CHAPTER 4 - Nursing Pharmacology
advertisement

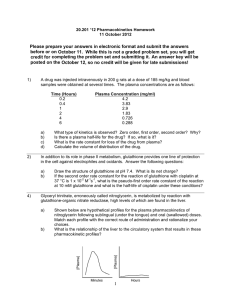
CHAPTER 4 PHARMACOKINETICS LEARNING OUTCOME 1 Explain the applications of pharmacokinetics to clinical practice. Concepts Pharmacokinetics is the movement of drugs through the body and how the body handles medication. Knowing pharmacokinetics allows the nurse to better understand the actions and side effects of medications in patients and the many obstacles, such as membranes, barriers, fluids, and physiological processes, a drug faces to reach its target cells. LEARNING OUTCOME 2 Identify the four components of pharmacokinetics. Concepts Identify the four components of pharmacokinetics. Figure 4.1 Four Processes of Pharmacokinetics LEARNING OUTCOME 3 Explain how substances travel across plasma membranes. Concepts 1. Most drugs must cross plasma membranes to produce their effects. Drugs use one of two processes to cross body membranes: diffusion, or passive transport, and active transport. 2. Diffusion is movement of chemicals from an area of higher concentration to an area of lower concentration. Drug molecules that are small, nonionized, and lipid soluble will usually pass through plasma membranes by diffusion. 3. Active transport is the movement of a chemical against a concentration or electrochemical gradient. Drug molecules that are large, ionized, or water-soluble pass through the plasma membrane by active transport or carrier proteins. LEARNING OUTCOME 4 Discuss factors affecting drug absorption. Concepts Most drugs need to be absorbed to produce an effect. Absorption of medications occurs by the movement of a substance from its site of administration, across body membranes, to circulating fluids. Absorption is the primary pharmacokinetic factor determining the length of time it takes a drug to produce its effect. The following factors can affect drug absorption: route of administration; drug formulation; drug dosage; digestive Adams Ch 04-1 motility; exposure to enzymes in the digestive tract; blood flow to the site of drug administration; degree of ionization of a drug; pH of local environment; and drug–drug, food–drug, or dietary supplement/herbal product–drug interactions. LEARNING OUTCOME 5 Explain the metabolism of drugs and its application to pharmacotherapy. Concepts 1. Metabolism, also called biotransformation, is the process of chemically converting a drug to a form that is more easily removed from the body. The liver is the primary site of drug metabolism. Biochemical reactions such as hydrolysis, oxidation, and reduction occur to medications as they pass through the liver. 2. Most metabolism in the liver is accomplished by the hepatic microsomal enzyme system, which is sometimes called the P-450 system. This system inactivates drugs and accelerates their excretion. 3. Oral drugs enter the hepatic-portal circulation before being distributed to other body tissues. This first-pass effect can metabolize many oral drugs to an inactive form, so other routes of delivery (i.e., sublingual, rectal, or parenteral routes) need to be considered. This process occurs by the drug’s being absorbed and entering the hepatic-portal circulation to go directly to the liver. Here the hepatic microsomal enzymes metabolize drugs to inactive forms and the drug then conjugates and leaves the liver. The final step distributes the drug to the general circulation. See Figure 4.4. 4. Other factors that may affect the pharmacotherapy of drugs metabolized by the liver are chemical alterations that make some drugs more active than the original form; some drugs increase metabolic activity in the liver. Infants and elderly patients have decreased hepatic metabolic activity, patients with severe liver damage have decreased metabolic activity, and patients with certain genetic disorders lack specific metabolic enzymes. In all of these cases, the drug dosage may need to be adjusted. LEARNING OUTCOME 6 Discuss how drugs are distributed throughout the body. Concepts Medications are distributed or transported throughout the body by the blood. The greater the blood flow to an area, the higher concentration of a drug is delivered to that area. 1. Lipid-soluble drugs are more completely distributed to body tissues and are not limited by the barriers that stop water-soluble drugs. LEARNING OUTCOME 7 Describe how plasma proteins affect drug distribution. Concepts 1. Many drugs bind with plasma proteins to form drug–protein complexes. These complexes are too large to cross capillary membranes, so the drug is not distributed to body tissues. Drugs bound to proteins circulate in the plasma until they are released or displaced from the drug–protein complex. 2. Drugs and other chemicals compete with each other for plasma–protein binding sites. Some agents have a Ch 04-2 Adams greater affinity for the binding sites and displace other agents from the plasma proteins. The displaced drug can reach high levels and produce adverse effects. Figure 4.3 Plasma–Protein Binding and Drug Availability Figure 4.4 First-Pass Effect LEARNING OUTCOME 8 Identify major processes by which drugs are excreted. Concepts 1. The primary site of excretion is the kidney. Ionized and water-soluble drugs are filtered at the glomerulus and remain in the filtrate for excretion. Drug–protein complexes are sometimes secreted into the distal tubule of the nephron. Secretion mechanisms are less active in infants and older adults. Certain drugs may be excreted more quickly if the pH of the filtrate is changed. 2. Renal failure will diminish excretion of medications, and drugs are retained for extended times, so dosages must be reduced. 3. Drugs may be excreted by other organs. Drugs that can be changed into a gaseous form are excreted by the respiratory system. Respiratory excretion of drugs depends on diffusion, gas solubility, and pulmonary blood flow. Water-soluble drugs may be eliminated in glandular secretions such as saliva, sweat, or breast milk. Some drugs are eliminated through biliary excretion. LEARNING OUTCOME 9 Explain how enterohepatic recirculation might affect drug activity. Concepts Some drugs are secreted in the bile. Most of the bile is circulated back to the liver by enterohepatic recirculation. A percentage of the drug may be recirculated with the bile numerous times and prolong the activity of the drug for several weeks after therapy has been discontinued. LEARNING OUTCOME 10 Explain the applications of a drug’s plasma half-life (t1/2) to pharmacotherapy. Concepts Plasma half-life is the length of time required for a medication to decrease concentration in the plasma by onehalf after administration. The plasma half-life describes a drug’s duration of action. The greater the half-life, the longer it takes a medication to be excreted. Drugs with short half-lives need to be given more frequently than drugs with long half-lives. The plasma half-life of a drug will increase in a patient with renal or hepatic disease, and to prevent toxic drug levels the drug is given less frequently or the dosage is reduced. Adams Ch 04-3 Figure 4.6 Single-Dose Drug Administration . LEARNING OUTCOME 11 Explain how a drug reaches and maintains its therapeutic range in the plasma. Concepts Repeated doses result in an accumulation of a drug in the bloodstream. A plateau is reached, and the level of the drug in the plasma is maintained continuously within the therapeutic range. At this level equilibrium occurs where the amount of drug administered is equal to the amount of drug eliminated, and there is a continuous therapeutic level of the drug that is being distributed to body tissues. LEARNING OUTCOME 12 Differentiate between loading and maintenance doses. Concepts 1. A loading dose is a higher amount of drug given once or twice so the plateau is reached faster and the drug quickly produces a therapeutic response. 2. Maintenance doses are given to keep the plasma–drug concentration in the therapeutic range. Figure 4.7 Multiple-Dose Drug Administration Ch 04-4 Adams