification Symptom 1st degree Bleeding only 2nd degree Prolapse at defaecation, but spontaneous return to anal canal 3rd degree Prolapse and requires manual replacement 4th degree Can’t be replaced Anal fissures result in painful defaecation and minor rectal bleeding. They can be treated using local anaesthetic gels. more online at http://homepage.virgin.net/nemonique.sam/noteindx.htm page 4 of 5 Nem’s Notes… Phase 2 Year 2 GASTROENTEROLOGY 4 (page 5 of 5) Colon, Rectum & Anus Anal Abscess & Fistulae Perianal abscesses develop between internal and external sphincters. They usually result from infection. Crohn’s is sometimes responsible. Symptoms include: (a) Extreme perianal pain (b) Fever (c) Discharge of pus Spontaneous rupture may lead to fistulae. Abscesses are treated by surgical drainage and fistulae are laid open with car to avoid damage to the anal sphincters. Faecal Incontinence Causes (a) Faecal impaction with overflow diarrhoea (b) Anorectal (i) rectal prolapse (ii) anal stricture (iii) haemorroidectomy (iv) anal dilatation (v) rectal carcinoma (c) Post childbirth damage to pelvic floor innervation (d) Neurological disorders (i) spinal trauma to S2-4 (ii) spina bifida (iii) multiple sclerosis (e) Senile dementia (f) Congenital abnormalities of anus/rectum (g) Impalement injuries (h) Diabetes mellitus with autonomic involvement Management Treatment for underlying causes is often unsatisfactory more online at http://homepage.virgin.net/nemonique.sam/noteindx.htm page 5 of 5