Practice Leaflet> - Goring & Woodcote Medical Practice
advertisement

New Pond Row Surgery
New Pond Row Surgery
35 South Street
Lancing, BN15 8AN
Telephone: 01903 851073
0870 890 2516
Fax:
Website
www.newpondrow.co.uk
When the surgery is closed call 01903 851073
Welcome to New Pond Row Surgery
We are continuing to develop our surgery website as a way of presenting all our patients with an
up to date resource for all information relating to our practice. We will keep it current with any
news, developments & details that are relevant to the practice & our patients.
Have a look around our website and please do send us some feedback. We can use your thoughts
to improve our online services & further develop the website to make it a more useful, practical
application for our patients.
The ability to order repeat prescriptions on-line remains popular. Later this year we are piloting
online booking for a proportion of appointments and will expand that service if the trial is
successful.
Have your say and join our Patient Participation Group
Ethos of the Practice:
"The continual successful and harmonious development of the practice, its staff and the services
it provides to all stakeholders through the unremitting pursuit of excellence. To be a centre of
excellence, working in partnership with our patients so that we offer services of the standard we
expect our families to receive at the same time providing a happy and balanced working
environment"
If you require urgent Medical Advice out of surgery hours
Please call the new NHS 111 service
Call 999 for any life threatening emergency
MAY CLOSURE TIMES FOR NEW POND ROW SURGERY
MAY DAY 4 MAY 2015
SPRING BANK HOLIDAY 25 MAY 2015
For medical emergencies please call above numbers
Please make sure you put your prescription in early to avoid any delays
Appointment System
Further to the recent trial we have now implemented a revised appointment sytem which we
hope eases access and provides a more flexible service for patients. We have listened to patient
feedback from the trial and adopted changes in an attempt to meet patients' expectations. The
new system builds on the Doctor triage model for urgent needs that we have adopted over the
last 2 years but maintains prebookable future appointments. Once again we will monitor the new
system to ensure it delivers an improved service.Also don't forget there are a limited number of
bookable Saturday morning appointments available each week.
Repeat Prescriptions
If you are on regular medication and your condition is stable, it may be possible to obtain
post-dated prescriptions for up to 6months in advance. Please mention this to your Doctor
or Chronic Disease Nurse specialist at your next review if you are interested in this service.
.
Blood Tests Now By Booked Appointment
Opening Hours
The surgery is open at the following times
Monday:
08:00 to 13:00
14:00 to 19:30
Tuesday:
07:30to 13:00
14:00 to 18:00
Wednesday:
08.00 to 13:00
14:00 to 18:00
Thursday:
08:00 to 13:00
14:00 to 18:00
Friday:
08:00 to 13:00
14:00 to 18:00
Weekend:
Closed
Closed
We operate a saturday morning surgery in conjunction with the other 3 practices in Lancing. A
GP from each of the surgeries are rota'd to work 1 in 4 saturday mornings, that is one of our GP's
will be working every 4th saturday only.
When We Are Closed
At nights and weekends, a recorded message will advise you to contact
111
Please do not ask to see a doctor out of hours unless you genuinely cannot wait until the surgery
re-opens.
Call 999 in an emergency. Chest pains and / or shortness of breath constitute an
emergency.
The surgery will be closed on the following afternoon's from 12:30pm until 5:30pm for staff
training sessions.
12th February 2015; 26th March 2015; 19th May 2015
16th June 2015; 15th July 2015; 16th September 2015
14th October 2015; 18th November 2015
Please note these are subject to change at short notice
Appointments
Monday 8.00 am to 7.30 pm; Tuesday, Thursday and Friday 8.00 am to 6.00 pm; Thursday 7.30
am to 6.00 pm. Saturday 4 pre-bookable appointments are available at Old Shoreham Road
Surgery. The surgery is closed between 1.00 pm and 2.00 pm.
Please remember that all the doctors are not available every day but if the doctor of your choice
is not available you will be offered an appointment with one of the others. Doctor and nurse
appointments are prebookable up to 2 weeks in advance.
In an attempt to meet the demands and expectations of our patients we have over the last 2 years
developed the concept of GP led triage for a significant proportion of the doctor consultations.
The underlying idea of this is to the allow improved access to your Doctor and greater flexibility
for a mutually convenient appointment where this is required. When you feel you need the
advice of a doctor there are now several options open to you: pre-bookable appointment, with the
doctor of your choice, can be made up to 2 weeks in advance (and includes extended week day
hours and Saturday mornings) by contacting the reception. If no suitable appointment is available
you will be offered a pre-bookable appointment with another doctor. If you feel your need is
more pressing than these appointments can provide, you will be invited to be added to the Triage
List on the day you phone(Patients are added to the list between 08.00- 11.00hr). You will
be asked to provide a brief reason for wanting to see the doctor as this assists the doctors grading
the urgency of your case, although we understand you may feel this is a private matter and you
are under no obligation to give a reason, in which case simply tell the receptionist that it is a
'personal matter'. Please make sure reception have an up-to-date contact number. The doctor
will try to phone you back within 2 hours. The outcome of that telephone consultation may allow
resolution of your concern(about 30% of cases), identification of the need for a face-to-face
consultation with the doctor either that day or at a later mutually agreed time(perhaps after
further tests have been undertaken) or management of the problem by another member of the
clinical team.eg. our highly trained practice nurses.
Urgent cases presenting outside the 'Triage Window' are dealt with by the Duty Doctor on call.
Since introducing the above concept we have been able to increase the capacity of appointments
by about 25%. As usual, our patients have been very receptive to innovation in the practice,
where they appreciate that is in attempt to provide a better service, with increasing numbers
favouring the system on patient surveys we have undertaken.
Home Visits
We will visit patients at home if they are too ill or infirm to come to the surgery. Please do not
ask for a visit if you are able to come to the surgery.
We do not consider lack of transport a valid reason meriting a visit from a doctor. It will help us
if requests for home visits are made before 10.00am if possible.
Please allow 3 working days for a repeat prescription request. The white form attached to your
computer prescription can be ticked against the items you need, and the form should then be
placed in the box in the surgery vestibule.
As you will see from this website we are now also offering the facility to order your repeat
prescriptions on-line.
We do not accept repeat prescription requests over the telephone unless you are housebound. If
you provide a stamped addressed envelope, we can post your prescription to you.
Your medical condition and medication will be reviewed regularly. Your prescription will show
a Medication Review date which will usually be set on your Birthday or 6 months after that to
integrate with our Chronic Disease Recall Programme. If the date is overdue when you put in
your request the Doctor will need to review your notes before issuing (for patient safety) and will
reset the date (this may cause a slight delay in signing) the doctor may add a personalised
message advising actions that need to be taken in response to this review. In the unlikely event
that this recall date is more than 6months overdue, please bring this to the attention of the
reception staff.
Prescriptions Charges and Exemptions
Extensive exemption and remission arrangements protect those likely to have difficulty in paying
charges (NHS prescription and dental charges, optical and hospital travel costs).
The NHS prescription charge is a flat-rate amount which successive Governments have thought
it reasonable to charge for those who can afford to pay for their medicines. Prescription
prepayment certificates (PPCs) offer real savings for people who need extensive medication.
NHS charges
From 1 April 2013, the charges are:
Prescription (per item): £7.85
12-month prepayment certificate (PPC): £104.00
3-month PPC: £29.10
If you will have to pay for four or more prescription items in three months, or more than 14 items
in 12 months, you may find it cheaper to buy a PPC. The charge for a single prescription item is
£7.85, whereas a three month PPC will cost you £29.10 and a 12 month PPC £104.00.
Telephone advice and order line 0845 850 0030
General Public - Buy or Renew a PPC On-line
There is further information about prescription exemptions and fees on the NHS website
(www.nhs.uk/NHSEngland/Healthcosts/Pages/Prescriptioncosts.aspx)
Please allow 72 hours, excluding weekends and Bank Holidays, for your request to be processed.
Any problems please telephone the surgery.
Clinics & Services
Clinics and Services
We offer the following clinics and services
Antenatal Care (midwife led clinics off site)
Childhood Immunisations
Coronary Heart Disease clinic
Diabetic clinic
Asthma/COPD checks
Minor Surgery - including cryotherapy
Smoking Cessation Clinics
Travel advice & vaccinations
Contraceptive Services-including Coil Fitting and Implants.
Walk-in Sexual Health Clinics 3:00-6:00pm Wednesdays (New)
Acupuncture ( Dr Starbuck only)
Patients with Chronic Medical Conditions(i.e. Diabetes, Hypertension, Heart Disease,
Asthma/COPD Chronic Kidney Disease and Epilepsy) will receive an invitation to attend the
necessary clinic either Annually or 6monthly depending on the condition. The letter of invitation
explains how the system operates to make sure you have all the appropraite checks each year.
Health Promotion
New patients on repeat medication may require an appointment with a doctor. Women
are advised to make an appointment with the nurse either every 3 or 5 years for a cervical smear
depending on age, invitations will be automatically sent to you by post.
Family Planning
As we are a small practice, we think it more appropriate to offer contraceptive advice and
services by appointment with a doctor, rather than running a separate family planning clinic.
Emergency contraception –the “morning after” pill– can be provided up to three days after a
contraceptive accident. Female doctors are available to provide Coil fitting and Contraceptive
implants. In addition New Pond Row is now hosting a walk-in Sexual Health clinic one day a
week.
Sickness Certificate
You do not need a doctors’ certificate for any illness lasting 6 days or less.Your employer may
however require you to complete a self-certification form (SC2) which is available from your
employer or on the HMRC website (www.hmrc.gov.uk/forms/sc2.pdf) .For any illness lasting
longer than 6 days, you will need a doctor's certificate(Fit Note); the doctor will normally need to
see you or have a telephone consultation with you for this and for any further renewals.
Non NHS Services
These include private sickness certificates of all kinds, insurance claim forms including travel
cancellations, and some medical examinations e.g. HGV and taxi medicals. There is a charge for
these services. The Current price list is on display in the waiting room.
Test Results
Test Results
All special test results (blood tests, urine samples, x-rays etc) are checked by the doctors. You
will be contacted if further action is needed, other than that previously arranged.
Please do not ask receptionists for any test results, unless this was advised by the doctor.
Patient Registration
Pre-registration
If you wish to pre-register click on the link below to open the form. When you have completed
all of the details, click on the "Send" button to mail your form to us. When you visit the surgery
for the first time you will be asked to sign the form to confirm that the details are correct.
Pre-registration Form
When you register you will also be asked to fill out a medical questionnaire. This is because it
can take a considerable time for us to receive your medical records. There is an online version of
this file too, which you may fill out and send to us. When you come to the surgery you will be
asked to sign this form to confirm that the details are correct.
Online medical questionnaire for new patients
Note that by sending the form you will be transmitting information about your self across the
Internet and although every effort is made to keep this information secure, no guarantee can be
offered in this respect.
Alternatively you may print off a registration form, fill it out and bring it in with you on your
first visit to the practice.
Registration Form (www.mysurgerywebsite.co.uk/regforms/gpregistration1.pdf)
Confidentiality
Confidentiality
The practice complies with Data Protection and Access to Medical Records legislation.
Identifiable information about you will be shared with others in the following circumstances:
To provide further medical treatment for you e.g. from district nurses and hospital
services.
To help you get other services e.g. from the social work department. This requires your
consent.
When we have a duty to others e.g. in child protection cases Anonymised patient
information will also be used at local and national level to help the Health Board and
Government plan services e.g. for diabetic care.
If you do not wish anonymous information about you to be used in such a way, please let us
know.
Reception and administration staff require access to your medical records in order to do their
jobs. These members of staff are bound by the same rules of confidentiality as the medical staff.
Suggestions & Complaints
Suggestions & Complaints
We make every effort to give the best service possible to everyone who attends our practice.
However, we are aware that things can go wrong resulting in a patient feeling that they have a
genuine cause for complaint. If this is so, we would wish for the matter to be settled as quickly,
and as amicably, as possible.
Simply contact the Practice Manager and she will set all the necessary wheels in motion. Further
written information is available on the complaints procedure from reception. We are continually
striving to improve our service. Any helpful suggestions would be much appreciated and a
suggestion box is located in the waiting area.
Zero Tolerance
In accordance with Government and NHS Guidelines, this Practice has a policy of zero tolerance
for violent or abusive behaviour towards any member of the Practice Team.
Any patient behaving in such a manner will be removed from our list.
Patient Rights
Patient Rights
You will be treated with respect and as a partner in your care. Being a partner means you have
responsibilities too.
We will:
Ensure our patients have 24-hour access to medical advice.
Aim for you to have access to a suitably qualified medical professional within 48 hours
of your initial contact during surgery hours, or in an urgent case, the same day.
Work in partnership with you to achieve the best medical care possible.
Involve you and listen to your opinions and views in all aspects of your medical care.
The prevention of disease, illness and injury is a primary concern.
The medical staff will advise and inform you of the steps you can take to promote good health
and a healthy lifestyle. We would respectfully ask that you:
Let us know if you intend to cancel an appointment or are running late.
Treat staff with courtesy and respect. Reception staff may have to ask some personal
questions to assist us in providing you with the best service
Inform the practice staff of any alterations in your circumstances, such as change of
surname, address or telephone number. Please ensure that we have your correct telephone
number, even if it’s ex-directory.
As patients, you are responsible for your own health and that of any dependents. It is important
that you adhere to information and advice given to you by health professionals, and co-operate
with the practice in endeavouring to keep you healthy.
Training
GP Training
Medical students and Nursing students attend the practice from time to time. We hope that you
will co-operate with us and help the students to learn about general practice.
However, you will be informed of their presence in advance, and if you do not want them to be
present at a consultation, your wishes will be respected. This will not affect your treatment in any
way.
Friends & Family Test
The FFT is a feedback survey that supports the fundamental principle that people who use NHS
services should have the opportunity to provide feedback on their experience. That feedback
should be used to improve services for patients.
The approach is to be as flexible and inclusive as possible, while minimising the burden on
providers and on patients who want to provide feedback.
The FFT question asks if people would recommend the services they have used and offers a
range of responses. When combined with supplementary follow-up questions, the FFT question
provides a mechanism to highlight both good and poor patient experience.
The free text comments are a rich source of information, which provide staff with a greater depth
of understanding about the experience of patients. The results are available much more quickly
than traditional survey methods, which enables us to take swift action where required.
The FFT results are also one useful source of information which can help to inform choice for
patients and the public. The presentation of the FFT results will change to a more transparent
presentation of the data which both patients and staff will find easier to understand and use.
The results will be available on the Practice Web site; NHS England website and NHS
Choices and providers can use these results to track their progress over time.
The questionnaire will be available in the reception areas from the 1st December 2014, please
spend a moment to complete it and help us shape the future of your surgery
We intend to collate the written comments on a quarterly basis, analysis them from which we
will be able to take note of what our patients likes and what is needed to improve the already
high quality services we supply to our patients. It is our intention wherever practical take your
comments forward and implement them in the practice.
Survey Results
Response Category
Extremely
Likely
Likely
45
24
Neither
Likely
Extremely Don’t
Unlikely
nor
unlikely
Know
unlikely
1
0
1
2
January Collection Method
Hand
Telephone Tablet
Written Call
Kiosk
73
0
0
SMS /
Smartphone
Text
Other
Or On-line
Message
0
0
0
Percentage of extremely likely and likely
Response Category
95%
Total
73
Extremely
Likely
Likely
41
Neither
Likely
Extremely Don’t
Unlikely
nor
unlikely
Know
unlikely
29
8
1
1
Total
2
82
February Collection Method
Hand
Telephone Tablet
Written Call
Kiosk
82
0
SMS /
Smartphone
Text
Other
Or On-line
Message
0
0
0
Percentage of extremely likely and likely
0
85%
Response Category
March
Extremely
Likely
44
Neither
Likely
Extremely
Unlikely
nor
unlikely
unlikely
Likely
21
1
0
Don’t
Know
0
0
Total
66
Collection Method
Hand Telephone Tablet
Written
Call
Kiosk
66
0
SMS /
Smartphone
Text
Other
Or On-line
Message
0
Percentage of extremely likely and
likely
0
0
0
98%
Patient information usage
‘Better Information means better care' leaflet
As you are aware, every household in England is receiving the leaflet ‘Better Information means
better care leaflet (www.england.nhs.uk/wp-content/uploads/2014/01/cd-leaflet-01-14.pdf) ’
during January. The leaflet helps support GP practices in raising awareness amongst patients
about how their information is used for purposes beyond their direct care, including for
the care.data (www.england.nhs.uk/2014/01/15/geraint-lewis/) programme
(www.england.nhs.uk/2014/01/15/geraint-lewis/)
Misconceptions
There are a number of public misconceptions about how data will be used. These are mostly due
to a confusion around the different types of data that will be released by the Health and Social
Care Information Centre (HSCIC). To make it easier for the public to understand, we are
referring to the different types as: red (personal confidential data), amber (pseudonymised)
and green (aggregated or anonymised) data. Each “colour" of data is protected by a different
suite of privacy safeguards. For an explanation, see this blog
(www.england.nhs.uk/2014/01/15/geraint-lewis/) by the Chief Data Officer.
For the avoidance of doubt:
Data will not be made available for the purposes of selling or administering any kind
of insurance (www.england.nhs.uk/2014/01/20/guardian-story/)
Data will not be shared or used for marketing (www.england.nhs.uk/wpcontent/uploads/2014/01/cd-patient-faqs.pdf) purposes
NHS England and the HSCIC will not profit (www.england.nhs.uk/2014/01/20/guardianstory/) from providing data to outside organisations
Privacy Impact Assessment
For patients who wish to understand more about how we protect their data, we have published
a privacy impact assessment (www.england.nhs.uk/wp-content/uploads/2014/01/pia-caredata.pdf) for the care.data programme. This document provides details about the privacy
implications of the programme (both negative and positive) and explains how we are mitigating
each risk. In addition, the HSCIC has published a privacy impact assessment
(www.hscic.gov.uk/media/12931/Privacy-ImpactAssessment/pdf/privacy_impact_assessment_2013.pdf) for all the personal data it processes,
which includes the data extracted for care.data.
Patient Information
Sharing information can help improve understanding, locally and nationally, of the
most important health needs and the quality of the treatment and care provided by
local health services. It may also help researchers by supporting studies that identify
patterns in diseases, responses to different treatments and potential solutions.
See leaflet for details
Care_UK_leaflet.pdf
‘Better Information means better care' leaflet
As you are aware, every household in England is receiving the leaflet ‘ Better Information means better care leaflet
(www.england.nhs.uk/wp-content/uploads/2014/01/cd-leaflet-01-14.pdf) ’ during January. The leaflet
helps support GP practices in raising awareness amongst patients about how their information is used for purposes
beyond their direct care, including for the care.data (www.england.nhs.uk/2014/01/15/geraint-lewis/)
programme (www.england.nhs.uk/2014/01/15/geraint-lewis/)
Misconceptions
There are a number of public misconceptions about how data will be used. These are mostly due to a confusion
around the different types of data that will be released by the Health and Social Care Information Centre (HSCIC).
To make it easier for the public to understand, we are referring to the different types as: red (personal confidential
data), amber (pseudonymised) and green (aggregated or anonymised) data. Each “colour" of data is protected by a
different suite of privacy safeguards. For an explanation, see this blog
(www.england.nhs.uk/2014/01/15/geraint-lewis/) by the Chief Data Officer.
For the avoidance of doubt:
Data will not be made available for the purposes of selling or administering any kind of insurance
(www.england.nhs.uk/2014/01/20/guardian-story/)
Data will not be shared or used for marketing (www.england.nhs.uk/wpcontent/uploads/2014/01/cd-patient-faqs.pdf) purposes
NHS England and the HSCIC will not profit (www.england.nhs.uk/2014/01/20/guardianstory/) from providing data to outside organisations
Privacy Impact Assessment
For patients who wish to understand more about how we protect their data, we have published a privacy impact
assessment (www.england.nhs.uk/wp-content/uploads/2014/01/pia-care-data.pdf) for the care.data
programme. This document provides details about the privacy implications of the programme (both negative and
positive) and explains how we are mitigating each risk. In addition, the HSCIC has published a privacy impact
assessment (www.hscic.gov.uk/media/12931/Privacy-ImpactAssessment/pdf/privacy_impact_assessment_2013.pdf) for all the personal data it processes, which
includes the data extracted for care.data.
Travel Information
info12_field1
Disabled Access
Our surgery has suitable access for disabled patients.
All the patient areas including the waiting room, the consulting rooms and the toilets, have
wheelchair access.
On-Line access
As part of the government's initiative of communication with the surgery, the following services
will be available on-line from the 1st April 2015
[1] On-line repeat prescriptions will be accessible via an on-line facility, those currently using
this website will be contacted and invited to move to the 'Patient UK' facility. on 31st March
2015 the option to use this site for ordering your repeat prescription will cease. Those wishing to
take up this opportunity will be given the option to do so.
[2] Booking and cancelling appointments - initially a very limited number of appointments will
be available to be booked and will be confined to the appointments for Monday evenings
[6:30pm to 7:30pm] and early morning on one day per week [7:30am to 8:00am] but will
increase the availability later on
[3] Access to medical records - you will be able to view the summary of your personal medical
records on-line, the information will be restricted at the moment to Medication; test results;
problems; allergies and the topics will widen in the future
Over the coming months we will be sending a letter of invitation to join the schemes which will
necessitate you visiting the surgery with a form of identification which will trigger a password
and instructions how to join the scheme
Patients Medical Library(beta version)
(www.webmentorlibrary.com/pdffiles/pilsl8.pdf)
Ear Care
ONLY FOR PATIENTS WITH NEW ONSET DEAFNESS
OR KNOWN PROBLEMS WITH EAR WAX
Ear Syringing/Ear Care – Self Help for Patients
We have changed from Ear Syringing to Ear Bulbing. It is more effective, safer and less
uncomfortable
If there is a build-up of wax in your ear(s) please read the following self-help guide as you may
not need an appointment.
What is ear wax?
Ear wax is normal and is produced to form a protective coating over the skin in the ear canal.
Ears are normally self-cleaning – the movement of your jaw whilst eating and talking helps to
move the wax along the canal where it will usually fall out naturally without you noticing.
Why is my ear blocked with wax?
The amount of ear wax produced varies from person to person; some people produce excessive
amounts which can lead to a blockage in the ear canal.
You are more likely to develop a blockage of wax in the canal if you:
use cotton ear buds to clean your ears as this pushes the wax deeper into the canal
wear a hearing aid, ear plugs or use in-ear speakers for iPods or similar - as these can all
interfere with the natural process of wax expulsion
have abnormally narrow ear canals
have a particularly hairy ear canal
are elderly – because the ear wax you produce is drier and harder
have a dry skin problem such as eczema or psoriasis
Advice to help you manage and prevent ear wax blockage
If you experience any of the following, you should seek advice from your GP or Nurse
Practitioner
pain
discharge or bleeding from the ear
sudden deafness or buzzing
foreign bodies in the ear
dizziness
Prevention
If your ears are regularly becoming blocked with wax, after clearing the blockage we will usually
suggest that you use olive oil drops as above around once per week to keep the wax soft and
encourage the natural process of wax expulsion. Do NOT use cotton buds – they only make
things worse.
Treatment:
Step One- Olive oil Drops
The following needs to be done 2 -3 times daily for a minimum of 14 days.
Lie on your side with the most affected ear uppermost
Pull the outer ear gently backwards and upwards to straighten the ear canal
Put 2-3 drops of olive oil into the affected ear(s) and gently massage just in front of the
ear
Stay laying on your side to allow the wax to soak in for around 10 mins
Afterwards, wipe away any excess oil but do not plug your ear with cotton wool as this
simply absorbs the oil
Your hearing problem may initially worsen after first starting to use the olive oil drops; this is
why we advise you to concentrate on treating one ear at a time if both ears are blocked with wax.
Proceed to Step Two if no results.
Step Two- Self Syringing with an Ear Syringing Bulb
The ear syringing bulb can be purchased from any chemist on its own or with ear drops as
combination pack. Instructions on how to use will be given by chemist. Examples include the
Portia Rubber 60 ml Ear Syringe and the Otex Express Combi pack. Ear syringing bulbs are
widely used in the US and Europe and are the standard way of managing ear wax in those
countries.
The bulb is very easy to use, safe and reusable. It is preferable to use olive oil drops instead of
hydrogen peroxide drops which may be supplied in a combination pack.
Proceed to Step 3 if no improvement
Step Three- Single treatment Ear Irrigation (Ear Syringing)
Please book an appointment to see our practice nurses for Ear Irrigation (Syringing)
This treatment is offered only once as it may be uncomfortable and not very effective
Proceed to Step 4 if no improvement
Step Four- Referral for Microsuction
Referral will be made by the clinician where appropriate
Further information is available from www.patient.co.uk (www.patient.co.uk/) or from NHS 111
on 111.
October 2014
Asthma
Asthma is a common condition that affects the airways. The typical symptoms are
wheeze, cough, chest tightness, and shortness of breath. Symptoms can range from
mild to severe. Asthma cannot be 'cured', but treatment usually works well to ease
and prevent symptoms. Treatment is usually with inhalers. A 'typical' person with
asthma may take a preventer inhaler every day (to prevent symptoms developing),
and use a reliever inhaler as and when required (if symptoms flare up).
This leaflet gives a general overview of asthma. There are other leaflets in this series called
'Asthma - Picture Summary', 'Asthma - Peak Flow Diary', 'Asthma - Peak Flow Meter' and
'Inhalers for Asthma'.
What is asthma and who does it affect?
Asthma is a condition that affects the smaller airways (bronchioles) of the lungs. From time to
time the airways constrict (narrow) in people who have asthma. This causes the typical
symptoms. The extent of the narrowing, and how long each episode lasts, can vary greatly.
Asthma can start at any age, but it most commonly starts in childhood. At least 1 in 10 children,
and 1 in 20 adults, have asthma. Asthma runs in some families, but many people with asthma
have no other family members affected.
What are the symptoms of untreated asthma?
The common symptoms are cough and wheeze. You may also become breathless, and develop a
feeling of chest tightness. Symptoms can range from mild to severe between different people,
and at different times in the same person. Each episode of symptoms may last just an hour or so,
or persist for days or weeks unless treated.
What are the typical symptoms if you have mild (untreated) asthma?
You tend to develop mild symptoms from time to time. For example, you may develop a mild
wheeze and a cough if you have: a cold, a chest infection, be in the hay fever season, or when
you exercise. For most of the time you have no symptoms. A child with mild asthma may have
an irritating cough each night, but is often fine during the day.
What are the typical symptoms if you have moderate (untreated) asthma?
Without treatment: you typically have episodes of wheezing and coughing from time to time.
Sometimes you become breathless. You may have spells, sometimes long spells, without
symptoms. However, you tend to be wheezy for some of the time on most days. Symptoms are
often worse at night, or first thing in the morning. You may wake some nights coughing or with a
tight chest. Young children may not have typical symptoms. It may be difficult to tell the
difference between asthma and recurring chest infections in young children.
What are the typical symptoms of a severe attack of asthma?
You become very wheezy, have a 'tight' chest, and have difficulty in breathing. You may find it
difficult to talk because you are so breathless. Severe symptoms may develop from time to time
if you normally have moderate symptoms. Occasionally, severe symptoms develop 'out of the
blue' in some people who normally have just mild symptoms.
What causes asthma?
Asthma is caused by inflammation in the airways. It is not known why the inflammation occurs.
The inflammation irritates the muscles around the airways, and causes them to squeeze
(constrict). This causes narrowing of the airways. It is then more difficult for air to get in and out
of the lungs. This leads to wheezing and breathlessness. The inflammation also causes the lining
of the airways to make extra mucus which causes cough and further obstruction to airflow.
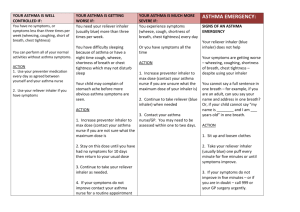
The following diagram aims to illustrate how an episode of asthma develops.
What can make asthma symptoms worse?
Asthma symptoms may flare up from time to time. There is often no apparent reason why
symptoms flare up. However, some people find that symptoms are triggered, or made worse, in
certain situations. It may be possible to avoid certain triggers which may help to reduce
symptoms. Things that may trigger asthma symptoms include the following.
Infections. Particularly colds, coughs, and chest infections.
Pollens and moulds. Asthma is often worse in the hay fever season.
Exercise. However, sport and exercise are good for you if you have asthma. If necessary,
you can use an inhaler before exercise to prevent symptoms from developing. But, as a
rule, exercise-induced asthma often represents under-treated asthma. If it occurs it may
indicate a need to step up your usual preventer treatment (see below).
Certain drugs. For example, about 1 in 50 people with asthma are allergic to aspirin
which can trigger symptoms. Other drugs that may cause asthma symptoms include: antiinflammatory painkillers such as ibuprofen (eg Neurofen®), diclofenac, etc, and betablockers such as propranolol, atenolol, or timolol. This includes beta-blocker eye-drops
used to treat glaucoma.
Smoking and cigarette fumes. If you smoke and have asthma, you should make every
effort to stop. See a practice nurse for help if you find it difficult. 'Passive' smoking can
make asthma worse too. Even where adults smoke away from the presence of children,
smoke on clothes, hair, etc, may make asthma worse. All children deserve to live in a
smoke-free home. In particular, children with asthma.
Other fumes and chemicals. For example, fumes from paints, solvents and pollution.
The increase in air pollution may be a reason why asthma is becoming more common.
Emotion. Asthma is not due to 'nerves', but such things as stress, emotional upset, or
laughing may trigger symptoms.
Allergies to animals. Such as pet cats, dogs, and horses. Animals do not trigger
symptoms in most cases, but some people notice that their symptoms become worse
when close to certain animals.
House dust mite. This is a tiny creature that lives in mattresses and other fabrics around
the home. If you are allergic to it, it may make symptoms worse. It is impossible to get
rid of house dust mite completely. To greatly reduce their number takes a lot of time and
effort and involves: using special mattress covers, removing carpets, removing or treating
soft toys, etc. However, if symptoms are difficult to control with treatment, and you are
confirmed to be allergic to house dust mite, then it may be worth considering trying to
reduce their number. See separate leaflet called 'Allergy to House Dust Mite and Pets'.
Some foods. This is uncommon. Food is not thought to be a trigger in most cases.
Some people only develop symptoms when exposed to a certain 'trigger'. For example, exerciseinduced asthma. As mentioned above, exercise can make symptoms worse for many people with
asthma. But, some people only develop symptoms when they exercise, and are fine the rest of the
time. Another example is that some people only develop symptoms when exposed to specific
chemicals.
How is asthma diagnosed?
Sometimes symptoms are typical, and the diagnosis is easily made by a doctor.
If there is doubt then some simple tests may be arranged. A peak flow meter is commonly used
to help confirm that symptoms are due to asthma (see below). Sometimes a test called spirometry
may be done to confirm the diagnosis. This involves breathing into a machine that measures the
rate and volume of airflow in and out of your lungs.
What is the the peak flow meter?
This is a small device that you blow into. A doctor or nurse will show you how. It measures the
speed of air that you can blow out of your lungs. No matter how strong you are, if your airways
are narrowed, your peak flow reading will be lower than expected for your age, size, and sex. If
you have untreated asthma, then you will normally have low and variable peak flow readings.
Also, peak flow readings in the morning are usually lower than the evening if you have asthma.
You may be asked to keep a diary over two weeks or so of peak flow readings. Asthma is usually
confirmed if you have low and variable peak flow readings over several days. Peak flow readings
improve when the narrowed airways are opened up with treatment. Regular peak flow readings
can be used to help assess how well treatment is working.
What are the treatments for asthma?
For most people with asthma, most of the symptoms can be prevented with treatment. So, you
are able to get on with normal life, school, work, sport, etc.
Inhalers
Most people with asthma are treated with inhalers. Inhalers deliver a small dose of drug directly
to the airways. The dose is enough to treat the airways. However, the amount of drug that gets
into the rest of your body is small so side-effects are unlikely, or minor. There are various inhaler
devices made by different companies. Different ones suit different people. A doctor or nurse will
advise on the different types. See separate leaflet called 'Asthma - Inhalers' for more details.
Drugs delivered by inhalers can be grouped into 'relievers', 'preventers' and 'long acting
bronchodilators'.
A reliever inhaler is taken 'as required' to ease symptoms. The drug in a reliever inhaler
relaxes the muscle in the airways. This makes the airways open wider, and symptoms
usually quickly ease. These drugs are also called 'bronchodilators' as they dilate (widen)
the bronchi and bronchioles (airways). There are several different reliever drugs. For
example, salbutamol and terbutaline. These come in various brands made by different
companies. If you only have symptoms every 'now and then', then the occasional use of a
reliever inhaler may be all that you need. However, if you need a reliever inhaler three
times a week or more to ease symptoms, a preventer inhaler is usually advised.
A preventer inhaler is taken every day to prevent symptoms from developing. The drug
commonly used in preventer inhalers is a steroid. There are various brands. Steroids work
by reducing the inflammation in the airways. When the inflammation has gone, the
airways are much less likely to become narrow and cause symptoms. It takes 7-14 days
for the steroid in a preventer inhaler to build up its effect. Therefore, it will not give any
immediate relief of symptoms. However, after a week or so of treatment, the symptoms
have often gone, or are much reduced. It can take up to six weeks for maximum benefit.
You should then continue with the preventer inhaler every day even when your
symptoms have gone - to prevent symptoms from coming back. You should then not
need to use a reliever inhaler very often, (if at all).
A long acting bronchodilator may be advised in addition to a preventer inhaler. One
may be needed if symptoms are not fully controlled by the preventer inhaler alone. The
drugs in these inhalers work in a similar way to 'relievers', but work for up to 12 hours
after taking each dose. They include salmeterol and formoterol. (Some brands of inhaler
contain a steroid plus a long acting bronchodilator for convenience.)
Spacer devices are used with some types of inhaler. They are commonly used by children, but
many adults also use them. A spacer is like a small plastic chamber that attaches to the inhaler. It
holds the drug like a reservoir when the inhaler is pressed. A valve at the mouth end ensures that
the drug is kept within the spacer until you breathe in. When you breathe out, the valve closes.
So, you don't need to have good co-ordination to inhale the drug if you use a spacer device. A
face mask can be fitted onto some types of spacers, instead of a mouthpiece. This is sometimes
done for young children and babies who can then use the inhaler simply by breathing in and out
normally through the mask.
Tablets to open up the airways
Most people do not need tablets as inhalers usually work well. However, in some cases a tablet
(or in liquid form for children) is prescribed in addition to inhalers if symptoms are not fully
eased by inhalers alone. Some young children use liquid medication instead of inhalers.
Steroid tablets
A short course of steroid tablets (such as prednisolone) is sometimes needed to ease a severe or
prolonged attack of asthma. Steroid tablets are good at reducing the inflammation in the airways.
For example, a severe attack may occur if you have a cold or chest infection.
Some people worry about taking steroid tablets. However, a short course of steroid tablets (for a
week or so) usually works very well, and is unlikely to cause side-effects. Most of the sideeffects caused by steroid tablets occur if you take them for a long time (more than several
months), or if you take frequent short courses of high doses.
What are the dosages of treatment?
Everyone is different. The correct dose of a preventer inhaler is the lowest dose that prevents
symptoms. A doctor may prescribe a high dose of a preventer inhaler at first, to quickly "get on
top of symptoms". When symptoms have gone, the dose may then be reduced by a little every
few weeks. The aim is to find the lowest regular dose that keeps symptoms away.
Some people with asthma put up with symptoms. They may think that it is normal to still have
some symptoms even when they are on treatment. A common example is a night time cough
which can cause disturbed sleep. But if this occurs and your symptoms are not fully controlled tell your doctor or nurse. Symptoms can often be prevented. For example, by adjusting the dose
of your preventer inhaler, or by adding in a long acting bronchodilator.
A 'typical' treatment plan
A common treatment plan for a 'typical' person with moderate asthma is:
A preventer inhaler (usually a steroid inhaler), taken each morning and at bedtime. This
usually prevents symptoms throughout the day and night.
A reliever inhaler may be needed now and then if breakthrough symptoms occur. For
example, if symptoms flare up when you have a cough or cold.
If exercise or sport causes symptoms, then a dose of a reliever inhaler just before the
exercise usually prevents symptoms.
The dose of the preventer inhaler may need to be increased for a while if you have a
cough or cold, or during the hay fever season.
Some people may need to add in a long acting bronchodilator, or tablets, if symptoms are
not controlled with the above.
At first, adjusting doses of inhalers is usually done on the advice of a doctor or nurse. In time,
you may agree an 'asthma action plan' with your doctor or nurse. This means that you make
adjustments to the dose of your inhalers, depending on your symptoms and/or peak flow
readings.
Does asthma go away?
There is no once-and-for-all cure. However, about half of the children who develop asthma 'grow
out of it' by the time they are adults.
For many adults, asthma is variable with some good spells and some spells that are not so good.
Some people are worse in the winter months, and some worse in the hay fever season. Although
not curable, asthma is treatable. Stepping up the treatment for a while during bad spells will often
control symptoms.
Some other general points about asthma
It is vital that you learn how to use your inhalers correctly. In some people,
symptoms persist simply because they do not use their inhaler properly, and the drug
from the inhaler does not get into the airways properly. See your practice nurse or doctor
if you are not sure if you are using your inhaler properly.
See a doctor or nurse if symptoms are not fully controlled, or if they are getting
worse. For example, if:
o a night time cough or wheeze is troublesome
o sport is being affected by symptoms
o your peak flow readings are lower than normal
o you need a reliever inhaler more often than usual
An adjustment in inhaler timings or doses may control these symptoms.
See a doctor urgently if you develop severe symptoms that are not eased by a reliever
inhaler. In particular, if you have difficulty talking due to shortness of breath. You may
need emergency treatment with high dose reliever drugs and other treatments, sometimes
in hospital. A severe asthma attack can be life-threatening.
You should have an influenza immunisation every autumn (the 'flu jab') if you need
continuous or repeated use of high dose inhaled steroids and/or take steroid tablets and/or
have had an episode of asthma which needed hospital admission.
Further help and information
Asthma UK
Summit House, 70 Wilson Street, London EC2A 2DB
Asthma Helpline: 0845 7 01 02 03 Web:
http://www.webmentorlibrary.com/files/external_link.asp?target=http://www.asthma.org.uk
(www.webmentorlibrary.com/files/external_link.asp?target=www.asthma.org.uk)
Offers help and advice, and campaigns for a better deal for people with asthma.
References
Asthma
(www.webmentorlibrary.com/files/external_link.asp?target=www.cks.library.nhs.uk/asth
ma) , Clinical Knowledge Summaries (2007)
British Guideline on the Management of Asthma
(www.webmentorlibrary.com/files/external_link.asp?target=www.sign.ac.uk/guidelines/f
ulltext/101/index.html) , British Thoracic Society and SIGN (May 2008 - updated 2009)
Brian J Lipworth
(www.webmentorlibrary.com/files/external_link_medline.asp?target=www.bmj.com/cgi/c
ontent/full/318/7180/380) ; Modern drug treatment of chronic asthma. BMJ
1999;318:380-384 ( 6 February )
No authors listed
(www.webmentorlibrary.com/files/external_link_medline.asp?target=www.ncbi.nlm.nih.
gov/entrez/query.fcgi?cmd=Retrieve%26db=PubMed%26dopt=Abstract%26list_uids=1
0829349) ; Inhaler devices for asthma. Drug Ther Bull. 2000 Feb;38(2):9-14. [abstract]
Comprehensive patient resources are available at
http://www.webmentorlibrary.com/files/external_link.asp?target=http://www.patient.co.uk
(www.webmentorlibrary.com/files/external_link.asp?target=www.patient.co.uk)
Disclaimer: This article is for information only and should not be used for the diagnosis or
treatment of medical conditions. EMIS has used all reasonable care in compiling the information
but make no warranty as to its accuracy. Consult a doctor or other health care professional for
diagnosis and treatment of medical conditions. For details see our conditions
(www.webmentorlibrary.com/files/external_link.asp?target=www.patient.co.uk/disclaimer.asp) .
© EMIS 2009 Reviewed: 15 Oct 2008 DocID: 4196 Version: 39
disclaimer (www.webmentorlibrary.com/files/disclaimer.asp)
[{0000-0593} pilsl8]
(www.webmentorlibrary.com/pdffiles/pilsl8.pdf)
Asthma
Asthma is a common condition that affects the airways. The typical symptoms are
wheeze, cough, chest tightness, and shortness of breath. Symptoms can range from
mild to severe. Asthma cannot be 'cured', but treatment usually works well to ease
and prevent symptoms. Treatment is usually with inhalers. A 'typical' person with
asthma may take a preventer inhaler every day (to prevent symptoms developing),
and use a reliever inhaler as and when required (if symptoms flare up).
This leaflet gives a general overview of asthma. There are other leaflets in this series called
'Asthma - Picture Summary', 'Asthma - Peak Flow Diary', 'Asthma - Peak Flow Meter' and
'Inhalers for Asthma'.
What is asthma and who does it affect?
Asthma is a condition that affects the smaller airways (bronchioles) of the lungs. From time to
time the airways constrict (narrow) in people who have asthma. This causes the typical
symptoms. The extent of the narrowing, and how long each episode lasts, can vary greatly.
Asthma can start at any age, but it most commonly starts in childhood. At least 1 in 10 children,
and 1 in 20 adults, have asthma. Asthma runs in some families, but many people with asthma
have no other family members affected.
What are the symptoms of untreated asthma?
The common symptoms are cough and wheeze. You may also become breathless, and develop a
feeling of chest tightness. Symptoms can range from mild to severe between different people,
and at different times in the same person. Each episode of symptoms may last just an hour or so,
or persist for days or weeks unless treated.
What are the typical symptoms if you have mild (untreated) asthma?
You tend to develop mild symptoms from time to time. For example, you may develop a mild
wheeze and a cough if you have: a cold, a chest infection, be in the hay fever season, or when
you exercise. For most of the time you have no symptoms. A child with mild asthma may have
an irritating cough each night, but is often fine during the day.
What are the typical symptoms if you have moderate (untreated) asthma?
Without treatment: you typically have episodes of wheezing and coughing from time to time.
Sometimes you become breathless. You may have spells, sometimes long spells, without
symptoms. However, you tend to be wheezy for some of the time on most days. Symptoms are
often worse at night, or first thing in the morning. You may wake some nights coughing or with a
tight chest. Young children may not have typical symptoms. It may be difficult to tell the
difference between asthma and recurring chest infections in young children.
What are the typical symptoms of a severe attack of asthma?
You become very wheezy, have a 'tight' chest, and have difficulty in breathing. You may find it
difficult to talk because you are so breathless. Severe symptoms may develop from time to time
if you normally have moderate symptoms. Occasionally, severe symptoms develop 'out of the
blue' in some people who normally have just mild symptoms.
What causes asthma?
Asthma is caused by inflammation in the airways. It is not known why the inflammation occurs.
The inflammation irritates the muscles around the airways, and causes them to squeeze
(constrict). This causes narrowing of the airways. It is then more difficult for air to get in and out
of the lungs. This leads to wheezing and breathlessness. The inflammation also causes the lining
of the airways to make extra mucus which causes cough and further obstruction to airflow.
The following diagram aims to illustrate how an episode of asthma develops.
What can make asthma symptoms worse?
Asthma symptoms may flare up from time to time. There is often no apparent reason why
symptoms flare up. However, some people find that symptoms are triggered, or made worse, in
certain situations. It may be possible to avoid certain triggers which may help to reduce
symptoms. Things that may trigger asthma symptoms include the following.
Infections. Particularly colds, coughs, and chest infections.
Pollens and moulds. Asthma is often worse in the hay fever season.
Exercise. However, sport and exercise are good for you if you have asthma. If necessary,
you can use an inhaler before exercise to prevent symptoms from developing. But, as a
rule, exercise-induced asthma often represents under-treated asthma. If it occurs it may
indicate a need to step up your usual preventer treatment (see below).
Certain drugs. For example, about 1 in 50 people with asthma are allergic to aspirin
which can trigger symptoms. Other drugs that may cause asthma symptoms include: antiinflammatory painkillers such as ibuprofen (eg Neurofen®), diclofenac, etc, and beta-
blockers such as propranolol, atenolol, or timolol. This includes beta-blocker eye-drops
used to treat glaucoma.
Smoking and cigarette fumes. If you smoke and have asthma, you should make every
effort to stop. See a practice nurse for help if you find it difficult. 'Passive' smoking can
make asthma worse too. Even where adults smoke away from the presence of children,
smoke on clothes, hair, etc, may make asthma worse. All children deserve to live in a
smoke-free home. In particular, children with asthma.
Other fumes and chemicals. For example, fumes from paints, solvents and pollution.
The increase in air pollution may be a reason why asthma is becoming more common.
Emotion. Asthma is not due to 'nerves', but such things as stress, emotional upset, or
laughing may trigger symptoms.
Allergies to animals. Such as pet cats, dogs, and horses. Animals do not trigger
symptoms in most cases, but some people notice that their symptoms become worse
when close to certain animals.
House dust mite. This is a tiny creature that lives in mattresses and other fabrics around
the home. If you are allergic to it, it may make symptoms worse. It is impossible to get
rid of house dust mite completely. To greatly reduce their number takes a lot of time and
effort and involves: using special mattress covers, removing carpets, removing or treating
soft toys, etc. However, if symptoms are difficult to control with treatment, and you are
confirmed to be allergic to house dust mite, then it may be worth considering trying to
reduce their number. See separate leaflet called 'Allergy to House Dust Mite and Pets'.
Some foods. This is uncommon. Food is not thought to be a trigger in most cases.
Some people only develop symptoms when exposed to a certain 'trigger'. For example, exerciseinduced asthma. As mentioned above, exercise can make symptoms worse for many people with
asthma. But, some people only develop symptoms when they exercise, and are fine the rest of the
time. Another example is that some people only develop symptoms when exposed to specific
chemicals.
How is asthma diagnosed?
Sometimes symptoms are typical, and the diagnosis is easily made by a doctor.
If there is doubt then some simple tests may be arranged. A peak flow meter is commonly used
to help confirm that symptoms are due to asthma (see below). Sometimes a test called spirometry
may be done to confirm the diagnosis. This involves breathing into a machine that measures the
rate and volume of airflow in and out of your lungs.
What is the the peak flow meter?
This is a small device that you blow into. A doctor or nurse will show you how. It measures the
speed of air that you can blow out of your lungs. No matter how strong you are, if your airways
are narrowed, your peak flow reading will be lower than expected for your age, size, and sex. If
you have untreated asthma, then you will normally have low and variable peak flow readings.
Also, peak flow readings in the morning are usually lower than the evening if you have asthma.
You may be asked to keep a diary over two weeks or so of peak flow readings. Asthma is usually
confirmed if you have low and variable peak flow readings over several days. Peak flow readings
improve when the narrowed airways are opened up with treatment. Regular peak flow readings
can be used to help assess how well treatment is working.
What are the treatments for asthma?
For most people with asthma, most of the symptoms can be prevented with treatment. So, you
are able to get on with normal life, school, work, sport, etc.
Inhalers
Most people with asthma are treated with inhalers. Inhalers deliver a small dose of drug directly
to the airways. The dose is enough to treat the airways. However, the amount of drug that gets
into the rest of your body is small so side-effects are unlikely, or minor. There are various inhaler
devices made by different companies. Different ones suit different people. A doctor or nurse will
advise on the different types. See separate leaflet called 'Asthma - Inhalers' for more details.
Drugs delivered by inhalers can be grouped into 'relievers', 'preventers' and 'long acting
bronchodilators'.
A reliever inhaler is taken 'as required' to ease symptoms. The drug in a reliever inhaler
relaxes the muscle in the airways. This makes the airways open wider, and symptoms
usually quickly ease. These drugs are also called 'bronchodilators' as they dilate (widen)
the bronchi and bronchioles (airways). There are several different reliever drugs. For
example, salbutamol and terbutaline. These come in various brands made by different
companies. If you only have symptoms every 'now and then', then the occasional use of a
reliever inhaler may be all that you need. However, if you need a reliever inhaler three
times a week or more to ease symptoms, a preventer inhaler is usually advised.
A preventer inhaler is taken every day to prevent symptoms from developing. The drug
commonly used in preventer inhalers is a steroid. There are various brands. Steroids work
by reducing the inflammation in the airways. When the inflammation has gone, the
airways are much less likely to become narrow and cause symptoms. It takes 7-14 days
for the steroid in a preventer inhaler to build up its effect. Therefore, it will not give any
immediate relief of symptoms. However, after a week or so of treatment, the symptoms
have often gone, or are much reduced. It can take up to six weeks for maximum benefit.
You should then continue with the preventer inhaler every day even when your
symptoms have gone - to prevent symptoms from coming back. You should then not
need to use a reliever inhaler very often, (if at all).
A long acting bronchodilator may be advised in addition to a preventer inhaler. One
may be needed if symptoms are not fully controlled by the preventer inhaler alone. The
drugs in these inhalers work in a similar way to 'relievers', but work for up to 12 hours
after taking each dose. They include salmeterol and formoterol. (Some brands of inhaler
contain a steroid plus a long acting bronchodilator for convenience.)
Spacer devices are used with some types of inhaler. They are commonly used by children, but
many adults also use them. A spacer is like a small plastic chamber that attaches to the inhaler. It
holds the drug like a reservoir when the inhaler is pressed. A valve at the mouth end ensures that
the drug is kept within the spacer until you breathe in. When you breathe out, the valve closes.
So, you don't need to have good co-ordination to inhale the drug if you use a spacer device. A
face mask can be fitted onto some types of spacers, instead of a mouthpiece. This is sometimes
done for young children and babies who can then use the inhaler simply by breathing in and out
normally through the mask.
Tablets to open up the airways
Most people do not need tablets as inhalers usually work well. However, in some cases a tablet
(or in liquid form for children) is prescribed in addition to inhalers if symptoms are not fully
eased by inhalers alone. Some young children use liquid medication instead of inhalers.
Steroid tablets
A short course of steroid tablets (such as prednisolone) is sometimes needed to ease a severe or
prolonged attack of asthma. Steroid tablets are good at reducing the inflammation in the airways.
For example, a severe attack may occur if you have a cold or chest infection.
Some people worry about taking steroid tablets. However, a short course of steroid tablets (for a
week or so) usually works very well, and is unlikely to cause side-effects. Most of the sideeffects caused by steroid tablets occur if you take them for a long time (more than several
months), or if you take frequent short courses of high doses.
What are the dosages of treatment?
Everyone is different. The correct dose of a preventer inhaler is the lowest dose that prevents
symptoms. A doctor may prescribe a high dose of a preventer inhaler at first, to quickly "get on
top of symptoms". When symptoms have gone, the dose may then be reduced by a little every
few weeks. The aim is to find the lowest regular dose that keeps symptoms away.
Some people with asthma put up with symptoms. They may think that it is normal to still have
some symptoms even when they are on treatment. A common example is a night time cough
which can cause disturbed sleep. But if this occurs and your symptoms are not fully controlled tell your doctor or nurse. Symptoms can often be prevented. For example, by adjusting the dose
of your preventer inhaler, or by adding in a long acting bronchodilator.
A 'typical' treatment plan
A common treatment plan for a 'typical' person with moderate asthma is:
A preventer inhaler (usually a steroid inhaler), taken each morning and at bedtime. This
usually prevents symptoms throughout the day and night.
A reliever inhaler may be needed now and then if breakthrough symptoms occur. For
example, if symptoms flare up when you have a cough or cold.
If exercise or sport causes symptoms, then a dose of a reliever inhaler just before the
exercise usually prevents symptoms.
The dose of the preventer inhaler may need to be increased for a while if you have a
cough or cold, or during the hay fever season.
Some people may need to add in a long acting bronchodilator, or tablets, if symptoms are
not controlled with the above.
At first, adjusting doses of inhalers is usually done on the advice of a doctor or nurse. In time,
you may agree an 'asthma action plan' with your doctor or nurse. This means that you make
adjustments to the dose of your inhalers, depending on your symptoms and/or peak flow
readings.
Does asthma go away?
There is no once-and-for-all cure. However, about half of the children who develop asthma 'grow
out of it' by the time they are adults.
For many adults, asthma is variable with some good spells and some spells that are not so good.
Some people are worse in the winter months, and some worse in the hay fever season. Although
not curable, asthma is treatable. Stepping up the treatment for a while during bad spells will often
control symptoms.
Some other general points about asthma
It is vital that you learn how to use your inhalers correctly. In some people,
symptoms persist simply because they do not use their inhaler properly, and the drug
from the inhaler does not get into the airways properly. See your practice nurse or doctor
if you are not sure if you are using your inhaler properly.
See a doctor or nurse if symptoms are not fully controlled, or if they are getting
worse. For example, if:
o a night time cough or wheeze is troublesome
o sport is being affected by symptoms
o your peak flow readings are lower than normal
o you need a reliever inhaler more often than usual
An adjustment in inhaler timings or doses may control these symptoms.
See a doctor urgently if you develop severe symptoms that are not eased by a reliever
inhaler. In particular, if you have difficulty talking due to shortness of breath. You may
need emergency treatment with high dose reliever drugs and other treatments, sometimes
in hospital. A severe asthma attack can be life-threatening.
You should have an influenza immunisation every autumn (the 'flu jab') if you need
continuous or repeated use of high dose inhaled steroids and/or take steroid tablets and/or
have had an episode of asthma which needed hospital admission.
Further help and information
Asthma UK
Summit House, 70 Wilson Street, London EC2A 2DB
Asthma Helpline: 0845 7 01 02 03 Web:
http://www.webmentorlibrary.com/files/external_link.asp?target=http://www.asthma.org.uk
(www.webmentorlibrary.com/files/external_link.asp?target=www.asthma.org.uk)
Offers help and advice, and campaigns for a better deal for people with asthma.
References
Asthma
(www.webmentorlibrary.com/files/external_link.asp?target=www.cks.library.nhs.uk/asth
ma) , Clinical Knowledge Summaries (2007)
British Guideline on the Management of Asthma
(www.webmentorlibrary.com/files/external_link.asp?target=www.sign.ac.uk/guidelines/f
ulltext/101/index.html) , British Thoracic Society and SIGN (May 2008 - updated 2009)
Brian J Lipworth
(www.webmentorlibrary.com/files/external_link_medline.asp?target=www.bmj.com/cgi/c
ontent/full/318/7180/380) ; Modern drug treatment of chronic asthma. BMJ
1999;318:380-384 ( 6 February )
No authors listed
(www.webmentorlibrary.com/files/external_link_medline.asp?target=www.ncbi.nlm.nih.
gov/entrez/query.fcgi?cmd=Retrieve%26db=PubMed%26dopt=Abstract%26list_uids=1
0829349) ; Inhaler devices for asthma. Drug Ther Bull. 2000 Feb;38(2):9-14. [abstract]
Comprehensive patient resources are available at
http://www.webmentorlibrary.com/files/external_link.asp?target=http://www.patient.co.uk
(www.webmentorlibrary.com/files/external_link.asp?target=www.patient.co.uk)
Disclaimer: This article is for information only and should not be used for the diagnosis or
treatment of medical conditions. EMIS has used all reasonable care in compiling the information
but make no warranty as to its accuracy. Consult a doctor or other health care professional for
diagnosis and treatment of medical conditions. For details see our conditions
(www.webmentorlibrary.com/files/external_link.asp?target=www.patient.co.uk/disclaimer.asp) .
© EMIS 2009 Reviewed: 15 Oct 2008 DocID: 4196 Version: 39
disclaimer (www.webmentorlibrary.com/files/disclaimer.asp)
[
H0000-0593} pilsl8]
Below is a link to an information sheet on High Blood Pressure
http://www.patient.co.uk/health/High-Blood-Pressure-(Hypertension).htm
(www.patient.co.uk/health/High-Blood-Pressure-(Hypertension).htm)
A Brief History of New Pond Row Surgery
For anyone interested here is a link to a short presentation Dr Starbuck made to the Patient
Participation Group
https://www.dropbox.com/s/nq5xm3kzq1tx3qb/New%20Pond%20Row%20History.pptx
Staff Details
Doctors
Dr David P Starbuck
MB ChB (1979 Leeds) MRCGP PgC(Medical Imaging)
Dr Kay Htun
MB BS (1990 Yangon) MRCGP DFFP
Dr Farhana Anjum
MB BS MRCGP DFFP
Dr Jess Heaver
Based at Old Shoreham Road
Dr Caroline Wilton
Based at New Pond Row
Dr Marianne Jackson
Specialist Nurses
Nurse Vanessa Dimtris
Nurse Amanda Jones
Healthcare Assistants
Ms Julie Goodridge
Practice Management
Mr Derek D Burks
Practice Manager
Mrs L Phillips
Senior Administrator
Mrs Sue Owen
Reception Manager
Mrs Stephanie Seacombe
Manager
Mrs Patsy Smith
Data information Manager
Administration
Mrs Margeret Gibson
Secretary
Ms Linda Power
Clinical Administrator
Reception
Judith
Receptionist
Jennifer
Receptionist
Michelle
Receptionist
Louise
Carol
Admin/Reception
Heather
Reception