EMERGENCY DELIVERY
advertisement

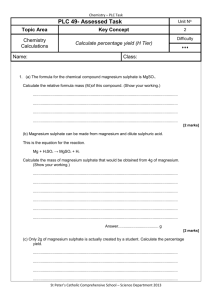
Emergency Delivery Pre-eclampsia / eclampsia EMERGENCY DELIVERY On rare occasions, women in labour may present to the Emergency Department. There are three main groups: 1. Women who have had antenatal care but are from out of town and unaware that there are no obstetric services here. 2. Concealed / denied pregnancy – with no antenatal care 3. In labour with complications e.g. trauma, haemorrhage or eclampsia. The later 2 cases are high risk of themselves and the first is of increased risk because of lack of expertise here. It is desirable to triage the patient to the resuscitation room. ASSESSMENT History LNMP Gestation Antenatal history and carer Previous pregnancies and complications Medial history Medications Allergies Contractions / blood loss / rupture of membranes ? Multiple babies Examination General examination Abdominal examination - Presenting part - Foetal HR (normal 120 – 160) - Lie - Position - Station - Contractions Vaginal examination - Cervical dilation - Effacement - Softening - Position - Station - Presentation attitude - Descent Do not do a PV if any bleeding. Assess via sterile speculum examination. Once assessment is complete, discuss with the obstetrician on call at NWH as the options are: Delivery in ED + obstetric assistance. If cervical dilation is >6cm, position occiput anterior and contractions are regular, delivery is imminent and the patient should not be transferred. Caesarean at Auckland Transfer to NWH If delivery is imminent, paediatric backup can be obtained by paging 777 for a paediatric emergency to resus. If more time is available, liaise with the paediatric medical registrar or consultant. MANAGEMENT OF LABOUR Necessary equipment is in the “baby box” in the resus store room. 1st Stage (Rhythmic contractions 10cm dilated) Observation Maternal vital signs PV loss Contractions Foetal heart rate (120 – 160) CTG if available (not currently) Analgesia Opiates – IV boluses Entonox Reassurance Hydration IV fluids – take blood for FBC, groups and hold Nil orally 2nd Stage (Full cervical dilation to delivery) Continue as above Lithotomy position is easiest for the inexperienced attendant. Control the head, which will rotate as it is delivered. Consider episiotomy: - if going to tear - 10ml 1% lignocaine - right lateral Check for cord when head delivered and remove it from the head. If very tight clamp with 2 cord clamps and cut between. Wipe the face and suction nose and mouth. Deliver shoulders – anterior then posterior by gentle down ward traction. Clamp the cord at 30 seconds. Cut with sterile scissors. Dry the baby and keep warm. See “Neonatal Resuscitation”. Palpate for a second baby. 3rd Stage (Delivery of the Placenta) Give oxytocin - oxytocin 5 units or 5 units IV or - ergometrine 0.25mg IM or - syntometrine (5 units oxytocin + 0.5mg ergometrine) IV Controlled cord traction – 1 hand on uterus other steady pressure on placenta / cord. Rub up the fundus Check the placenta for: - size (15 – 20cm) - thickness (2 – 2.5cm) - weight 500g - calcification - completeness If the placenta has not been delivered in 30 minutes, or there is excessive blood loss (600ml = PPH). manual evacuation in theatre is required. 4th Stage (1st hour) Continue monitoring Clean up the patient, repair any episiotomy or tear if confident, if not place a pack and refer to obstetric registrar. Give fluid Transfer the mother and baby to National Women’s Baby check should be done by paediatric registrar PRE-ECLAMPSIA / ECLAMPSIA DEFINITIONS 1. PRE-ECLAMPSIA Syndrome occurring after 20 weeks of pregnancy with some or all of: Hypertension: > 90mmHg diastolic > 140mmHg systolic > 25mmHg rise Renal impairment - Proteinuria > +1 on dipstick - Generalised oedema Severe pre-eclampsia is defined as the addition of one of the following: Hypertension: Proteinuria: > +3 on dipstick > 5g / 24 hours Olguria: Creatinine: > 0.09mmol/L Neurological symptoms: Pulmonary oedema Liver dysfunction: Haematological dysfunction: - Thrombocytopaenia - DIC - Haemolysis > 110 diastolic > 160 systolic <500mls / 24 hours <30mls / hr - Persistent headache - Visual disturbance - Hyper-reflexia with clonus - Agitation / confusion - Right UQ pain - Elevated bilirubin - Elevated transaminases 2. HELLP SYNDROME Syndrome of haemolysis. Elevated liver enzymes and low platelets. 40% develop DIC. Other complications include intrahepatic haemorrhage, subcapsular haematoma formation and liver rupture. 1/3 if cases are diagnosed post-partum. 3. ECLAMPSIA Seizures occurring after 20 weeks of pregnancy. They may occur postpartum. MANAGEMENT Following standard emergency resuscitation, specific management aims to control hypertension and seizures. General Management Left lateral decubitus position or supine with wedge ABC’s Monitor - Maternal BP, ECG, Sa02, pulse, urine output. Consider arterial line and CVP - Foetal HR Discuss with the NWH obstetric physician on call as soon as practical. SPECIFIC MANAGEMENT 1. 2. Seizures (eclampsia) / severe pre-eclampsia The anti-convulsant of choice is magnesium sulphate – see “Magnesium Sulphate Infusion”. Uncontrolled seizures require standard seizure management, which may include phenytoin or intubation and barbiturate infusion. Delivery is indicated once the patient is stable. Usually the patient can be stabilised for transport to National Women’s. Hypertension Treatment aims to maintain placental blood flow whilst preventing maternal complications: Treat: Systolic >160mmHg Diastolic >110mmHg Reduce to 130 – 130mmHg Reduce to 95 – 100mmHg The agent of choice is: Hydralazine - Direct arteriolar vasodilator. Improves placental flow. - 5mg IV bolus then infuse at 2 – 20mg/hour There is no evidence that one other anti-hypertensive is better than another however a B-blocker may be needed to control the tachycardia induced by hydralazine or if hydralazine is inadequate in controlling the BP. Labetolol Non selective beta-blocker. Does not decrease placental flow. - 10mg IV bolus then infuse at 1 – 2mg/min NB: Magnesium sulphate is also an anti-hypertensive agent and may be adequate on its own Coagulopathy Standard management i.e. Vitamin K; FFP REFERENCES: 1. Duley L; Gulmezaglu A.M; Henderson-Smart D.J. Anticonvulsants for women with pre-eclampsia. (Cochrane Review) In : The Cochrane Library Issue 3, 2000. Oxford : Update Software. 2. Duley L; Henderson-Smart D.J. Drugs for rapid treatment of very high blood pressure during pregnancy. (Cochrane Review) In : The Cochrane Library Issue 3, 2000. Oxford : Update Software. 3. Duley L; Henderson-Smart D.J. Magnesium sulphate versus diazepam for eclampsia. (Cochrane Review) In : The Cochrane Library Issue 3, 2000. Oxford : Update Software. 4. Duley L; Henderson-Smart D.J. Magnesium sulphate versus phenytoin for eclampsia. (Cochrane Review) In : The Cochrane Library Issue 3, 2000. Oxford : Update Software. MAGNESIUM SULPHATE INFUSION Indications: The indications for use of magnesium sulphate infusions are: Eclamptic seizure Or Pre-eclampsia with: Persistent severe headache, or Repeated visual disturbance, or Hyper-reflexia with more than 2 beats of clonus, or Agitation or confusion Special Precautions: Special precautions need to be taken with the following conditions: Myasthenia Gravis or other neuromuscular disorder Cardiac disease - arrhythmia or cardiomyopathy Current drug therapy - lithium - aminoglycoside (gentamicin) - paralysing anaesthetic agents Renal impairment urine output <30ml/Hr creatinine >0.08 In these patients, toxicity is a major risk and the Obstetric Physician should be consulted before magnesium sulphate is used. An alternative anticonvulsant (e.g. phenytoin) may be more appropriate. DOSAGE AND THERAPEUTIC GOAL Therapeutic Goal: 1. To eliminate clonus 2. Therapeutic range = 2.5 – 3.5 mmol/L Dosage: MgSO4 comes in 5ml ampoules containing 10mmol = 2.54g Step 1 Action Loading 5g (20mmol) intravenously over 20 minutes (2x5ml amps) in 100ml of 0.9% normal saline by infusion pump over 20 minutes. Mix well. 2 Maintenance Follow immediately by a maintenance infusion of 1.5g (6mmol)/hr i.e. 10g (40mmol) (4x5ml amps) into 80ml of 0.9% normal saline making a total volume of 100ml / (withdraw 20ml from 100ml bag of base fluid first). Mix well. Concentration = 0.1g (0.4mmol)/per ml. 1.5g (6mmol)/hr = 15ml/hr 3 The loading dose may be accompanied by flushing, nausea and vomiting. Give Maxolon 10mg IV as a slow bolus if required. 4 5 After one hour of infusion check the serum magnesium level. If serum magnesium level is sub therapeutic give a further loading dose by infusion pump over 20 minutes. Serum Magnesium Dose over 20 minutes <1.8 2.5g (10mmol) over 20 minutes 1.8 – 2.2 1.25g (5mmol) over 20 minutes >2.2 nil Then continue maintenance infusion 6 Repeat serum assay 2 hourly until a stable therapeutic level is reached i.e. constant serum level over 2 assays 2 hours apart on the same infusion rate. If the therapeutic goal is not achieved with this regimen seek the advice of the Obstetric Physician 7 8 Measure the serum creatinine at the same time as each magnesium level. Magnesium sulphate infusion is continued for a minimum of 24 hours post delivery. MONITORING OF MAGNESIUM SULPHATE INFUSION Goal The goal of clinical monitoring is to avoid magnesium toxicity. Maternal The following table describes maternal monitoring of magnesium sulphate infusion. Step Recordings ½ hourly Laboratory Tests Monitor Tendon reflexes BP Oxygen saturation Urine Output Serum magnesium Finding Absent or reduced <110/70 <95% <30ml/hr x 2 <2.1 >3.5 Action Stop infusion. Consult Obstetric Physician immediately Continue as per protocol Stop infusion. Consult Obstetric Physician immediately Continue as per protocol Serum Creatinine <0.08 >0.08 Stop infusion. Consult Obstetric Physician immediately Once a stable therapeutic level is reached without evidence of toxicity, monitoring may be relaxed to 2 hourly. Foetal Recordings Step Foetal monitoring should be performed per obstetric instructions Magnesium Sulphate Effects Magnesium sulphate may reduce variability and increase length and frequency of non-reactive cycles. Magnesium sulphate will not alter baseline rate nor produce decelerations. Any such changes are suggestive of hypoxia and should be managed according to usual obstetric criteria. A 60 minute baseline CTG prior to magnesium sulphate loading is useful but should not delay appropriate magnesium loading. TOXICITY AND ANTIDOTE Toxicity Toxicity is usually seen in the context of renal impairment. Magnesium causes an osmotic diuresis; therefore an “adequate” urine output alone is not indicative of adequate renal function. It is essential to measure the serum creatinine at regular intervals i.e. with each serum magnesium level. Symptoms of Toxicity The following symptoms may indicate toxicity: - Absent reflexes Hypotension, vomiting, flushing, drowsiness, slurred speech Respiratory depression / arrest Cardiac arrhythmia / arrest Note: Toxicity is a clinical diagnosis. Serum magnesium levels associated with toxicity are variable but always >4mmol/L. Minor toxic symptoms may be seen at lower levels. Management of Toxicity ABC’s Calcium gluconate 1g (1 x 10ml amp) in 100ml 0.9% normal saline over 20 minutes The antidote reverses the anticonvulsant effect and therefore seizures may be precipitated. Alternative anticonvulsants should be considered during reversal. REFERENCE Magnesium Sulphate Infusion. Clinical Procedures Manual. NWH April 1998.