About PAGER - Pediatric / Adolescent Gastroesophageal Reflux
advertisement

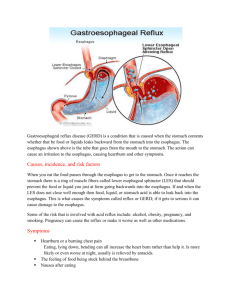
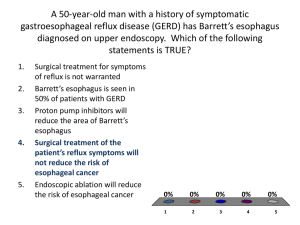
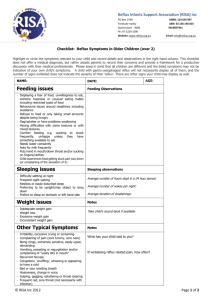
About PAGER The Pediatric/Adolescent Gastroesophageal Reflux Association, Inc. (PAGER) is a 501(c)(3), non-profit organization that was formed in 1992 to provide information and support to parents of children diagnosed with gastroesophageal reflux (GER). Mission PAGER’s mission is to: 1) gather and disseminate information on pediatric gastroesophageal reflux (GER) and related disorders; 2) provide educational and emotional support to patients with GER, their families, and professionals; 3) promote awareness of GER within both the medical community an the general public; and 4) promote research into the causes, treatments, and eventual cure for pediatric GER. provide Services PAGER provides information on tests, procedures, and home-care techniques via brochures, medical journal articles, and video tapes. PAGER also offers an open space for parent-to-parent support and advice from trained expert parents through forums, support groups, e-mail, and on the phone. PAGER staff provide in-service training for professionals and paraprofessionals, and teaches Pediatric GERD 101 classes at local hospitals. PAGER is undertaking several projects to raise awareness of GERD in the medical and parental communities. PAGER also distributes a quarterly newsletter, Reflux Digest. Who We Are PAGER’s governing Board of Directors is comprised of parents of children with GER, adults with GER, and individuals with scientific or professional expertise. PAGER has a very small staff of committed parents as well as a large team of experienced parent volunteers who receive extensive training. History PAGER was founded as the Capital Area Pediatric Heartburn and Reflux Association by Beth Pulsifer-Anderson in 1992. Two years later, Anderson launched one of the first websites for a non-profit organization, where net surfers could access information about GER (which at the time was not readily available). CAPHRA was renamed PAGER in 1996 to reflect its geographic expansion – instead of only working out of Montgomery County, MD, PAGER now includes members across the nation and the world. In 1997, PAGER entered into a partnership with researchers at the Allegheny General Hospital Center for Genomic Studies. Three years later, the researchers successfully mapped the gene for inherited reflux and published their findings in the Journal of the American Medical Association on July 19, 2000. 1998 saw the development of the Expert Parent Volunteer program by an Americorps volunteer. PAGER now maintains a pool of 30 or so trained parent volunteers who can give advice on dealing with reflux. Membership Membership is now free. Parents of children with reflux can sign up and post in PAGER’s on-line forums (found at http://www.reflux.org/reflux/webdoc01.nsf/(vwWebPage)/Forums.htm?OpenDocument) for advice and support. The PAGER website (www.reflux.org) receives over 100,000 hits a month and is the internet’s largest source of information on reflux. Contact P.O. Box 486 Buckeystown, MD 21717-486 301-601-9541 message center http://www.reflux.org gergroup@aol.com 501(c)(3) # 52-1800883 Executive Director: Beth Anderson: 301-213-9533 Volunteer Coordinator: Jennifer Rackley 870-416-2039 * * * About GER Gastroesophageal reflux is the inappropriate backwashing of stomach contents into the esophagus. Reflux occurs when the lower esophageal sphincter muscle that controls the opening between the stomach and the esophagus relaxes too often and/or does not work properly. There are three stages of GER: normal, GER, and GERD. It is common for babies to spit up and/or experience “wet burps;” however, if the infant experiences frequent episodes of reflux and gains weight slowly, he or she may have gastroesophageal reflux. Cases in which reflux causes more severe medical problems are labeled gastroesophageal reflux disease. The severity of GER ranges from mild to life-threatening, and children may experience different symptoms. Common Symptoms of GER and GERD PAIN: irritability, constant/sudden crying, back arching, abdominal pain above the belly button, chest pain, heartburn, burning sensation in the esophagus, pain while swallowing, bloating, throat pain. Rare: Pain migrating to the shoulder join/shoulder blade/back. DIGESTIVE: frequent spitting up and vomiting (especially after six months of age), frequent wet/sour burps, wet hiccups, sensation of food returning into the throat more than an hour after eating. Rare: Projective vomiting, forceful vomiting through the nose and mouth, nausea. EATING: pickiness with foods/textures, food intolerances, tolerating only small amounts at each meal despite hunger, difficulty swallowing, weight loss or slow weight gain, extreme belching, eating only when sleepy, gagging, choking, refusing food. RESPIRATORY: constant runny nose, coughing, choking, wheezing, hoarse voice, frequent sinus and respiratory infections, bronchitis, croup, wheezing asthma, night cough, throat clearing, noisy or labored breathing, breathlessness. Rare: laryngospasms (severe choking), sleep apnea (pauses in breathing), aspiration, pneumonia. DENTAL: bad breath, unusual cavity pattern (holes on the points of teeth rather than in crevices), worn tooth enamel, excessive salivation SLEEP: night waking, pain/heartburn when lying down, coughing, frequent ear infections, resists lying down, only sleeps when upright on shoulder/car seat/wedge DEVELOPMENT: delayed motor milestones due to restricted positioning, excessive crying, anxiety, attention problems due to chronic pain and lack of sleep ESOPHAGEAL: esophageal ulcers, strictures (scars causing food to get stuck when swallowing), globus (painful muscle spasm when swallowing), esophagitis Facts You Should Know About GER - The Mattson Jack Group estimates that approximately 7 million children and adolescents under 17 in the US suffer from GER. - GER is usually diagnosed through a trial of diet and medication. Other procedures to determine diagnoses include an endoscopy (visual examination of the inside of the body using a flexible, lighted tube), a pH probe (a monitoring of the pH by inserting a small probe through the nose into the esophagus), and an upper GI test/barium swallow (where the patient swallows a solution containing barium which coats the esophagus for viewing on a series of x-rays). - Children with reflux can usually be treated by their primary care physician, but those who do not respond to treatment may need to consult a specialist such as a pediatric gastroenterologist, pulmonologist, ENT (Ears, Nose and Throat), or Allergist. - Most children outgrow GER by their second year. For some, however, especially those who a history of reflux in the family, reflux episodes can continue through adolescence and even into adult life. - GER can be aggravated by allergies and food intolerances, as well as smoke, alcohol, and an unhealthy diet. If breast-feeding, the mother may want to keep a log of food intake and monitor intake of high acid foods, caffeine, and spicy food. - Home care techniques include thickening formula or breast milk with rice cereal (heavier food may stay down more easily), holding the baby upright for half an hour after feeding, giving smaller and more frequent feedings, and burping the baby sufficiently. Parents should consult a doctor about specific sleep positioning such as elevating the head of the crib, using a wedge, or other position. - Reflux may appear to subside but may come back during a time of stress, illness, or change of diet. - Kids and adolescents with acid reflux can usually participate in all sports and activities, though sports emphasizing abdominal muscles may aggravate symptoms. - Medication for reflux includes antacids that neutralize acid (like over-the-counter Mylanta or Maalox), acid suppressors (H2s) that reduce acid production (i.e., Zantac, Tagamet, Pepcid, Axid), and acid blockers (PPIs) that eliminate acid production (such as Prevacid, Prilosec, Aciphex, Nexium). Barriers can coat the esophagus or form foam in the stomach, and motility medications can help food to move through the digestive tract (such as Reglan). - Surgery is a last resort but can be called upon if the child is unresponsive to medical treatment or with certain complications, such as aspiration (secretions into the trachea and lungs). A Nissan Fundoplication is the most common surgical procedure for acid reflux in the US. - Foods that are difficult to digest include: broccoli, cabbage, brussel sprouts, tomatoes, onions, garlic, rubbarb, kale, apples, citrus fruits, figs, milk, coffee, tea, carbonated beverages, caffeinated beverages, beans, oats, chili powder, vinegars, chocolate, peppermint, creamy foods, black pepper, honey, gravies, fried fatty food, and foods with “air” (baked goods, sucking from a straw), red meat with connective tissue that has not been tenderized Other Resources Dr. Sears: go to www.askdrsears.com and enter “reflux” in the search line. This site is sponsored by Dr. William Sears, who is both a pediatrician and an author who has written on this topic. National Digestive Diseases Information Clearinghouse of the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institute of Health’s Publication No. 030882, June 2003: http://digestive.niddk.nih.gov/ddiseases/pubs/gerd/ The North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) http://www.naspghan.org/

![Pediatric Gastroesophageal Reflux [10/29/2012]](http://s3.studylib.net/store/data/006891937_1-0f6e6daf80afae340b7d2470e47ece6c-300x300.png)