RISA-Checklist-for-doctors-child over two years
advertisement

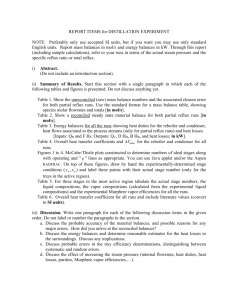
Reflux Infants Support Association (RISA) Inc PO Box 1598 Fortitude Valley Queensland 4006 Ph: 07 3229 1090 Website: www.reflux.org.au ARBN: 124 656 097 ABN: 64 158 190 024 INC9897441 Email: info@reflux.org.au Checklist: Reflux Symptoms in Older Children (over 2) Highlight or circle the symptoms relevant to your child and record details and observations in the right hand column. This checklist does not offer a medical diagnosis, but rather assists parents to record their concerns and provide a framework for a productive discussion with their medical professionals. Please keep in mind that all children are different and the listed symptoms may not be indicative of your own child's symptoms. A child with gastro-oesophageal reflux will not necessarily display all of them, and the number of signs exhibited does not indicate the severity of their ‘reflux'. There are other signs your child may display as well. NAME: DATE: Feeding issues Feeding Observations AGE: - Displaying a fear of food, unwillingness to eat, extreme fussiness or unusual eating habits including restricted types of food - Behavioural issues around mealtimes including avoidance - Refusal to feed or only taking small amounts despite being hungry - Gag/splutter or have problems swallowing - Having difficulties with some textures or with mixed textures - Comfort feeding e.g. wanting to snack frequently, unhappy unless they have something available to eat - Needs water constantly - Asks for milk frequently - Puts hand in mouth/down throat and/or sucking on fingers/clothes - Child experiences food getting stuck part way down (or complaining of the sensation of it) Sleeping issues - Difficulty settling at night - Frequent night waking - Restless or easily disturbed sleep - Preferring to be upright/may object to lying down - Prefers to sleep on stomach or left hand side Weight issues - Inadequate weight gain - Weight loss - Excessive weight gain - Inconsistent weight gain Other Typical Symptoms - Irritability, excessive crying or screaming - Complaining of pain (sore tummy, sore neck) - Being clingy, extremely sensitive, easily upset, demanding - Vomiting, posseting or regurgitation and/or complaining of “yukky bits in mouth” - Recurrent hiccups - Congestion, ‘snuffling’, wheezing or appearing to have a cold - Bad or sour smelling breath - Hoarseness, change in voice - Gulping, gagging, spluttering or throat clearing - Frequent red, sore throat (not necessarily with infection) © RISA Inc 2012 Sleeping observations Average number of hours slept in a 24 hour period: Average number of wakes per night: Average duration of awakenings: Notes Take child’s record book if available Notes What has your child said to you? If verbalising reflux related pain, how often? Page 1 of 2 - Recurrent ear, throat, sinus or chest infections or croup - Drooling or excessive salivation - Unexplained behavioural issues - Asks for Panadol/Dymadon/Paracetamol/ Mylanta NAME: DATE: AGE: Is there a history of gastro-oesophageal reflux in your family? Yes/No Details: Does your child have a history of reflux as an infant? In-home strategies you have tried Notes To minimise reflux: Increase time between dinner/drinks and bed Elevating the bed head to sleep Smaller meals more often Diet Modification: Any dietary modifications you have tried Other Concerns Notes Describe any potential triggers that may be relevant: Bowel motions (e.g. diarrhoea, constipation, mucous, blood, unusual colour, offensive odour) Skin rashes Allergies or intolerances Potential triggers for reflux flares e.g. illness, change of routine, stress, vaccinations, constipation, being overtired, types of food Medical therapies/ investigations: Notes Other medical issues that may be relevant: Medical recommendations © RISA Inc 2012 Notes Page 2 of 2