1 - CANO-ACIO
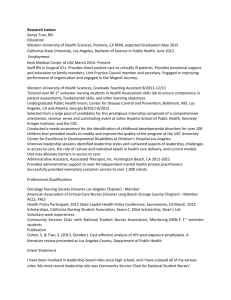
advertisement

CANO 2005 Conference Keynote Presentations Keynote I Life in the Balance Kendrick Lacey, MD Author, “Flu Shot” Ever get the feeling that life is leaving you behind? Ever snap at your spouse or friend for something that’s actually your own fault? Ever want to run away to a deserted island? Ever feel that even one more tiny request for your time, will drive you to scream into your purse, or will leave you drooling on the floor? Dealing every day with cancer and death, suffering and despair, demands and deadlines, can leave us all with our own sanity hanging by a thread. We cannot provide the best possible care for those who depend on us, unless we are able to weather the emotional storm that threatens to wash us away; and that storm is there, if not today then tomorrow. Your own well being, your own professional career, and in some cases your own life may hang in the balance. There is no guaranteed, certified cure for the stresses that bellow at us from behind every demand in our lives; but adding a little balance in your life can buoy you up when you’re feeling swamped. ************************************************* Avez-vous jamais l’impression que le train de la vie vous a laissée en route? Avez-vous déjà manqué de patience envers votre époux ou un de vos amis pour quelque chose dont vous étiez en fait responsable? Vous arrive-t-il de vouloir vous enfuir dans une île déserte? Sentez-vous parfois que si quelqu’un exigeait une partie aussi infime soit-elle de votre temps, vous alliez exploser et « péter les plombs »? Faire face, jour après jour, au cancer, à la mort, à la souffrance et au désespoir, aux demandes et aux échéances, peut nous laisser à deux doigts de devenir complètement fous. Nous ne pouvons pas fournir des soins optimaux aux patients qui dépendent de nous à moins d’être capables de tenir le coup face à la tempête affective qui menace de nous submerger. Et si cette tempête n’est pas là aujourd’hui, elle pourrait fort bien l’être demain. L’équilibre peut se rompre et votre propre bien-être, votre propre carrière et, dans certains cas, votre propre vie peuvent être en jeu. Il n’existe aucun remède garanti à 100% pour les stresseurs qui se cachent derrière chacune des demandes dont nous sommes assaillis dans la vie. Mais en ajoutant un peu d’équilibre à votre vie, vous vous sentirez maintenue à flot lorsque vous avez l’impression d’être emportée par le courant. Keynote II Nursing Presence: a Powerful Imprint Presented by Sue Ness on behalf of Beth Sparks, RN, BScN, MN Have you ever wondered why it is that you really connect with certain people and that you may meet them years later and they will remember you and say something like: “I never forgot you: you made such a difference in my life when I was sick”. As a nurse and a consumer of health care, I have had the privilege of being cared for by nurses who have left a lasting imprint in my heart, mind and soul. It was not what they did for me but how they did it during the provision of care. This leads me to conclude that it is not the tasks we do for individuals in health care that make a difference to them but rather, the way we are with them when we carry them out. Illness usually makes us reassess our priorities in life and see things from a different perspective. “The death rate is very low from dust on the piano”, is one of my favorite new expressions and serves me well as I undergo chemotherapy and continuing health challenges. Humor is an integral part of living and has amazing healing properties, to which we can all attest. I will share with you, nursing strategies, which can make a profound difference to individuals as they navigate the health care system. I will also touch on the comments of your planning committee “that time can erase many things, but it can never erase the caring and enduring friendships we share with others”. ************************************* Vous êtes vous déjà demandé pourquoi il arrive qu’un contact étroit se noue entre vous et certaines personnes dès que vous vous rencontrez pour la première fois et que quand vous les revoyez plusieurs années plus tard, elles se souviennent très bien de vous et vous disent : «Je ne vous ai jamais oubliée; vous avez fait une telle différence pour moi lorsque j’étais malade.» En tant qu’infirmière et que consommatrice de soins de santé, j’ai eu le privilège d’avoir été soignée par des infirmières qui ont laissé leur marque durable dans mon cœur et dans mon âme. Lorsqu’elles dispensaient les soins, ce n’était pas ce qu’elles faisaient pour moi qui comptait, mais bien la manière dont elles le faisaient. Cela m’amène à conclure que ce ne sont pas les tâches que nous effectuons pour le compte de nos clients qui font une différence pour eux, mais plutôt la manière dont nous nous comportons avec eux lorsque nous les accomplissons. «Le taux de décès dû à l’accumulation de poussière sur le piano est très bas» est une des nouvelles expressions que je me suis inventées, que j’affectionne et qui me sont des plus utiles au moment de subir mon traitement de chimiothérapie et de faire face à mes défis de santé continus. L’humour fait partie intégrante de la vie et il possède d’incroyables propriétés curatives, et je suis là pour le prouver. Je vais partager avec vous des stratégies infirmières qui peuvent faire une immense différence pour les personnes qui cheminent à travers le système de soins de santé. Je vais également aborder le commentaire de votre comité organisateur selon lequel « le temps efface bien des souvenirs, mais il ne peut pas effacer la sollicitude et les amitiés durables que nous partageons avec les autres. » Keynote III The Images of Oncology Nursing: A Lasting Imprint Nancy Guebert RN, BSN, MCEd It has been said that nursing is a powerful experience that is based upon the interactions between the nurse, the patient and the family. It is the time when we give our best each and every day; where we experience moments of inspiration and innovation. It is through the teachings of our patients and families that we are taught many valuable lessons and where we are given the tools that we need everyday. It is where we find and experience the meaning of courage and strength; where the purpose of oncology nursing is made real. It is through these interactions that we create the images of oncology nursing. Utilizing art and music and based upon my personal journey as an oncology nurse, a lasting image of oncology nursing will emerge with the hope that it will be forever imprinted on our hearts and minds. ****************************************************** On dit parfois que les soins infirmiers constituent une expérience forte qui repose sur les interactions entre l’infirmière, le patient et les proches. Ce sont les moments où nous donnons le meilleur de nous-mêmes jour après jour; lorsque nous éprouvons des moments d’inspiration et faisons preuve d’innovation. Nos patients et les membres de leur famille nous permettent d’apprendre de précieuses leçons et nous donnent les outils dont nous avons besoin chaque jour. C’est auprès d’eux que nous trouvons le sens des termes « courage » et « force » et que nous les éprouvons; c’est auprès d’eux que la raison d’être des soins infirmiers en oncologie se concrétise. C’est par le biais de ces interactions que nous créons les images des soins infirmiers en oncologie. Je vais faire appel à des oeuvres artistiques et musicales et mettre à profit mon cheminement personnel à titre d’infirmière en oncologie pour faire naître une image durable des soins infirmiers en oncologie en espérant qu’elle restera gravée dans nos cœurs et nos esprits. 2 17th Annual National CANO Conference · Moncton · October 2-5, 2005 Abstracts WORKSHOP I BULLYING AND INTIMIDATION IN THE WORKPLACE – HOW TO RECOGNIZE AND HOW TO RESPOND WORKSHOP II (Abstract 1 of 3) HELPING CANCER PATIENTS MANAGE FATIGUE: CASE ILLUSTRATIONS Patricia Benjaminson, RN, CON(C); Kristie Morydz, RN, BN, CON(C); CancerCare Manitoba, Winnipeg, Manitoba Lois Dumenko-Russell, RN, BN, CON(C); Terry Kelly, RN, BScN, CON(C); Tom Baker Cancer Centre, Calgary, Alberta Nurses are increasingly aware of the detrimental and long lasting effects of workplace bullying. “(Bullying) affects staff absenteeism, turnover, productivity and morale, as well as patient care.” (Sweet 2005) Nurses who are subjected to intimidation and bullying become poor advocates. Some may even leave the profession of nursing altogether. Workplace bullying can affect the meaningful relationships that are important to job satisfaction. Ultimately the patients and families can be affected by poor job satisfaction, as it results in lack of job interest and loss of experienced staff. Randle (2003) states, “A clear relationship exists between nurses’ self-esteem and the delivery of patient care” (p. 400). The difficulty with bullying in the workplace is two-fold; those who experience the behavior do not report or confront the problem and those who are witness to it turn a ‘blind-eye’ (Jackson, Clare & Mannix, 2002). Job satisfaction and reduced workplace stress are important factors in the retention of nurses. In oncology particularly, there is a lack of experienced oncology nurses and retention of nurses and ensuring job satisfaction should be a priority. Sengin (2003) states, “relationships with co-workers and supervisors, team work, as well as collaboration with physicians in decision-making about patient care are important correlates of job satisfaction” (p. 317). The first anti-bullying law in North America came into effect in June 2004 when Quebec amended its Labour Act to deal with psychological harassment in the workplace. The Commision des norms du travail states “one in ten Quebec workers has been the subject of harmful bullying, intimidation or belittlement by a boss or co-worker”. (Canada Safety Council 2004) This workshop will explore how to recognize bullying and its consequences. We will discuss the nurses’ process of working through and recovering from bullying and the impact on the workplace environment and nursing morale. We will explore the tools required to conquer the ongoing detrimental behaviour that continues through each generation of nurses. Fatigue is the most prevalent symptom during cancer therapy and many oncology patients experience post treatment chronic fatigue for months or years following therapy. Case studies of typical oncology patients will be discussed including their fatigue presentation, interventions and outcomes. The first case discusses the situation of a 45 year old female breast cancer patient on FEC chemotherapy. This patient experienced excessive severe fatigue during chemotherapy due to negative lifestyle changes, which accompanied her reaction to her breast cancer diagnosis. The second case presents a 53 year old male with chronic fatigue two and a half years following allogeneic blood stem cell transplant for diffuse large cell lymphoma. The third case profiles a 76 year old female with multiple myeloma who had been unable to leave her home for one year due to severe, debilitating fatigue. Symptom screening tools, including the Brief Fatigue Inventory and the Edmonton Symptom Assessment Tool, will be used to demonstrate initial symptom assessments and outcomes. These cases illustrate the variety of patient fatigue presentations and the severity of the impact of fatigue for people with cancer. Patient reporting and the use of symptom assessment tools, demonstrate the effectiveness of nurse provided fatigue management education and strategies for cancer patients. WORKSHOP II (Abstract 2 of 3) BUILDING TOWARDS THE FUTURE: A NURSE FATIGUE CLINIC RUN WORKSHOP II (Abstract 3 of 3) AND YOU THINK YOU’RE EXHAUSTED: MANAGEMENT FOR CANCER PATIENTS FATIGUE Lois Dumenko-Russell, RN, BN, CON(C); Terry Kelly, RN, BScN, CON(C); Tom Baker Cancer Centre, Calgary, Alberta Lois Dumenko-Russell, RN, BN, CON(C); Terry Kelly, RN, BScN, CON(C); Tom Baker Cancer Centre, Calgary, Alberta For many years in oncology fatigue was accepted as a part of the cancer experience. As more patients were cured, and cancer was recognized as a chronic disease, improved symptom management was crucial to quality of life. Comprehensive pain and symptom control clinics have been developed over the last two decades but until recently fatigue was the forgotten symptom. Fatigue has been recognized as the most distressing symptom in people with cancer impacting the physical, emotional, cognitive, financial and social aspects of patients’ lives. Patients most affected include those with excessive fatigue experienced with cancer treatments, post treatment chronic fatigue and those with moderate to severe symptoms contributing to fatigue such as anemia, insomnia, depression and deconditioning. A nurse run Fatigue Management Clinic has been developed to assist patients experiencing cancer related fatigue to manage and minimize their fatigue by providing comprehensive assessments, interventions and follow up care. Our Fatigue Management Clinic will be presented including the program purpose, the Nurse Coordinator role, referral pattern to the program, patient statistics, areas of intervention and future directions. Oncology nurses are the best health professionals to utilize evidence-based practice to assist oncology patients to manage fatigue, recover from cancer therapy and/or learn to live with chronic disease. Fatigue is now recognized as the leading symptom requiring management in oncology care. Patients report fatigue to be the most distressing symptom associated with cancer and it’s treatment, more distressing even than pain or nausea and vomiting, which, for most patients can be managed with medication (Ashbury et al, 1998). Fatigue though remains a symptom often unaddressed. The NCCN Practice Guidelines (2004) defines cancer related fatigue as an unusual, persistent, subjective sense of tiredness related to cancer or cancer treatment that interferes with usual functioning. Fatigue is nearly a universal symptom with cancer treatment and for patients the manifestations of cancer related fatigue are numerous. The Winningham Psychobiological-Entropy Model of Functioning demonstrates the complexity of fatigue in people with cancer. This presentation discusses how cancer patients describe their fatigue, the impact on patients, factors contributing to fatigue, a comprehensive fatigue assessment and nursing interventions to assist patients to handle their fatigue and maximize their wellness. WORKSHOP III CANO RESEARCH COMMITTEE WORKSHOP WORKSHOP IV SEXUAL HEALTH IN BMT Learning how to read and appraise the value and clinical significance of research for clinical practice Joan Hamilton, MScN; Deborah McLeod, RN, MN, PhD; Capital Health QEII Cancer Care Program, Halifax, Nova Scotia Michelle Lobchuck1, RN, PhD; Natasha Murdoch2, RN, BSN, CON(C); 1 Faculty of Nursing, University of Manitoba; 2 Nursing Education Program of Saskatchewan, SIAST Kelsey Campus, Saskatoon Cancer and its treatment have the potential to severely impact how a person experiences him or herself as a sexual being. Such changes may have profound implications for physical and psychosocial wellbeing. One treatment that commonly impacts all aspects of sexual health is blood and marrow transplantation (BMT). Studies suggest that many patients and their partners want help with this area of their experience but hesitate to ask. Health professionals often do not raise the questions, expecting that patients will raise the issues if they have concerns. The result may be a conspiracy of silence with neither patients nor health professions raising sexual health issues. Health professionals also identify a sense of uncertainty and lack of skill in talking with patients and their partners about their sexual relationship. The purpose of this presentation is to provide oncology nurses with beginning appraisal skills in reading research literature and evaluating study recommendations for their value in changing clinical practice. In particular, as part of evaluating research studies, critical issues to address when considering the use of study recommendations in clinical practice will be considered. For example participants will consider whether the results are impressive considering the risks and costs to patients, meaning and value to patients, relevance to one’s own clinical population, safe and effective use of the recommended change in practice, as well as organizational, logical, financial, or time barriers. As a basis for discussion, participants will be asked to read and appraise both a quantitative and qualitative research article using a reference provided by the facilitators. WORKSHOP V (Abstract 1 of 2) DEVELOPING AN INTRASPINAL ANALGESIA PROGRAM FOR COMPLEX CANCER PAIN IN TERTIARY CARE AND COMMUNITY SETTINGS Cindy Shobbrook, RN, MN, ACNP, CON(C); Allyson Clarke, RN, MSc(A); Princess Margaret Hospital, University Health Network, Toronto, Ontario Intraspinal analgesia (IA) is routinely used to manage procedural pain in acute-care settings however, it is rarely used to manage complex cancer pain in the home setting. An IA program was established at a tertiary cancer center to enable patients to live at home with acceptable pain control. This workshop is designed to address some of these gaps. We plan to focus on both content and skill development. Participants will have the opportunity to discuss the current literature regarding the physical and psychological sexual health changes that can occur with transplant, along with the interventions that may be useful. Teaching guidelines will be reviewed with copies provided to group participants. The second half of the workshop will focus on skill development with dyadic and small group exercises. Case examples will be presented for practice and discussion. Topics addressed will include such issues as maintaining intimacy and a satisfying sexual relationship in the face of physical and psychosocial constraints, dealing with anxiety, lack of desire, dyspareunia, menopausal symptoms and body image. The emphasis will be placed on opening up conversations that allow assessment of the difficulty to occur and providing sexual health education. A selected bibliography for further reading list will be provided. WORKSHOP V (Abstract 2 of 2) LEARNING FROM TRAGEDY: PRACTICE RISK ISSUES FOR INTRASPINAL LINES AND COMPLEX CANCER PAIN Cindy Shobbrook, RN, MN, ACNP, CON(C); Princess Margaret Hospital, Toronto, Ontario This presentation examines the use of intraspinal analgesia as a novel modality to control complex cancer pain and explores challenges in achieving effective communication around patient care between tertiary and community settings. Through examination of a case study involving the untimely death of a patient, this presentation explores critical issues in communication. The IA program evolved in three stages. The first included establishing identification criteria for patients with complex pain. Admission to a tertiary cancer centre in Toronto facilitated catheter insertion and adjustment of intraspinal medications. This stage necessitated development of an IA education program for nurses. The second stage involved developing and coordinating community resources to monitor and support patients after discharge. Liaison with community stakeholders involved negotiating commitment from regional providers early in the assessment process so that upon discharge, patients could access specialized care in the home. The third stage arose from increasing IA patients cared for in the community resulting in regional dialogue with home health care, emergency medical service and community hospital providers to respond to IA complications. In November 2004, a woman with metastatic cancer and intractable pain was admitted to a large cancer center for insertion of an intrathecal catheter to control pain. Following an uneventful 10-day admission, she was discharged home with support of skilled nursing and medical personnel. Two weeks later, she died in her local community hospital -- not from progressive disease or complications with the catheter or infused medication, but from misidentification of the intrathecal line. The autopsy report disclosed cause of death to be from infusion of intravenous fluids and anti-seizure medications into the intrathecal line. Clinical documentation from community, emergency medical service, and community hospital providers identified the intrathecal line to be one of epidural, intravenous, and central venous, and intravenous origin. With planned coordinated teamwork, tertiary and community care providers can achieve acceptable cancer pain control with IA in the home setting and respond to complications as they arise. In reviewing this case study, opportunities for enhancing systems of communication, education and coordination of tertiary and regional resources will be examined. WORKSHOP VI ACHIEVING QUALITY IN CANCER CARE: MEETING THE CHALLENGES OF IMPLEMENTING CANO STANDARDS AND COMPETENCIES IN NURSING PRACTICE Doris Howell1, RN, PhD; Lynne Penton, RN, MN, CON(C); Shari Moura, RN, MN, CON(C); 1University Health Network, Toronto, Ontario Standards of practice are increasingly viewed as important for ensuring patients and their families receive consistent high quality care. The Canadian Association of Nurses in Oncology Standards of Care for Individuals and Their Families: Roles and Competencies were found in an environmental scan conducted by the Canadian Strategy for Cancer Control to meet all the principles of the Alpha International Principles for Health Care Standards (ISQua, 2004; Canadian Council on Health Services Accreditation, 2004). Yet, many cancer care organizations have not yet implemented the CANO standards and competencies. Implementing standards in organizations and facilitating their application and uptake into practice can be extremely challenging. This workshop will focus on pragmatic evidence-based strategies for implementing change in practice settings using the standards as a model for application of the techniques. At the end of the workshop session learners will be able to: (1) demonstrate increased knowledge of the CANO standards and their use in facilitating high quality cancer care; (2) apply specific practical and evidence-based strategies for implementing practice change using the Standards as the model; (3) introduce a conceptual model that allows participants to visualize how the standards and competencies link to the roles of generalist, specialist and advanced oncology nurses. SCHERING / CANO LECTURE TOUCHED BY A NURSE: THE IMPRINT OF EXEMPLARY ONCOLOGY NURSING CARE HELEN HUDSON LECTURE LEAVING OUR IMPRINTS: AN EXPLORATION THERAPEUTIC NURSE-PATIENT RELATIONSHIP Beth Perry, RN, PhD; Athabasca University, Edmonton, Alberta Cathy Kiteley1, RN, MSc, CON(C), CHPCN(C); Dorothy Vaitekunas2, RN, MN, ACNP, CON(C), CHPCN(C); 1 Credit Valley Hospital, Mississauga, Ontario; 2 Mount Sinai, Toronto, Ontario This research based presentation examines the relationship between exemplary oncology nursing practice and professional fulfillment. What inspires nurses to choose oncology and subsequently what gives them impetus to continue in this field? To answer this question, oncology nurses were invited to recall moments in their careers when they were satisfied that they had chosen the “right” career. Data, in narrative form, were collected through an innovative online research technique called web-based narrative exchange. Submissions were analyzed using three approaches, narrative analysis (Priest, Robert & Woods, 2003), poetic interpretation (van Manen, 1990) and photovoice (Woolrych, 2004). This multi-level analysis using stories, poems and photographs furnishes evidence and provides a participatory means of sharing intimate human experience. Findings reveal that oncology nurses who provide excellent care, and make strong connections with their patients, are also usually very well satisfied with their careers. Specifically, nurses provide exemplary care and report attaining professional fulfillment when they achieve connection, affirm value, enable hope and help patients finding meaning. These themes, along with the overarching theme of joint transcendence are described in this presentation. Perhaps this talk will reawaken memories of similar experiences thus enhancing confidence, self-esteem and energy in the nurses present affirming in them that they are unquestionably leaving an imprint. INTO THE Oncology nursing aims to promote physical and psychosocial well-being of individuals and families at risk for, or living with a life threatening illness. A basic component of nursing practice is the nurse-patient relationship (Canadian Nurses Association, 2002). This relationship has been shown to have a positive impact on individuals’ wellbeing as they journey through their cancer experience (Herth,1995). While the nurse-patient therapeutic relationship is fundamental to nursing care and may be quite subtle in its transaction, it is a complex phenomena with every encounter being meaningful and impacting both the patient and nurse. Reflecting on the nature of this relationship can facilitate a richer and deeper awareness of the unique contribution oncology nurses make in the lives we touch and are touched by. This presentation will explore the therapeutic nurse patient relationship in oncology nursing. The authors intend to facilitate self reflection and increased awareness of both the art and science of the therapeutic relationship. In particular, qualities of the nurse patient relationship, the importance of communication, both verbal and nonverbal and the use of silence will be explored. We will introduce the notion of coaching, an intentional way of being with patients which in turn facilitates autonomy and self efficacy. We will incorporate theory, evidence, experiential learning along with story telling, music, poetry and video images to convey our message. I-01-A FATIGUE: WHAT IT IS AND WHAT IT IS NOT Karin Olson, RN, PhD; Faculty of Nursing, University of Alberta, Edmonton, Alberta Early work by our research group identified 4 behavioural patterns that distinguish individuals who experience fatigue from those who do not, despite common treatment and disease profiles. More recently we reconceptualized fatigue by comparing the findings of studies of fatigue in populations experiencing it due to illness (chronic fatigue syndrome, depression, cancer), work (shift work), and leisure activities (recreational distance runners). We are now completing studies using ethnoscience and grounded theory designed to refine our conceptualization of fatigue. This process has provided an opportunity to distinguish fatigue from tiredness and exhaustion and to create a framework that could facilitate the identification of linkages between the behavioural markers of these three concepts and potential physiological mechanisms. In this paper, I will present our final definitions of tiredness, fatigue, and exhaustion and our theoretical model, and outline work underway to link these concepts to potential physiological markers. I will also outline the ways in which we intend to use these behavioural and physiological markers to develop and test nursing interventions. I-01-B CANCER-RELATED FATIGUE: WHAT IS A BREAST CANCER SURVIVOR’S PERSPECTIVE? Michelle Anglehart, RN, BN, MN (candidate), CON(C); South East Health Care Authority, Moncton, The experience of fatigue for breast cancer survivors is one of the most common and debilitating symptoms of breast cancer treatment. While debilitating fatigue during cancer treatment may be expected, impairment of functional status beyond treatment is often unexpected by the woman, her family and even health care professionals. This study was undertaken to learn how this societal taken-for-granted knowledge that cancer-related fatigue is timebound to cancer treatment, contributes to the phenomenon of cancer-related fatigue following treatment. Van Manen's (1997) hermeneutic phenomenological approach to human science is used to describe the phenomenon and develop an interpretation of the meaning of living with fatigue. Ten interviews were completed with five breast cancer survivors with cancerrelated fatigue following the completion of treatment. This interpretation is currently being developed and will be complete by the summer of 2005. The intent of phenomenological research is to develop an interpretation that transforms our understanding of the phenomena. Women’s stories will be used in the interpretation to help us understand the taken-for-granted knowledge about the experience of living with fatigue. Such an understanding may help nurses become more empathic and supportive. I-01-C THE DEVELOPMENT OF A FATIGUE COLLABORATIVE CARE PLAN Kathy Coulson1, RN, MScN, ACNP, CHPCN(C); Diane Batchelor2, RN, MScN, ACNP, CON(C); Elizabeth Jeffery1, RN, MSc; Sharon Preston3, RN; 1Kingston General Hospital, Kingston, Ontario; 2Diane Batchelor Advanced Practice Nurse Cancer Care, Gananoque, Ontario; 3 Kingston, Frontenac, Lennox & Addington Palliative Care Integration Project, Kingston, Ontario Fatigue continues to be a prevalent and disruptive symptom for cancer patients. There are multiple etiologies of cancer-related fatigue including co-morbid conditions, the physical, psychological and spiritual distress of cancer, and the consequences of cancer treatment. When confronted with a multiplicity of issues, fatigue often becomes a lesser priority. Frequently health care professionals view fatigue as a “normal” consequence of treatment or the disease process. Failing to address fatigue can have a major impact on quality of life. In a needs survey of cancer patients in South Eastern Ontario, 19% stated that fatigue was an under addressed issue. Reducing the severity of fatigue requires a team approach that involves adequate nutrition, correction of anaemia, pain and symptom management, exercise, and counselling. The nurse, social worker, nutritionist, physician and physical therapist should all play a role. Using an interdisciplinary approach, a Collaborative Care Plan (CCP) for Fatigue is under development based on current best practice and a review of the literature. A representative group of health care professionals from across the region, led by a CCP Consultant, Project Manager and Advanced Practice Nurse work together to achieve consensus and make the plan transferable to the practice setting. This presentation will address the development and content of the CCP and plans for implementation. I-02-A CANCER PATIENT NAVIGATOR: AN INNOVATIVE NURSING ROLE THAT ENHANCES INTEGRATION, COORDINATION AND CONTINUITY OF CARE FOR CANCER PATIENTS Charlene Porter1, RN, BScN, CON(C); Joanne Cumminger2, RN, BScN, CON(C); Darolyn Walker3, RN, BScN, CON(C); 1St. Martha’s Regional Hospital, Antigonish, Nova Scotia; 2Pictou County Health Authority, New Glasgow, Nova Scotia; 3South West Health Authority, Yarmouth, Nova Scotia Cancer Patient Navigator is a multi skilled nursing role that guides, supports and educates cancer patients, their families and health professionals throughout the cancer continuum, facilitating timely access to quality, standard cancer care in a culturally sensitive manner. Patients, families and health care professionals in Nova Scotia identified the need for improved coordination, information and support from the time of cancer diagnosis. Oncology Nurses are in a position to identify the extensive range of physical, psychological, social, emotional, and practical needs of cancer patients and with the learned navigation skills, they can strive to ensure that cancer patients have access to timely information, coordinated care and community supports. This presentation will discuss the key findings and conclusions of the peer- reviewed evaluation conducted on the patient navigator role. It will discuss how navigators have had a positive impact and resulted in improved community cancer care. The presenters will show how navigators have become an important source of support in dealing with the emotional turmoil, educational needs and logistical challenges associated with cancer. I-02-B TAKING A PILOT TO FLIGHT: IMPLEMENTATION OF NURSE LED CHANGES TO OUR AMBULATORY CLINIC I-02-C NURSING DOCUMENTATION DILEMMAS IN AMBULATORY CANCER CARE DELIVERY: CHANGE IS GOOD! Aldyn Overend, RN, BSN, CON(C); Bev Seguna, RN, BSN; Sylvia Baillie, RN, CON(C); Maureen Ryan, RN, BSN, BA, CON(C); BC Cancer Agency, Centre for the Southern Interior, Kelowna, British Columbia Grace I. Bradish, RN, MScN, ACNP, CON(C); Lyn Kligman, RN, MN/ACNP(C), CON(C); Glenda Hayward, RN, MScN; Gwen Abdallah, RN, CON(C); Tara Johnston, RN, BScN, CON(C); Sue Kudirka, RN, CON(C); Jill Ross, RN, CON(C); London Regional Cancer Program, London Health Sciences Centre, London, Ontario In 2004, nurses at the Centre for the Southern Interior struggled with how to best align nursing resources with patient needs. A growing number of patient referrals, additional oncologists and limited nursing resources continue to challenge us. Within our current care delivery model nurses know that patient needs are often unmet as there is limited time for comprehensive assessment and care planning for patients and their families. Over the past year several organizational initiatives have been implemented into our ambulatory care unit (ACU) to help support nurses in their practice allowing them time to provide quality patient care. Nurses initiated an evidence based pilot project to help identify those patients at greatest risk and with highest care needs. This presentation will discuss the pilot project, challenges faced in its implementation and changes which occurred. In doing so, we will elaborate on change agents, nursing assessment tools utilized and the provincial nursing liaisons that occurred. Finally, we will talk about our current position in the quest to deliver a higher quality level of nursing care. A chart audit (2003) of patient self-reported cancer-related symptoms using the Edmonton Symptom Assessment Scale (ESAS) revealed significant deficiencies in existing out patient documentation processes. These included incongruity between patient and nurse assessment and an absence of documented interventions such as referral of patients with significant selfreported symptoms or patient and family education. After two years of persistence, new and revised documentation tools have been pilot tested in one disease site group (Lung) with anticipated centre-wide implementation imminent. Formatting has been carefully considered to be ready for eventual integration within an Electronic Patient Record, currently in development. A nursing committee working in consultation with interdisciplinary partners, has created tools that condenses a cancer treatment summary, medication profile, patient problems list, interventions including education, and patient outcomes in one convenient location in the patient’s ambulatory chart. A summary of this project will be presented with results compared to previous chart audit as reported at CANO 2003. I-03-A INFLUENCE OF HOSPITAL CHARACTERISTICS ON NURSES’ RESEARCH USE Greta Cummings, RN, PhD; Carole A. Estabrooks, RN, PhD; William K. Midozi, MSc; Lars Wallin, RN, PhD; University of Alberta, Edmonton, Alberta There is an increasing awareness that organizational influences are important to research uptake by nurses in the goal to achieving evidencebased practice. Our study objectives were to develop a theoretical model of hospital characteristics that predict nurses’ research use and estimate this model using databases reflecting four different contexts defined by the PARIHS research implementation framework. The sample was drawn from a census of nurses working in acute care hospitals in Alberta. Three variables that operationalized PARIHS dimensions of “context” (culture, leadership, and evaluation) were used to sort cases into four mutually exclusive databases reflecting different levels of context. Our theoretical model was then estimated four times using structural equation modeling and the four datasets. Hospital characteristics that had a positive impact on nurses’ research use were control over practice, nurse-to-nurse collaboration, support for innovation, and facilitation of research use. Less time to nurse and greater emotional exhaustion led to less reported research use. Nurses working in contexts reflecting positive culture, leadership and evaluation also reported significantly more research use than nurses working in any contexts that lacked any of three dimensions. Our findings highlight the combined importance of culture, leadership and evaluation to increase research use when creating and supporting professional practice environments. The PARIHS model also is an appropriate guide to implementing research into practice by focusing on hospital characteristics that improve the contexts in which nurses work. I-03-B APPLICATION OF A NURSING WORKLOAD MEASUREMENT SYSTEM IN AN AMBULATORY ONCOLOGY SETTING Mary Bennett1, RN, BN, CON(C); Cindy Cummings Winfield, RN, BScN, CON(C); Miriam Dobson, RN, BScN, CHPCH(C); 1Tom Baker Cancer Centre, Calgary, Alberta The transition in oncology care from inpatient to outpatient settings, coupled with increased complexity of cancer treatments has significantly impacted nursing workload in ambulatory oncology. The use of patient visits as a measure of nursing workload is no longer sufficient to forecast staffing levels or validate budget requirements. Five years ago a provincial nursing initiative was undertaken to develop a nursing workload measurement system that captured direct and indirect nursing activities in our outpatient clinics and chemotherapy units. The workload form was interfaced with our electronic scheduling system, which resulted in minimal time necessary for nurses to complete and simplified data entry. Ongoing audits were incorporated to validate the accuracy and completeness of the workload data. The workload system has now been adapted for use in other nursing subspecialty areas including radiation therapy, bone marrow transplant and fatigue clinics. This presentation will describe the process of developing the workload system and provide examples of the workload forms used in various practice settings. The monthly, quarterly and annual reports that are generated will be discussed including how they are used to monitor the volume and complexity of nursing care. In addition, future plans for validating our methodology and assigned times for each workload unit will be presented. I-03-C INDUCED PERSPECTIVE-TAKING: ASSISTING FAMILY CAREGIVERS TO ACHIEVE ENHANCED PERCEPTUAL ACCURACY ON LUNG CANCER PATIENT SYMPTOM EXPERIENCES Michelle M. Lobchuk1, RN, PhD; Jacquie D. Vorauer2, PhD ; Lesley F. Degner1, RN, PhD; Dan Chateau 3, PhD; Donna Hewitt1, RN ; 1Faculty of Nursing, University of Manitoba, Winnipeg, Manitoba; 2Department of Psychology, University of Manitoba, Winnipeg, Manitoba; 3Biostatistics, Community Health Sciences, Faculty of Medicine, University of Manitoba, Winnipeg, Manitoba In response comparability literature it is inferred that family caregivers are reasonably good at “stepping inside the patient’s shoes” in order to accurately respond to patient symptoms. To test this assumption, the authors examined the effects of different perspective-taking instructions that prompted 98 family caregivers to think about lung cancer patients’ symptoms in different ways. The two main aims were: (1) to estimate the effects of a randomized, counterbalanced sequence of perspective-taking instructional sets on caregiver accuracy scores for patient symptom experiences and (2) to examine the influence of gender, the caregiver’s personal history with a cancer diagnosis, and aspects of the ‘caregiving relationship’ on caregiver judgment accuracy. There were no order effects for four perspective-taking instructional sets on caregiver accuracy scores. Findings suggested a superiority of instructions for caregivers to imagine the patient’s perspective over imagining their own perspective in relation to promoting caregiver responses that more closely approximated patient self-reports. Self-oriented instructions produced caregiver responses that were most discrepant from patient self-reports. While gender had no significant effects on discrepancy scores, the degree of patient-caregiver communication had a positive impact on decreasing the amount of discrepancy by caregivers on patient symptom experiences. I-04-C BLAZING A TRAIL: INNOVATION IN NURSING PRACTICE Colleen Valente, RN(EC), MN(C), CON(C), CHPCN(C); Thunder Bay Regional Health Sciences Centre, Integrated Cancer Program, Thunder Bay, Ontario The provision of high quality health care for Canadian residents is the primary focus of nursing in this country. The demographics of Canada are changing. As Canadian residents age, they will develop the diseases of aging, including cancer. Those suffering from a cancer diagnosis in this country, represent a growing number of patients with specialized, complex needs. There are not enough oncology specialists to ensure that all the needs of cancer patients are met, nor is it appropriate to invest the time of oncologists in the more routine aspects of patient care. The provision of cancer care requires the coordinated, collaborative approach that is the strength of nursing practice. Nurse practitioners in oncology are capable of improving the care of cancer patients and facilitating the journey of cancer patients through the continuum of care. This presentation will discuss the innovative application of the nurse practitioner role in the provision of high quality cancer care. I-04-A EFFECT OF SPECIALIZED ONCOLOGY NURSES ON CONTINUITY OF CARE, UNMET NEEDS AND QUALITY OF LIFE IN COMMUNITY CANCER PATIENTS Doris Howell1, RN, MScN, PhD; Jonathan Sussman2, MD; Kevin Brazil 2, PhD; Tim Whalen2, MD; Nancy Pyette2, MSc; Daryl Bainbridge2, MSc (candidate); 1 University Health Network, Toronto, Ontario; 2Supportive Care Cancer Research Unit, Juravinski Cancer Centre, Hamilton, Ontario Individuals with cancer/families continue to report unmet needs and difficulty accessing supportive care in the community. Research has demonstrated that supportive care is fragmented resulting problems in care coordination, psychosocial distress and poor quality of life. Specialized oncology nurse models using theorydriven evaluation methods have demonstrated performance objectives of care coordination. There is a need to evaluate if these models improve health status outcomes. The focus of this paper is to present the findings of a cohort longitudinal study designed to examine the effect of specialized oncology nursing care on patientfocused outcomes. Outcomes measured in this community-based sample of cancer patients were: care continuity, unmet needs, therapeutic self-care, and quality of life. Patterns of health care utilization in this patient population of community-based cancer patients were also explored. Study results will be presented and discussion will focus on health care policy implications and the challenges of conducting community-based research in a seriously ill cancer patient population. I-05-A (Abstract 1 of 2) A PHASED APPROACH TO DEVELOP NURSING INDICATORS IN CANCER CARE Esther Green1, RN, MSc(T), MScN(T); Janet Rush2, RN, PhD; Margaret Fitch3, RN, PhD; 1 Cancer Care Ontario, Toronto, Ontario; 2 McMaster University, Hamilton, Ontario; 3Toronto-Sunnybrook Cancer Program, Toronto, Ontario With increasing demand for professional and financial accountability, nurses have been challenged to delineate their contributions within the system and in particular, demonstrate that the care is of high quality. Nurses work within multi-disciplinary teams and outcomes directly related to nursing interventions are often problematic to define. There is a growing body of evidence that suggests that nursing contributions to patient and health outcomes are identifiable. Much of this work is in relation to hospital care, for example, the relationship of nurse staffing and staff mix to patient safety and outcomes. However, there is minimal work that has been completed to date in relation to the identification of outcomes related to cancer patients in the ambulatory environment. Cancer Care Ontario has developed a framework and undertaken to define beginning indicators through a process that involves systematic review of the evidence. In March 2005, an Expert Panel consisting of oncology nurses involved in practice, education and research came together to begin the first phase of work in developing nursing indicators in cancer care. The purpose of this presentation will be to report on the first phase of work, the results of the Expert Panel discussions and subsequent consensus on the indicators and outline the next phases of work. We believe that this work is meaningful for oncology nurses across Canada and may provide impetus for inter-provincial discussion and collaboration. I-05-A (Abstract 2 of 2) PARTICIPATIVE REGIONAL PLANNING: NURSES AS KEY STAKEHOLDERS I-05-B ARE THERE QUALITY WORK CANADIAN ONCOLOGY NURSES? Esther Green1, RN, MSc(T), MScN(T); Janet Rush2, RN, PhD; Harry Milne3, RN, MScN; 1Cancer Care Ontario, Toronto, Ontario; 2McMaster University, Hamilton, Ontario; 3 London Regional Cancer Program, London, Ontario Debra Bakker1, RN, PhD; Michael Conlon2, MSc, PhD; Karin Olson3, RN, PhD; Greta Cummings 3, RN, PhD; Lorna Butler4, RN, PhD; Margaret Fitch5, RN, PhD; Esther Green6, RN, MSc(T); 1School of Nursing, Laurentian University, Sudbury, Ontario; 2Northeastern Ontario Regional Cancer Program, Sudbury Ontario; 3Faculty of Nursing, University of Alberta, Edmonton, Alberta; 4School of Nursing, Dalhousie University, Halifax, Nova Scotia; 5Cancer Care Ontario, Toronto, Ontario In January 2004, Regional Cancer Centres were integrated into host hospitals. This, among other service delivery strategies, represented a major shift in the model of cancer care in Ontario. Stakeholder participation in shaping care that fit the provincial vision and goals was central to the planning framework. In the Southwest Region, nursing input was an essential element of planning. A survey to obtain opinion about proposed changes was conducted among attendees of an oncology nursing retreat on professional practice (n = 63). A pre-retreat, 10-item survey was distributed that asked nurses to rank and provide comments on key issues. The response rate was 41/63 (65%). The results were presented at the practice retreat, to stimulate discussion, refine and validate the findings. There was a high level of support for proposed regional strategies such as a one-number-tocall for oncology information, teamwork, partnerships, a single oncology health record, and best practice guidelines. This participative approach to planning demonstrated solid respect for oncology nurses’ opinion, motivated these key stakeholders for impending change, and fostered collaboration in the strategic initiatives. The results of this work, including the Participative Planning Framework, provide valuable information about process engagement of oncology nurses that can be used by nursing leaders and policy makers in building and sustaining a model of integration. I-05-C (Abstract 1 of 4) PROFESSIONAL AUTONOMY AND DEVELOPMENT FOR ONCOLOGY NURSES PROFESSIONAL Dauna Crooks1, RN, DNSc, PhD; Esther Green2, RN, MHSc; Mary Fergeson-Pare3, RN, PhD; Doris Howell3, RN, PhD; Debra Bakker4, RN, PhD; Joan Tranmer5, RN, PhD; Pat Sevean6, RN, PhD (candidate); Margaret Fitch 7, RN, PhD; Laurel Plewes7, BScN; Shirley Sharkey8, RN; Nancy Lefevre8, RN, MScN; 1Hospital for Sick Children, Toronto, Ontario; 2 Cancer Care Ontario, Toronto, Ontario; 3 University Health Network, Toronto, Ontario; 4Laurentian University, Sudbury, Ontario; 5 Queen’s University, Kingston, Ontario; 6 Lakehead University, Thunder Bay, Ontario; 7Toronto-Sunnybrook Regional Cancer Centre, Toronto, Ontario; 8Saint Elizabeth Health Care, Markham, Ontario Compounding the problem for oncology nursing development is the lack of available educational programs and incentives for completion of specialized education by employing agencies. This is especially important when one considers that new technologies, complex treatment protocols, telephone triage and management, as examples, require greater educational input, expertise, autonomy and skill than has previously been needed in acute and community based oncology care. This presentation focuses on the survey data from oncology nurses about their present professional development practice and where oncology nurses seek to develop themselves and their profession. Categories of discussion include: evidenced based education and application, research involvement, presentation, and leadership. ENVIRONMENTS FOR Improving the work lives of nurses has been identified by the Canadian Nursing Advisory Committee as the key focus for addressing the nursing shortage and widespread job dissatisfaction across the country. Recent qualitative work by our research team suggests that healthcare restructuring over the past decade has created challenges and sometimes conflicts for Canadian oncology nurses in providing comprehensive care to meet the needs of cancer patients and their families. Therefore, to more fully examine the quality of oncology nurses’ working lives, over 600 oncology nurses were surveyed across Canada for the purpose of collecting information about their work environment and professional practice. This presentation will describe the findings of this survey by identifying workforce management, professional practice and knowledge transition factors present in oncology settings and the linkages among these factors and their relationship to organizational climate and professional well-being. In addition, the study findings describe the quality of oncology work environments as perceived by groups of oncology nurses based on age, education, clinical setting, and geographical region. The results of this study provide valuable information about the current state of oncology nursing in Canada that can be used by nursing leaders and policy makers in building and sustaining a quality oncology nursing workforce in the future. I-05-C (Abstract 2 of 4) ONCOLOGY NURSE DEMOGRAPHICS: “KNOW” ABOUT THE ONTARIO GROUP? WHAT DO WE Dauna Crooks1, RN, DNSc; Esther Green2, RN, MHSc; Mary Fergeson-Pare3, RN, PhD; Doris Howell3, RN, PhD; Debra Bakker4, RN, PhD; Joan Tranmer5, RN PhD; Pat Sevean6, RN, PhD (candidate); Margaret Fitch7, RN, PhD; Laurel Plewes7, BScN; Shirley Sharkey8, RN, Nancy Lefevre8, RN, MScN; 1 Hospital for Sick Children, Toronto, Ontario; 2 Cancer Care Ontario, Toronto, Ontario; 3 University Health Network, Toronto, Ontario; 4Laurentian University, Sudbury, Ontario; 5Queen’s University, Kingston Ontario; 6 Lakehead University, Thunder Bay, Ontario; 7Toronto-Sunnybrook Regional Cancer Centre, Toronto, Ontario; 8 Saint Elizabeth Health Care, Markham Ontario. Despite increasing needs from the growing sector of individuals with cancer or at risk for the disease, there is no database to assist in health human resource planning for the next decade. Secondly, even if a resource plan existed, there is no research evidence to support the requirements for the level of registered nursing practice relative to patient/family needs or differentiation of clinical activities between generalized, specialized or advanced levels of oncology nursing practice. This presentation describes who is practicing in oncology in Ontario at the specialized and advanced categories as defined by CANO. The study group surveyed nurses in all health care sectors in Ontario providing care to oncology patients in adult and pediatric settings. We will present ideas for a comprehensive data base and will compare our results with published CIHI and CNA data. Data presented will include: level of expertise in oncology, retirement data, years in oncology service, proportion of oncology in practice as examples. Finally, we will propose strategies for cancer care human resource planning. I-05-C (Abstract 3 of 4) ONCOLOGY NURSING IN ONTARIO: A SYNTHESIS OF SURVEY DATA TO PLAN OUR PROFESSIONAL FUTURE Dauna Crook 1, RN, DNSc; Esther Gree 2, RN, MHSc; Mary Fergeson-Par3, RN, PhD; Doris Howell3, RN, PhD; Debra Bakker4, RN, PhD; Joan Tranmer5, RN PhD; Pat Sevean6, RN, PhD (candidate); Margaret Fitch7, RN, PhD; Laurel Plewes7, BScN; Shirley Sharkey8, RN, Nancy Lefevre8, RN, MScN; 1 Hospital for Sick Children, Toronto, Ontario, 2 Cancer Care Ontario, Toronto, Ontario; 3University Health Network, Toronto, Ontario; 4Laurentian University, Sudbury, Ontario; 5 Queen’s University, Kingston Ontario; 6 Lakehead University, Thunder Bay, Ontario; 7Toronto-Sunnybrook Regional Cancer Centre, Toronto, Ontario; 8Saint Elizabeth Health Care, Markham Ontario. This presentation will synthesize the results of a survey of oncology nurses in a variety of settings in Ontario. The survey captured the thoughts of specialized and advanced oncology nurses about where they work, what they do, who they collaborate with and how independent they are in their practice. Results disclose areas of concern for development of oncology roles and future leadership. The presentation will focus on the larger picture of demographic issues and challenges to come in retirements, expertise, educational levels, and help us to begin to define Human Health Resource planning issues for the oncology nurse group. The presentation also highlights the ambiguity, role overlap and lack of clarity in deciphering and enacting oncology nursing roles at the specialized and advanced practice levels. In addition, the issues and differences by context of practice and geographic area will be highlighted. I-05-C (Abstract 4 of 4) THE FUTURE OF ONCOLOGY NURSING: WHERE DO WE WANT TO GO AND WHAT BARRIERS OR PROMOTERS EXIST FOR FUTURE ROLE DEVELOPMENT Dauna Crooks1, RN, DNSc; Esther Green2, RN, MHSc; Mary Fergeson-Pare3, RN, PhD; Doris Howell3, RN, PhD; Debra Bakker4, RN, PhD; Joan Tranmer5, RN PhD; Pat Sevean6, RN, PhD (candidate); Margaret Fitch7, RN, PhD; Laurel Plewes7, BScN; Shirley Sharkey 8, RN, Nancy Lefevre8, RN, MScN; 1 Hospital for Sick Children, Toronto, Ontario, 2Cancer Care Ontario, Toronto, Ontario; 3 University Health Network, Toronto, Ontario; 4Laurentian University, Sudbury, Ontario; 5Queen’s University, Kingston Ontario; 6 Lakehead University, Thunder Bay, Ontario; 7Toronto-Sunnybrook Regional Cancer Centre, Toronto, Ontario; 8Saint Elizabeth Health Care, Markham Ontario. Minimal research has been undertaken to discover the impact on care delivery of oncology nursing roles in Canada. This presentation will focus on survey results examining the clinical role functions of oncology nurses at the specialized and advanced levels of practice with specific reference to the expectations oncology nurses have for their future scope of practice. Oncology nurse perceptions of barriers to role change will be addressed. We will present potential solutions to overcome barriers, allowing oncology nurses to work to full scope of practice and evolve in their roles as patient care needs change Finally, issues for educational preparation and support will be addressed and a strategy for the future will be put forward. I-06-A FOSTERING PROFESSIONAL NURSING PRACTICE ON A TERTIARY CARE INPATIENT PEDIATRIC ONCOLOGY UNIT I-06-B TUMORS OF GLIAL ORIGIN: CONFINED COMPLEXITY Patricia McCarthy, MScN; Children’s Hospital of Eastern Ontario, Ottawa, Ontario Cindy Cummings-Winfield, RN, BScN, CON(C); Susan King, RN, BScN, CON(C); Cross Cancer Institute, Edmonton, Alberta The realities faced by oncology nurses today, such as the ever increasing acuity of oncology patients, staffing, safety and workload issues challenges the focus and spirit of even the most seasoned oncology nurse. The nursing staff on the inpatient pediatric oncology unit at this hospital are very junior. There are 28/40 nurses under the age of 29 years. We need to develop strategies and systems aimed at developing the skill and confidence of junior nurses to face the complex realities of everyday practice. Tumors of the central nervous system (CNS) are a diverse group of heterogeneous, benign and malignant, primary neoplasms and metastatic tumors. There are over 100 histologic classifications of primary brain tumors alone. Gliomas are the most commonly occurring primary brain tumor. The purpose of this poster will be to share the learning and outcomes of an RNAO advanced clinical fellowship, undertaken by the oncology APN at this pediatric hospital in the fall of 2004. The goals of the fellowship were 1) to examine the factors and processes that foster professional nursing practice on a tertiary care pediatric oncology unit, and 2) to develop an understanding of the leadership skills and strategies that create positive change within a nursing system. The candidate utilized multiple methods to immerse herself into the culture of the inpatient unit. She conducted literature reviews on practice models and empowerment of nurses. She conducted focus groups with nurses, utilized observation and informal discussions with patients /families and hospital nursing leaders and maintained a reflective journal. She discussed ideas and progress with her mentoring team regularly and consulted with nursing experts during a site visit to a center of nursing excellence. An integrated plan for fostering the growth and development of junior oncology nurses was developed. This plan includes implications for nursing practice, education and research, and addresses sustainability of outcomes from the fellowship. Even though glial tumors are confined to the CNS they can result in a multitude of disabling sequelae. Patients and their families are faced with difficult treatment decisions. This complexity is compounded with ethical considerations when patients experience cognitive and perception problems. Excellence in oncology nursing care requires the nurse to be knowledgeable about treatment modalities for brain tumors, anticipated symptoms specific to this patient population, and appreciation of the impact this disease has on the patient and their family. This presentation will review the anatomy of the CNS, and epidemiology, etiology, and classification and staging of glial tumors. Clinical presentation, diagnosis and treatment of glial tumors will be discussed. The presentation will conclude with a review of the unique complications experienced by the patient with a glial tumor and their family, quality of like issues and nursing interventions. I-06-C UPDATE ON ACUTE MYELOID LEUKEMIA Gail Macartney, RN, MSc(A), ACNP, CON(C); Ottawa Hospital, Ottawa, Ontario The overall incidence of acute leukemia is approximately 4/100,000 individuals. The incidence in people aged 60 or over rises to about 10/10,000 individuals. Acute myeloid leukemia (AML) refers to a series of relatively well-defined hematopoietic neoplasms involving cells committed to the myeloid cell line. Individuals diagnosed with acute leukemia need to become informed about this potentially life threatening disease, generally within a very short period of time. This presentation will review the clinical features, diagnosis and prognosis of AML. The pathobiology of AML will be reviewed with a focus on cytogentic and molecular genetic diagnostic tools. This presentation will empower nurses working with AML patients to better understand the pathogenesis of this disease and rationale for therapy. Consequently, their ability to provide comprehensive care will be enhanced. II-01-E EXAMINING THE CONTRIBUTION OF LEADERSHIP STYLES TO 30-DAY PATIENT MORTALITY IN ALBERTA HOSPITALS Greta Cummings, RN, PhD; William K. Midodzi, MSc; Carole A. Estabrooks, RN, PhD; University of Alberta, Edmonton, Alberta Background: Emotionally intelligent (resonant) nursing leadership has been shown to mitigate the negative effects of hospital restructuring on nurses’ health and wellbeing, thereby supporting the nurses’ ability to provide quality care to patients. The purpose of this study was to examine the contribution of resonant nursing leadership, as reported by nurses in acute care hospitals in Alberta, to one outcome ─ 30-day patient mortality. Method: Data for 18,142 adult medical patients discharged from 49 hospitals in Alberta in 1999 were used to measure patient demographics, co-morbidities and outcomes. The responses of registered nurses working in these same hospitals to the Revised Nursing Work Index (NWI-R) were used to measure the predominant nursing leadership styles (resonant, dissonant or mixed) in each hospital. Analysis: We used a two level hierarchical linear model (patients at level 1 and hospitals at level 2) to determine the contribution of patient demographics, co-morbidities, hospital characteristics and nursing leadership styles to patient mortality. The level 1 model consisted of patient demographic, co-morbidity and outcome variables. The level 2 model consisted of variables measuring hospital characteristics and nursing leadership styles. Results: Nursing leadership styles significantly contributed to differences in mortality of medical patients across hospitals, after adjusting for patient co-morbidities, demographic factors, and hospital characteristics. Hospitals with resonant leadership had significantly lower patient mortality than those with dissonant or mixed (neither completely resonant nor dissonant) leadership. II-01-D SUPPORTING PATIENTS BETWEEN DIAGNOSIS AND REFERRAL FOR TREATMENT: INFORMATION & SUPPORT NEEDS OF PATIENTS DIAGNOSED WITH HEAD & NECK CANCERS Maurene McQuestion1, RN, BScN, APN, CON(C), MSc (candidate); Doris Howell2, RN, PhD; David Wan3, BSc; 1 Princess Margaret Hospital, University Health Network; 2RBC Financial Group Chair in Oncology Nursing Research, University Health Network, University of Toronto; 3University of Toronto School of Medicine; Toronto, Ontario. Supportive care has been defined as meeting the needs of those affected by cancer in the domains of physical, informational, psychosocial, emotional, practical and spiritual needs across the cancer experience (Fitch, 1994). Most research in the area of head and neck (H&N) cancer has focused on the efficacy of treatment modalities and the assessment and management of treatment side effects and toxicities. While there has been a focus of understanding the needs of other patient populations in the early diagnostic phase, little or no attention has been directed toward understanding the information and support needs of this group of patients. Their needs may be particularly unique in light of social and demographic factors, lifestyle risks for cancer, difficulties with eating / swallowing, and the potential for disfiguring surgery or challenging treatments. Understanding the needs of patients newly diagnosed with H&N cancer is important for developing nursing care measures and delivery models as well as integrating supportive care measures early in the continuum that extend into the survivorship period.A research project was developed to assess the needs of this patient population between diagnosis and referral for treatment. Focus groups were held with 12 participants to explore the informational and support needs of patients with head & neck cancer during the transition period between diagnosis and referral to the treatment centre. The presentation will review the literature on supportive care, share themes derived from the focus groups and offer recommendations to better support patients in the community and at the treatment centre. II-01-F “I’D RATHER DIE THAN GO TO EMERG”: PATIENT’S PERSPECTIVES ON EMERGENCY ROOM VISITS FOR FEBRILE NEUTROPENIA Arlene Court, RN, BScN, CON(C); Sharon Lemon, RN, BScN, CON(C); Grace Sangle, RN, CON(C); Sunnybrook & Women’s Health Sciences Centre, Toronto, Ontario Febrile neutropenia is the number one oncological emergency experienced by most cancer patients. A chart review at this cancer centre showed 122 patients visited the institution’s emergency room for chemotherapy induced febrile neutropenia in a twelvemonth period. Patients frequently verbalize distress about waiting times, triage processes and inconsistent management by the hospital team at emergency room visits. Nurses question the effectiveness of patient teaching that prepares patients for self-care regarding fevers. A retrospective randomized telephone survey was conducted with twenty breast cancer patients who attended the emergency room for febrile neutropenia. The telephone interviews utilized a questionnaire, which addressed areas of patient concern and the nurses’ questions regarding patient teaching. The findings of the telephone survey will be shared with resulting recommendations. New tools for patient management approaches are required to effectively support patients with febrile neutropenia. By listening to our patients and implementing new strategies, the oncological emergency of febrile neutropenia can be managed. We can do better. II-02-D SHAPING THE FUTURE OF PALLIATIVE CARE NURSING: THE DEVELOPMENT OF SPECIALITY COMPETENCIES Deborah Gavelle, BScN, MHS (candidate); Lillian Locke, BScN, MPA; SCO Health Services, Ottawa, Ontario To be effective at relieving suffering and improving quality of life, caregivers including nurses must be able to identify and respond to complex/multiple issues that patients and families face. (CHPCA, 2002) Competencies are the skills, knowledge, personal attributes and judgments expected of nurses to provide safe, ethical and effective care (CNO, 1999). Nursing competencies are defined as statements which describe expected performance, behaviours and reflect the professional attributes required in a given role, situation and practice setting (College of Nurses of Ontario, 1999). Specialty nursing competencies represent the specific knowledge, skills and personal attributes required for a nurse to care for a particular patient population. The goal of the Specialty Nursing Competency program is to provide exemplary care to patients and their families receiving care through nursing excellence. The specific objectives of the program are: to promote reflective practice, articulate practice expectations and plan and implement learning opportunities to facilitate nurses maintaining and gaining knowledge, skills and ability within their practice context. This presentation will describe the components of the program, the speciality competencies required by palliative care nurses, the integration of the competencies with a professional practice model, and the impact on patients and families. II-02-F IMPLEMENTING BEST PRACTICE GUIDELINES FOR PALLIATIVE CARE WITHIN A CANCER CENTRE Kathy Coulson1, RN, MScN, ACNP, CHPCN(C); Elizabeth Jeffrey1, RN, MSc; Diane Batchelor2, RN, MScN, ACNP, CON(C); Sharon Preston3, RN; 1Kingston General Hospital, Kingston, Ontario; 2 Diane Batchelor Advanced Practice Nurse Cancer Care, Gananoque, Ontario; 3Kingston, Frontenac, Lennox & Addington Palliative Care Integration Project, Kingston, Ontario This presentation will outline how a cancer center participated in the development and implementation of best practice guidelines for palliative patients through its involvement in a regional palliative care project. The Palliative Care Integration Project is an exciting initiative with the goal of attaining the best quality of life for patients and families for whom curative therapies are no longer possible. Discontinuity of care, inconsistent pain and symptom management, few assessment tools, little evidence based practice, variable knowledge and under-utilization of resources were identified through regional research as persistent problems in palliative care. A unique regional strategy to integrate palliative care was developed. Over 100 individuals representing 25 organizations were involved in the project. The key objectives were to facilitate easy, uncomplicated access to palliative care by implementing validated assessment tools, care plans and supporting guidelines. Individuals from the participating organizations were divided into teams for development of three evidence based generic care plans for stable, transitional and end-of-life patients, as well as, two symptom focused care plans for pain and dyspnea. Other teams focused on implementation (education and documentation). The broad based interdisciplinary consultation used in developing the project resulted in a network of contacts and a ground swell of enthusiasm. The strategies as well as the successes and challenges of implementation within a cancer centre will be highlighted. II-02-E PROGRAM PLANNING AND EVALUATION: ENHANCING ONCOLOGY PALLIATIVE CARE THROUGH INTEGRATION OF BEST PRACTICES Vicki Lejambe, RN, BScN, CON(C); Saint Elizabeth Health Care, Markham, Ontario Best practice guidelines (BPG’s) as defined by the Registered Nurses Association of Ontario, “are systematically developed statements (based on best available evidence) to assist practitioners' and clients' decisions about appropriate health care. Guidelines are a resource tool, to be used in assessing current practices, developing policies, procedures, protocols, educational programs, quality standards, and assessment and documentation tools, within a practice setting”. This presentation will describe a program planning process that integrated BPG’s to enrich our oncology palliative care program. The innovative enhancements include : Adopting Client Palliative Performance Scale scores to identify level of care provider; Creation of ‘Smarter’ documentation tools to enhance and cue practice from an evidence base; and Creation of client educational material and records to fully support informed decision making and participation in planning and delivery of care. The audience will learn about the framework and tools used to guide program planning. They will be introduced to our documentation tools that enhance and cue evidence based practice, and will share in the evaluation results to date. Although conducted in a community setting, the strategies used to enhance nursing practice have broad application in a wide range of clinical settings. II-03-D DECISION-MAKING AMONG WOMEN DIAGNOSED WITH STAGE I & II BREAST CANCER: A NOVA SCOTIA PERSPECTIVE Brenda Sabo 1, RN, MA, PhD Student; Carman Giacomantonio 2,3, MD; Daniel Rayson 2,3, MD; Maureen Nolan 2,3, MD; 1 QE II Health Sciences Centre, Halifax, Nova Scotia; 2 Capital District Health Authority, Nova Scotia; 3 Nova Scotia Cancer Centre How clients within the healthcare system make decisions about their treatment(s) has been an important focus of healthcare delivery since the early 1990’s. As health professionals we need to understand how clients make decisions, support their approach and provide the necessary resources for the client (based on their suggestions) to make a fully informed decision about the care they desire. A province-wide initiative was undertaken using a mixedmethod (survey, interviews and focus groups) approach to explore how women diagnosed with stage I & II breast cancer made their decision choices about treatment, how satisfied they were with their choices, and what changes are necessary to improve or enhance their ability to make decisions consistent with their beliefs, values and style. The survey resulted in a 57% positive response rate. Fifty-one percent of the respondents preferred an active decision making role (based on the definition by Degner & Sloane, 1992). Age was the only variable to be significantly associated with decision satisfaction The findings from this project will be presented along with implications for research and practice II-03-E DEVELOPMENT AND EVALUATION OF AN INFORMATION AND TEACHING PACKAGE FOR OLDER ADOLESCENTS AND YOUNG ADULTS WITH CANCER Andréa Maria Laizner, N, PhD; Emily Ingram, BA; David Wright, BSc; Nancy Hutchison, N, MScA, CON(C); Christine Leblanc, N, BScN, CON(C); McGill University Health Centre (RVH), Montreal, Quebec Literacy and health are connected. Nurses contribute to better health or learning outcomes for individuals by using plain language health information. The term “health literacy” refers to an individual’s capacity to read and comprehend medical information and instructions. More recently, it refers to facilitating access to information that enables individuals to make informed choices, influence events, and exert greater control over their lives. Given that approximately 20 to 30 percent of Canadian youth are not completing high school and that anxiety as well as cancer related fatigue could interfere with comprehension, it is extremely important that health information be written using clear health communication and plain language. A team of nurses, graphic artists, translators, and volunteers worked together to prepare information materials for the Older Adolescent and Young Adult Program in Oncology. These materials, English and French versions, would serve to orient new patients and their families to the program. Nurses could use these materials as a teaching package with this target group when talking about disease, chemotherapy treatment, side effect management and use of resources. This presentation describes the process used to develop the materials and to evaluate their content and usefulness for a target group of patients. Guided by the work of The Centre for Literacy of Quebec and others, specific emphasis in the evaluation of the materials was placed on layout (appearance and appeal), readability, and client satisfaction. II-04-D HEALING TOUCH AS AN ADJUVANT HOLISTIC APPROACH INTEGRATED WITH ALLOPATHIC MEDICINE FOR ONCOLOGY PATIENTS Jeanne Balcom, RN, HTP; Beauséjour Regional Health Authority, Moncton, New Brunswick Focusing on true self-care and personal healing through your own inner process is an important focal point in this presentation. As stated in Healing Touch a Guidebook for Practitioners: "The first part of our life is spent finding our identity, and the second part of our life is moving into our greater identity as spiritual beings. This maturing is called individuation and it differentiates from the achievementorientated nature of our early life's work. Anyone who is serious about helping others needs to individuate-to be less dependant on outside opinions and be able to hear the inner guidance that is available through daily, committed practice". What is Healing Touch? Healing Touch is a nursing continuing education multi-level program in energy-based therapy. It uses touch to influence the human energy field centers to bring balance and alignment to individuals. Body, mind, emotion, and spirit, are touched through this therapeutic process. Some benefits of Healing Touch as an adjuvant therapy with oncology patients are: relieving pain, promoting relaxation, improving energy level and supporting the dying process. This presentation explores an oncology nurse's vision, with the support and help of others, the integration of Healing Touch within the health care system in a community. II-03-F MY CARE SOURCE-EMPOWERING PATIENT MANAGED CARE Claudette DeLeonardo, RN, BScN, MSN(C), CAE; Grand River Hospital, Kitchener, Ontario My CARE Source is an innovative web-based, patient-centric application that assists patients to navigate their way through the confusing and complex system of cancer care. My Care Source, a personalized support and disease management tool actively engages patients in their health. Patients become their own “project manager” by engaging in proactive and informed management of their journey through treatment. Patients have identified gaps in cancer services specifically in dissemination of information, provision of supportive care and delivery of services (CCS, 2003). Barriers to obtaining information include knowing how and where to obtain specific information and accessing a health care provider. A coordinated strategy that provides evidencebased health information is essential in meeting the needs of patients with cancer. Other patient portals exist in healthcare however; My CARE Source is the first to our knowledge that delivers fully integrated treatment plans that provide patients with a personalized plan of care including links to relevant patient education along with the ability to document, track and monitor symptoms and/or side effects of treatment. Evidence-based sources are used to develop treatment protocols and build the content library. Two surveys have been conducted to evaluate the functionality and content of the application. All participants stated they found the application easy to navigate and to read. All participants stated they would recommend the portal to others. II-04-E THERAPEUTIC TOUCH™: AN EXTENSION OF PROFESSIONAL SKILLS IN CLINICAL ONCOLOGY NURSING Caroline Merritt, RN, CON(C); Atlantic Corporation, Hampton, New Brunswick Health Sciences Therapeutic Touch is a modern version of several ancient healing practices. It is a process of energy exchange. The practitioner uses his/her hands as a focus for promoting healing in the patient. Therapeutic Touch was developed in the early 1970’s through the pioneering work of Dolores Krieger, Ph.D., R.N., a professor at New York University, and Dora Kunz, a natural healer. Research has shown that Therapeutic Touch can promote relaxation and provide a sense of comfort and well being, by readily eliciting the relaxation response. It has been shown to be helpful for symptom management for cancer patients, and those journeying toward end of life. Canada’s national accreditation committee for Cancer Care Centers recommends that nursing staff offer Therapeutic Touch to inpatients to assist in pain control and enhance the patients’ sense of well being. Therapeutic Touch blends the art and science of nursing. Nurse Healers- Professional Associates International, Inc. and the Therapeutic Touch Network of Canada are the professional governing bodies whose mission it is to lead, inspire, and advance excellence in Krieger- Kunz Therapeutic Touch. This presentation will provide an introduction to Therapeutic Touch for Oncology nurses, focusing on its principles and practical applications, and will offer experiential exercises for the participants. II-04-F SPIRITUAL ASSESSMENT: REFLECTIONS FROM YESTERDAY, IMPRINT FOR TOMORROW Brenda Caldwell, RN, BScN, CON(C); Margaret Baker, RN, BSN, CON(C), CHPCN(C); Stephanie Burlein-Hall, RN, BScN, MEd, CON(C); Interlink Community Cancer Nurses, Toronto, Ontario Spiritual care is important to patients who are suffering form a lifethreatening illness such as cancer (Schnoll, Harlow, & Bower, 2000) and an important aspect of holistic nursing care. (Musgrave, McFarlane, 2004). Previously, no framework was used to guide patient/family discussion regarding spiritual care issues by a group of specialized community oncology nurses. During the development of a comprehensive patient/family assessment tool, the nurses identified the need to incorporate the spiritual domain into the new assessment tool. After reviewing the literature, Pulchalski’s FICA spiritual assessment tool (Pulchalski, Romer 2000) was chosen for implementation. The presentation will provide an overview of spiritual care within a supportive care framework. Results of a chart review evaluating the use of the FICA tool, and a peer survey highlighting the challenges in getting at issues of meaning for patients living with cancer, will be featured. Nurses are uniquely positioned to be available when patients experience spiritual distress. Providing oncology nurses with practical frameworks that can facilitate the assessment of spiritual needs is important in providing the holistic care needed to leave an imprint for tomorrow. II-05-D (French) PROBABILITÉ DE PARTICIPATION D’UNE POPULATION QUÉBÉCOISE ASYMPTOMATIQUE À UN PROGRAMME DE DÉPISTAGE DU CANCER COLORECTAL Louise Bouchard1, inf., PhD; Johanne Roy2, inf., MSc; Geneviève Baron2, MD, MSc, FRCPC; 1 Université de Montréal; 2 Direction de la Santé Publique de la Montérégie. Au Canada, le cancer colorectal représente la deuxième forme de cancer la plus meurtrière. Des groupes canadiens recommandent un programme de dépistage de ce cancer dans un proche avenir. L’objectif de cette étude qualitative était d’explorer les perceptions d’une population québécoise asymptomatique sur le cancer colorectal et sa prévention et leur opinion sur trois tests de dépistage après avoir reçu une information détaillée sur ces derniers. Six focus group (n =58 participants) ont été formés. Les résultats révèlent que les participants peuvent nommer plusieurs mesures de prévention primaire du cancer colorectal, ses symptômes et facteurs de risque, mais certaines croyances persistent sur son étiologie, son évolution et la fréquence du « sac » de colostomie. Le quart des participants, surtout des femmes, connaissent certains tests pour les avoir déjà passés dans un contexte symptomatique. Selon les résultats, il est peu probable que ces individus participeraient au dépistage du cancer colorectal s’il était implanté dans un proche futur. Ces derniers sous-estiment leur risque personnel à contracter ce cancer et sont peu renseignés sur son histoire pré-cancéreuse naturelle. Leur notion de dépistage est inscrite dans un contexte symptomatique. Ils subiraient certains tests de dépistage si leur médecin traitant les leur recommandait fortement. Ils se sont cependant montré prêts à recevoir plus d’information sur le sujet. Les participants ont livré des opinions critiques à l’égard du système de santé invitant les chercheurs à une réflexion quant à l’approche éducative à déployer pour favoriser leur participation au programme de dépistage colorectal. II-05-D (English) PROBABILITY OF PARTICIPATION OF AN ASYMPTOMATIC QUEBEC POPULATION TO A COLORECTAL CANCER SCREENING PROGRAM Louise Bouchard1, PhD; Johanne Roy2, MSc; Geneviève Baron2, MD, MSc, FRCPC; 1Université de Montréal; 2Direction de la Santé Publique de la Montérégie In Canada, colorectal cancer represents the second deadliest form of cancer. Canadian groups have recommended implementing a screening program for this form of cancer in the near future. The objective of this qualitative study was to explore the perceptions of an asymptomatic Quebec population on colorectal cancer and its prevention as well as their opinions on three screening tests after receiving detailed information about these tests. Six focus groups (n=58 participants) were formed. The results reveal that the participants were able to name the symptoms and risk factors of colorectal cancer as well as many primary prevention measures, but certain beliefs persist about its etiology, evolution and the frequency of the colostomy bag. One quarter of the participants, mostly women, know some of these tests by having experienced them in a symptomatic context. According to the results, it is unlikely that these individuals would participate in colorectal screening if it was implemented in the near future. These subjects underestimate their personal risk of contracting this form of cancer and are not well informed about the disease’s natural history. Their notion of screening comes from a symptomatic perspective. They would undergo certain screening tests if their attending physician strongly recommended them. However, they are willing to receive more information on the subject. The participants gave critical opinions on the health care system thus making researchers think about which educational approach to use to encourage participation in the colorectal cancer-screening program. II-05-E EARLY-STAGE PROSTATE CANCER TREATED BRACHYTHERAPY: NAVIGATING IN A GREY ZONE BY Robert Roy, BSc; Dr. Leon Richard Oncology Centre, Moncton, New Brunswick Prostate cancer affects approximately 20,000 Canadians every year. When a man is diagnosed with this form of cancer, he is confronted with difficult decisions regarding the available treatments. It is also common for men with prostate cancer and their families to be concerned about the disease. However, the majority of people become less worried once they have learned more about the disease and after the treatments have begun. Having a contact person, with whom the patient can establish a trusting relationship and receive guidance in terms of care, are some of the functions of a brachytherapy nurse case manager. Since long-term posttreatment follow-ups will be required and brachytherapy treatment centres are far apart, local follow-up, which is often desired by the patient, is possible. In these cases, follow-up is safely ensured by the local general practitioner, in collaboration with the nurse case manager and the brachytherapy centre’s team. The purpose of this presentation is to examine the implementation of the role of brachytherapy nurse case manager from a treatment centre that serves the population of the Atlantic provinces. II-05-E (French) CANCER PRÉCOCE DE LA PROSTRATE TRAITÉ CURIETHÉRAPIE; NAVIGUER DANS UNE ZONE GRISE PAR II-05-F (English) UNACCEPTABLE DELAYS IN THE DIAGNOSIS AND TREATMENT OF BREAST CANCER: A FRANCOPHONE COMMUNITY ENSURES BETTER COORDINATION Robert Roy, BSc; Dr. Leon Richard Oncology Centre, Moncton, New Brunswick Linda Varner, BScN, CSIO(C); Dr. Leon Richard Oncology Centre, Moncton, New Brunswick Le cancer de la prostate touche environ 20 000 canadiens chaque année. Lorsqu’un homme est diagnostiqué avec ce type de cancer, il est confronté à des décisions difficiles quant aux traitements offerts. Il est également commun de voir que les hommes atteints d’un cancer de la prostate et leurs proches soient inquiets face à cette maladie. Toutefois, la plupart d’entre eux constatent que leurs préoccupations diminuent une fois qu’ils comprennent mieux la maladie et que le traitement débute. Avoir une personne contact avec qui le patient peut établir un climat de confiance, lui permettant d’être guidé vers une prise en charge, est une des fonctions d’un infirmier gestionnaire de cas en curiethérapie. Puisque un suivi à long terme post traitement s’impose, et que les centres de traitements en curiethérapie sont situés à distance; un suivi local, souhaité par le patient, est souvent possible. Lorsque c’est le cas, un suivi est assuré en toute sécurité par l’omnipraticien local, en collaboration avec l’infirmier gestionnaire de cas et l’équipe de curiethérapie du centre. Cette présentation aura pour but de faire un retour sur l’implantation du rôle d’un infirmier gestionnaire de cas en curiethérapie à partir d’un centre de traitement qui désert la population des provinces Atlantique. According to the Cancer Advocacy Coalition of Canada (2000), a woman living in one of the Atlantic Provinces has fewer chances of surviving breast cancer than if she lived in British Columbia or Ontario. It has been documented that delays have an influence on the stage of disease at the time of diagnosis and consequently, the prognosis. Survivors, who are assisting newly diagnosed women, reported significant delays in the diagnosis and treatment of breast cancer in New Brunswick as well as the lack of support for these women during the investigation period. These observations (2000 – 2002) were confirmed by a retrospective study of breast cancer cases referred to an oncology centre in New Brunswick. A breast clinic was created to improve access to services. Thanks to the services of an oncology navigator nurse, in collaboration with committed partners, those unacceptable delays were reduced by 58 % (2003 – 2004). In addition, ad hoc and continuous support was provided to the women who were referred to the clinic. Algorithms for the diagnosis and follow-up were developed. These measures did not create additional costs to the health care system. The objective of this presentation is to explain this innovative model, the role of the navigator nurse and the transferability potential of this model to other communities. II-05-F (French) DÉLAIS INACCEPTABLES DANS LE DIAGNOSTIC ET LE TRAITMENT DU CANCER DU SEIN; UNE COMMUNAUTÉ FRANCOPHONE ASSURE UNE MEILLURE COORDINATION III-01-A SUPPORTING HOPE IN PALLIATIVE CARE PATIENTS AND FAMILIES: THE CHALLENGES AND BENEFITS FOR ONCOLOGY NURSES Linda Varner, inf. BSc Inf., CSIO(C); Centre d’oncologie Dr-LéonRichard, Moncton, N.B. Allyson Clarke, RN, MSc; Princess Margaret Hospital, University Health Network, Toronto Ontario Selon le Cancer Advocacy Coalition of Canada (2000),une femme vivant dans les provinces Atlantiques, a moins de chance de survivre un cancer du sein que si elle habite en Colombie-Britannique ou en Ontario. Il est bien documenté que les délais influent le stade de la maladie au moment du diagnostic et par le fait même, le pronostic. Des survivantes, accompagnant des femmes nouvellement diagnostiquées, ont rapporté des délais considérables lors du diagnostic et du traitement du cancer du sein au N.-B. ainsi que le manque de soutien pour ces femmes pendant la période d’investigation. Une étude rétrospective des cas de cancer du sein référés à un centre d’oncologie au N.-B. a confirmé ces constats (2000-2002). Une clinique du sein fut mise sur pied afin d’améliorer l’accès aux services. Grâce à la présence d’une infirmière navigatrice en oncologie, en collaboration avec des partenaires engagés, ces délais inacceptables furent réduits de 58% (2003-2004). De plus, du soutien ponctuel et continu aux femmes référées fut assuré. Des algorithmes pour le diagnostic et le suivi furent élaborés. Ces démarches n’ont pas été plus onéreuses pour le système de santé. Cette présentation a pour objectif d’expliquer ce modèle novateur, le rôle de l’infirmière navigatrice et le potentiel de transférabilité de ce modèle aux autres communautés. Hope has been identified as playing a critical role in effective coping and quality of life for all individuals. Oncology nurses work with their patient’s hope every day. Research has begun to show the impact nurses have in this area and the key role they can play in supporting their patient’s hopes. Most definitions describe hope as directly linked to the individual’s desires for the future. Both patients and nurses struggle with the challenge this creates when an individual becomes palliative and is unable to be cured. Many health care professionals describe the difficult balance between false hope and hopelessness. This presentation will discuss the concept of hope and how this can be promoted in palliative care patients. It will present current research around hope and will discuss strategies for oncology nurses to assist patients both with their transition into the palliative stage of care and throughout their palliative care experience. The focus will be on case scenarios that discuss the challenges of supporting transitions around some of oncology patient’s common hopes, such as “hope for a cure”. III-01-B CARING FOR THE DYING PATIENT AND CAREGIVERS DEVELOPMENT OF A BROCHURE: SHARING PRACTICAL ADVICE ON HOW TO MANAGE POTENTIAL PHYSICAL CHANGES AT THE END OF LIFE Patty McQuinn, RN, MSc(A), CHPCN(C); Eleanor Nicholson, RN; South Regional Health Authority, Moncton, New Brunswick A recent poll indicated that 90% of Canadians wish to remain in their own homes during the final stages of life; yet only 6% of informal caregivers feel they could adequately care of their loved ones without hospice palliative care support. Our teams are part of a provincial home care program that has been involved in palliative care for over 24 years. Our community-based program uses a multidisciplinary team approach in delivering care. The home care teams have utilized several information sheets in the past to assist caregivers by explaining what to anticipate when a death is expected to occur at home. We have been working to develop and implement a concise family friendly information brochure for the teams to use. The brochure will not replace explanations to the families. It is to help provide guidance, practical advice and support when families of home palliative patients are asking questions related to end of life. The information brochure was trialed and the results documented. This presentation will highlight the developmental effectiveness and content of the end of life brochure. process, References 2004 January, Canadian Hospice Palliative Care Association information fact sheet Ferrell, R.B. & Coyle, N. (Eds). (2001). Textbook of Palliative Nursing, New York: Oxford University Press III-02-A “EVEN LONGER LENGTHS OF STAY…” Pamela J. West, RN, MSc, ACNP, CON(C), CHPCN(C); Rouge Valley Health System, Centenary Site, Toronto, Ontario Cancer care is changing rapidly (and for the better). In days gone by, the end point for all clinical trials was ‘survival’. In the mid nineties, quality of life and instruments to measure this phenomenon were introduced, and both survival and the quality inherent in those extra few weeks/months became the valued outcome. However, it is a new century: a new millennium. There is an emerging and significant concept that will have incredible impact on care provided generally, and more specifically on patients with a cancer diagnosis receiving that care. This concept is “stable disease”. The chronicity of treated disease is becoming more of a reality, and prognostication and ever-increasing guessing game. This paper will review the literature on prognostication, the concept of stable disease and explore how oncology practice is beginning to measure this phenomenon. Stable disease opens the door for other new and evolving concepts such as cancer rehabilitation. Ideally patients will have longer and better illness trajectories and nurses will have longer journeys accompanying them in their illness experience. III-01-C HOSPICE PALLIATIVE CARE TELEPHONE PROTOCOLS FOR WESTERN CANADA CALL CENTRE PROGRAMS: A TELENURSING INNOVATION Carolyn Tayler, RN, BN, MSA, CON(C); V. Clark, RN; M. Aherne, BComm, MEd; J. Béasse, MA; C. Brenneis, RN, MHSA; A. Einsiedel, PhD; L. McManus, RN, BN, MPA; M.J. Paquin, RN, MSc; A. Syme, RN, MN; C. Taylor, RN. BSN, MS; The Pallium Project – Phase II Background: Within the last ten years, call centre programs were launched in Alberta (AB), British Columbia (BC), Manitoba (MB), and Saskatchewan (SK), with start dates ranging from 1994 (MB) to 2003 (SK). This service is a creative approach to the principle of primary health care and the potential for collaborative work among health disciplines and sectors. Project Goal: To provide palliative patients, caregivers and the public living in Western Canada 24/7 Hospice Palliative Care (HPC) telenursing access to HPC assessment, information and referral to appropriate existing resources. Project Description: This nursing project meets the needs expressed by Canadians in a national HPC survey. In fact, 50% of respondents indicated that they would use a provincial telephone or telehealth service for HPC information (Ipsos-Reid, 2004).The project supports the development and integration of HPC telephone protocols for Western Canada call centre programs by March 31, 2006. This has a potential for ramification across Canada. Focus of the Presentation: This presentation will detail the development of the project, its status and outcomes as of September 2005. Conclusion: This telenursing innovation has the potential to affect the lives of many cancer patients and their families and improve primary care access to specialized services through an already existing and validated infrastructure of the provincial Call Centre Programs. III-02-B A DEMONSTRATION OF TEAM EFFORT: MANAGING AN OUTBREAK OF VANCOMYCIN RESISTANCE ENTEROCOCCI ON A MEDICAL AND RADIATION ONCOLOGY UNIT Eleanor Miller, RN, BScN, MEd; Catie Challoner, RN; Mena Carengi, RN, BScN; Dr. Richard Fralick, MD, CCFP; Carmen Gosselin RN; Sunnybrook and Women’s College Health Sciences Centre, Toronto, Ontario The impact of an outbreak of Vancomycin Resistant Enterococci (VRE) poses a challenge and risks for patients and staff. The application of effective teamwork, collaboration and strategic focus are essential for managing the outbreak that had the potential of sabotaging the effective function of a patient care unit. From August 2004 to November 2004 a total of 9 confirmed cases of VRE were identified on the unit. Following several meetings with key players within the organization, an out-break was confirmed. As a team, we acted quickly to abort this outbreak. Various measures were implemented to control the outbreak including, 80% increase in staff core competency training and certification in infection control. Other interventions include placement of patients with VRE in private rooms, cohorting of patients and nursing staff, strict surveillance of all patients admitted and discharged from the unit and the re-training of support staff that clean the patients’ rooms. Further strategies include daily double cleaning of patient’s rooms, and several measures of designated equipment to each patient. With such aggressive measures the outbreak was eventually controlled. This presentation will highlight the cooperative effort of the team, strategies implemented and lessons learned from this crisis. III-02-C PRIMARY NURSING IN RADIATION ONCOLOGY: THE PAST, THE PRESENT AND THE FUTURE III-03-A IMPLEMENTING THE WCCNR STOMATITIS STAGING SYSTEM Gail Monk, RN, CON(C); Donna Gies, RN, CON(C); Tom Baker Cancer Centre, Calgary, Alberta. Karin Olson1, RN, PhD; Cindy Cummings-Winfield2, RN, BScN, CON(C); 1 Univeristy of Alberta; 2Cross Cancer Institute, Edmonton, Alberta The Radiation Oncology Nurse is a specialist in the care of individuals receiving radiation therapy as a primary or adjuvant treatment for cancer. The nurse must be experienced in all aspects of cancer care and work with many members of the healthcare team to coordinate services and ensure quality patient care. The role of the nurse is multidimensional and has evolved in response to the escalating number and complexity of patients. In the past the role of the RT nurse was not well defined and was basically one of trouble shooting and support. The patient experiencing significant radiation toxicity was often admitted to the hospital for symptom management until completion of their treatment. Today most symptoms and concerns can be effectively managed on an outpatient basis. As patients continue to present with more complex problems, knowledge and ingenuity will be key in meeting their needs. In previous studies, Canadian oncology nurses identified the need for a valid and reliable stomatitis severity assessment tool. A tool developed from interviews with nurses, dentists and physicians was developed to meet this need, tested for reliability and validity and published in the August 2004 issue of the Canadian Oncology Nursing Journal. We are now in the process of implementing this tool as a component of standard nursing care in our hospital. This paper will outline our implementation protocol, plans for evaluation and future directions for stomatitis interventions. In this presentation, we will share programs we have implemented, including the Patient Care Model and describe how the Primary Nurse functions as part of the multidisciplinary team in the RT department at our Cancer Centre. We will discuss how the development of collaborative approaches to patient care enhances the quality of care and improves job satisfaction for all disciplines. We will present ideas for future goals of nursing in Radiation Oncology. III-03-B DEVELOPMENT OF AN EVIDENCE-BASED ORAL CARE GUIDE FOR HEMATOLOGY/ONCOLOGY PATIENTS III-03-C RISK PERCEPTION AND NATURAL HEALTH PRODUCTS IN PEOPLE LIVING WITH CANCER Prisco Salvador, RN, MScN; Lillian Martinez, RN; Kiing Eng Chan, RN; Princess Margaret Hospital, Toronto, Ontario Lynda G. Balneaves 1, RN, PhD; M.J. Verhoef; H. Boon; J. Carey. 1 School of Nursing, University of British Columbia This project describes one inpatient unit’s experience in developing and managing oral mucositis in patients diagnosed with hematological malignancies. The purpose of this study was to explore the risk perceptions of people with cancer using natural health products (NHPs). This study was a secondary analysis of three qualitative studies exploring NHP utilization across diverse cancer populations. Indepth, open-ended questions were conducted with over 30 individuals with cancer. The analysis focused on participants’ perceptions of risk related to NHPs and how risk perceptions influence treatment decisions. Participants reported taking part in a “balancing” process as they made decisions about NHPs. Therapies perceived to “do no harm” were considered to be safe and appropriate choices. NHPs were perceived to hold fewer safety risks than conventional treatments and were described as “natural” and “supportive”. Risks that were commonly mentioned included loss of support from physicians, cost, false hope, and interactions with conventional cancer therapies. Risk perceptions about NHPs were influenced by the degree of trust held in those giving advice and information sources used and by participants’ previous experiences with NHPs. Anecdotal stories from cancer survivors were particularly influential in participants’ treatment decisions. Individuals with cancer have relatively low risk perceptions about NHPs and rely on lay sources of information for treatment decisions. The findings raise concerns about the safe and informed use of NHPs and highlight the need for educational strategies that support accurate risk perceptions in people living with cancer. Oncology nurses have identified oral mucositis as a primary concern that adversely affects hematology/oncology patients undergoing chemotherapy. Despite improvements in treatment protocols (e.g., use of growth colony stimulating factors and therapeutic doses of antibiotics) over the last decade, the incidence and severity of oral mucositis remain significant. Cognizant of the impact of oral mucositis on a patient’s psychological well-being and quality of life, a core group of oncology nurses took a leadership role to better manage oral mucositis leading to the development of a unit-based oral care guide that can be used in any oncology settings. The group selected the Neuman systems model (Neuman & Fawcett, 2002) as a conceptual framework and synthesized information derived from the literature and from their clinical practice experiences. An oral care flowchart was also developed to ensure coordinated and continuous delivery of oral care and other services to the patients. Educational presentations for staff RNs and other healthcare providers were conducted to familiarize them about the oral care guide. The implementation of an oral care guide as a primary preventive intervention has the potential to minimize the occurrence or reduce the severity of oral mucositis after chemotherapy. III-04-A WEB-BASED LEARNING – IS IT THE NEXT STEP IN ONCOLOGY PALLIATIVE CARE EDUCATION? III-04-B REGISTERED NURSES 2005 LEARNING NEEDS SURVEY ACROSS THE CONTINUUM OF CANCER CARE-PRELIMINARY RESULTS Vicki Lejambe, RN, BScN, CON(C); Saint Elizabeth Health Care, Markham, Ontario Linda Robb Blenderman, RN, BNSc, MSc, CON (C); 2Margareth Santos Zanchetta, PhD, DN, MNSc; 3Brenda Weir, RN, BScN, MBA; 4Linda Morgan, RN, BNSc., CON(C); 5Jane Warner, RN, BNSc, MSc, CON(C), 2 Ena Howse, RN, PhD; 1Cancer Centre of Southeastern Ontario at Kingston General Hospital, 2Queen’s University, 4 All Care Health Services and 5Hotel Dieu Hospital-Kingston, Ontario, 3 Northumberland Hills Hospital, Cobourg, Ontario Creating an environment of continuous learning and delivering standardized, evidence based oncology palliative care education presents unique challenges in today’s health care environment. Highly mobile, geographically dispersed clinicians combined with complex care requirements and an increased body of knowledge, have resulted in the need to transform oncology palliative care education. We have harnessed the power of the intranet to provide nurses’ access to evidence based education, on line resources, and opportunities for synergistic learning about oncology palliative care. This innovative approach provides an “anytime and anywhere” environment of knowledge creation. Built on the principles of adult education, and collaborative learning, our interactive web-based solution supports nurses in advancing their knowledge and practice in oncology palliative care. This presentation will describe the online learning environment, the educational content, and the knowledge resources within the webbased education program. Evaluation results will be shared and linked to enhancements required for the further development and improvement of this program. Lessons learned will be shared regarding implementation and change management strategies, along with the identified supports required for successful transformation of professional development and learning in oncology palliative care for health care professionals. In Ontario, cancer is recognized as a major health problem. Assisting individuals to live well with cancer is a challenge that nurses in cancer care can meet when they are educated and apply standards of care. Inconsistencies in levels of oncology nursing knowledge and expertise were identified as a priority for the Regional Oncology Nursing Council of Southeastern Ontario. The council will contribute to the improvement of regional cancer care with the results of a needs based education program. A Learning Needs Survey of nurses across the care continuum working with individuals and families with or at risk for cancer will provide the basis. The goals of the survey are to establish a profile of nurses in cancer care, identify their education needs, current education resources and preferred modes of learning. The survey instrument used was a modified version of the “Nurses Needs Assessment in Cancer Care Education” developed by Cancer Care Nova Scotia (CCNS) in collaboration with the Canadian Association of Nurses in Oncology (CANO). The presentation will share preliminary results and how they may provide direction in furthering education in cancer care for Southeastern Ontario. III-04-C IMPLEMENTING REGIONAL STRATEGIES TO STRENGTHEN KNOWLEDGE TRANSLATION FOR ONCOLOGY NURSES III-05-A (English) – refer to page 73 for French PREOPERATIVE INFORMATION SESSION FOR WOMEN WITH GYNAEOLOGICAL CANCER 1 Joanne Brodeur, BSc; Thérèse Vincent, BSc; Nicole Tremblay, MSc, CSIO(C); Lucie Bédard, BSc, MBA; Jacinthe Brodeur, BSc, CSIO(C); Chantal Bélanger, BSc; Josée Beaudoin, Dt.P. clinicienne; Centre Hospitalier de l’Université de Montréal. Linda Robb Blenderman, RN, BNSc, MSc. CON(C); 2Brenda Bass, RN, HBSc. (Zoology), BScN, MBA; 3Brenda Weir, RN, BScN, MBA; 4 Jane Warner, RN, BNSc, MSc.; Dorothy Broeders-Morin5, RN, DHA; 1 Cancer Centre of Southeastern Ontario at Kingston General Hospital; 2 Ontario Breast Screening Program-Southeast Region; 4Hotel Dieu Hospital and 5St. Elizabeth’s Health Care-Kingston, Ontario; 3 Northumberland Hills Hospital, Cobourg, Ontario Access to timely oncology nursing knowledge is increasingly complex across a variety of settings and environments resulting in barriers to care coordination and evidence-based practices. To create an effective and supportive professional environment while addressing contextual barriers the Regional Oncology Nursing Council of Southeastern Ontario lobbied and received resources to implement a regional Website. The Website will act as a knowledge translation vehicle for enhanced information dissemination and implementation of regional evidence-based cancer care. This presentation will outline the steps involved in planning, implementing, marketing the Website and illustrate its usefulness to direct care nurses, students, educators, administrators and researchers. This presentation will contribute knowledge on how websites can assist nurses in accessing current information in their daily practice. In recent years, the development of the role of a nurse navigator and the creation of a continuous quality improvement team for gynaecological oncology care allow for the identification of areas for improvement in the care provided. Among these, the need to better plan for the return home of women who have had gynecooncology surgery was earmarked as a priority. Even though a lot of significant effort was made by the team to prepare these patients’ release, many problems surfaced only once the patient returned home. Fatigue, difficulty to care for oneself, various worries associated with surgery and anxiety were identified as frequent problems. At the beginning of 2005, following this study, a project of information and preoperative education sessions intended for these patients was started. The purpose of these sessions is to better inform the patients about the surgery and detect problem situations before admission so that they can be corrected beforehand. The project leaders will present the contents of the program and various resulting observations. IS NOW THE TIME REGARDING EXERCISE? III-05-B TO MAKE RECOMMENDATIONS Nicole Temblay, MSc, CSIO(C); Hôpital Notre-Dame For many years, the number of articles on the benefits of exercise has been multiplying. The effects of exercise have also been studied in oncology, particularly as a means of decreasing fatigue associated with cancer. The findings are that exercise is definitely an effective means. Consequently, in various oncology centres, many nurses are encouraging cancer patients to exercise in order to fight fatigue. However, at what frequency, at what intensity, for how long and over what period of time? Does research data now allow us to answer these questions? After reviewing the literature, the author will discuss the various research results in order to guide this aspect of practice. SOMMES NOUS À L’HEURE DES RECOMMANDATIONS EN MATIÈRE D’EXERCICE? Depuis de nombreuses années, les écrits sur les bienfaits de l’exercice sur la santé se multiplient. Dans le domaine de l’oncologie, l’exercice a été également étudié, notamment comme intervention pour diminuer la fatigue reliée au cancer. Il en est ressorti que l’exercice est bel et bien un moyen efficace en ce sens. Il s’ensuit que, dans les divers centres d’oncologie, de nombreuses infirmières incitent maintenant les personnes atteintes de cancer à faire de l’exercice afin de mieux lutter contre la fatigue. Mais à quelle fréquence le faire, à quelle intensité, quelle doit en être la durée et pour combien de temps ? Les données de recherche permettent-elles, d’ores et déjà, de répondre à ces questions ? L’auteure, s’inspirant de revues des écrits sur le sujet, discutera des divers résultats de recherche afin de guider la pratique en ce sens. III-05-C (French) LA VIE APRÈS LES TRAITEMENTS POUR UN CANCER: QUELQUES PISTES D’ACTION POUR MIEUX PRÉPARER LES PATIENTS AUX DIFFICULTÉS DE L’APRÈS-TRAITEMENT. Le cancer provoque un bouleversement chez la personne atteinte et ses proches. La fin des traitements à visée curative est habituellement perçue comme un soulagement et le début du retour à la « vie normale ». Cependant, pour beaucoup de personnes, cette étape de l’après-traitement est lourde de difficultés et elles réalisent alors que la vie ne sera plus jamais pareille à ce qu’elle était avant le cancer. Tant sur le plan physique que psychologique, social et spirituel, la maladie a laissé des traces. Comment vivre maintenant avec l’incertitude et la crainte de la récidive à apprivoiser, le sentiment d’être abandonné par l’équipe traitante, la lenteur de la récupération physique et la persistance de la fatigue, les changements de l’image corporelle, etc. À partir de la littérature et de la clinique, cet atelier abordera les principales difficultés vécues par les patients dans l’après-traitement et les moyens élaborés par notre équipe pour mieux préparer les patients à cette étape. III-05-C (English) LIFE AFTER CANCER TREATMENTS: A FEW COURSES OF ACTION TO BETTER PREPARE PATIENTS FOR POSTTREATMENT PROBLEMS Nathalie Gravel, inf. BSc; Marie de Serres, MSc inf., CSIO(C); Geneviève Lambert, Travailleuse Social; Centre Hospitalier Universitaire de Québec, Québec City, Québec Cancer deeply affects an individual and their loved ones. The end of curative treatments is usually seen as a relief and the beginning of a return to a “normal life”. However, for many people, this posttreatment stage has many problems and they realize that life will never be the same as it was prior to the cancer. From physical, psychological, social or spiritual perspectives, the disease leaves deep marks: how to live with the uncertainty, and fear that the cancer will recur, the feeling of being abandoned by the treatment team, the slow rate of physical recovery and persistent fatigue, the change in body image, etc. Based on literature and clinical practice, this workshop will address the main problems confronting patients once the treatments are complete and the means developed by our team to better prepare patients for this phase. IV-01-D CLINICAL TRIAL ONCOLOGY NURSING – PART OF THE CANCER CARE TEAM Florence Kronstal, RN, BSN; Nancy Hartt, RN, BSN; Karn WilkieBoyd, RN, BSN; British Columbia Cancer Agency – Centre for the Souther Interior, Kelowna, British Columbia Medical decision making rests on evidence-based practice which is largely the result of clinical trials. The role of the Clinical Trials Nurse (CTN) is an added dimension to the specialty of oncology nursing. There is a need to have comprehensive knowledge of research methodology as well as standards of nursing practice to ensure safe and ethical patient care. The CTN coordinates all aspects of clinical trials including assessing patients and coordinating their care with other members of the cancer care team and a wide range of administrative and regulatory processes. Clinical trials are available for all tumor groups in the settings of curative, supportive and palliative care. Participating in a clinical trial is a unique experience for a patient. At our centre, the CTN is the primary oncology nurse for the trial participant and is therefore closely involved with the patient’s experience. A focus of patient care, education and advocacy is combined with data collection and protocol compliance requirements. This presentation will focus on the CTN as an integral member of the cancer care team. We will outline the unique highlights and challenges within this role as we seek to improve patient outcomes using the most advanced cancer treatments available. IV-01-F MEASURING OUTCOMES OF NURSE-LED CARE: IMPLICATIONS FOR PATIENTS, NURSES AND THE INTERDISCIPLINARY TEAM IV-02-D STATE OF THE SCIENCE REVIEW: DIAGNOSIS AND MANAGEMENT OF EPIDURAL SPINAL CORD COMPRESSION Tracy Truant, RN, MSN; Susan Bartnik, RN, BSN; Patti Devon, RN, CON(C); Mary Scott, RN; Joy Bunsko, RN, BSN, CON(C); Brenda Ross, RN, BSN, CON(C); British Columbia Cancer Agency, Vancouver and Surrey, British Columbia Milena Segatore, RN, MScN, MNI-PG; Karen Lock, RN, MN, CON(C); North York General Hospital, Toronto, Ontario A growing body of research based evidence is pointing toward improved outcomes for ambulatory patients receiving care within nurse-led clinics (Corner, 2003; Loftus & Weston, 2001). At one Provincial Cancer Agency, revisions to the ambulatory care delivery model included nurse-led Patient Support Clinics (PSCs) as an integral component which maximally aligns nursing resources with patient needs and complements the existing medically oriented clinics. Within the PSCs, Registered Nurses practice to their full scope to deliver care to patients and families that meet their expressed needs (e.g. symptom management; education; treatment decision making support, referral to resources; navigation of cancer care system, etc). Through implementation of PSCs, it is anticipated that patients will receive timely, professional nursing care that enhances satisfaction with nursing care, enables treatment to be completed on time, enhances self care ability, and improves quality of life. To ensure these outcomes were achieved through the implementation of nurse-led PSCs, a rigorous evaluation plan was articulated and implemented. Written surveys, interviews, and focus groups were utilized to gather data at baseline, three months and one year post implementation. This presentation outlines the plan and process used to evaluate the implementation of PSCs in the ambulatory setting, identifying outcomes for patients, nurses and the interdisciplinary team. Recommendations for future implementation and evaluation of nurse-led PSCs will be summarized. IV-02-E INDUCTION CHEMOTHERAPY FOR ACUTE MYELOID LEUKEMIA: A CASE STUDY FOR UNDERSTANDING ONCOLOGICAL EMERGENCIES Gail Macartney, RN, MSc(A), ACNP, CON(C), The Ottawa Hospital, Ottawa, Ontario About 3,900 new cases of leukemia are diagnosed each year in Canada. As the population ages, the incidence of acute myeloid leukemia (AML) appears to be rising, particularly in the population over the age of 60 years. Treatment-related myelodysplasia and leukemia in survivors of cancers diagnosed in childhood and young adulthood also appears to be rising. The goal of remission induction chemotherapy in AML is the rapid restoration of normal bone marrow function. This presentation will review the most standard remission induction regimen for AML. A case study will be used to highlight the possible complications that can occur as a result of this treatment. Oncologic emergencies related to this treatment will be reviewed including tumor lysis syndrome, disseminated intravascular coagulation and febrile neutropenia with a focus on nursing assessment and intervention. Epidural spinal cord compression (ESCC) is a neuro-oncologic emergency, which, if not diagnosed promptly, carries significant morbidity. History is often the key to diagnosis: Patients can often literally pinpoint the site of their lesion. However, radiologic investigation is critical to definition of the lesion and surgical planning. Magnetic resonance imaging modalities have revolutionized the evaluation of spinal cord and roots; computerized tomography (CT) remains invaluable for surgical planning especially when the architecture or stability of the spine is affected by the lesion. Plain X-rays, though frequently used, have a minimal role in the diagnosis of ESCC The goal of treatment – be it medical, radiologic and/or surgical - is preservation of existing neurological function and quality of life through aggressive pain control, decompression of neural elements and recreation or preservation of spinal stability. Definitive treatment is directed at eradicating or controlling the underlying malignancy. Even in the setting of aggressive disease, aggressive surgical palliation of cord compression may be appropriate to preserve quality of life. This session will review the emergency management of the patient once the diagnosis of ESCC is suspected: Following a discussion of investigative imaging modalities, surgical approaches to the spine will be discussed and illustrated. The session will conclude with a review of the current role of radiotherapy and adjunctive therapies. IV-02-F UNBLOCKING THE MYSTERY – THE MALIGNANT BOWEL OBSTRUCTIONS MANAGEMENT OF Shari Moura, RN, MN; CON(C), Sunnybrook and Women’s College Health Sciences Centre – Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario There are multiple factors that contribute to the suffering experienced by patients with advanced or end-stage cancer. Malignant bowel obstruction (MBO) is a frequent clinical complication for patients with advanced gastrointestinal cancer, gynecological cancer, or metastatic disease to the peritoneal cavity. The prevalence of MBOs in patients with gynecological or gastrointestinal cancers is generally unknown (Feuer & Broadley, 2003). Recent descriptive research suggests that the incidence of bowel obstructions ranges from 5% to 51% in patients with ovarian cancer and from 10% to 28% in patients with gastrointestinal cancer (Hardy, et al., 1998 & Jolicoeur & Faught, 2003). When patients and family members are dealing with the diagnosis of a MBO, the options explored with them include medical and surgical interventions to reduce or relieve MBO related symptoms. An understanding of the management of MBO is integral to the care of patients and their families in the midst crisis and the possibility of impending death. The paper will explore, appraise, and summarize evidence from scientific and descriptive research regarding the use of surgical and non-surgical interventions for MBOs for patients with advanced or end stage gynecological and gastrointestinal cancer. Knowledge gained in this presentation will strengthen cancer nurses understanding of the common symptoms experienced by patients who present with MBO, possible treatments and, nursing assessments required to evaluate the effectiveness of the treatment. IV-03-D OVARIAN CANCER AWARENESS: CHALLENGES AND FACILITATING FACTORS IN THE DEVELOPMENT AND DISSEMINATION OF INFORMATION PRODUCTS FOR CANADIAN WOMEN Fran Turner1, MS; Margaret I. Fitch2, RN, PhD; Elisabeth Ross3, MHSc; 1Ovarian Cancer Information Project; 2Toronto Sunnybrook Regional Cancer Centre; 3National Ovarian Cancer Association; Toronto, Ontario Although ovarian cancer is the fourth leading cause of cancer-related death in women and leading cause of death in gynecological malignancies, most women know little about this disease—many believe it is detected with a Pap smear. Developing and disseminating information about ovarian cancer to a range of audiences, including well women, has been the mandate of a three-year Canada-wide initiative. A needs assessment was conducted with women and health care professionals using phone interviews, focus groups and surveys to identify information gaps about ovarian cancer as a basis for new product development. A variety of strategies were also employed in the development and dissemination of awareness materials in English and French as well as in other languages (Portuguese, Chinese, Tamil and Punjabi). Collaboration with community agencies was essential in designing information materials for diverse cultural groups. Following the recommendations of a wide range of stakeholders (N=380), efforts at dissemination are directed toward going where the women are, integrating with existing initiatives, and using multiple approaches. This presentation will profile the awareness materials and describe approaches utilized to develop, disseminate and evaluate them. It will also address the challenges of creating information materials in different languages and of ensuring that they reach the intended audiences. IV-03-F NURSE-LED CHEMOTHERAPY ASSESSMENT CLINICS: A PILOT PROJECT INVOLVING ADJUVANT BREAST CANCER PATIENTS Patricia Bieronski, RN, BScN, CON(C); Margaret Samide, RN, CON(C); Maureen Watt-Smith, RN, CNCC(C); Donna Van Allen, RN, BHScN, CON(C); Grand River Regional Cancer Centre, Kitchener, Ontario At this fast paced Community Cancer Centre the medical oncologists spend an average of 4.8 hours per day doing assessments for patients on active chemotherapy. These oncologists see 230 new patients per year providing primary care for both hospitalized and ambulatory cancer patients. This pilot project of nurse-led assessment clinics considers the use of expert oncology nurses to assess a patient’s readiness for his/her next chemotherapy cycle. The pilot project was 6 months long. The first 3 months was devoted to development, orientation, education and early implementation of a nurse-led assess clinic. The final three months were considered ‘steady state’ and indicators were measured to evaluate the outcome. The purpose of this pilot was to establish if the use of expert oncology nurses to assess readiness for chemotherapy would improve patient access, management of current patient volumes, and ensure ongoing quality of care. Our presentation will introduce the evidence based assessment tool, algorithms for each potential area of concern, and the medical directives to support nursing practice. The results of the evaluation will be shared to establish this exciting new role for expert oncology nurses. IV-03-E THE JOURNEY BEYOND BREAST CANCER: EMPOWERING BREAST CANCER SURVIVOR;S WITH WELLNESS STRATEGIES Carole Beals, RN, BScN, CON(C); Tracey Keighley-Clarke, RN, BA, MScH (in progress), CON(C); Royal Victoria Hospital, Barrie, Ontario “Survivorship begins with diagnosis and continues for the rest of your life”. (Muller, 1990). Quality of life is gaining importance for breast cancer patients as treatment advances increase survivorship. Breast cancer survivors experience many demands of illness across the physical, psychological, social, and spiritual domains. Research has shown that once breast cancer patients end their active treatment, links to support are often ended. In 2002, the Royal Victoria Hospital, (RVH) Barrie received a grant from the Canadian Breast Cancer Foundation to develop a breast cancer retreat. The goal of the retreat was to “increase breast cancer survivor’s knowledge of wellness and health strategies post breast cancer treatment through a weekend retreat experience”, and “to provide survivor’s with life-long health strategies and a network of peers which could evolve into a healing community model”. Results obtained from the surveys and focus groups demonstrated that the information and education strategies utilized at the retreat improved the quality of life of the survivors. This presentation will examine how the Cancer Care Program at RVH used the results of the retreat findings to develop a survivorship model to provide information, education, and wellness strategies for all breast cancer survivors within our community. PSYCHOLOGICAL EXPERIENCE IN PATIENTS IV-04-D DISTRESS AND POST-SURGICAL PHYSICAL SYMPTOM COLORECTAL CANCER Vanessa Buduhan, RN, MN; University of Manitoba, Winnipeg, Manitoba Colorectal cancer (CRC) is the second most frequent cause of cancerrelated deaths among Canadians (NCIC, 2003). Patients often experience several physical and psychological symptoms from their cancer or related treatment (Zaza & Baine, 2002). The purpose of this study was to ascertain the prevalence rates of psychological distress (PD), physical symptom experience (PSE), and the relationship between these variables in post-surgical CRC patients. The Theory of Unpleasant Symptoms (Lenz et al., 1997) guided this descriptive, correlational study. PD was measured by the Hospital Anxiety and Depression Scale (Zigmond & Snaith, 1983), and PSE was measured by the Memorial Symptom Assessment Scale (Portenoy et al., 1994) in a convenience sample (n = 35). In this sample, the prevalence of PD post-surgically was 43%. The most prevalent physical symptoms reported were lack of energy (89%), pain (83%), and dry mouth (83%). There was a significant relationship between PD and the PSE (r = 0.573, p < 0.001). Open-ended questions revealed that many patients (~50%) had no concerns about hospital discharge. These findings suggest that many patients are experiencing significant psychological and physical symptoms post-operatively prior to hospital discharge. Furthermore, patients are unaware of potential problems that can occur once discharged home. Standardized screening and patient education emphasizing psychosocial care, symptom management, and about what to expect after surgery is necessary to ensure a successful transition from hospital to home. IV-04-E EXPLORING FAMILY NURSING PRACTICES IN ADULT ONCOLOGY SETTINGS Deborah L. McLeod1,2, RN, PhD; Dianne Tapp3, RN, PhD; Mary Campbell1, RN, MScN; Nancy Moules3, RN, PhD; Teri Crawford2, RN, MN; 1 QE II Health Science Centre; 2 Dalhousie University; 3 University of Calgary The experience of cancer is often devastating, affecting many aspects of a family’s life. Families clearly desire competent care, understandable information, involvement in decision-making about treatment and compassionate recognition of both patient and family members’ distress. However, there are many barriers that make it difficult for nurses to provide family nursing in our individually focused health care systems. Even in the face of such barriers however, nurses find ways to respond to the needs of families but how that care is lived out in practice is poorly understood and often invisible. Family nursing practices in oncology settings have rarely been studied and consequently are not well described in the literature. In this presentation, we report on the first phase of a three phase study designed to explore, describe, and interpret family nursing practices in an adult ambulatory care oncology setting. The purpose of the project is to understand more about how nurses care for families. Specifically, how do they support the involvement of families and address their concerns and distress given the limitations of the system. In the first phase, participant observations and interviews were completed with 10 nurses and 10 families. The interviews and field notes were transcribed and interpreted in the hermeneutic tradition. Exemplars of excellence as well as identified barriers to family care will be discussed. Giving voice and visibility to excellence in family nursing practices opens up possibilities to strengthen this aspect of oncology nursing practice and education. IV-05-D BENEFITS AND LIMITATIONS OF TELEPHONE TRIAGE IN ONCOLOGY Nicole Tremblay1, MSc inf. CSIO(C); Jacinthe Brodeur, BSc inf., CSIO(C); Julie Piché, BSc inf., CSIO(C); 1 Hôpital Notre-Dame In Canada, telephone triage or telephone consultation service in oncology care will soon celebrate its tenth anniversary. Even though the telephone is the fastest and most effective way to use professional expertise between two appointments1, does this method, which was implemented in numerous oncology centres, meet the needs of cancer patients? The authors will review Canadian experiences in this area and present a report on the two years of operation of a Quebec telephone consultation service. They will also address the legal and training issues. Various data regarding the accessibility and continuity of care as well as the prevention of certain complications and the reinforcement of the educational aspects will be presented. The possibilities and the limitations of such a service as an alternative to the emergency room will also be discussed. Stacey, D. & Fawcett, L. (1997). Telephone triage: An important role for oncology nurses. Canadian Oncology Nursing Journal, July 1997, 178-179. BENFAITS ET LIMITES DU TRIAGE TÉLÉPHONIQUE EN ONCOLOGIE Au Canada, dans les milieux de soins oncologiques, le triage téléphonique ou service de consultation téléphonique fêtera sous peu son dixième anniversaire. Bien que le téléphone constitue le moyen le plus efficace et rapide de recourir à une expertise professionnelle entre deux rendez-vous1, ce moyen mis en place, dans bon nombre de centres d’oncologie, répond-il aux besoins des personnes atteintes de cancer ? Les auteures feront un retour sur les expériences canadiennes à cet égard et présenteront le bilan de deux années de fonctionnement d’un service québécois de consultation téléphonique. Elles aborderont aussi les enjeux de la formation et les aspects légaux. Diverses données concernant l’accessibilité et la continuité des soins ainsi que la prévention de certaines complications et le renforcement d’aspects éducatifs seront présentées. Les possibilités et les limites d’un tel service en tant qu’alternative à l’urgence seront également discutées. 1 Stacey, D. et Fawcett, L. ( 1997 ). Telephone triage : An important role for oncology nurses. Canadian Oncology Nursing Journal, juillet 97, 178-179. IV-04-F EFFECTIVE COMMUNICATION IN ACUTE CANCER CARE: PERSPECTIVES OF PATIENTS, FAMILY MEMBERS AND NURSES Fay J. Strohschein1, MSc (candidate); Sarah Thirlwell1, 2, RN, MSc; Shona Hutton2, RN, BSc (candidate); Antoinette Ehrler2, RN, BSc; Hélène Ezer1, RN, PhD; 1 McGill University; 2 Sir Mortimer B. Davis Jewish Hospital; Montreal, Quebec Effective communication is a core element of a quality cancer care environment and has been identified as a priority in cancer nursing research. Communication can directly impact on health and functional outcomes for patients, influence coping and adjustment to illness for patients and their family members, and affect the work-related stress experienced by nurses. However, there is little recent empirical evidence of what comprises effective communication in acute cancer care. This presentation will describe the results of a qualitative research study that examined experiences of effective communication in acute cancer care from the perspectives of patients, family members and nurses. Data were obtained through semi-structured interviews and were analyzed using grounded theory methodology. The findings of this study may be used to guide nurses in developing evidence-based strategies to facilitate effective communication in acute cancer care. In addition, the findings of this study may be used to guide nurse administrators’ interventions in promoting an environment conducive to effective communication between patients, family members and nurses, thus contributing to quality cancer care. IV-05-E (English) THE POSITIVE EFFECTS OF THE USE BY NURSES OF A SIMPLE DELIRIUM SCREENING TOOLS WITH PATIENTS IN ONCOLOGY AND PALLIATIVE CARE Marie de Serres, MSc inf., CSIO(C); Pierre Gagnon, MD, FRCP; Jean-David Gaudreau, PhD; Centre Hospitalier Universitaire de Québec, Québec City, Québec Delirium is a complication that occurs occasionally with patients in oncology and frequently with palliative care patients. As delirium fluctuates, it is only through constant surveillance that it is possible to detect it early and prevent it from getting worse. This workshop will present the experiments in the use of a delirium screening instrument in two institutions: a palliative care home and an hemato-oncology and bone-marrow transplant unit. In palliative care, the Confusion Rating Scale (CRS), a small and simple tool, has been used by nurses since 1997 (Gagnon, Allard, Masse et al., 2000). An improved version of the CRS was later validated for oncology and bone-marrow transplant patients. This new scale has been used for three years and is called “Échelle de dépistage du délirium” [Delirium Screening Scale] (Gaudreau, Gagnon, Tremblay et al., publication pending). Caregivers observed concrete results after using these tools: decrease in the number of patients having severe delirium, decrease in the number of patients needing constant surveillance, reduction in the use of restraints. The screening tool and the results of its use will be presented in this workshop. IV-05-E (French) LES EFFETS POSITIFS DE L’UTILISATION PAR LES INFIRMIÈRES D’UN OUTIL SIMPLE DE DÉPISTAGE DU DÉLIRIUM CHEZ LES PATIENTS EN ONCOLOGIE ET EN SOINS PALLIATIFS Marie de Serres, MSc inf., CSIO(C); Pierre Gagnon, MD, FRCP; JeanDavid Gaudreau, PhD; Centre Hospitalier Universitaire de Québec, Québec City, Québec Le delirium est une complication qui se présente occasionnellement chez les patients en oncologie et fréquemment en soins palliatifs. Le delirium étant fluctuant, c’est par une surveillance constante qu’il peut être possible de le dépister précocement et d’éviter que le problème s’aggrave. IV-05-F (English) LITERATURE REVIEW TO DEVELOP AN EVIDENCE-BASED TOOL FOR THE INITIAL ASSESSMENT OF ONCOLOGY PATIENTS France Robert1, inf. BSc, CSIO(C); Johanne Gagnon2, inf. PhD; 1 Centre Hospitalier Universitaire de Québec, Hôtel-Dieu de Québec; 2 Faculté des Sciences Infirmières, Université Laval, Québec Our approach is part of a research internship at the Bureau de transfert et d’échange de connaissances (BETC) [Office of knowledge transfer and exchange] that involves a partnership between Laval University’s Faculty of Nursing and a teaching hospital with a supraregional focus in oncology. The objective was an evidence-based improvement of the initial assessment. Cet atelier présentera les expériences d’utilisation d’un instrument de dépistage du delirium dans deux établissements: une maison de soins palliatifs et une unité d’hémato-oncologie et greffe de moelle. En soins palliatifs, le Confusion Rating Scale (CRS), un outil bref et simple, est utilisé par les infirmières depuis 1997 (Gagnon, Allard, Masse et al., 2000). Une version améliorée du CRS a ensuite été validée auprès d’une clientèle d’oncologie et de greffe de moelle. Cette nouvelle grille est utilisée depuis trois ans et est appelée Échelle de dépistage du délirium (Gaudreau, Gagnon, Tremblay et al., sous presse). L’utilisation de ces outils a apporté des résultats concrets observés par les soignants: diminution des patients qui présentent un délirium sévère, diminution du nombre de patients nécessitant une surveillance constante, réduction des contentions . On présentera dans cet atelier l’outil de dépistage et les résultats de son utilisation. Method: databases such as Current Contents, CINAHL, Medline, Cochrane Library and Psyclit were consulted for the period 1990 to 2004. This presentation examines work proposals that emerge from the literature review. The following elements are available to structure the collection tool: extensive knowledge of the patients’ needs, selection of a conceptual framework, use of practice standards such as NIC, NANDA or CONEP, the use of a theoretical model on change management, an implementation procedure using a quality improvement approach, selection of a compatible format with electronic health records. IV-05-F (French) RECENSION DES ÉCRITS POUR L’ÉLABORATION D’UN OUTIL D’ÉVALUATION INITIALE DU PATIENT EN ONCOLOGIE À PARTIR DE RÉSULTANTS PROBANTS IV-06-D (Abstract 1 of 2) WORKLOAD MEASUREMENT FOR ONCOLOGY ADVANCED PRACTICE NURSES: HOW CAN THE IMPRINT TO PRACTICE BE EVALUATED WITHOUT IT? France Robert1, inf. BSc, CSIO(C); Johanne Gagnon2, inf. PhD; 1 Centre Hospitalier Universitaire de Québec, Hôtel-Dieu de Québec; 2 Faculté des Sciences Infirmières, Université Laval, Québec J. Colleen Johnson, RN, MN, CON(C); Cindy Murray, RN, MN; Princess Margaret Hospital, University Health Network, Toronto, Ontario Notre démarche se situe dans le cadre d’un stage de recherche au Bureau de transfert et d'échange de connaissances (BTEC) qui implique un partenariat entre la Faculté des sciences infirmières de l’Université Laval et un centre hospitalier universitaire à vocation suprarégionale en oncologie. L’objectif visait l’amélioration de l’évaluation initiale basée sur des résultats probants. MÉTHODE: Les banques de données telles Current Contents, CINAHL, Medline, Cochrane Library et Psyclit ont été consultées de 1990 à 2004. Cette communication présente des propositions de travail émergentes de la recension des écrits. Pour structurer l’outil de collecte on retrouve les éléments suivants : la connaissance approfondie des besoins de la clientèle, le choix d’un cadre conceptuel, l’utilisation de standards de pratique comme le NIC, le NANDA ou le CONEP, l’utilisation d’un modèle théorique sur la gestion du changement, un mode d’implantation qui respecte une démarche d’amélioration de la qualité, la sélection d’un format compatible avec l’informatisation du dossier médical. DISCUSSION: La recension des écrits a démontré un manque d'études scientifiques avec des méthodes rigoureuses permettant de produire des résultats probants sur l'efficacité des outils de collecte de données en oncologie. Workload measurement should be an expectation for every oncology advanced practice nurse. In an environment of continuous fiscal restraint advanced practice nurses have an obligation to demonstrate their value. Workload measurement is one strategy that can be used to communicate the importance of their contributions to the administrative members of the healthcare team. However, measuring the activities of advanced practice nurses is a complex and intimidating process. The role expectations for advanced practice nurses involve both clinical and non-clinical activities therefore consideration to both areas must be included. The clinical component for advanced practice nurses involves the time and/or activities related to patient care including interviewing, assessments, interventions and telephone contacts. The non-clinical component for advanced practice nurses includes the leadership, teaching, research and professional activity domains of practice. This presentation will review the literature regarding workload measurement for APNs as well as the experience of advanced practice nurses from one oncology tertiary centre that have been using a variety of measurement tools for the past four years. Discussion: the literature review reveals a lack of scientific studies with rigorous methods producing conclusive results on the effectiveness of data collection tools in oncology. IV-06-D (Abstract 2 of 2) ADVANCED PRACTICE NURSING IN ONCOLOGY: SHARING THE EXPERIENCES OF YESTERDAY AND TODAY TO SHAPE THE PRACTICE FOR TOMORROW Cindy Murray, RN, MN; J. Colleen Johnson, RN, MN, CON(C); Princess Margaret Hospital, University Health Network, Toronto, Ontario Advanced practice nurses specializing in oncology are practicing in many provinces across Canada. The roles and issues for oncology advance practice nursing are constantly evolving and there are numerous similarities and differences depending on provincial legislation, political environments and health care institutions. In many cases advanced practice nurses are practicing in healthcare settings as the solitary advanced practice nurse. In larger settings, with multiple oncology advanced practice nurses, busy daily practices leave them little time left to share their experiences, issues or concerns with fellow advanced practice nurses. This workshop is an opportunity for advanced practice nurses to come together to share experiences and discuss issues relevant to advanced practice nursing such as medical directives, role responsibilities, practice patterns, collaborative relationships, and credentialing. From novice to expert, this workshop will provide a learning opportunity for currently practicing oncology advanced practice nurses, nurses considering a future as an advanced practice nurse and/or administrators wanting to learn more about the issues that affect the role. Sharing past and present experiences may help to enhance the future role of advanced practice nurses in oncology. V-01-B AN EXPLORATORY STUDY OF ONCOLOGY HEALTH PROFESSIONAL’S KNOWLEDGE, EXPERIENCES AND ATTITUDES OF BEST PRACTICE USE OF ADVANCE DIRECTIVES WITHIN AN ADVANCED CARE PLANNING PROCESS Janice Wright, RN, MS, ACNP; Susan Robinson RN, MN; Princess Margaret Hospital, Toronto, Ontario Advance care planning refers to the process of preparing for likely scenarios near the end of life and includes identification of a person’s knowledge of their medical history, condition, values, preferences, and personal and family resources. An advance care directive (ACD) is a document that describes an individuals future preferences for medical treatment. It is done prior to an event that would render one unable to express those preferences. There is a growing societal expectation that personal wishes will be respected. At the same time there is a need for improved clinical processes whereby an incompetent person’s prior wishes about end of life decision making are known and there is clarity in communication at the time that critical decisions need to be made. Prior to considering implementation of an institutional process of best practice use of advanced care directives it was essential to explore Oncology Health Professional’s knowledge, attitudes, experiences with Advance Directives and Advance Care Planning. The knowledge, attitude and experiences with Advance Directives of Oncology Health Professionals at a major comprehensive cancer centre has been examined using the KAESAD or Knowledge, Attitudinal, Experiential Survey on Advance Directives (Jezewski). Analysis of the survey responses in the four essential study objectives will be presented. V-01-A PROFESSIONAL ACCOUNTABILITY: A SURGICAL ONCOLOGY UNIT EXPERIENCE Mary Glavassevich, RN, BA, MN; Suman Iqbal, RN, CON(C); Anita Long, RN; Sunnybrook and Women’s College Health Sciences Centre – Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario The challenge for nurses to practice in a decentralized model, in which they are accountable for their practice, is well documented Porter O’Grady, 1992. A professional model of nursing is described as one in which the nurses are accountable for decisions about their practice and one that enhances stag satisfaction. Since 1997, staff nurses on a surgical oncology unit have been accountable for assessing and evaluating their nursing practice through the development of a unit-based nursing council. Nurses assume leadership roles as chair and co-chair of the unit council and are members of the hospital-wide nursing council. The patient care manager, Advanced Practice Nurse, and educator provide support, however, it is the nurses themselves who take the lead in addressing the nursing practice issues identified on the unit within the outlined terms of reference for the unit council. Nurses at unit based meetings focus on the standards of nursing practice developed within the organization, the College of Nurses of Ontario and the current national oncology nursing standards. The goal of focusing on nursing issues rather than operational issues requires particular skills and focus. The nurses are positive about this approach and have been pleased with the patients’ satisfaction survey results. Nurses feel that the council has contributed to the high quality care they are providing to their patients. This presentation will focus on the development of the unit council, challenges encountered and strategies utilized by the nurses to maintain momentum. TO “BSN” OR NOT TO “BSN” V-01-C Patti Devion1, RN, CON(C); Elizabeth Cooper1, RN, CON(C); Laurel Nicholson1, RN; Susan Hirowatari2, Student Nurse; Tracy Truant1, MSN; 1British Columbia Cancer Agency, Fraser Valley Centre, Surrey, British Columbia; 2 Kwantlen University College, British Columbia As of January 2005, a baccalaureate degree in nursing is the entry to practice standard for Registered Nurses in Canada (CNA, 2004). Many questions arise for diploma prepared nurses who have been working in the profession of nursing for many, many years and have a wealth of experience, expertise and knowledge. What about diploma prepared expert oncology nurses? How will this new CNA standard affect their practice and/or their views on returning to complete their BSN? How can employers and universities support diploma prepared nurses to return to school to attain their BSN? These are some of the questions that were asked of diploma and BSN prepared nurses. This issue was investigated by diploma prepared nurses employed at a Provincial Cancer Agency who have returned to university to attain their BSN. In collaboration with two University Schools of Nursing they undertook this project as part of their community development course. Using a variety of data collection techniques, common themes were identified by working nurses, employers and faculty members surrounding the struggles and frustration that returning RN’s experience in pursuit of higher education. This presentation will discuss some of the barriers and enabling factors identified by RN's along with some strategies to help employers and universities facilitate diploma prepared nurses to receive their BSN. V-02-A PATIENT FOLLOW-UP VIA VIDEOCONFERENCING: ADVANTAGES AND CHALLENGES TO PATIENTS AND HEALTHCARE PROFESSIONALS Nicole McDonald, RN; Audrey Oliver, RN; Terry Koski, RN, CON(C); Carolle Thibeault; Northeastern Ontario Regional Cancer Centre of the Hôpital Régional de Sudbury Regional Hospital, Sudbury, Ontario The long-term follow-up of oncology patients in a large geographical area creates many challenges. Barriers to patient adherence for follow-up often stems from the inconvenience of travel, especially in the winter months. Videoconferencing technology in Northern Ontario has provided the capability to connect to our patients in many communities for follow-up care. The utilization of this technology in our ambulatory oncology setting has increased dramatically over the last 2 years from a few cases to approximately 180 cases per month. With the increased use of this technology, primary nurses face increased responsibilities in managing patients. For example, as the primary nurse is not physically attending the patient, her assessment and interviewing skills must be enhanced to ensure the patient’s needs are being met. In addition to seeing well follow-up patients, physicians and nurses share test results, monitor side effects and address palliative care issues such as pain control. This presentation will outline the advantages for the patient, and also the challenges faced by the health-care team in managing such a large number of patients via this technology. Information collected from interviews of patients, physicians, nurses and clerical support will be reported and the perceived advantages and disadvantages will be discussed. V-02-C THE EFFECTIVENESS AND EFFICIENCY OF AN INDIVIDUALIZED TELEPHONE COUNSELING INTERVENTION FOR PEOPLE WITH CANCER Lynn Coulter 1, RN, MN; Barbara Downe-Wamboldt 2, RN, PhD; Lorna Butler 2, EN, PhD; Patricia Melanson 2, RN, MN; Janice Keefe 3, PhD; Jerome Singleton 4, PhD; David Bell 5, MD; Gina Browne 6, RN, PhD; Teri Crawford 2, RN, MN, Research Coordinator; 1 Queen Elizabeth II Health Sciences Centre, Halifax, Nova Scotia; 2 Dalhousie University, School of Nursing, Halifax, Nova Scotia; 3 Mount Saint Vincent University, Family Studies Gerontology, Halifax, Nova Scotia; 4 Dalhousie University, School of Health and Human Performance; 5 Dalhousie University, Faculty of Medicine; 6 McMaster University, Hamilton, Ontario Extensive evidence indicates that cancer patients suffer considerable emotional distress as a result of their disease and treatment. Psychological factors such as difficulty coping and poor adjustment to illness influences both quality of life and the use of health resources. Current literature clearly indicates a need to provide evidence-based interventions to increase the patient’s ability to cope successfully with their personal cancer experience. The aim of this study was to determine the effectiveness and efficiency of individualized problem solving counseling provided by registered nurses over the telephone for persons with cancer and to determine for whom and with what characteristics the intervention was most acceptable, effective and efficient. This study used a longitudinal, randomized controlled design to assess the effect and expense of usual clinic care (control group, n = 75) versus individualized problem solving counseling intervention (experimental group, n = 76) for patients diagnosed with breast, lung or prostate cancer. The intervention group, in addition to the usual follow-up care, was provided telephone problem solving counseling sessions over a 4 month period following surgery. Measures of adjustment to illness, depression, coping, and health resource expenditure were completed at baseline, post intervention (4 months) and at 8 months. The finding from this study and implications for practice will be the focus of this presentation. . V-02-B ONCOLOGY TELEPHONE PRACTICE GUIDELINES & ONLINE DOCUMENTATION: THE PERMANENT IMPRINT Patti Marchand, RN, MN, CON(C); Linda Klich, RPN; R.S. McLaughlin Durham Regional Cancer Centre, Oshawa, Ontario The past year has seen the introduction of telephone practice guidelines in our ambulatory oncology clinic. Consistency, continuity and confidence have not always been the hallmark of telephone practice in our institution. An education manual containing telephone nursing practice standards and symptom management guidelines and an interactive presentation including case studies were developed externally and shared with staff to launch their usage in our clinic. In addition, our center incorporated the guidelines into a pocket guide to ensure easy accessibility. The next necessary step was the inclusion of the guidelines into the current online documentation system. In collaboration with the information technology department, documentation screens were built, piloted and moved to “live.” Staff nurses addressing telephone calls in the middle of busy clinics, found that the user-friendly screens facilitated complete and efficient documentation, consistent with nursing standards. This presentation will enable nurses to view the documentation screens that were created and are now being utilized in the ambulatory oncology setting. An audit captured the details of the guidelines’ application and highlighted situations when the guidelines were not used, but should have been. These situations were further explored through interviews with individual nurses. Information gathered identified gaps in telephone practice, evident in both symptom recognition and management. These lessons learned will be shared to positively influence the imprint of documentation excellence. V-03-A BREAST CANCER INFORMATION DISSEMINATION STRATEGIES – FINDING OUT WHAT WORKS Margaret I. Fitch 1, PhD; Irene Nicoll 2, MBA; Sue-Keller-Olaman 3, PhD; 1 Sunnybrook and Women’s Health Sciences Centre; 2 Ontario Breast Cancer Information Exchange Partnership; 3 Ontario Breast Cancer Community Research Intiative; Toronto, Ontario Information about breast cancer is more available now than ever before, yet women still report that they received "no information" at the time of their diagnosis or treatment for breast cancer. The aim of this project was to help groups and individuals engaged in the dissemination of information about breast cancer learn the best strategies to use so all women will have easy access to that information. The qualitative research was conducted in two phases from November 2003 to August 2004. First, 28 breast cancer survivors were interviewed. Three themes emerged from these discussions: the shock of diagnosis; the onus being on the patient to search for information; and the different types of information that breast cancer survivors want. Interviewees also shared their negative and positive experiences in the cancer care system. Secondly, to learn multiple viewpoints, focus groups were held with breast cancer survivors in nine locations in Ontario (n=127) and three focus groups were conducted with information providers (n=25) using the three themes as a framework to guide the discussions. Participants validated the themes and identified two programs using “best practices” to provide information for women: a structured breast health centre in eastern Ontario and a peer support program operating in rural southwestern Ontario. The presentation will highlight the study findings that include implications for practice, education, and research. V-03-B NURSING SUPPORT PROGRAM TO DECREASE OR PREVENT SIDE EFFECTS OF CAELYX (PEGYLATED LIPOSOMAL DOXORUBICIN) IN PATIENTS WITH RECURRENT EPITHELIAL OVARIAN CANCER (REOC) Veronique. Lebel 1, RN; Nathalie Grenier 1, RN;; M. Gill 2, RN; T. Mullen 3, RN; K. Mitchinson 4, RN; M. Foster 5, RN; S. Lewis 6, RN; K. Seborn 7, RN; A. Rodgers 8, BSc; J-F. Pouliot 8, PhD; CHUM – 1 Hôpital Notre-Dame, Montreal, Quebec; 2 Tom Baker Cancer Centre, Calgary, Alberta; 3 Juravinski Cancer Centre, Hamilton, Ontario; 4 Royal Victoria Hospital, Barrie, Ontario; 5 Lakeridge Health Centre, Oshawa, Ontario; 6 Peel Memorial Hospital, Brampton, Ontario; 7 London Regional Cancer Centre, London, Ontario; 8 Schering Canada Inc., Pointe-Claire, Quebec Background: A significant long-term survival with Caelyx compared to topotecan was recently reported in a phase III randomized study of women with REOC (Gordon Gyn. Oncol. 2004). Caelyx is known to be relatively less toxic than topotecan and conventional doxorubicin, however side effects may lead to sub-optimal drug exposure and treatment discontinuation. Methods: A nursing support program was created to determine if patient education through proactive nursing intervention could decrease the occurrence and/or severity of side effects. Patients were educated about potential toxicities of Caelyx and received instructions on the prevention and management of side effects. Results: Caelyx was administered to 112 ovarian cancer patients as 2nd, 3rd and 4th line therapy in 51%, 34% and 15% of patients, respectively. The average dose of Caelyx was 40.4 mg/m2 (35-50) every 28 days for an average of 4.01 cycles (1-23). Clinical symptoms and/or radiological evaluation stabilized or improved in 69% of patients. Overall the frequency of adverse events, in these heavily pretreated patients, was similar to that observed in a previous phase III clinical trial (Gordon JCO 2001) where patients had received only one prior therapy. However, the incidence of grade 3/4 palmar-plantar erythrodysesthesia and mucositis were reduced from 21% to 4% and 8% to 3%, respectively. Conclusion: The nursing support program helped to reduce the severity of PPE and mucositis in patients receiving Caelyx for REOC. V-03-C MOVING PRACTICE FORWARD AT PRINCESS MARGARET HOSPITAL: NURSES TRANSFUSING AUTOLOGOUS PERIPHERAL BLOOD STEM CELLS Katherine Trip, RN, MN (ACNP); Norman A. Franke, MD; Princess Margaret Hospital, Toronto, Ontario The infusion of autologous peripheral blood stem cells has long been the domain of physicians. Building on literature from Australia, the physicians and nurses at our hospital developed a procedure that would enable Registered Nurses to transfuse thawed stem cells rather than having this remain a physician only responsibility. It was hoped that patients would tolerate the new method of infusion as well as or better than reinfusion by IV push. Engraftment data are routinely collected and show there is no delay in engraftment when stem cells are transfused rather than pushed into the circulation. This presentation will focus on the process of moving practice from a physician only responsibility to a shared responsibility between physicians and nurses. Outcome data regarding patient side effects and engraftment will be shared, as will the protocol utilized by our nurses. V-04-A SHOULD ONCOLOGY NURSES ACCEPT PRIVATE INDUSTRY SPONSORSHIP; IT IS ETHICAL WEIGHING, THE ODDS? V-04-B A CELEBRATION – RAINBOWS: THE MANY COLOURS OF ONCOLOGY NURSING Janis Stewart 1, BScN, CON(C); Shelagh Knight 2, RN; 1 Princess Margaret Hospital, Toronto, Ontario; 2 Astra Zeneca, Toronto, Ontario Cathy Doyle, RN, CON(C); Vicki Barton, RN; Marge Blokker, RN, BA, CON(C); Susan Collins, RN, MScN, ACNP, CON(C); Wendy Gillis, RN, MScN, ACNP, CON(C); Susan Ludlow, RN, BA; Gloria Murdoch, RN, MScN, ACNP, CON(C); Patricia Stalker, RN, BScN, CON(C); Angela Vinet, RN; London Health Sciences Centre, London, Ontario Oncology nurses have the luxury of often being in a situation where they can access paid education/financial support from pharmaceutical companies or they are offered an honorarium to give educational sessions on behalf of pharmaceutical companies. Should this practice exist and how do nurses draw the line and ensure they are not being unduly influenced? This presentation will inform the attendees about the currently published guidelines related to the sponsorship and marketing practices. The current Canada’s Research-Based Pharmaceutical Companies (Rx &D) have regulations regarding private industry sponsorship of health care professionals. The Oncology Nursing Society (ONS) and its affiliates have a set of policies that guide decision-making with regard to sponsorship and the National Institutes of Health (NIH) published an extensive report concerning conflict of interest for health care professionals. Two nurses who have had the unique experience to have worked in both the hospital sector and the pharmaceutical sector will present a selection of the currently published recommendations and guidelines. Having a clear understanding of these regulations will provide nurses with a framework to guide decision-making around accepting private sponsorship. A case study model will be used to present situations; the models will be based on real situations recounted by oncology nursing colleagues. In planning our 2004 cancer nursing conference, it was our goal to end the day with a celebration of oncology nursing using an audio/visual presentation format. Wanting to capture the experiences of nurses, we asked them what brings them joy, what gives them rewards and why they remain in such a demanding speciality. We then set about to videotape and photograph oncology nurses and patients. The overwhelming responses reflected their compassion, the importance of coworkers, the value of humour, and their unique relationships with patients. A physician and the daughter of one of the nurses also volunteered to provide their insights. Together with the interviews, photographs of nurses and patients, and a thoughtful selection of music, we created a 22 minute movie presentation titled: Rainbows: The Many Colours of Oncology Nursing. This movie exceeded our expectation. It not only invoked a celebration, but also laughter and tears leaving a lasting imprint as it touched nurses in a very personal way. It inspired a renewed awareness that together we share beliefs, values and passion in our relationships with our patients and with each other. The purpose of this presentation is to share the video depicting a glimpse into oncology nursing. V-04-C WHAT DO ONCOLOGY NURSES DO? Dauna Crooks1, RN, DNSc; Esther Green2, RN, MHSc; Mary Fergeson-Pare3, RN, PhD; Doris Howell3, RN, PhD; Debra Bakker4, RN, PhD; Joan Tranmer5, RN, PhD; Pat Sevean6, RN, PhD (candidate); Margaret Fitch7, RN, PhD; Laurel Plewes7, BScN; Shirley Sharkey8, RN; Nancy Lefevre8, RN, MScN; 1Hospital for Sick Children, Toronto, Ontario; 2Cancer Care Ontario, Toronto, Ontario; 3University Health Network, Toronto, Ontario; 4Laurentian University, Sudbury, Ontario; 5 Queen’s University, Kingston, Ontario; 6Lakehead University, Thunder Bay, Ontario; 7Toronto-Sunnybrook Regional Cancer Centre, Toronto, Ontario; 8Saint Elizabeth Health Care, Markham, Ontario The Ontario Role Function Study group, using survey techniques, examined the full scope of clinical role functions for clinical oncology nursing practice. Role functions included the following: assessment, prevention, medical directives, counseling, education, psychosocial support, evaluation and palliative care. Nurses were asked to self identify as specialized or advanced practitioners as per CANO descriptions. They noted what role functions they performed, if they did not perform the role function themselves, who did it. Finally, they identified the degree of independence in performing each function. We will present the data for selected role function categories as illustrations of the scope of practice of oncology nurses, identify areas of role overlap and clarify specifics of each role category, Survey results will be of value to educators and administrators in assessing and defining role parameters, and role definitions. In addition it will guide educators in nursing to create useful educational programming and clinical administrators to identify areas where nurses are underutilized in oncology care. V-05-B PREPARING ONCOLOGY NURSES: ORIENTATION REALITY IN 2005 Beverley Page1, RN, BScN, CON(C); Margaret Fitch, RN, PhD; Laurel Plewes, RN, BScN; 1Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario A worldwide shortage of nurses, altered hiring practices, shorter inpatient stays and increased patient acuity has contributed to changing orientation needs for ambulatory oncology nurses. Preparation of specialty oncology nurses is being challenged in various ways. Newly hired nurses must be prepared quickly to function competently in new roles and units and feel pressure from performance expectations. In one ambulatory cancer centre, nurses starting employment during 2003 and 2004 (n=21) were invited to participate in an intensive evaluation of their own orientation, identify pressures, strengths and weaknesses and make suggestions for improvement. Interviews were accomplished through focus groups and via telephone (n=16, 76.17%) and centred around questions designed by educator, clinical practice leader and managers. Results of the interviews yielded themes and key pressures for new nurses. They identified system weaknesses and educational needs and suggested creative educational approaches. These data are being integrated into the cancer centre’s revised nursing orientation program. New challenges in nursing practice frequently lead to identification of education needs and developing new strategies and innovations in nursing education. Sharing strategies and innovations allows oncology nurse educators to meet challenges, support new nurses and address the crisis of inadequate preparation for oncology specialty practice. V-05-A LEAVING OUR IMPRINT: A COLLABORATIVE ONCOLOGY NURSING EDUCATION PROGRAM INVOLVING THE CROSS CANCER INSTITUTE AND THE AGA KHAN UNIVERSITY HOSPITAL Tayreez Mushani-Kanji, RN, BScN, CON(C), CHPCH(C); Cindy Cummings-Winfield, RN, BScN, CON(C); Khurshid Khowaja, PhD; Cross Cancer Institute, Edmonton, Alberta The opportunity to collaborate with an institution in another continent has the potential to forge a long term relationship especially as it relates to the sharing of oncology nursing knowledge that will ultimately lead to enhanced patient care. The department of Nursing Education at the Cross Cancer Institute (CCI) had the unique occasion to partner with Nursing Education at the Aga Khan University Hospital (AKUH) in Karachi, Pakistan. The recognition of oncology nursing as a specialty at the AKUH was instrumental in establishing contact between the two institutions and the subsequent development of an oncology nursing education program. This presentation will begin by describing the events that lead to this unique collaborative educational endeavor. This will be followed by outlining key considerations such as culture, distance and lack of available oncology nursing resources in Karachi that impacted course design in Canada. The challenges inherent in teaching oncology nursing to practicing nurses whose first language is not English, coupled with the challenges encountered in a third world country will also be shared. The course was evaluated to ascertain participants’ self-perceptions, views on oncology nursing, theory assimilation and clinical application. The results of this evaluation will be presented. Finally, we will discuss how such an experience left an imprint on both sides of the oncology nursing world and planted the seeds for future collaboration. V-05-C CLINICAL LEADERSHIP IN ACTION – AN EVALUATION STUDY OF THE IMPACT OF CLINICAL LEADERSHIP DEVELOPMENT FOR ONCOLOGY STAFF NURSES Lynne Penton1, RN, MN, CON(C); Janet Rush2, RN, PhD; Sandra McFarlane2, RN, MHSc 3Juravinski Cancer Centre, Hamilton, Ontario; 1Registered Nurses Association of Ontario; 3McMaster University, Hamilton, Ontario Leadership can be found throughout an organization. Leadership is not limited to one person in any work setting. It is based on relationships and actions, not on positions. (Buzzotta et al. 1996) In the oncology nursing milieu as in other practice areas there has been renewed interest in the notion that every nurse has the ability to provide leadership in some way. There is also some evidence to suggest that previous beliefs about leadership as an inherent trait are untrue and that all nurses, given opportunity and understanding, can demonstrate leadership behaviours. This in turn may strengthen clinical practice, improve job satisfaction and create positive results in patient care outcomes while fostering nursing retention. Kouzes and Posner (2002) have identified the five measurable components of leadership behaviour; they can be measured using a valid and reliable tool. To explore these notions, a funded, approved study is underway in a Regional, Cancer Centre. This presentation will involve a discussion of the underlying values driving the project, the concept of leadership among oncology staff nurses, the study maneuver, and the methods for measuring leadership attributes. V-06-A (Abstract 1 of 2) A FIFTEEN- MINUTE FAMILY CENTRED NURSE ASSESSMENT IN ONCOLOGY Anne Plante, MSC inf.; Christiane Salée; Lucie Laporte, BSc inf.; Hôpital Charles LeMoyne, Greenfield Park, Québec Theme: family centred care, family nursing interventions, oncology assessment for new patients. Nursing Faculties and nursing directions of all institutions are investing a lot of efforts to promote family centred care in various settings. Those initiatives have improved results in care settings. Our regional hospital has worked in partnership with eight local oncology clinics to implement family centred care and family nursing interventions ``way of doing``. In the context of limited human and financial resources, it was quite a challenge. We structured a nursing assessment tool to evaluate all new patients in the oncology program. It is based on the ``15-minute family interview`` model from Wright and Leahey. The 15-minute family interview is not a strategic decontextual nursing tool. In fact, it is a flexible interview guide that is embedded in family nursing practice. It enhances the relationship between nurses and family. It promotes the nurse’s philosophical assumptions and obligations to relate adequately with families, especially in oncology. The use of this tool has changed not only nursing practices, but the whole team practice. VI-01-D A CONCEPT ANALYSIS OF SUFFERING LEADS TO THE HEALING AND TRANSFORMATION MODEL FOR MULTIDISCIPLINARY PSYCHOLOGICAL INTERVENTION Lynn Hryniuk1, RN, MSN; Wm. Hryniuk2, MD; 1CarePath Inc., Dundas, Ontario; 2Cancer Advocacy Coalition of Canada, Toronto, Ontario Psychosocial and spiritual interventions lack a coherent model for assessing needs of cancer patients and families, and multi-disciplinary care is frequently not sharply focused on meeting these needs. A concept analysis of Suffering yielded the “Transformation and Healing” model allowing for a more logical approach. The analysis determined how Suffering is defined, its causes, what are its preconditions, its natural history, and its positive and negative consequences: Suffering can end or lead to turmoil without resolve. With this sequence defined, (i.e. suffering exists, has a beginning, a process and an end), after careful interview each individual’s personal sources of Suffering can be understood, required interventions and care disciplines identified, and outcomes evaluated. Moreover, the points of entry for interventions can be defined more precisely and logically. Interventions can come from the individual’s own resources, or from health care professionals, spiritual and psychological counselors, family and friends. The informed patient can choose interventions from these according to need, interest, and ability. With insight and assistance, the Suffering can end more rapidly. At that end point “Healing” occurs and usually a different life views are acquired which is “Transformation”. V-06-A (Abstract 2 of 2) ONCOLOGY INTERDISCIPLINARY TEAM MEETING Anne Plante, MSc inf.; Christine Mimeault, BSc inf.; Hôpital Charles LeMoyne, Greenfield Park, Québec Themes: Health care teams, oncology team work, quality improvement Nurses, physicians and all other health care professionals are being asked to work on a team model in delivering their care. The knowledge that each health professional brings from their practice discipline, coupled with the theory of ``team working`` (methods to organize interdisciplinary clinical meetings) can greatly accelerate the opportunities for improvement in the quality of care and the quality of life for all oncology patients. A thirty minute video explains the process followed to implement such a vision. Support was given to all professionals in using new habits, working in teams, and approaching the work environment as a system. The nurse’s role in this interdisciplinary, patient, family centred care model is essential and central. It will be well illustrated throughout the video presentation. VI-01-E FACTORS ASSOCIATED WITH FUNCTIONAL WELL BEING IN OLDER PERSONS LIVING WITH CANCER Joan Tranmer1, RN, PhD; Linda Robb Blenderman2, RN, MScN; Esther Green3, RN, MSc(T); et al; 1 Kingston General Hospital, Kingston, Ontario; 2Cancer Centre of Southeastern Ontario; 3Cancer Care Ontario The purpose of this prospective cohort study was to obtain a profile of personal health and social factors associated with functional well being in older persons diagnosed with cancer. Three hundred and fifty patients, greater than 65 years of age, diagnosed with cancer at the Southeastern Ontario Cancer Centre participated in the study. At baseline and 3 months following enrollment, the following validated measures were collected via written questionnaire or telephone interview: (1) health related quality of life using the MOS SF12 and the EORTC QLQ – C30; (2) symptom distress using the Memorial Symptom Assessment Scale (MSAS); (3) physical activity using the Physical Activity Scale for the Elderly (PASE) and (4) informal social support using the Medical Outcome Social Support Survey. Data collection and analysis is in progress. We will report on the personal, health and social support factors that are correlated to functional well being. It is anticipated that the information gained from this study will enhance nurses’ understanding of, and care in regard to age related issues. RN VI-02-D THE IMPRINT OF MRS. L: A UNIQUE CLINICAL JOURNEY WITH PAGET’S DISEASE OF THE VULVA Jennifer Parkins, RN, BScN, CON(C); Pat Bieronski, RN, BScN, CON(C); Gloria Hasenpflug, RN, CON(C); Grand River Regional Cancer Centre, Kitchener, Ontario Gwendolyn D. Bourdon, RN, BScN, MEd; Stephanie Burlein-Hall, RN, BScN, MEd, CON(C); Interlink Community Cancer Nurses, Toronto, Ontario A MULTIDISCIPLINARY LEADERSHIP VI-01-F LUNG CANCER CLINIC: Registered Nurses are innovative leaders in the implementation of a multidisciplinary lung cancer clinic at a regional cancer centre. Registered Nurses specialized in lung cancer triage all new lung cancer cases coming into the centre in collaboration with the medical team. Thus, there is a process of prioritization leading to the delivery of prompt and appropriate care for the lung cancer clients. Decisionmaking and clinical judgements are essential components to the Registered Nurse’s planning for the clinic. “The literature identifies two distinct phases in nursing and medical decision-making: (a) a diagnostic phase in which observation of a patient situation, data collection, and data processing lead to the identification of problems or decisions about diagnosis, and (b) a management phase in which plans of action and treatment options lead to interventions. In this kind of process nurses and physicians make decisions on the basis of the information processing theory” (Salantera, & Erikson, & Junnola, & Salminen, & Lauri, 2002, p. 280). Therefore, newly diagnosed lung cancer clients are seen for initial consultation by a medical oncology and a radiation oncology multidisciplinary team. On consultation, an individualized plan of care is developed for each client. Registered Nurses act as key contacts for the clients offering ongoing educational and holistic support. This presentation/poster will focus on the RN’s role for this clinic and ongoing evaluation of this pilot project. VI-02-E CREATIVE PARTNERSHIPS IN ACTION: RECOMMENDATIONS FOR A REGIONAL STRATEGY TO MANAGE BREAST CANCER RELATED LYMPHEDEMA Cathy DeGrasse 1, RN, MScN; Lisa Bitonti 2, BScN, RN, CON(C); Dr. Audley Bodurtha 3, MB, BS, FRCSC, FACS; 1 The Ottawa Regional Women’s Breast Health Centre; 2 The Ottawa Regional Cancer Centre; 3 The Ottawa Hospital; Ottawa, Ontario Women suffering from lymphedema and other stakeholders who have been helping women to cope with their breast cancer diagnosis and treatment have expressed two main challenges related to lymphedema: inconsistent acknowledgement by some health practitioners of lymphedema existence; and the overall coordination of lymphedema services within the community. An innovative multi-stakeholder process was used to determine a regional, evidence-based strategy to manage breast cancer-related lymphedema. A multi-stakeholder steering committee informed the process and developed a foundation document for a regional workshop. The purpose of the workshop was to make specific recommendations for a regional strategy. The workshop framework was based on the following five major themes identified by the steering committee: clinical pathways; communication strategies; education of women; education and training of health professionals; and research and quality improvement. Through large and small group facilitated dialogues, workshop participants adopted a working definition of lymphedema, provided feedback on the foundation document, and, identified the main priorities related to each theme. This project is consistent with a provincial cancer plan to improve access, measurement and reporting, evidence-based decision making, effective use of resources, and outcomes. This presentation will focus on the recommendations for a regional plan which was submitted to a palliative care consortium (the project funding body) and the Regional Cancer Centre for implementation. While many nurses may be familiar with Paget’s disease of the bone, extramammary Paget’s disease of the vulva is a rare non-squamous cell cutaneous adenocarcinoma with the true incidence and cause unknown. Challenges related to the rarity of this disease include limited knowledge and information about the disease, and inappropriate or unclear management guidelines, including those related to nursing care. Typical symptoms are non-specific and may include pruritis, irritation and pain, but occasionally patients may appear asymptomatic. Delay in diagnosis and treatment may be long, range 2-8 years (Tulchinsky, Zmora, Brazowski, Goldman, and Rabau, 2004) as the disease is often treated with topical preparations in the belief it is a benign dermatologic condition, such as dermatitis or eczema. Surgery is the most common treatment, however repeat excisions are often necessary due to the high incidence of local recurrence. To date, chemotherapy has not been effective for this population of predominately postmenopausal Caucasian women. Through the journey of Mrs. L, the author shares the ‘imprint’ of this patient on her practice and the clinical challenges in caring for one with a rare cancer. Sharing this experience will help other oncology nurses provide holistic and individualized nursing care through a review of this disease from past and present knowledge. VI-02-F NURSING’S IMPRINT ON PATIENT CARE: AN EVALUATION OF PATIENT SATISFACTION IN A RADIATION NURSING CLINIC Maurene McQuestion, RN, BA, BScN, CON(C), MSc (candidate); Barbara Willson, RN, BN, MS, CON(C); Sandra Chapman, RN, CON(C); Princess Margaret Hospital, University Health Network, Toronto, Ontario Patient satisfaction has been shown to be a nurse sensitive outcome as well as a measure of quality care provided by the multidisciplinary team (Spence Laschinger & Almost, 2003). In the ambulatory oncology setting, care is provided in several areas including new patient clinics, treatment review clinics, radiation treatment units, drop-in radiation nursing clinics, and in inpatient settings for overnight chemotherapy treatments. Existing patient satisfaction studies have focused on informational needs and information provision, satisfaction with physical and psychosocial adjustment, medical care, waiting times, technical competence of personnel, communication, access to care, and satisfaction with follow-up care, etc. (Frost, et. al., 1999; Goodwin, 2000; Gourdji, et. al., 2003; Hagedoorn, et. al., 2003). To date no studies have assessed patient satisfaction of care in an ambulatory radiation oncology setting. A pilot study assessing patient satisfaction based on the Picker Institute’s eight dimensions of patient centred care (PCC) was conducted with patients receiving care in a radiation nursing clinic (RNC). The RNC provides a setting where patients can be assessed by a registered nurse for new or ongoing problems or have procedures carried out in the period between their weekly review appointments with the radiation oncologist and RN Case Manager. Surveys were conducted with 57 patients who received care in the radiationnursing clinic. 10 patients also participated in a one-hour indepth interview about their experience in the clinic setting. This presentation will provide a brief overview of the model of PCC and share findings from the patient satisfaction survey and patient interviews. Results of this survey may serve as a model for the evaluation of patient satisfaction in other radiation treatment facilities. VI-03-D EMPOWERED CHOICES: NAVIGATING THE CONTINUUM OF CARE FOR WOMEN WITH BREAST CANCER Sally Turco, RN, CON(C); Misericordia Community Hospital, Edmonton, Alberta In July 2003, a funding grant from the Canadian Breast Cancer Foundation, Alberta/NWT chapter allowed the development a Nurse Navigator role, aimed at providing education and support to women at the time of diagnosis of breast cancer. The Nurse Navigator meets with women at the time of diagnosis and facilitates access to information and support in their decision making through surgery and in preparation for long-term treatment at the Tertiary Cancer Center. In addition, the Misericordia Community Hospital developed an innovative, quality program for women newly diagnosed with breast cancer. The purpose of the program, called Healing Connections, is the assessment, follow up, support and education of program participants and to provide a bridge from diagnosis to the long-term treatment programs at the Cancer Center. Patients are referred to the 5-week program as part of their preand post-operative care. Although the concept of such a program may be seen as basic, it is unique to the Capital Health Region. Participants come into the program after diagnosis of breast cancer and prior to surgery, and are followed by a team of health professionals until initial consultation at the Cancer Center, or until they decide to exit the program, knowing that they can return at any time. Outcomes reveal a high success rate of program participants in mobility, increased function, adaptability and a sense of well-being. Through these two initiatives, women with a diagnosis of breast cancer are well informed, well supported, and well prepared to adjust to life in the context of breast cancer. This presentation will outline the structure of the Healing Connections Program and the Role of the Nurse Navigator, and will present research VI-03-F investigating patient satisfaction and preparedness long termWITH cancer A DAY SURGERY AND RECOVERY IN for WOMEN care, as well as future directions LESION: for this uniqueEVALUATION program.. SUSPICIOUS BREAST OF A PSYCHOEDUCATIONAL NURSING INTERVENTION Nicole Allard, RN, PhD (candidate); Université du Québec a Rimouski, Québec This study assessed whether a nursing intervention based on selfregulation theory, the Attentional Focus and Symptom Management Intervention (AFSMI) could help women who underwent day surgery for breast cancer to achieve better health outcomes. The sample consisted of 117 patients with breast cancer who were outpatients and undergoing surgery as part of the initial treatment for their cancer. The outcomes were the subjects' symptomatology, emotional distress and functional status. Results showed significant differences between the experimental and control group at post-test on disruption in home management activities, total mood disturbance, confusion and tension scores implying that the intervention was effective in achieving these outcomes. As for symptom management, the intervention had no statistically significant effect. Future research should consider individualized intervention to help each woman cope with the healthcare situation and allow different ways to reach unexpressed needs in order to intervene more effectively. Findings from the present research have illustrated that a nursing intervention applied during immediate recovery of breast cancer surgery is quite clinically relevant to reduce emotional distress and usual functioning, the ultimate outcomes of coping. Self-regulation theory could effectively be used as a guide in developing nursing intervention programs in practice for patients with cancer undergoing day surgery as a primary treatment. VI-03-E IMPROVING WAIT-TIMES: THE ROLE OF THE NURSE NAVIGATOR IN BREAST HEALTH ASSESSMENT AND CANCER DETECTION Anne Matte, RN; Carole Mayber, MSW, RSW; Denise Gauthier-Frohlick, MA, Bed; Carolyn Jackson, RN; Sudbury Regional Breast Health Program, Supportive Care Oncology Research Unit, Hôpital Régional de Sudbury, Sudbury, Ontario As the Canadian health care system struggles to provide patients with timely access to medical care and treatment, more attention is focused on the role of the Nurse Navigator to effectively coordinate services and provide the necessary support to patients. This presentation will focus on the role of the Primary Nurse Navigator (PNN) developed at a regional breast health program that has contributed to reducing time to diagnosis for women and men who are investigated for a breast detected abnormality. Data will demonstrate that time to diagnosis has significantly decreased. The presenter will also share her experience working as a PNN and how it has changed her nursing practice. The regional breast health program opened in January 2000 and offers comprehensive services to women and men of all ages undergoing investigations for a breast abnormality. Examples demonstrating how the PNN is effective at reducing time to diagnosis are: Track breast detected abnormalities identified in Diagnostic Imaging Assess patient referrals based on a priority system Bridge dialogue within the interdisciplinary team (e.g. radiologists, pathologists, surgeons, oncologists, family physicians, social workers, and community partners). Participants attending will have a good understanding of how the Nurse Navigator role can be implemented to provide optimum care, reduce wait times, and the implication for nursing practice. VI-04-D FROM INPATIENTS TO OUTPATIENTS AND BEYOND Deborah Sanfelice, RN. OCN; Darlene Priestman, RN, CON(C); Susan Coffey, RN; Jeanie Son, BScN; Mari Dumbrell, RN; Princess Margaret Hospital, University Health Network, Toronto, Ontario The Transfusion Center was developed as an outpatient unit to provide blood transfusions, boluses and antibiotic therapy for solid tumor and hematology patients. As well, it supports other outpatient clinics by providing central line blood draws for their patients. The decreased availability of inpatient resources over the last five years has affected the volume of patients seen in The Transfusion Center, as well as the types of treatments administered there. The Transfusion Center frequently acts as a drop-in center for neutropenic patients, providing daily antibiotics, antifungal treatments and chemotherapy. The increased volume and variety of treatments have forced The Transfusion Center to make changes to cope with several issues such as staffing, space, time, budget and patient satisfaction. Working with advanced practice nurses, limiting the number of chemotherapies per week and alternating patient visits, The Transfusion Center has evolved into a highly skilled and functioning unit. While the future of health care remains uncertain, treatment and mortality for leukemia patients continue to improve. It is expected that the transfusion unit will continue to see an increasing number patients requiring complex care. The transfusion unit will continue to adapt and improve to provide a high level of care to these patients. V1-04-E PAIN POINTERS: WEB-BASED INNOVATION IN KNOWLEDGE TRANSFER Cindy Shobbrook, RN, MN, ACNP, CON(C); Princess Margaret Hospital, Toronto, Ontario Continuing education of health care professionals on the principles behind pain assessment and management is central to successful pain management. Literature suggests that a lack of interdisciplinary pain education contributes to ineffective pain management (McCaffrey & Pasero, 1999). Innovations in information technology create opportunities for creative education delivery including electronic learning that provides health care professionals access to convenient web-based education. A 3-site tertiary hospital in Toronto embraced an opportunity to disseminate consistent interdisciplinary pain management education organization wide. One nursing strategy initiated several years ago is “Pain Pointers”, a monthly one-page newsletter exploring topics in pain management. Previously distributed via hardcopy and email to targeted staff, Pain Pointers evolved into an electronic format distributed to team members through the corporate intranet. In addition to traditional text, Pain Pointers contains an embedded video relaying visual and audio reinforcement of pain assessment and management principles. Maintaining an electronic archive enables interdisciplinary team members to revisit previous issues. In 2004, twelve Pain Pointers issues averaged 500 viewings monthly. The accompanying video was viewed approximately 320 times. Further work is required to evaluate the impact of this method of knowledge transfer on practice and patient outcomes related to pain management. This presentation will explore Pain Pointers’ design and examples of VI-05-D the interactive format. THE ROLE OF THE CLINICAL NURSE SPECIALIST AND RESEARCH NURSE IN THE MCGILL UNIVERSITY CANCER NUTRITION AND REHABILITATION PROGRAM FOR PATIENTS WITH CACHEXIA Michelle Dumas1, 2, RN, MSc; Nancy Lee Brown2, 3 , GPL, MSc(A), Neil MacDonald1, 2, MD; Nelda Swinton1, 2, RD, MA; Sarah Thirlwell1, 2, RN, MSc; Mary-Ann Dalzell, PT, MSc(A)2, PT, MSc(A); 1 SMBD Jewish General Hospital, Montreal, Quebec; 2Cancer Nutrition-Rehabilitation Program, McGill University, Montreal, Quebec; 3McGill University Health Centre, Monreal General Hospital, Montreal, Quebec Patients with advanced cancer commonly lose their appetites, lose weight and become profoundly weak and tired. These symptoms are the hallmarks of cachexia, which impairs quality of life and contributes to morbidity and mortality in one-half of all cancer patients. The McGill University Cancer Nutrition and Rehabilitation Program (CNR) was instituted in 2002 to provide a multi-site, interdisciplinary approach to the management of cachexia and cachexia research. The CNR team consists of physicians, physiotherapists, clinical nurse specialists, nutritionists and a research nurse who offer a comprehensive approach to managing cachexia through sophisticated nutritional counseling, drug therapies, tailored exercise programs, and psychosocial interventions. Within the interdisciplinary team, the clinical nurse specialist and research nurse fulfill key roles. Both identify patients at risk for cachexia and assess the impact of cachexia on patients and their families. The clinical nurse specialist offers evidenced-based strategies for symptom management and assists patients, families and healthcare professionals to integrate the CNR interventions into the patient’s care plan. The research nurse oversees the quality of research protocols, biologic samples collection, and data management. This presentation will focus on the unique expertise that these nurses bring to the CNR program and on how that expertise translates into improved quality of care for the patients and their families, while making a significant contribution to cachexia research. VI-04-F THE ROAD LESS TRAVELED – CONTINUOUS LIDOCAINE INFUSIONS FOR THE TREATMENT OF NEUROPATHIC CANCER PAIN Virginia M. Jarvis, RN, RM, BScN, MPC, OCN; The Ottawa Hospital Regional Cancer Centre, Ottawa, Ontario Approximately 30-90% of patients with a diagnosis of cancer will experience pain at some time during their illness, with more advanced cancers exhibiting more severe and complex pain syndromes. Of these patients, approximately 34% will develop pain of neuropathic origin. While the treatment of nociceptive pain has improved substantially over the last 20 years, effective treatment for neuropathic pain remains elusive (Portenoy & Lesage 1999). Bolus doses of intravenous (IV) Lidocaine have been used for the treatment of neuropathic pain for many years. However, the use of continuous IV infusions for the treatment of severe cancer pain is an emerging treatment modality. This presentation will review two cases where a continuous infusion of IV Lidocaine was used to control severe neuropathic cancer pain. The discussion will address some of the issues that were of concern to pharmacy, senior administration as well as the problems encountered by the nurses who were caring for the patients in both the inpatient and community settings. VI-05-E CREATING A VISION FOR ONCOLOGY NURSES: THE ROLE OF ADVANCED PRACTICE NURSES Debbie Miller, RN, MN, ACNP, ET; Shari Moura, RN, MN, CON(C); Rosemary Cashman, RN, MA, MSc(A), ACNP; Barbara Fitzgerald, RN, MSN; Angela Boudrean, RN, MN, CON(C); Sunnybrook and Women’s College Health Sciences Centre – Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario Advanced Practice Nurses (APN) fulfill various domains of practice, which may include direct care, education, research, publication and professional leadership, and systems support (Ackerman et. al, 1996). In a large tertiary health care centre, APNs working in the oncology program have varied clinical roles, but all work towards supporting, advancing and influencing the professional growth of oncology nurses. The Canadian Nurses Association (CNA, 2002) describes competencies related to advanced nursing practice, which includes nursing leadership. Strategies to advance oncology nursing practice includes the leadership role of APNs in the specialized care of oncology patients, as well as their work on various intra-and interdisciplinary committees and program councils. The APN vision for oncology nursing has been a driving force for nursing leadership and has influenced nursing practice and education in our cancer centre. This presentation will provide participants with an overview of the various APN roles at a leading cancer centre. The involvement of the APN in creating a vision for oncology nursing, the implementation of nursing practice standards, the provision of nursing education through formal and informal professional development activities, and specific committee/council work will also be highlighted. VI-05-F PROMOTING THE FUTURE OF ADVANCED PRACTICE NURSES (APN) IN PALLIATIVE CARE: A NURSING FELLOWSHIP PROGRAM Deborah Gravelle1, BScN, MHS (candidate); Lillian Locke1, BScN, MPA; Frances Fothergill Bourbonnais2, RN, PhD Full Professor; 1SCO Health Services; 2School of Nursing, University of Ottawa; Ottawa, Ontario While completion of a graduate degree is currently considered the most effective means of acquiring the competencies for an APN, it is also essential that novice advance nurse practitioners have additional opportunities to integrate previous clinical experience and education in the specialty setting. Programs currently exist in Australia, Great Britain and the United States. This program is the only one available presently in Canada. The Palliative Care Nursing Fellowship is a 12 month program for Registered Nurses completing the Masters of Nursing Program at the University of Ottawa. The program is tailored depending on the experience and learning needs of the fellow. There are time allotments for course work, clinical work, research endeavours and education. The nursing fellowship provides clinical and academic preparation for a nurse who would like to pursue a position as an Advanced Practice Nurse in Palliative/End of Life care, this occurs through a collaborative relationship between the Palliative Care Program of SCO Health Services and the University Of Ottawa School Of Nursing. Leadership and learning are indispensable to each other. - John F. Kennedy . To develop leaders in palliative care nursing one must contribute to the education of those leaders. This presentation will describe the collaboration between clinical and academia settings in the development of a speciality fellowship. It will describe the components of the fellowship including the logic model, objectives, and outcomes of the program. VI-06-E THE ABZ’S OF A ZEVALIN PROGRAM Nancy Hutchinson, RN, BPHE, BA, MScN, CON(C); McGill University Health Centre – Royal Victoria site, Montreal, Quebec The future of malignant hematology and oncology care will involve the administration of medications beyond the current chemotherapies and monoclonal antibodies. Diseases, such as Non-Hodgkin’s lymphoma can now be treated by radioimmunotherapy. In October of 2004, we administered our first infusion of Zevalin in our outpatient oncology day centre. As the treatment requires considerable coordination between the multi-disciplinary radioimmunotherapy team as well as the pharmaceutical company, a Zevalin coordinator was designated. The ABZ’s of Zevalin coordination is presented here. Implications for nursing practice including treatment side effects, transfusional and supportive care needs, patient/family education and staff development are discussed. Radioimmunotherapy is a promising modality and can be safely administered in oncology settings. . VI-06-D “DOES IT MAKE YOUR MOUTH WATER?”: A PATIENT FOCUSED METHOD OF EVALUATING THE BEST PRODUCT TO INDUCE SALIVATION IN PATIENTS RECEIVING I-131 DRINK FOR THE TREATMENT OF THYROID CANCER Monique Levesque King, BN, RN, MN, CON(C); Elizabeth Mabey, RN; Atlantic Health Sciences Corporation, Saint John, New Brunswick Radioiodine is a radiation therapy in which radioactive iodine (I131) is administered to destroy or ablate thyroid cancer. Radioiodine is absorbed not only by thyroid tissue but also by other tissues, including the salivary glands. This can result in salivary gland pain, swelling and subsequent dry mouth (xerostomia). The goal of this treatment is to deliver enough radiation to destroy the thyroid tissue, with every effort made to minimize damage to the salivary glands. Patients are encouraged to drink fluids frequently and to suck on lollipops or candies to induce salivation during treatment. Salivation helps flush the excess radiation out of the salivary glands and can help reduce the occurrence and/or severity of these side effects. Increasing patient complaints of throat pain and swelling was the impetus to investigate whether other products might improve patient outcomes in relation to these side effects. This presentation will focus on the processes one unit undertook to involve their patient population in determining the best product to induce salivation following radioiodine ablation. Preliminary survey results will be discussed. Samples of the four products evaluated will be available. VI-06-F PERMANENT BREAST SEED IMPLANT IN EARLY STAGE BREAST CANCER: AN EXPANDED ROLE FOR ONCOLOGY NURSES Lisa A. Verity, RN, BScN, CON(C); Nancy Hurst, RN, CON(C); Tanya Holownych, RN, BScN; Barb Nayler, RPN, CRA; Barbara Fitzgerald, RN, MSN, Clinical Practice Leader/Advance Practice Nurse Breast Cancer is the most commonly diagnosed cancer in Canadian women. A large portion of women who undergo breast conserving surgery (BCS) will receive adjuvant external radiation (XRT). Conventional adjuvant radiation treatment can be associated with skin toxicities, treatment interruptions and significant changes to normal life routines. These challenges have led to examining ways in which treatment and associated impact on quality of life can be improved. Permanent Breast Seed Implant (PBSI) is a pioneering treatment approach for women with early stage breast cancer. PBSI involves implanting small beads of pallidium that release very low doses of radiation over the course of two months. It is a half day procedure under local anesthesia. Since this treatment is specifically different from standard approaches, a phase I/II study examining PBSI has been initiated at a cancer centre in Toronto. It is the first centre to trial this approach in the world. If the goal of PBSI and clinical outcomes are achieved, this approach will dramatically reduce treatment times and costs, and will change the conventional approach of care for these breast cancer patients. This presentation will provide a description of the expanded role of the oncology nurse caring for women undergoing this treatment including direct care, education, patient coordination, and data acquisition. Potential nurse sensitive research, specific to the unique issues these patients face, will be discussed. P-01 A NEEDS ASSESSMENT TO DEVELOP A PROACTIVE NUTRITIONAL INTERVENTION AND NUTRITION RESOURCE FOR PATIENTS WITH MULTIPLE MYELOMA Devi Ahuja, RN; Christine Chen, MD; Sunshine Giesbrecht, BSc; Joyce Nyhof-Young, PhD; Princess Margaret Hospital, Toronto, Ontario Nutritional problems in multiple myeloma stem from complications of the disease, treatment toxicities, and psychological barriers, such as depression and anxiety. Renal impairment, anemia and steroid induced diabetes, common complications of myeloma, mandate specific dietary modifications. Limited mobility from bone pain, neuropathy, myopathy and fatigue may prohibit regular access to fresh foods and proper preparation of meals. Optimal nutrition improves therapeutic efficacy and alters clinical outcomes in cancer patients (Rivadeneira et al, 1998). Nutritional information “specific” to myeloma is needed. At our institution, an educational plan tailored to the nutritional needs of myeloma patients has been initiated. As an initial phase, a needs assessment survey is being conducted. Thirty randomly selected myeloma patients with chronic fatigue were individually interviewed, and completed a semi-structured nutrition questionnaire. This questionnaire is a patientgenerated subjective global assessment tool developed internally and consists of 155 myeloma-specific questions. We will present the findings of our needs assessment, which will facilitate the integration of a proactive nutritional intervention to myeloma patient care and the development of a nutrition resource with a myeloma-specific diet. Results will also assist in developing future clinical trails focused on nutrition in myeloma patients. P-02 AN INNOVATIVE ONCOLOGY NURSING ORIENTATION PATHWAY: A COLLABORATIVE PROGRAM FROM NOVICE TO EXPERT ACROSS ALL UNITS OF A PROGRAM Elaine Avila, RN, BScN; Angela Boudreau, RN, MN, CON(C); Amy Melnick, RN, MN (candidate); Beverley Page, RN, BScN, CON(C); Joan Pope, RN, MN; Sunnybrook & Women’s College Health Sciences Centre, Toronto, Ontario The changing nursing workforce has accentuated the nursing shortage in health care institutions. In 2003 - 2004, this cancer program, hired 61 nurses. Of those hired, 41% were new graduates, 20% were nurses with no oncology background, and 39% had a minimum of 2 years oncology experience. The lack of experienced nurses, the increasing acuity and complexity of cancer care, and the amalgamation of the cancer center with the host hospital emphasized the need to evaluate orientation. Oncology nursing leaders developed a structured, competency-based orientation pathway. The pathway supports the educational needs of new nurses, increases their capacity to practice safely, and provides ongoing learning opportunities to advance their expertise. This process is pivotal in the development of novice to expert oncology nurses. The pathway is organized in three phases. Phase I combines corporate and general oncology orientation. Common themes and competencies provide new nurses with the initial knowledge in cancer care. Phase II provides specific competencies for surgical, medical, and radiation oncology both in inpatient and outpatient units. Phase III offers ongoing education related to complex cancer care. P-03 THE CLOT THICKENS: DEEP VEIN THROMBOSIS: A PROGRAM FOR THE CANCER PATIENT This presentation will focus on the development process of the P-04 oncology nursing orientation pathway.WITH ChangesRECTAL in today’sCANCER nursing MANAGEMENT OF PATIENTS workforce require nursing leadership teams to develop innovative RECEIVING TRADITIONAL RADIATION THERAPY VS. approaches to oncology nursing orientation programs. BRACHYTHERAPY: A TEAM APPROACH Sylvi Baillie, RN, CON(C); Maureen Lee, RN, CON(C); Heather Fashanu, RN; BC Cancer Agency, Centre for the Souther Interior, Kelowna, British Columbia Astride Bazile, BSc, MEd; Lorraine Brown, BScN; Radiation Oncolody Department, McGill University Health Centre, Montreal, Quebec. Oncology patients are at an increased risk of developing a deep vein thrombosis (DVT). The most recent statistics indicate that ten percent of cancer patients will develop this potentially life threatening complication. Patients presenting with a DVT may be identified at any point during the continuum of care in the clinical areas of ambulatory care, chemotherapy and radiation therapy. Nurses at our centre are leading an initiative that will improve patient care outcomes following a diagnosis of a DVT. Currently at our centre there is no formalized process for teaching and/or follow up care for patients who present with a DVT. This presentation will outline an overall strategy to implement a standard approach to improve service delivery for this population of patients and strengthen the quality and effectiveness of care. Brachytherapy is a method of internal radiation therapy that has been used for a number of years for different tumor sites. Rectal intracavitary High Dose Rate (HDR) brachytherapy is a fairly innovative technique, developed at this teaching university health center. Patients with a diagnosis of rectal cancer face many challenges: pain, discomfort, and the possibility of a permanent colostomy, all of which can be very distressing. Nurses specialized in radiation oncology play a key role in the care of this patient population. Often the patient’s first contact is the nurse so that establishing a trusting relationship is critical. This presentation will describe the multidisciplinary approach to the assessment of patients’ needs, teaching about the treatment plan, coordination of radiation therapy with chemotherapy and prevention and management of acute side effects. A comparison between traditional external beam radiotherapy and intracavitary HDR brachytherapy with respect to the nursing care of these patients will be presented. Furthermore, a discussion of the importance of a multidisciplinary approach to ensure the delivery of the treatment in a timely fashion will be included. The goal of this presentation is to provide information on the role of the radiation oncology nurse with patients diagnosed with rectal cancer and to demonstrate how a team approach is fundamental to achieve comprehensive care. P-05 VENOUS THROMBO-EMBOLISM DISEASE PATIENT IN THE CANCER Carole Beals, RN, BScN, CON(C); Royal Victoria Hospital, Barrie, Ontario “Thrombotic events represent one of the most common complications and frequent causes of mortality in patients with malignancy” (Goldenburg, Kahn and Solyman, 2003). In fact, the risk of thrombosis is reported to be six times greater in patients diagnosed with cancer (Heit et al., 2000). There is a strong association between cancer and venous thromboembolism (VTE) with little data to assist clinicians in predicting which cancer patients will develop VTE (Geerts et al., 2004). Armand Trosseau suggested this link as early as1865 and recent research is directed towards understanding this relationship and formulating interventions for the purpose of primary and secondary prevention of VTE in cancer patients. A number of authors have described Virchow’s triad of symptoms and pathologic factors contributing to the development of thrombotic disorders in cancer patients (Haliquist Viale & Schwartz, 2004; Prandoni Piccioll, 1998). The triad of symptoms includes a hypercoaguable state, stasis, and endothelial injury. Additional risk factors contributing to VTE include use of central venous access devices, chemotherapy, surgery, hormonal therapy, and patients diagnosed with mucinous adenocarcinomas of the pancreas, lung, breast, ovary and gastrointestinal tract. P-06 CHANGING THE PATH OF PATIENT EDUCATION: EVALUATING A NEW DIRECTION Angela Boudreau, RN, MN, CON(C); Kathy Beattie, RN, OCN; Sherrol Palmer-Wickham, RN, BScN, CON(C); Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario With rising patient volumes and increasingly complex chemotherapy treatments one challenge is to provide chemotherapy information in ways that result in improved retention, comprehension and desired behavioral outcomes. The chemotherapy unit at a large cancer treatment center piloted group chemotherapy information sessions for patients and families. The sessions addressed: 1) common side effects of chemotherapy and 2) processes involved in navigating the system. The goal was to decrease the amount of information provided in the initial treatment visit to the chemotherapy unit, allowing for a more focused discussion of the patient’s individual treatment. As a result, information retention would improve. A secondary goal was to streamline patient teaching time. The pilot evaluated: 1) a pre and post information session survey to determine knowledge; 2) a pre-chemo survey to determine knowledge retention and identify knowledge differences between attendants and non-attendants; and 3) a threat assessment scale, a profile of mood states scale and a self care behavior tool. These measurements identify differences between provision of incremental information versus a bolus of information during the first chemotherapy. This presentation will examine the identification, screening, prevention, management and new advances in the treatment of VTE in cancer patients. This presentation will highlight: the successes and challenges of creating a new education program; results of the patient surveys; the influence of timing on self care behaviors and nurses perception of the group teaching session. P-07 THE NURSING PERSPECTIVE ON TREATMENT OF BREAST CANCER: EXTERNAL BEAM RADIATION THERAPY VS. BRACHYTHERAPY P-08 DETERMINING THE ACCURACY OF ONCOLOGY NURSES IN PREDICTING THE SURVIVAL OF PATIENTS WITH ADVANCED METASTATIC CANCER Lorraine Brown, BScN; Astride Bazile, BScN, MEd; Radiation Oncology Department, McGill University Health Centre, Montreal, Quebec Grace Chan, RN, CON(C); Kin Wah Fung, MSc; Kathy Katherine Enright, MD; Shari Moura, RN, MN, CON(C); Carmen RN; Emily Sinclair, BSc, MRT(T); Edward Chow, MBBS; Sunnybrook & Women’s College Health Sciences Centre, Ontario, Canada Patients with breast cancer face a multitude of challenges such as alteration in body image, which may in turn affect their femininity, and fear of the unknown. Undergoing major treatments such as surgery, chemotherapy, and external beam radiation therapy become part of the experience and the difficult battle against breast cancer. The role of the nurse in radiation oncology is to support women during that battle, thereby alleviating as much physical and psychological suffering as possible at each of these steps. Among all the treatment options for breast cancer, high dose rate (HDR) interstitial brachytherapy remains fairly unknown to many nurses yet is regularly offered at selected centers in North America and Europe. This presentation will provide an overview of the nursing assessment and teaching that is provided to women with breast cancer undergoing radiation therapy, particularly with HDR brachytherapy, at this teaching university health center. This will include a comparison of the differences between traditional external beam radiation therapy and HDR brachytherapy for breast cancer as well as an examination of the nurse’s role in prevention and management of side effects related to each of these radiotherapy treatments. The objective of this presentation is to familiarize nurses with HDR interstitial brachytherapy and to explore the nursing and patient implications involving this treatment. Li, BSc; Gosselin, Toronto Toronto, Precise prediction of survival of terminally ill cancer patients is important for both the family and health care professionals. To the patients and their family, it is often the paramount issue. They need the information to plan and address the end-of-life issues and to optimize their remaining time together. Health care professionals employ this estimate to plan for timely supportive services and appropriate allocation of resources. Accurate prediction of life expectancy of terminally ill cancer patients is a difficult task for health care professionals, especially nurses who have very little training in this practice. The study included thirty-three nurses with varying experience, employed in an ambulatory cancer centre. The research method was based on analysis of five real cases of patients with metastatic disease. The cases were analyzed retrospectively. The subjects ranked the five most important prognostic factors based on: 1) symptom distress scores; 2) Karnofsky Performance Status and; 3) other individual variables. Additionally, the subjects estimated the mean, the shortest and longest survival times for each patient case. Study results have enhanced our understanding of oncology nurses’ perception of the impact of prognostic factors and the nurses’ ability to predict survival. Further research is required into the development of prognostic prediction tools to aid accuracy in survival prediction. III-05-A (French) – from page 56 (English) SÉANCES D’INFORMATION EN PRÉOPÉRATOIRE FEMMES ATTEINTES D’UN CANCER GYNÉCOLOGIQUE POUR Joanne Brodeur, BSc; Thérèse Vincent, BSc; Nicole Tremblay, MSc, CSIO(C); Lucie Bédard, BSc, MBA; Jacinthe Brodeur, BSc, CSIO(C); Chantal Bélanger, BSc; Josée Beaudoin, Dt.P. clinicienne; Centre Hospitalier de l’Université de Montréal. Ces dernières années, le développement du rôle d’infirmière pivot et l’établissement d’une équipe d’amélioration continue de la qualité des soins en oncologie gynécologique a permis d’identifier certaines cibles d’amélioration dans les soins offerts. Parmi ces cibles d’amélioration, la nécessité de mieux planifier le retour à domicile des femmes subissant une chirurgie gynéco-oncologique est ressorti comme prioritaire. En effet, bien que des efforts importants soient fournis par l’équipe pour préparer le départ de ces patientes, beaucoup de problèmes ne devenaient connus que lors du retour à domicile. La fatigue, la difficulté de prendre soin de soi, diverses inquiétudes reliées à la chirurgie et l’anxiété ont été identifiés comme des problèmes fréquents. Suite à ce constat, un projet de séances d’information et d’enseignement préopératoire destinées à cette clientèle a été débuté au début de l’année 2005. Ces séances visent notamment à mieux renseigner la clientèle sur la chirurgie et à détecter des situations problématiques avant l’admission afin d’intervenir pour corriger la situation. Les auteures du projet présenteront le contenu du programme et les diverses constatations qui en résultent. P-11 STREAMLINING PATIENT CENTRED DELIVERY MODEL OF THE FUTURE CARE: NURSING CARE Anne DeVries, RN, CON(C); Janice McLorn, RN, CON(C); Laurie Locke, RN; St. Thomas Elgin General Hospital, St. Thomas, Ontario The challenge in 1987 was to provide seamless cancer care through our community hospital serving approximately 70,000 people. The problem of a fragmented referral system and lack of continuity in patient care between the regional centre and the local medical community needed to be addressed. By making the referral coordinator the pivot around which the community clinic worked, patient referrals between the regional centre and the community hospital have become much more streamlined and efficient. This resulted in better use of resources through a team approach covering the whole continuum of care. Communication between health care professionals at the regional centre and the local clinic is enhanced by the collaborative working relationships. As a result, today leading edge chemotherapy treatment and follow-up is delivered in a timely and effective manner, in a patient centred setting within their own community. Working closely with the regional cancer center has closed the gaps and provides integrated patient centred cancer care. The clinic is often looked to as a model for other communities to study and emulate. While constantly building on past performance and maintaining collaborative working relationships, the clinic will continue to provide the best cancer care a community hospital can offer. P-12 EXAMINING POSSIBLE INCENTIVES AND BARRIERS TO EXERCISE FOR REDUCING CANCER-RELATED FATIGUE IN MEN WITH PROSTATE CANCER UNDERGOING RADIATION AND/OR HORMONAL THERAPY Megan Doyle, RN, BScN, MN(C); University of Manitoba/PEI Cancer Treatment Centre Fatigue has been shown to be the most common side effect of cancer and is reported to decrease the quality of life for clients suffering from the disease and its treatment (Magna & Noose, 2003; Stone, 2002). Exercise has been proposed as one intervention to combat cancerrelated fatigue; however, the majority of the research has been performed with breast cancer clients. In order to ensure the possible effectiveness of exercise; a further exploration of the possible adherence issues is required, specifically for other types of cancers. One of the purposes of this exploratory study was to measure the fatigue level of men with prostate cancer. Another purpose of the study was to explore the possible incentives and barriers to exercise, with the same population, to help reduce cancer-related fatigue. A convenience sample of 31 men participated in the study. Three instruments were used to elicit data from participants. Results are being analyzed and will be available in April, 2005. From this data, exercise interventions can be designed that will aid in attracting clients and increasing the rates of adherence over the long term. The most significant outcome from this study was a further understanding of the meaning of fatigue for this population. P-13 PRACTICAL ISSUES IN ESTABLISHING PET SCANNING IN YOUR CENTRE Michelle English, RN; Cross Cancer Institute, Edmonton, Alberta Positron Emission Tomography (PET) is the latest imaging technique offered to oncologic patients at the Cross Cancer Institute in Edmonton AB. PET scanning creates a unique role for nursing. This presentation will look at the issues related to PET scanning an its’ impact on nursing care. PET scanning uses a radiolabeled analogue, flurodeoxyglucose (FDG) which allows imaging and quantification of invivo intracellular glycolysis. Imaging with PET identifies lesions that can escape detection by other techniques. PET also allows detection of response to anti-cancer treatment modalities. PET imaging is a standard of care in many developed nations but in Canada, PET is an investigational procedure which requires clinical trial investigation to prove its safety and efficacy. The Cross Cancer Institute is the only centre in Alberta currently seeking approval for PET imaging as a standard of care. Nursing issues related to the use of this diagnostic tool include compliance with Health Canada regulations, funding concerns, patient and staff education, and manpower issues. Based on PET’s widespread use outside of Canada, there is an inevitability that PET will become a reality of your nursing practice. PET is the tool of tomorrow P-14 LEAVING AN IMPRINT ON THE CARE OF THOSE AFFECTED BY LUNG CANCER TOMORROW: THE EXPERIENCE OF REGIONAL CARE PATH DEVELOPMENT Valerie Fiset, RN, MScN, CON(C); Lorraine Montoya, BSN, CON(C); The Ottawa Hospital Regional Cancer Centre, Ottawa, Ontario The care of individuals with suspected lung cancer or proven lung cancer is extremely complex. State-of-the-art care often requires input from many sources, necessitating an interdisciplinary approach. Unfortunately, numerous referrals to a variety of specialists and care providers may result in fragmented, poorly coordinated, and even inappropriate care. The anticipated growth in incidence rates will have a compounding negative impact on care for patients and families experiencing a lung cancer diagnosis, or living with the disease. Through interdisciplinary collaboration with regional stakeholders, improving healthcare practitioner and public education, and fostering continuous quality improvement activities, Regional Clinical Pathways will help to better coordinate comprehensive inpatient and outpatient services thus improving resource utilization (i.e. avoid duplication of tests, reduce emergency visits; decrease wait times), and ultimately lead to better clinical outcomes for individuals and their families affected by lung cancer. This presentation will describe the process of development and implementation of Regional Care Paths to address the needs of those living with lung cancer and their families. Specifically, the presentation will address how the Regional Clinical Pathways will enhance 1) the quality of care of patients and families; 2) system efficiencies and effectiveness and 3) knowledge transfer and evidence-based practice. P-15 MONITORING PATIENT PERSPECTIVES ON SATISFACTION WITH INFORMATION P-16 HOW WELL ARE SEXUAL CONCERNS OF CANCER PATIENTS ADDRESSED: PROVIDER AND PATIENT PERSPECTIVES Margaret I. Fitch, RN, PhD; Laurel Plewes, RN, BScN; Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario Margarent I. Fitch, RN, PhD; Gerry Beaudoin, MSW; Laurel Plewes, RN, BScN; Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario An individual’s capacity to cope with the many changes and challenges following a diagnosis of cancer is influenced to a great extent by their access to relevant, understandable information. The information needs to be about the disease, its treatment, expected side effects, and available supports and resources to manage with the illness. Many cancer patients have described heightened emotional distress when they are not able to obtain the information they need. Providing patient information, then, is an important aspect of the activities within a cancer care program. However, in addition to providing information, is it important to know whether or not the provision of the information is appropriate from the patient perspective. The service of delivering patient information ought to be monitored on a regular basis. Given the busy nature of our clinical settings and a desire not to overburden patients, this performance monitoring must be accomplished with data collection tools that are easily administered and scored. The purpose of this work was to implement a performance monitoring approach to the provision of patient information in an ambulatory setting. A psychometrically sound indicator tool has been introduced that measures patient perspectives regarding the importance of, and satisfaction with, the provision of selected information in the cancer setting. This presentation will describe the data collection approach and the resulting data gathered during the 5 rounds of data collection (N1=540; N2=39, N3=42, N4=59, N5=63). Trends in the data observations will be presented as well as discussion about the implications of such an approach for quality improvement initiatives in patient information. Cancer has more than a physical impact. There are emotional, social, psychological, spiritual and practical consequences. Patients confront a multitude of change and may well experience challenges in having their needs addressed in busy clinical settings. This is particularly the case for complex or sensitive psychosocial needs such as those related to sexuality. A project was undertaken in our ambulatory setting to explore how well we were addressing patient concerns regarding sexual issues. Initially, interviews were conducted with oncologists (n=10), nurses (n=10), social workers (n=10) and radiation therapists (n=5) to explore their perspectives regarding the approaches they used in their daily practice to address patients’ sexual concerns. In many instances, discussion with patients about this topic occurred in relation to informed consent procedures or questions revised by patients. The majority of health care professionals indicated they had very few conversations with patients about the impact of cancer on sexuality and often waited for patients to raise the topic. A second set of interviews was conducted with cancer patients. Twenty individuals shared their perspectives about the topic. These patients confirmed that cancer had evoked concerns regarding sexuality and described barriers they experienced to raising/discussing these concerns with health care professionals. This presentation will highlight the findings from these two inquiries and stimulate dialogue about practice change. P-17 DIALYSIS AND PAIN MANAGEMENT: A CHALLENGE Corsita Garraway, RN, MSN, FNP, CON(C), CHPCN(C), Acute Care Nurse Practitioner; Oncology & Palliative Care, St. Joseph’s Health Centre, Toronto, Ontario Management of cancer pain is a complex process in itself without the presence of Chronic Renal Failure as a co-morbidity. There is a plethora of treatments available to manage a patient’s pain. Chronic Renal Failure is an added challenge to care providers in modifying treatment plans and providing individualized care to patients. In this workshop, nurses will be provided with: 1) A review of the pain pathway. 2) Causes of cancer pain. 3) Treatment modalities in cancer pain. 4) Review of renal system. 5) Challenges of pain management in Chronic Renal Failure patients receiving dialysis. P-19 NURSING INTERVENTION: AN APPROACH TO TREATING GAS PAIN Mary Glavassevich, RN, BA, MN; Shari Moura, RN, MN, CON(C); Brenda Leung, RN, BSc; Janet King, RN; June Raymond, RN, BScN; Sunnybrook & Women’s College Health Sciences Centre – Sunnybrook Regional Cancer Centre, Toronto, Ontario A desire for developing a nursing intervention to treat gas pain was initiated by concerns of nurses on our surgical oncology units and as a result of our recent study exploring patients’ experience of gas pain following abdominal surgery. Patients described their experience of postoperative gas pain as being moderate to severe (Glavassevich et al., CANO Conference, 2004). Nurses expressed concerns that they were not meeting the needs of their patients experiencing gas pain. In our large tertiary hospital, current postoperative pain management protocols do not address the gas pain experience. Patients who experience gas pain may be reluctant to mobilize. A recent literature review has shown limited research pertaining to gas pain and no research focusing on the gas pain experience of patients having abdominal surgery for cancer. Thomas et al., 2002, evaluated the effects of rocking, diet modifications and anti-flatulent medication on gas pain following cesarean section. Hence, there is a need to develop and evaluate nursing interventions to lessen the experience of gas pain for oncology patients having abdominal surgery. This presentation will discuss the nursing interventions utilized and the outcome evaluation. In addition, the information will serve to develop best practice guidelines for the care of surgical oncology patients. P-18 A DECISION TREE FOR FEBRILE NEUTROPENIA: MEDICAL ONCOLOGY SOLID TUMOUR AND LYMPHOMA PATIENTS Wendy Gillis, RN, MScN, CON(C), ACNP; Marcia Langhorn, RN, CON(C); Catherine Bond-Mills, BSc (Pharm); Susan Poirier, BSc (Pharm); Anne Marie Bombassaro, BSc (Pharm), PharmD; London Health Sciences Centre, London, Ontario Neutropenic fever is a common and serious complication of cancer chemotherapy. Timely, appropriate, and effective decision-making is vital to minimize morbidity and mortality. In keeping with the goals of the London Regional Cancer Program (LRCP) many patients undergoing cancer chemotherapy are managed in regional cancer centres and home communities. This document was developed in response to requests from our regional partners for assistance in managing neutropenic fever. To implement the above goals a decision tree was developed for patients with solid tumours and lymphoma. It incorporated the latest guidelines from the Infectious Diseases Society of America (IDSA) (2002). It was based on current practices at the LRCP and London Health Sciences Centre (LHSC). The document provides not only a guideline for real-time reference, but also serves as an educational tool for health care practitioners. It promotes consistency of treatment for neutropenic patients with fever. An algorithm was created for determining the most appropriate therapy based on level of risk, presence of defined focus, history of penicillin allergy, and response to therapy at 48 hours. It guides the practitioner in decision-making at distinct times within the episode of fever and neutropenia. The process of development was a collaborative effort involving nursing, pharmacy, and infectious diseases with ongoing feedback from the medical oncologists and hematologists at the LRCP/LHSC. The document will be evaluated and updated to remain current with evidence-based practice. P-20 INFORMATION: KEY TO REDUCE FEAR OF THE UNKNOWN Laurie Greaves, RN, BScN, CON(C); Joanne Svela, RN, CON(C), MN; McLaughlin Durham Cancer Centre, Oshawa Bone marrow aspiration and biopsy is a common investigative procedure to confirm or diagnose a hematological or potential cancer diagnosis. The decision to perform a bone marrow assessment is based on the patient’s clinical presentation and abnormal hematological findings. At our oncology clinic, oncologists perform approximately three to four bone marrow procedures daily. It is the role of the oncology nurse to provide a verbal explanation of the procedure and post instructions. Historically, this education was done immediately prior to the procedure. The patient is usually apprehensive with a high level of anxiety, which is triggered by an understandable fear of the unknown. Observations of patients by the oncology nurse demonstrate a decrease in anxiety followed by this brief explanation. In response to our observations, a bone marrow procedure pamphlet including discharge instructions will be developed. By providing this information we will demonstrate benefit in increasing patient’s preparation. We anticipate the time prior to the procedure will become more valuable for the patient by creating an opportunity for reinforcement and support. This presentation will show how the pamphlet was developed. We will report on the evaluation of our impact of the education intervention on anxiety. We believe this education tool will have a lasting and very positive imprint on our patients’ well being. P-21 IMPROVING QUALITY OF LIFE: IMPLEMENTING BEST PRACTICE FOR MANAGING CHRONIC ONCOLOGICAL WOUNDS IN A COMMUNITY INPATIENT SETTING P-22 BRIDGING THE GAP… FOR TOMORROW; COMMUNITY CLINICS, EDUCATION AND PATIENT TEACHING THOUGH AN ELECTRONIC ENVIRONMENT Anne Hack, RN; Shelley Debison, RN; Royal Victoria Hospital, Barrie, Ontario Donna Holmes, RN, BHScN, CON(C) ; Grand River Regional Cancer Centre “The perception of quality of life is unique to each individual patient and family member. Living with a cancer related lesion causes significant lifestyle changes, potentially impacting the ability to have control over one’s life” Barton and Parslow 1998 Malignant wounds present a unique challenge to caregivers and patients. Challenges include wound containment from drainage, odour control, and pain management. A wound treatment program is important to minimize distressing symptoms and to maximize quality of life. Malignant wounds are characterized by visible changes in the skin. Some lesions may result from a primary skin cancer e.g., melanoma, squamous or basal cell tumours. Others develop as a secondary lesion from infiltration in the late stages of disease. Lesions caused by radiation therapy or extravasations will have a predicted outcome. Other lesions, such as fistulae, malignant cutaneous wounds, and those coming from surgical seedings, have less defined outcomes. In order to improve the management of these types of wounds, a multidisciplinary approach is required. Local oncology networks (LON) are community based oncology clinics developed to bring cancer care closer to home. The main purpose of LON’s are to extend the electronic environment to community sites. Community staff were involved in the development of the clinics from the initial stage. Education, orientation, and set up of the clinic is achieved through an electronic environment. Nurses play a pivotal role in the leadership of these clinics by identifying the patients at high risk for symptom management as well as those needing additional supportive care and providing the navigational aspects for the treatment and outcomes of care. Nurses assist the patient through the educational components of their care by providing access through an electronic environment in their home. As a result of implementing LON, patients will be able to view their treatment regimen, appointments, and side effects management at home. In order to evaluate the outcomes associated with this innovative network, the following variables were assessed: Usage, ease of access, and network links between sites, Patient and staff satisfaction and wait times. This presentation will highlight how our Community Care in-patient centre implemented the Registered Nurses Association of Ontario (RNAO) Best Practice Guidelines for care of malignant wounds to improve the quality of life of our patients. P-23 MEASURING CANCER PATIENT CARE COMPLEXITY AND INTENSITY OF NURSING CARE NEED: AN INITIAL VALIDATION STUDY OF AN INSTRUMENT BASED ON SUPPORTIVE CARE DOMAINS Doris Howell 1, RN, PhD; Eva Pathak 2, RN, BScN; Stephanie BurleinHall 2, RN, MScN; Barb Mildon, RN, MN (candidate); Linda Lee-O’Brien Pallis, RN, PhD; Souraya Sidani, PhD; 1 University Health Network; 2 Interlink Community Cancer Nurses’ Toronto, Ontario Nursing workload measurement using validated instruments is a standard in hospitals. These instruments have limited relevance for predicting nursing resource use in community-based oncology nursing care. Care delivery in the community is multifaceted with care focused on the multiple domains of supportive care need. Socio-demographic, social support structure, family, environment, and illness-characteristics and the degree of supportive care need may impact on patient complexity and nursing care need. A measurement system is needed that measures these variables from a supportive care needs perspective that can predict nursing resource use. This paper will describe the development of a “Supportive Care Case Complexity/Intensity of Need Scale (SCCSI)”, based on the Fitch (1997) seven domains (informational, emotional, psychological, social, spiritual, practical, physical) of supportive care needs. The results of the initial validation study to examine the psychometric properties of this instrument for predicting nursing resource use in the community will be described. The potential use of the community-based oncology care will be discussed with a focus on future research priorities. P-24 INTRODUCTION OF A GUIDED IMAGERY PROGRAM FOR SURGICAL ONCOLOGY PATIENTS Stephanie Raimondi, RN, BN; Sylvia Huber, RN, MN, CON(C); Pat LewisVanderbrink, RN, BN; Foothills Medical Centre, Calgary Health Region, Calgary, Alberta Guided imagery is a therapeutic technique that uses the power of the mind to effect physiological and psychological change by focusing on relaxation, positive thoughts and images. Research has shown the benefit of guided imagery in managing stress in everyday life and in a variety of illnesses and treatment settings including surgery and chemotherapy. The stress and anxiety accompanying a cancer diagnosis and its treatment are well-recognized. Patients undergoing cancer surgery experience a variety of physical and emotional stressors. The effectiveness of guided imagery in enhancing recovery by decreasing stress and anxiety pre- and postoperatively and reducing postoperative pain and opioid use has been well documented. In order to help patients cope with distress and challenges, increase their sense of participation in care, and to enhance our holistic approach to nursing care, a guided imagery program was introduced. This presentation will provide an overview of guided imagery as a therapeutic intervention, the process of introducing its use on acute care surgical units, and implications for nursing staff. Patient evaluations regarding the use of guided imagery and its perceived benefit before and after surgery, and as an ongoing strategy to optimize wellness, will be discussed. P-25 NURSING MANAGEMENT OF PATIENTS REQUIRING IRON CHELALATION THERAPY FOR TRANSFUSIONAL IRON OVERLOAD P-26 IMPLEMENTING COLLABORATIVE CARE NURSING PRACTICE ON A GYNECOLOGY-ONCOLOGY SURGICAL UNIT: A SUCCESS STORY Barbara Hues, RN, BScN, CON(C); CancerCare Manitoba, Winnipeg, Manitoba Pat Lewis-Vandenbrink, BN; Tanya Miller, BN; Foothills Medical Centre, Calgary Health Region, Calgary, Alberta Long term dependence on red cell transfusion leads to iron overload since the body has no mechanism to excrete excess iron. Iron is most damaging to the heart, liver, and pancreas, and overload is eventually fatal unless the iron burden is decreased by chelation. Iron overload typically occurs after >20 units of red cells have been given. In the Oncology clinic, the patients most often at risk are those with myelodysplastic syndromes. Providing high quality patient care during staffing shortages and limited financial resources is a challenge faced by today’s health care system. Historical approaches to staffing models are no longer useful in this new environment as they do not produce enduring, cost effective solutions. Creative planning is required to utilize all levels of staff to their potential. The underlying principle is to have the right caregiver for the patient at the right time, in the right place, for the right cost. If this principle is followed, patient outcomes and satisfaction of patients, families and staff will be enhanced. The focus of this presentation will be on the nursing implications of iron chelation therapy with deferoxamine. This drug is given by longterm infusion, either subcutaneously or through a central venous catheter. Treatment is thus a cumbersome process requiring patient education and ongoing monitoring. There are physical, emotional and social consequences for the patient, and the treatment is not suitable for all patients. The nature of myelodysplasia, including limited life span, thrombocytopenia and immune defects add to the challenges of management. Nurses can take responsibility for monitoring patients receiving iron chelation and to assess for both problems and benefits. The presentation will be useful in establishing criteria for initiating and discontinuing iron chelation treatment. Practical insights for a nursemonitored course of treatment will be provided. P-27 SAFE HANDLING: LEARNING FROM THE PAST TO PROTECT OUR FUTURE Christine Gloin, RN, BA, CON(C); Heather Logan, RN; Carment Gosseling, RN; Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario Safe handling of hazardous drugs is a practice that must continually improve in order to protect patients, families, staff and the workplace from unnecessary exposure to potential danger. As oncology nurses who work daily with antineoplastic agents, we believe this is an important issue to examine. In 2003, the Oncology Nursing Society (ONS) released guidelines for safehandling of hazardous drugs. In 2004, the National Institute for Occupational Safety and Health (NIOSH) issued an alert about preventing occupational exposures to antineoplastic and other hazardous drugs in health care settings. These publications led to the formation of a task force in a large tertiary teaching facility. The purpose of this task force was to collaboratively compare current practice within the facility to the newly published guidelines. The task force consisted of staff members from nursing, pharmacy, risk management, occupational health, environmental services and strategic sourcing. The focus areas scrutinized by the task force included inpatient and outpatient settings where the highest volume of hazardous drug storage, preparation, administration and disposal occurs. This poster will briefly illustrate: 1) the process involved in identifying safe handling practice, 2) procedures that needed modification, 3) implementation of new practices, and 4) in particular the impact on nursing and pharmacy. Successes, ongoing challenges and future directions will be shared. Due to staffing constraints and a desire by the Licensed Practical Nurses to increase their responsibilities and job satisfaction, their role was expanded. This resulted in restructuring of the care delivery model from team nursing to a Collaborative Care Nursing Model. RN’s and LPN’s work in collaboration, with individual assignments based on acuity and needs of patients and competencies, skills, experience of staff. This presentation focuses on how this initiative, of increasing the LPN’s scope of practice was implemented on a 27 bed Gynecology-Oncology Surgical Unit and how it led to the Collaborative Nursing Care model. As well, this presentation will share outcome data post implementation. CHEMOTHERAPY PROTOCOL P-28 HYPERSENSITIVITY AND ANAPHYLAXIS Gail Macartney, RN, MSc(A), ACNP, CON(C); Sean Hopkins, BSP; Lynne Jolicoeur, RN, BScN, CON(C); The Ottawa Hospital, Ottawa, Ontario Anaphylaxis and hypersensitivity reactions are feared complications related to chemotherapy delivery. When it is suspected, nurses do not have time to search for and read lengthy policies and procedures to determine their next steps. This easy to follow protocol was developed by a multidisciplinary team including nurses, pharmacists and physicians to facilitate appropriate decision making when anaphylaxis or hypersensitivity reactions are suspected. This protocol helps nurses identify the systemic clinical presentation of hypersensitivity and anaphylaxic reactions. High-risk drugs are identified. The assessment criteria and medical interventions are clearly outlined. Patient education and documentation guidelines are also included. This protocol can be useful in establishing nursing policies and procedure or unit specific medical directives. This poster presentation will outline the protocol. Copies of this userfriendly decision aid will be made available for electronic distribution. Additionally, posters can be enlarged, laminated and posted in chemotherapy treatment units for easy reference. No chemotherapy unit should be without one! P-29 EFFICACY OF A DECISION AID FOR TAMOXIFEN CHEMOPREVENTION MADE AVAILABLE ON THE WEB Wanda Martin, RN, MN; University of Victoria, Victoria, British Columbia A decision-making guide to be used in clinical practice was developed and evaluated to inform eligible women of chemoprevention with tamoxifen and then posted on the world wide web. As with the paper form of this guide, the web version had a poll asking whether the reader is interested in taking tamoxifen. Through this web poll and the “hit counter,” we have been able to evaluate the usefulness of delivering this decision-making guide for tamoxifen chemoprevention in this form. Problems that were encountered in the process and recommendations for web-based health information delivery will be made. Through this presentation we hope to receive feedback on this project and engage in dialogue on the best way to make this type of patient information available. P-31 RADIOTHERAPY IN PATIENTS WITH CARDIAC PACEMAKERS: A NEW CHALLENGE FOR ONCOLOGY NURSES Linda Robb Blenderman, RN, MSc, CON(C); Linda Giles, RN, BScN; Cancer Centre of Southeastern Ontario at Kingston General Hospital, Kingston, Ontario Cardiac devices may be affected by radiation used in the treatment of cancers of the breast, lung, chest wall, head and neck, skin and lymphomas (Last, 1998). The increasing use of cardiac devices has necessitated a Regional Cancer Centre to explore the Radiotherapy Nurses role with respect to the advanced specialized skill of cardiac monitoring. This presentation will provide an overview of how cardiac devices can impact radiotherapy, the professional and operational assessment of the nurses’ role as well as the challenges faced by the medical team in managing the care for these patients. We will report on results of a provincial and international radiotherapy nurses survey; professional practice standards and radiation oncology standards. It is anticipated that the information gained from this presentation will contribute to the future planning of oncology nurse’s skills to meet the increasing complex needs of cancer patients with co-morbidity conditions such as heart disease. P-30 THE TREATMENT OF GASTRO-INTESTINAL SIDE EFFECTS WITH T1-2 PROSTATE CANCER TREATED WITH 3D CONFORMAL RADIATION Margaret Pavlin, RN, PHN, CON(C); Grace Chan, RN, CON(C); Margaret Fitch, RN, PhD; Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario The gastro-intestinal (G.I.) side effects from radiation therapy for prostate cancer include proctitis and tenesmus. An informal survey of ten Canadian Cancer Centers identified a wide variation in clinical practice governing the management of these symptoms. One approach at our centre is to use psyllium to help control these symptoms. A review of the literature revealed one article to support this practice. The principles of evidence-based practice are based on the use of research, clinical experience and patient outcomes. In order to determine whether further investigations into the use of psyllium is warranted, nurses did a retrospective chart review to determine the prevalence of G.I. symptoms, treatment and overall effectiveness. They also developed a tool to measure the client experience of these symptoms and their impact on quality of life. This presentation will share the results of the review, the process of development of the survey tool and the patient survey. P-33 DEVELOPMENT, IMPLEMENTATION, AND EVALUATION OF A NEW PATIENT INFORMATION PACKAGE – A CHANGE MANAGEMENT STRATEGY Mary Scott, RN; Brenda Ross, RN, BscN; Jaspreet Battu, BScN Student; Hon Chen, BScN Student; Vancouver Centre, BC Cancer Agency, Vancouver, British Columbia; University of Victoria, Victoria, British Columbia Patients newly diagnosed with cancer require information to understand their disease and the treatment options available. Patients who attend busy ambulatory care centers can be expected to have needs for information about their disease, the resources available to them, and treatment options. Some patients will need additional nursing support to understand the treatment plan, make decisions, manage symptoms, and to access community resources. Nursing leaders have been challenged to find new ways to safely and efficiently prioritize patients’ need for nursing care during a time of fiscal restraint. A patient support clinic has been developed to better align nursing resources with patient needs to enhance patient outcomes. Making change can be difficult and nursing leaders had found it challenging to move the patient support clinic forward. Our center supports many student projects including one related to change management. The Unit’s Clinical Nurse Leader and Education Resource Nurse saw an opportunity to support both the learning needs of change project students and the change process itself. The students drafted a population-specific new patient information package in collaboration with the nursing group. The impact of this strategy on the change process and on other patient education strategies will be explored. P-34 DETECTING EPIDURAL SPINAL CORD COMPRESSION (ESCC) IN HIGH-RISK ONCOLOGY PATIENTS P-35 DEVELOPMENT OF AN ORIENTATION TO CLINICAL TRIALS NURSE COORDINATOR Milena Segatore1, RN, MScN, MNI-PG; Karen Lock, RN, BScN, MN, CON(C); 1 North York General Hospital, Toronto, Ontario Karen Sill, RN, CON(C), CCRP; Brenda Ross, RN, BScN; Vancouver Centre, BC Cancer Agency, Vancouver, British Columbia Advances in oncology have prolonged survival of many patients with cancer – unfortunately, frequently at the cost of significant morbidity. As survival has lengthened, there has been a parallel increase in the incidence and prevalence of ESCC in patients living with metastatic disease. Holding the key to preservation of baseline functional status and optimal pain control is early detection and prompt treatment, prior to the onset of neurological deficits. Detection, screening and ongoing clinical assessment by oncology nurses remains critical to achieving good patient outcomes. Retention of ambulatory function and continence are directly related to timeliness of diagnosis: The vast majority of persons ambulatory at diagnosis continue to walk, only half of paretic patients ambulate after treatment, and almost all who have lost their mobility at time of diagnosis never walk again. The role of Clinical Trials Nurse Coordinator is complex and expanding, and integral to an effective and functional Clinical Trials Unit. Recruitment and retention of Clinical Trial Nurse Coordinators is a challenge in our provincial cancer organization. As a result a need for a formal process to introduce nurses to the role was identified and a Clinical Trials Orientation was proposed. The purpose of this presentation is to provide oncology nurses with the knowledge and skills for screening and assessing patients at risk for ESCC. A case-based interactive approach will offer a comprehensive, efficient and feasible method for conducting spinal cord assessment that incorporates historical, functional and classical motor testing elements. Evidence-based assessment tools and clinical algorithms from the clinical neurosciences will be introduced. ESCC is an neurooncologic emergency. Early recognition of the signs and symptoms followed by prompt and aggressive surgical and or medical management are the keys to preserving sensori-motor and sphincter function and ensuring an acceptable quality of life for patients living with metastatic disease. P-36 PATIENT AND FAMILY EMPOWERMENT ON A SURGICAL ONCOLOGY UNIT: DEVELOPING A CARING MODEL OF PATIENT/FAMILY INTERACTION THAT SUPPORTS PARTICIPATION AND INFORMED DECISION MAKING Tracy Soloninka, RN, MBS, MS (oncology candidate), CON(C); Trish Murphy-Kane, RNm BScN, MN (candidate); Natalie Lalor, RN, BScN; Janice Azan, RN, BScN; Mount Sinai Hospital, Toronto, Ontario Patricia Benner states, “Within a practice lies its legacy”1. No where is this statement truer than oncology and palliative care. Spiritual distress becomes an unfortunate “state of being” when surgeons, nurses and the entire multidisciplinary team work at cross purposes and without a cohesive framework in identifying patient and family concerns around diagnosis and deciding next steps. Each of us truly care about the patient, but few of us have the self-awareness to meet and recognize each patient and family in their particular lifeworld. This unit has committed to developing a practice environment where caring and healing is a by-product of the daily team interaction. The Dreyfuss Model of Skill Acquisition supports experiential learning through different levels of defined competency. However, no practitioner can practice beyond their awareness and experience. Using the best practice guideline developed by the Registered Nurses Association of Ontario for Therapeutic Relationships as a foundation for self-reflection and developing self-awareness, the unit has developed a vision and framework to guide patients and families through the challenges of diagnosis and therapy. The presentation will lay out problem identification, needs assessment and program re-engineering of the existing framework. THE ROLE OF Collaboration between the Clinical Trials operational leaders, expert Clinical Trials Nurse Coordinators, and professional practice nursing leaders was essential for the success of this program. The program linked foundational knowledge of clinical trials with the strategies used to successfully implement clinical trials protocols in our organization. Newly hired staff had an opportunity to learn about the elements of clinical trials and their regulatory requirements, and to meet with and discuss trial implementation with members of the interdisciplinary Clinical Trials team. This paper will describe the content of the program and the processes use to introduce generalist oncology nurses to the role of Clinical Trial Nurse Coordinator. Challenges to implementation and plans for the continued refinement of the program will be discussed. P-37 DEVELOPMENT OF A NURSE-LED CLINIC IN GYNECOLOGICAL MALIGNANCY: THE ROLE OF THE ADVANCED PRACTICE NURSE Sharon Thomson, RN, MSc; BC Cancer Agency, Vancouver, British Columbia Evidence has shown that the development of medical/nursing partnerships gives women with a gynecology cancer diagnosis, access to the essential expert knowledge and information they need (Allen, 2003). Women with a gynecological malignancy can present with many different needs during the follow-up phase of their ‘cancer journey’. Nurses in advanced roles are in an excellent position to provide psychological, social and sexual rehabilitation, which are often complex needs of women, especially in the later years of follow-up. The new nurse-led clinic will run alongside a physician’s clinic, with the nurse seeing women within predefined criteria. This allows ready access to the physician should the patient feel they want a medical consultation, or if the nurse feels the patient should be reviewed. The nurse’s role will be to provide information, support, assessment, with any necessary referrals; and routine pelvic examinations and smears, as required, addressing both physical and psychological needs. The nurse-led clinic can therefore improve, not only collaboration with other members of the multi-disciplinary team, but also providing more holistic care of a continuous nature. This presentation will focus on the how the nurse-led clinic has been perceived by the advanced practice nurse, physicians and the women involved, since its introduction. The intended approach on how to evaluate this clinic will also be discussed. P-38 SENTINEL LYMPH NODE BIOPSY: AN INFORMATION GUIDE FOR PATIENTS Lisa Verity, RN, BScN, CON(C); Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario ABSTRACT: Twenty thousand women develop breast cancer in Canada annually and 30% will have lymph node involvement. Over the past decade the treatment of breast cancer has changed. Currently, efforts are focusing on less invasive surgical procedures such as Sentinel Node Mapping. The sentinel lymph node biopsy (SLNB) procedure is a relatively new procedure and it is an option for some. However, there is very little patient information available to help inform women of their choices in this area. There was no written information available in our centre or in any of the other major centres in Toronto. A literature review of SLNB teaching tools resulted in one article that included a patient guide. The author found this to be less than satisfactory. In collaboration with the oncology surgeons, a pamphlet was created that outlines the purpose of the procedure, preparation required, the procedure itself and the associated risks and benefits. The pamphlet is distributed to patients who are in the process of making decisions about their breast cancer treatment. REFERENCES: Swenson KK, Sladek ML, Lally RM, Tuttle TM. (2001). Educating patients on sentinel lymph node dissection for breast cancer. Cancer Practice, 9 (2): 92-96. Zack E. (2001) Sentinel lymph node biopsy in breast cancer: scientific rationale and patient care. Oncology Nursing Forum. 28(6): 997-1005. P-41 NURSING COMPETENCIES AND ORGANIZATIONAL SUPPORTS FOR THE URGENT CARE OF AMBULATORY CANCER PATIENTS: A CANO STANDARDS OF CARE APPROACH Kelly A. Walsh, RN, BSc; Eileen Lacroix, RN, BScN, MPA; Tracy L. Robertson, BScN, RN; Gregory Doiron, BSSc, MHA; Lisa A. Bitonti, BScN, RN; The Ottawa Hospital Regional Cancer Centre, Ottawa, Ontario Over the last decade, there has been a significant shift in cancer treatment delivery from the in-patient to the ambulatory environment. Increasingly complex and toxic treatment protocols and/or advancing disease can cause rapid, critical complications requiring urgent care. Resource-strapped hospital emergency rooms and homecare services contribute to the rise in urgent cases treated in ambulatory centres. Ambulatory oncology nurses require the appropriate knowledge and skills to provide urgent care as a member of an interdisciplinary team. Administrators are responsible for ensuring the appropriate organizational supports are in place to deliver quality patient care. Patients and families deserve timely access to coordinated, comprehensive care provided by skilled professionals (CANO, 2002). This presentation reports on the evaluation of the urgent care services at one ambulatory Regional Cancer Centre. Clinical nurses used the CANO Standards of Care (2002) as the framework for assessing current practice and operations, developing a plan to address identified practice/operational improvement opportunities, implementing changes and evaluating outcomes. The goals of this presentation are to raise oncology nurses’ awareness of the importance of their role in providing urgent care; to highlight the need for clinical professionals and administrators to work together to improve care; and to share a framework for providing urgent care in the outpatient oncology setting. P-39 MULTIPLE MYELOMA: THE PATIENT’S PERSPECTIVE Donnaleen Vlossak, RN, BScN, CON(C); Toronto Sunnybrook Regional Cancer Centre, Toronto, Ontario Multiple Myeloma is a severe debilitating and incurable malignancy that accounts for 1% of all new cancer cases, usually affecting older patients. It follows a variable and unpredictable course. After decades of clinical trials, patients still face a poor outcome. The purpose of this study was to gain an understanding of the impact of Multiple Myeloma on the patient. The research team felt a strong need to pursue this study in order to gain a better understanding of the ravages of the disease, side effects of the treatments, ability to work and to provide for one’s family, changes in self-image, and related psychosocial issues, and a shortened life expectancy. These issues can be difficult no matter what the patient’s age. This qualitative study was based on a convenience sample of 20 generated from a list of patients currently receiving treatment at Toronto Sunnybrook Regional Cancer Centre. In-depth telephone interviews, lasting from 30 to 90 minutes were taped and then transcribed verbatim. Themes, including decision- making, coping, relationships, dealing with treatments, and hopes for the future, were analyzed in the context of the disease trajectory. This initiative’s main objective is to fill the knowledge gap surrounding life with Multiple Myeloma. It is hoped that by having a more thorough understanding of the patients’ perspectives, the nurse will be better able to response to their needs. CONNECTING THRU IMPRINT CARING P-42 COMMUNICATION TO CONSISTENTLY Pamela J. West, RN, MSc, ACNP, CON(C), CHPCN(C); Rouge Valley Health System, Centenary Site, Toronto, Ontario As nurses working in cancer care, we all have favourite memories of special patients that we have cared for over the years: patients who have touched us deeply. These are patients who have left an imprint on our hearts-patients we will never forget. Nothing, not even time, will ever erase these memories. I contend that the imprint is mutual, experienced yesterday, today and hopefully tomorrow. How can we, as health care professionals, leave our imprint on patients unless we connect with them? Further, how can we connect without utilizing (perhaps even mastering) the art of communication? It is an honour and privilege to connect – really connect – with someone. When this connection involves a health care professional who works in cancer care, the connection and resulting imprint can be profound and last a lifetime. This paper will review basic and advanced communication and will explore what it is that health care professionals and patients feel is important in their connecting with one another. Using survey methodology, patients will share what they would say to a newly diagnosed cancer patient to enable effective communication with the health care team. Health care professionals will reveal what they would like to say to their patients. Results are interesting and refreshingly honest! The real secret is in the connection – where the imprint is left forever – in and on the heart!