Browlift
advertisement

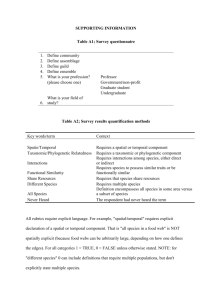
FOREHEAD BROW LIFT INDICATIONS The primary indication is ptosis of the brows and lateral aspect of the upper lid. In addition, the forehead brow lift will help correct: i. Transverse forehead lines ii. Glabella creases iii. Transverse folds at the root to the nose iv. Upper nasal and medial eyelid fullness In some patients, forehead or frown lines are the indication for forehead brow lift. If, once the brow has been lifted, there is still upper lid redundancy, then, in addition, the patient needs an upper blepharoplasty. patients in whom the distance from the midpupil to the top of the eyebrow was equal to or greater than 2.5 cm were not candidates to have their brow raised further. (McKinney) IDEAL EYEBROW POSITION AND CONTOUR (Ellenbogen, 1983) 1. The medial extent of the eyebrow is to a vertical line drawn through the alar base 2. The lateral extent of the eyebrow is to an oblique line drawn from the alar base through the lateral canthus 3. The medial and lateral ends of the eyebrow lie at about the same horizontal level 4. The apex of the brow lies on a vertical line drawn through the lateral limbus 5. The brow arches above the supraorbital rim in women(1cm) and lies at the supraorbital rim in men Measurements Supratarsal crease to upper edge brow =16mm Midpupil to bottom of brow at least 23mm Upper brow to hairline 5cm. ANATOMY (David Knize PRS 2000) Muscles Prolonged hyperactivity of facial muscles causes— 1. Transverse forehead wrinkles - frontalis 2. Brow ptosis- corrugator and orbicularis (lateral) 3. Glabellar wrinkling- corrugator, orbicularis, depressor and procerus Frontalis pulls the eyebrows up - inserts into supraorbital dermis, interdigitating with orbicularis Eyebrow depressors: 1. corrugator supercilli 2. procerus 3. medial head of the orbital portion of the orbicularis oculi 4. depressor supercilli (most superficial) Corrugator supercilli Oblique head - originate from the superiormedial orbital rim, passing thru orbicularis and insert to the dermis at the medial end of the eyebrow, just above the insertion of depressor supercilli. Vertical creases from over-action. Supplied by zygomatic branch Transverse head - originate from the superiormedial orbital rim (6mm from midline), passing thru orbicularis and insert to the dermis just superior to the middle third of the eyebrow (4cm from midline). Moves eyebrow medially – supplied by frontal branch Procerus arises from the UL cartilages and the nasal bones and inserts into the skin of the glabella region. Contraction transverse creases. Supplied by zygomatic branch Depressor supercilli - originate from the superiormedial orbital rim, superficial to corrugator and inserts into medial brow. Supplied by zygomatic branch Medial head of the orbital portion of the orbicularis oculi – inserts into the medial end of brow. Contraction causes oblique lines. Supplied by zygomatic branch Surgical anatomy. Each frontalis muscle originates from forehead galea aponeurotica and interdigitates with the orbicularis oculi muscle, which inserts into the eyebrow dermis. Superficial temporal fascia and temporalis fascia from the temporal fossa become confluent in the area of the zone of fixation (stippled) with galea aponeurotica and periosteum, respectively, from the forehead. The lateral frontalis muscle usually terminates or becomes markedly attenuated along the lateral margin of the zone of fixation, which extends to the temporal fusion line (TL) and the superior temporal line (STL) of the skull. A fibrous band (*) connects the orbital rim and the superficial temporal fascia deep to the lateral eyebrow. The corrugator supercilii (CSM) and procerus(PM) muscles may participate in the mechanism of eyebrow ptosis, with corrugator supercilii contributing to lateral eyebrow ptosis. Courses of the deep division of the supraorbital nerve and the frontal branch of the facial nerve (FB VII) are shown. The inferior temporal line(ITL) forms the margin of temporalis fascia as it inserts into bone. Periorbital and temporal ligamentous attachments with major neurovascular relationships: lateral view. Temporal ligamentous adhesion (TLA), supraorbital ligamentous adhesion (SLA), superior temporal septum (STS), inferior temporal septum (ITS), periorbital septum (PS), lateral brow thickening of periorbital septum (LBT), lateral orbital thickening of periorbital septum (LOT), sentinel vessel (SV), temporal branches of facial nerve (TFN), zygomaticotemporal nerve (ZTN), zygomaticofacial nerve (ZFN). Nerves Supratrochlear nerve in danger during dissection of the corrugator muscle in forehead lifting as it passes thru the muscle. Average distance from the nasion to the frontal notch/foramen - 25 mm bilateral supratrochlear(frontal) notch in 97%; however, 1% possess bilateral foramina, and 2% have a notch on one side and a foramen on the other Supraorbital nerve must be protected during an endoscopic subperiosteal forehead lift by not extending the blind dissection beyond 2 cm of the supraorbital margin. 25% foramen, 70% notch, 5% from multiple foramens Average distance from the nasion to supraorbital notch/foramen 31 mm 2 branches (medial/superficial and lateral/deep) Deep branch travels 0.5-1.5cm medial to superior temporal line between galea and periosteum - terminal branches of this deep supraorbital nerve branch pierce the galea near the coronal suture to supply scalp sensation Superficial branch enters frontalis 2-3cm above supraorbital rim - supply the forehead and up to 3.5 cm of the frontal scalp Also supplies upper lid and nasal root Frontal branch of facial nerve runs across the anterior temporal fossa within superficial temporal fascia before entering frontalis muscle landmarks – 1. runs in a line from 0.5 cm below the tragus to 1.5 cm above the outer upper part of the eyebrow (Pitanguy) 2. 2cm from the bony acoustic meatus (horizontal line) 3. junction of central 1/3 and lateral 1/3 of zygomatic arch or at about 24 mm from the point where the superior border of the zygomatic arch meets the helix. When approaching the region of the superior border of the arch, dissect deep to the superficial layer of the deep temporal fascia cephalad to the arch, proceeding subperiosteally to the caudal border of the arch. This point cannot be overemphasized because the fascial layers fuse at the superior border of the zygomatic arch and the nerve therefore becomes most susceptible to injury at this location. Supplies Frontalis, superior orbicularis, transverse head corrugator, superior end of procerus The temporal and zygomatic branches of the facial nerve pass through the zygomatic arch: 1, temporal branch of the facial nerve; 2, zygomatic branch of the facial nerve; 3, parotid gland; 4, lower aspect of the zygomatic arch; 5, lateral border of the orbicularis oculi muscle; 6, tragus. Sentinel vein (De la Plaza 1991) 5 mm lateral to the frontozygomatic suture line a tributary of the supraorbital vein at the height of the superior orbital rim, draining the temporal region, passing from the subcutaneous layer through the temporoparietal fascia, then through a perforation or attenuation in the deep temporal fascia to the temporalis muscle - the internal maxillary vein The temporal division of the facial nerve is usually found cephalad to the sentinel vein and, at the nearest point, they were a mean distance of 6.4 mm apart. do not use monopolar electrocautery on the sentinel vein itself because of the risk of a conducted thermal injury to the nerve Inadvertent transection of the sentinel vein adds to periorbital bruising, and ligation or occlusion of the vein seems to cause prominent temporal cutaneous veins postoperatively Mechanism of Brow Ptosis (Knize PRS 1996) mechanisms producing eyebrow ptosis has a relatively greater effect on the lateral eyebrow segment. The lateral eyebrow has less support from deeper structures than the medial eyebrow, and the balance of forces acting on the eyebrow selectively depresses the lateral segment. Three forces that act on the lateral eyebrow are 1. frontalis muscle resting tone, which suspends that eyebrow segment medial to the temporal fusion line of the skull 2. gravity, which causes the soft-tissue mass lateral to the temporal line (galeal fat pad) to slide over the temporalis fascia plane and push the lateral eyebrow segment downward 3. corrugator supercilii muscle hyperactivity in conjunction with action of the lateral orbicularis oculi muscle, which can antagonize frontalis muscle activity and directly facilitate descent of the lateral eyebrow. The axis point for these forces is the temporal fusion line of the skull near the superior orbital rim. BROW LIFT History Passot 1919 - elliptical excisions to elevate the brows and diminish crow's feet Passot 1930 - incision above the eyebrows with undermining and excision of excess tissue, with vertical excisions to relieve vertical rhytids 1926 Hunt – coronal incisions both within the hair-bearing scalp and at the anterior hairline and direct excisions within the forehead skin 1950s- measures to weaken frontalis (crosshatching, injecting alcohol in frontal branch) 1962 Gonzalez-Ulloa– complete circumferential forehead/face lifting 1964 Morel-Fatio – partial excision of frontalis 1965 Vinas made the following observations: 1. The inelastic aponeurotic-muscle layer, formed by the frontalis and its extensions adheres to the skin and does not permit free movement of it. Traction on the frontotemporal region with a finger will show this fixation of the skin, as it does not cause the wrinkles to disappear. 2. There are adhesions that prevent free movement of the soft tissues of the supraorbital regions over the bony orbital rims. Unless these adhesions are eliminated, traction from above will not give a permanent lift to the eyebrow 1993 Chajchir first described endoscopic browlifting Surgical Technique 1. Approach 2. Plane of Dissection 3. Type of fixation 4. Aims Restoration of brow position, symmetry and shape Avoid overcorrection and xs elevation of medial brow Classification (Ramirez) Type I: Open, Brow-Forehead Lift with Skin Excision Type II: Full Endoscopic, Brow-Forehead Lift, No Skin Excision Type III: Biplanar Brow-Forehead Lift Approaches Principle: the further the suspension point from the weight attached the less effective the lift 1. Direct browlift - advantage of a direct one-to-one correction of brow ptosis, but the tradeoff is a visible scar. More suitable in men with thicker brow or bald 2. Open browlift i. standard coronal incision ii. modified anterior hairline incision – advantages: maintenance of forehead size, a mechanically efficient lift, a direct attack on wrinkles, and a low incidence of hair loss. iii. Midbrow - Strip of mid-forehead skin excised at frontalis furrow 3. Endoscopic a. Standard (4-5 port – depending on convexity of forehead) i. Subperiosteal dissection to the nasal bones and supraorbital rims, and subsuperficial temporal fascia dissection medially to end at the sentinel vein and inferiorly to the superior edge of the zygomatic arch b. Extended i. extended over the lateral orbital rim, supraperiosteal up to the midborder of the lateral orbital rim. Recommended when the primary goal was elevation of the tail of the brow, as well as the desire to correct crow’s feet and elevate the lateral raphe of the lateral canthus. 4. Limited-incision a. Temporal incision (Knize) b. Transblepharoplasty - Attaching eyebrow flap to superiorly based periosteal flap (browpexy) 5. Combination procedures Plane 1. Subcutaneous direct, removes transverse wrinkles, preserves sensation posterior to incision Decrease flap vascularity, alopecia, poor scars and forehead anaesthesia For older pts with considerable transverse wrinkling, significant brow ptosis, 2nd or 3rd lift, option of shortening or lengthening forehead 2. Subgaleal Rapid, obvious plane, safe, facilitates muscle excision, bloodless Doesn’t allow skin to stretch Eyebrow movement occurs between leaves of galea at orbital rim Dissection in this layer—greatest degree of translation of brow Can start subgaleal and release orbicularis from periosteum or proceed subperiosteal 2cm above orbital rim 3. Subperiosteal Indirect lift Arcus marginalis must be released for elevation (periosteum/septal junction) Maintains natural gliding of forehead tissues by maintaining layer between periosteum and galea / frontalis Ancillary procedures Botulinum injection, fat injection, fat grafting, transpalpebral corrugator muscle resection, subcutaneous forehead rejuvenation, and endoscopic techniques for forehead rejuvenation. Combination with laser used to resect muscles (potassiumtitanylphosphate laser) or CO2 for resurfacing Open Approach (Pitanguy type) Forehead wrinkles and frown lines are marked pre-op. Standard coronal incision for patients with a normal or low hair line and normal to thick hair. The coronal incision is placed 7-9 cm behind the anterior hairline so that after resection, at least 5 cm of hair-bearing scalp remains anterior to the incision. Every 1mm of eyebrow elevation produces 1.5-2mm of retrodisplacement of hairline, 3mm when frontalis is removed. The anterior hairline incision is used for patients with a high hairline(eyebrow to hairline distance >5cm) or thin hair. In the temporal region, it curves round to meet the top of the ear like the coronal incision. The hair is parted in the line of the planned incision and held with elastics. If a facelift is done concomitantly, the incision continues pre-auricularly. The facelift is usually done first. Infiltration of local with vasoconstrictor. Ocular protection with a corneal shield or contact lens. Incision is parallel to the hair follicles and down to pericranium in one sweep. Dissection is sub-galeal (supra-periosteal), preferably with a scalpel as blunt dissection can cause irregular stripping of the galea and pericranium (ing post-op pain) and can avulse small sensory n branches resulting in anaesthesia and paraesthesia. Laterally, the dissection is just above the deep temporal fascia. STA and vein require ligation since they lie on the STF. Supra-orbital and supra-trochlear vessels and nerves identified and preserved. Using scissors, the dissection continues down the nose. Corrugator is divided close to the bone (leave about half of the muscle attached to the skin to avoid a postop depression in this area. The supra-trochlear nerve bundle normally lies in the corrugator so it must be searched for and protected at the time of corrugator division. Laterally, the flap is dissected down to the lateral orbital rims (level of the zygomatic arches) and the pericranium is incised over the orbital rim to the lateral canthus, releasing the periorbita. Glabella creases are marked from the outside by sticking needles through the skin and an incision is made vertically through the muscle on all 4 sides of the crease down to subcutaneous tissue to release the muscle forming as an island. May need to replace with fat grafts to avoid contour deformity. Frontalis resection serves 3 purposes: 1. Frontalis activity depth of transverse forehead lines 2. Permits greater flap expansion 3. Provides a raw surface for adherence to pericranium which helps stabilise the flap Can be done thru transverse incision only, vertical and horizontal incisions of aponeurosis, strip excision The course of the supra-orbital nerves are marked to prepare for resection of frontalis. A rectangle of frontalis is resected from between the supra-orbital nerves and between the hairline and a line 1 cm above the supra-orbital rim. Small triangles of frontalis can also be excised from lateral to the supraorbital nerves, but these triangles must be located 2 cm or more above the supra-orbital rim to spare the frontal br. Only muscle must be excised, not subcutaneous tissue, otherwise a depression will result. Re-draping is then done, 3 key sutures are inserted (centrally and laterally above each lateral limbus), excess is excised and closure over a drain The eyelids may not close completely for the 1st 12-24 hrs especially if an upper blepharoplasty has been done and so ocular protection is important. COMPLICATIONS Haematoma Less common than with facelift. The 2 main areas warranting caution are i. Medially at the root of the nose ii. At the skin edges. Alopecia Predominantly due to tension. Stretched scars will result in visible scar aloplecia. Frontal br Injury Rare. Can be transient d/t stretching or can be cut during dissection. Often the nerve can be seen laterally on the deep surface of frontalis entering it. Sensory Alterations Anaesthesia invariably occurs posterior to the coronal incision. Temporary losses can occur in the forehead, often associated with itching. Be aware of supraorbital and supratrochlear nerves Skin necrosis Asymmetry Of eyelids or eye brow Abnormal soft-tissue contour Especially after glabellar resection Lagophthalmos Usually occurs during the first 24 hrs, especially if concurrent blepharoplasty. Careful marking of upper lid skin redundancy is done while the brows are lifted to avoid excess skin excision. Scar Abnormal hair part and visible scar Glabellar fat injections have been reported to cause blindness (into ophthalmic vessels) Endoscopic brow lift . Advantages Avoids a coronal scar with possible hair loss and sensory disturbances. Avoids the “surprised look”. Marking Frown lines; supra-trochlear and supra-orbital bundles; midline of forehead The more curved the forehead, the further forward the incision needs to be Usually 4-5 ports depending on convexity of forehead o 1 central, 2 inline with pupil and 2 on extension of vector from alar—lat canthus Optimal vector of pull of lateral brow (dictates site of temporal incision) - usually from alar base through lateral canthus provides gentle elevation; from oral commissure through lateral canthus provides more vertical pull. Vector may lie between these 2. The temporal incisions should be made over the deep temporal fascia to allow fixation. Positioning Patient prone, head extends to or slightly beyond the head of the table to allow instrument manipulation. Arms at 45o. Head up to allow veins to flatten. Monitor at foot of bed, surgeon at head, scrub nurse on patients R, anaesthetist (L). Anaesthesia LA and vasoconstrictor always given at the incision sites. The supra-trochlear, supra-orbital and auriculo-temporal nerves are blocked. Tumescent technique with a more dilute solution to the entire forehead and anterior scalp. Incisions 1. Midline inverted T, transverse or vertical incision 2 cm behind the hairline. 15-20mm long 2. 2 small temporal incisions. Incisions through all layers to deep temporal fascia. Rollin Daniel advocates 5 incisions For procerus/corrugator myectomy, only the central incision is required. For brow lift, all 5 incisions are made. Parallel to the hair follicles. Either sub-galeal or sub-periosteal plane A sub-periosteal dissection is preferred as the dissection is simple and less bloody. Developing the Optical Cavity If sub-periosteal, blunt dissection (Joseph periosteal elevator) is used to link the 3 incisions as it is easier to lift the periosteum as a unit. Blunt, blind dissection is done with the periosteal elevator to within 1-2 cm of the superior orbital rim and laterally to the anterior temporal crest. For dissection of the subgaleal plane, spreading scissors are best. Dissection continues down to the radix, the central orbital rim and the anterior temporal crests. The elevator is used to lift the areolar tissue off the deep temporal fascia. The temporal incision is through all layers down to deep temporal fascia. Through the temporal incisions an elevator is inserted and the loose areolar tissue is swept off the deep temporal fascia. Laterally, separating this cavity from the mid-forehead cavity, at the anterior temporal crest, is the transition zone. This is divided from lateral to medial – the other way risks undermining temporalis. The temporal cavity should be extended down at least to halfway down the lateral orbital rim. Limited Eyebrow Lift (Knize PRS 1996) Mark vector, usually just lateral to the superficial temporal adhesion line Incision 4.5 to 5.0 cm long and placed about 1.5 to 2.0 cm behind the hairline, generally perpendicular to the selected vector line. Dissection deep to temporal parietal fascia, thru the zone of fixation and in the subperiosteal plane. 2.0 × 3.0 cm window is created in the temporalis fascia to expose temporalis muscle, with the expectation that the temporalis muscle will form a cicatricial adhesion to superficial temporal fascia under the transposed flap and help suspend it. superficial temporal fascia plane within the flap edge is advanced to the level marked preop. The deep surface of the superficial temporal fascia in the posterior scalp wound edge is exposed to this marked level. There the superficial temporal fascia in the edge of the advanced flap is sutured with a mattress 2-0 Vicryl suture or similar material to the posterior superficial temporal fascia. The suture should incorporate the underlying stable temporalis fascia whenever possible to help stabilize the transposed flap position. Flap elevation. After separating superficial temporal fascia planes from temporalis fascia and elevating a subperiosteal forehead flap over the frontal bone, the orbital ligament ( *) is transected to obtain optimal cephalad movement of superficial temporal fascia. This dissection includes release of periosteal attachments from the superior orbital rims. Guarded vertical spreading action with scissors along the course of the supraorbital nerve trunk at the orbital rim frees adjacent periosteal attachments with minimal risk of injury to the nerve. The level of the zone of fixation(slanted lines) medial to the temporal fusion line of the skull(TL) and the area of the superficial temporal fascia (STF) are indicated. 24 The temporal and central cavities are connected above, but in the region of the anterior crest - the transition zone - the frontal br can be at risk and the endoscope should be used. The endoscope is therefore inserted through the temporal incision, endo-elevator through the temporal incision and the transition zone divided down to the lateral brow. The frontal br lies in the roof of the optical cavity. The position of the frontal br must be borne in mind. Using this sub galeal (in the temporal region) and sub periosteal (in the frontal region) approach, the frontal br is usually heralded by the appearance of a prominent vein, the sentinel vein. Deeper plane dissections can be done to the lateral brow: either an intermediate plane dissection between the superficial and deep layers of the deep temporal fascia, or a deep plane dissection deep to the deep layer of temporal fascia, on the temporalis muscle, ie, Gillies lift plane. This last plane is done blind to the arch and lateral orbital rim and facilitates blind dissection of the transition zone. Muscle Resection Simple incision of muscle reconstitutes and excision is therefore recommended. Periosteum is divided with a sharp periosteal elevator. The procerus and corrugator are identified and spread. The fibres are resected by grasping and avulsion rather than by sharp techniques. Care must be taken to preserve the nerves. The presence of subcutaneous fat indicates the end of muscle resection. The edges are tapered. A post-op depression is usual initially, but disappears with subsidence of tumescence. Forehead Fixation Several methods. 1. Posterior undermining of the scalp allows epicranius to elevate the brow (functional brow elevation). 2. External brow fixation: dressings applied to compress the elevated brow to the underlying tissue until it adheres to the deep tissue. 3. Suture fixation laterally to the deep temporal fascia – some remove a window of deep temporal fascia to allow for greater adhesion 4. Screw, staple or suture fixation to bone. Screws are removed in 10 days The greater the size of the cavity created, the more efficient is elevation. Closure Drains advisable T-shaped closure allows removal of some skin. Dog-ears may be excised or surrounding scalp undermined, 2-0 absorbable dermal suture, staples. Steristrips to elevate the brow. Microfoam and compression dressing. 25 Alternative Approaches Existing incisions can be used. Can be done through the temporal part of a facelift incision. Can be done via a transnasal route during rhinoplasty (supplementary central brow incision needs to be done too). Post-op Care Elevate the head for 24 hours. Compression dressing maintained for 1-3 days after which an elastic head band is applied. Complications Hematoma Nerve injuries VII: usually a neuropraxia. supra-orbital, supra-trochlear Dysasthesias (burning, itching) Seroma Alopecia Contour irregularities due to muscle resection Poor cosmetic result Asymmetry insufficient or excess brow elevation recurrence of ptosis.