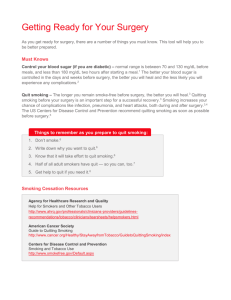
Questions
advertisement

ACNE • QUESTION 1 Your Aunt BettyJo yells at your brother Bud for his “dirty skin and habits” and tells him this is why he has such bad acne. Your reply is – a. Bud IS dirty and he should go scrub his face. b. Tell Bud he is just stressed with the bull riding competition looming and that is why he broke out. c. Calmly, explain to both of them that acne has nothing to do with dirty skin. d. You start crying because of all the horrible flashbacks to your teen years that his conversation has generated. Answer Question 1 C. While you may start crying from your traumatic, acne-scarred past, the best answer is C. Acne is not a result of dirty skin, improper cleansing, stress or other bad habits. Acne is a disease of the pilosebaceous units. All the scrubbing in the world won’t cure acne. QUESTION 2 True or false: Blackheads are dirty whiteheads. ANSWER QUESTION 2 • False. The discoloration of open comedones, or “blackheads”, is not dirt. Just remember acne, black heads, your brother Bud – none of them have to do with dirt! QUESTION 3 A woman in her twenties comes to clinic concerned about her moderate acne. She works as a lifeguard. What do you recommend as a first line agent to treat her acne? • • • • Clindamycin topical gel Tretinoin ointment Oral contraceptives Accutane ANSWER QUESTION 3 C. Oral contraceptives. OCPs are a safe and effective treatment for acne, especially for patients who are do not want to get pregnant. Avoid retinoids in this patient who is out in the sun regularly as it increases photosensitivity. QUESTION 4 An 18 year old man comes to clinic with severe, pustular acne on his back. He’s getting ready to go off to college where he will be on the varsity swim team. He’s terribly embarrassed about his problem and is desperate for help. You recommend: • Benzoyl peroxide wash • Aldapalene ointment • Tetracycline • Isotretinoin ANSWER QUESTION 4 C. Tetracycline. Topical agents may be challenging for this patient as his symptoms are on his back, and he may have difficulty reaching the affected area. Accutane is a possibility, but the physician prescribing it must be registered with the manufacturer’s System to Manage Accutane-Related Teratogenicity (SMART) program and LFTs need to be monitored monthly – not easy to do when he is off at college. Tetracylcine is a better first line choice. QUESTION 5 • Topical Antibiotics should generally be combined with what medicine to avoid inducing bacterial resistance? A: adapalene B: benzoyl peroxide C: isotretinoin D: antibacterial soap ANSWER QUESTION 5 B. Combining topical antibiotics with benzoyl peroxide can help mitigate bacterial resistance. While this combo is good, remember not to combine topical retinoids with benzoyl peroxide as they are oxidized by benzoyl peroxide . QUESTION 6 • Concerning isotretinoin therapy, which of the following is false? A: Monthly monitoring of LFT’s is required B: Women must use two forms of birth control while using isotretinoin C: Most patients require multiple courses of isotretinoin D: Isotretinoin is the only therapy that can induce permanent remission ANSWER QUESTION 6 • When using isotretinoin therapy, LFTs must be monitored monthly, the physician prescribing it must be registered with the manufacturer’s System to Manage Accutane-Related Teratogenicity (SMART) program, and women need to be counseled on the dangers of getting pregnant while on this therapy and then started on birth control. 40% of patients will not need any re-treatment. 40% will have recurrence but it will be able to be treated with agents that did not work in the past. 20% may need to be treated again with isotretinoin therapy. Afib Question 1 • In patients presenting with new onset AF, how often is there a concurrent diagnosis of myocardial infarction? • • • • • A: < 1% B: 2-5% C: 10-15% D: 25-33% E: 45-50% Answer to Question 1 • Answer: B, 2-5% • Active ischemia is associated with new onset atrial fibrillation. However, other signs or symptoms of unstable atherosclerotic disease are usually present at time of presentation. Question 2 • All of the following are risk factors for AF except? • • • • • A: Subclinical hyperthyroidism B: Obesity C: Elevated CRP D: Caffeine intake E: Obstructive sleep apnea Answer to Question 2 • D, caffeine intake • Subclinical hyperthroidism, obesity, elevated CRP, and obstructive sleep apnea are all established risk factors for incident AF. While a relationship exist between caffeine and arrhythmogenesis, there is no established risk of new onset AF in the doses of caffeine consumed by humans. Question 3 • A 72yo male comes to clinic for establishment of primary care. He has atrial fibrillation and receives rate control with a beta-blocker. He has mitral valve prolapse but no other significant past medical history. To reduce his risk of thromboembolism, you recommend: • • • • • A: Warfarin therapy with a goal INR of 2.0-3.0 B: Warfarin therapy with a goal INR of 2.5-3.5 C: ASA 81mg daily D: ASA 325mg daily E: No therapy. Warfarin is “rat poison,” and ASA is worthless. Answer to Question 3 • D: ASA 325mg daily • According to the ACC/AHA guidelines for management of atrial fibrillation, a patient who is less than 75 years old with no risk factors (HTN, EF<35%, CHF, CAD, previous CVA or TIA, DM) should receive ASA 325mg daily. Mitral valve prolapse without mitral stenosis has not been shown to increase risk of thromboembolism. Patients with atrial fibrillation and mitral stenosis should receive warfarin with a goal INR of 2.5-3.5. Question 4 • According to the ATRIA Study, what percentage of patients with atrial fibrillation who quality for anticoagulation are placed on warfarin? • • • • • A: 15% B: 27% C: 45% D: 53% E: 66% • D: 53% Answer to Question 4 • In the ATRIA study, only 53% of 13,428 ambulatory patients with a. fib and no contraindication to anticoagulation received warfarin. Additional studies have suggested that INRs are sub or supra-therapeutic in 26-39% of patients treated with warfarin. Question 5 True or False One advantage to the restoration of sinus rhythm in a patient with new onset atrial fibrillation, is that the patient will not require anticoagulation. Answer to Question 5 • False, if a patient has restoration of sinus rhythm from either electrical or pharmaceutical cardioversion it is suggested that all patients be continued on anticoagulation for at lease 3-4 weeks. It is thought that despite sinus rhythm there is a period of electrical mechanical disassociation following cardioversion and therefore risk of embolism continues. After 3-4 weeks there is still a risk of embolic disease if the patient has asymptomatic paroxysmal episodes of atrial fibrillation and the patient’s individual risk of embolism (i.e. age, structural heart disease) would need to be considered to define approprite anticoagulation. Alcoholism QUESTION 1 1. Mrs. S comes into clinic for the fourth time in 3 months. Her complaint is diffuse pruritis. Physical exam, lab tests and skin biopsy have been unremarkable except an MCV of 99 and an AST on one visit of 66 (ULN=40). She is quite anxious and somewhat agitated on this particular visit at 9:00a.m. She also smells of alcohol. She admits drinking to control her itching and reports alcohol has always been a large part of her and her husband’s social lives. An EToH level in clinic is 79. She refuses help to stop drinking as she thinks this is therapeutic for her itching. What should you do at this point? • • • • Re-evaluate for liver disease as an occult cause of itching Keep patient in clinic for 2-3 hours and call her husband to pick her up. Give both information on AA and other community based options for alcoholism Suspecting this level is not unusual for her, send her home with information on AA and other community based options for treatment Prescribe disulfiram and acomprosate with follow-up in one week *Answer is B. Her level is elevated but not terribly so. She has no signs of chronic liver disease. Keeping her and the community safe by securing transportation is the correct medical legal thing to do. Referral for help and early follow-up is indicated. Work-up for other liver disease can wait until she is not drinking. It may not be indicated at all once she is sober. QUESTION 2 2. Which is not a CAGE question? • • • • • Cut down Craved alcohol more than once a week Annoyed by questions Feel Guilty Eye-opener *Answer: 2 2a. What is the specificity of 2 positive CAGE questions? • 81-95% B) 52-92% C) 100% D) 30% *Answer: A Question 3 3. Mr. R. comes to clinic. His wife is accompanying him and demanding hospitalization for Mr. R for alcohol use. Mr. R.is 64 and his wife reports that he is drinking at least 750cc of grain alcohol daily. Mr. R is combative but coherent and adamantly refuses admission. He agrees to labs and possible outpatient treatment as his wife is threatening to leave him and clean out the checking account. Labs show an AST of 600 and ALT of 450. His PT is 14.1. His Albumin is 3.8. Platelets are 100K and HCT is 35 with an MCV of 102. Alcohol level is 279. The next appropriate step is: • Outpatient referral for psychosocial support in alcohol management • #1 and Disulfiram • Hospital admission • Schedule follow-up in 2 weeks, admonish him not to drink and then suggest outpatient alcohol treatment and naltrexone. *3-He is at high risk of complications from his alcohol abuse. He is likely to have significant withdrawal as his level is so high and yet he is coherent. This suggests dependence and tolerance. His abnormal labs suggest physical consequences and may worsen before improving. QUESTIONS 4. Which of the following is not associated with alcohol abuse? • • • • • Elevated MCV Elevated AST and ALT (more AST) Elevated GGT Elevated White blood cell count Elevated carbohydrate-deficient transferrin *Answer: Elevated White blood count. This is not usually indicative of alcohol use. 5. In patients with alcohol dependence which of the following is appropriate for treatment? • • • • Naltrexone for 6 months followed by psychosocial therapy Naltrexone and acamprosate without psychosocial therapy Brief interventions by the primary care physician Acamprosate with concomitant psychosocial therapy *Answer: 4. Acamprosate with concomitant psychosocial therapy-no therapy without psychosocial support has been studied or is currently appropriate 6. Which of the following statements about oral pharmacologic therapy is true? • • • • Acamprosate is an opioid antagonist that reduces the pleasurable effects of the alcohol Naltrexone is a synthetic analog of GABA which serves to reduce the craving associated with alcohol dependence Disulfiram with alcohol causes increased serum acetaldehyde and flushed face Disulfiram is not approved by FDA for alcohol dependence *Answer: 3. Disulfiram with alcohol causes increased serum acetaldehyde and flushed face Matching 7. Matching. Match the patient with the level of alcohol use: • The lawyer who drinks 8 beers after work three nights a week. Dependence 2. The lawyer who got fired because he was drinking too much and didn’t finish his work. 3. The lawyer who presented with withdrawal seizures. Risky Use Problem Drinking 4. The lawyer who just got his third DUI. Abuse Matching 8. Right before you go in to see one of your established patients, his wife pulls you aside and says that she is worried about how much he drinks. How do you approach this patient? • Immediately call the DMV to have his driver’s license taken away. 2) Prescribe Disulfiram and ask that he take it before he goes out with his friends. 3) Recommend this great new sports bar you just discovered in Raleigh. 4) Spend 15 minutes counseling the patient about his alcohol use and make plans for a follow-up visit to further discuss his drinking. *Answer: 4) Spend 15 minutes counseling the patient about his alcohol use and make plans for a follow-up visit to further discuss his drinking. 10 – 15 minute brief interventions by physicians have been shown to decrease drinking and its consequences at six-month follow-up, with a decrease by 10.5% in the prevalence of risky drinking among patients with heavy drinking but without alcohol dependence. GERD Question 1 Sascha, a 31 yo physician, eats Blazing wings at BW3 Chapel Hill. After dinner, he notes heartburn and epigastric discomfort. Thinking back, most spicy foods cause this sensation. His exam and labs are normal. Which is most appropriate at this time? • • • • • Upper Endoscopy Esophageal manometry Ambulatory 24-hr esophageal pH monitoring Barium swallow Trial of acid suppressive therapy Question 1 E. Trial of acid suppressive therapy Sascha has symptoms of classic GERD and a trial of acid suppressive therapy is best way to confirm diagnosis. Upper endoscopy indicated in patients with complications of GERD, usually characterized by weight loss, odynophagia, dysphagia Question 2 Miriam J., from Robeson County undergoes upper endoscopy for evaluation of dyspepsia. The EGD is normal. Exams, labs including H. pylori, are normal. What is the most appropriate empiric therapy for this patient. • PPI • Placebo • Ondansetron • Tegaserod • Maker’s and Ginger Question 2 A. PPI (although the Maker’s and Ginger would be nice) Some patients with non-ulcer dyspepsia may have GERD or gastric acid hypersensitivity. Up to 50% of patients with non-ulcer dyspepsia have complete resolution of symptoms on a PPI. 5-HT3 antagonists (alosetron and ondansetron) have not demonstrated efficacy. 5-HT4 antagonists (tegaserod) are currently under study for this disorder. 5-HT1 antagonists (sumatriptan, buspirone) do show response, but secondary to side effect profile, they are not currently recommended for non-ulcer dyspepsia (Bytzer P, Talley NJ. Dyspepsia. Ann Intern Med.2001;134(pt 2) 815-822. Question 3 Jason G. has a 20 year history of epigastric discomfort and heartburn. The heartburn is not related to food and used to respond to OTC antacids (not anymore). Upper endoscopy reveals intestinal metaplasia in his distal esophagus. PPI initiated with good symptomatic response. Which is the most appropriate for long-term management? • • • • Laproscopic fundoplication EGD every 2-3 years No follow up needed as he feels well Chronic PPI and EGD every 2-3 years Question 3 D. Chronic PPI and EGD every 2-3 years Surveillance endoscopy and biopsy will identify dysplasia and allow for earlier intervention. Patients found to have Barrett’s may have less transformation to dysplasia if maintained on chronic PPIs. Chronic Renal Failure Self-Assessment Questions (see last slide for answers) • According to the NKF-K/DOQI workgroup, CKD is defined by a GFR of: – – – – – < 20 mL/min/1.73 m2 < 40 mL/min/1.73 m2 < 60 mL/min/1.73 m2 < 80 mL/min/1.73 m2 < 100 mL/min/1.73 m2 Self-Assessment Questions 2. Which of the following U.S. racial/ethnic groups has higher-than-average incidence/prevalence of CKD: – – – – – Caucasians African-Americans Asian-Americans American Indians Everyone except Caucasians Self-Assessment Questions 3. Which out of the following is not a risk factor for progression of CKD – – – HTN Living in New England Hyperlipidemia – – Poverty Gender Self-Assessment Questions 4. A patient with a GFR of 25 asks you what there approximate risk of needing dialysis in the next five years. You tell them – – – – I have no idea, go see a real doctor 5% 1% 20% Self-Assessment Questions 5. Which of the following is not a potential complication of CKD? – – – – – HTN Anemia Hyperphosphatemia Malnutrition Never having to be admitted to 7800 Self-Assessment Questions 6. Patients with which of the following characteristics should be screened for CKD? – – – – – Diabetes Hyperlipidemia HTN A and C All of the above Self-Assessment Questions 7. A pt with stage 3 CKD has a serum phosphate level of 7.0 and a calcium of 7.9 (albumin 3.7). What should be done about his Ca and PO4 levels? – – – – Check a PTH and refer to endocrinology Calcium acetate 3x/daily Sevelamer 3x/daily 970-SPIN Self-Assessment Questions 8. A patient has CKD with a baseline Cr of 2.1, and DM2. BP for the last 2 visits have been 150s/90s, on no current antihypertensives, despite optimal diet and exercise. What would be your first-line agent? – – – – – Lisinopril Amlodipine Metoprolol Clonidine Irbesartan Self-Assessment Questions 9. Which of the following is not a reasonable indication to begin dialysis in a pt with CKD A. A stable Cr of 3.0 in a 50 y/o pt B. Fluid overload refractory to diuretics C. Uremia causing N/V D. Pericarditis E. Refractory poorly controlled HTN Answers to Self-assessment Questions: • C • E • B • D • E • D (HL has not been identified as an RF for the development of CKD, though it has been for progression) • B • A (D would be “non-inferior” to A, but would be much more expensive) • A COPD Questions 1) You should consider the diagnosis of COPD in the following patient types: • 60 year non-smoker with chronic cough and sputum production • 50 year old with a 15 pack-year tobacco history with no chronic respiratory symptoms • 45 yo smoker with 10 pack-year history with dyspnea • All of the above • Only a and c Answer is (D) Question 2 2) Staging of COPD severity is based primarily upon: • Frequency of respiratory symptoms • Severity of respiratory symptoms • FEV1/FVC • FEV1 Answer (D) Question 3 3) Which of the following is false regarding bronchodilators in COPD? • Short-acting inhaled agents such as albuterol and/or ipratropium are indicated in all stages of severity of COPD • Tiotropium is the most potent long-acting bronchodilator in COPD • It is recomended to continue usual doses of ipratropium in COPD patients being prescribed tiotropium D. Theophylline is generally reserved for patients unbale to tolerate inhaled long-acting agents or as an add-on to inhlaed long-acting bronchodilators Answer (C) Question 4 4) • • • • Which of the following is true regarding inhaled corticostreoids in COPD? Normally modifies progression of disease Decreases frequency of flares in COPD patients with severe to very severe disease Recommended for mild and moderate disease- similar to asthma Turbuhaler(R) inhaler provides excellent lung deposition in most COPD patients Answer: (B) Question 5 5) Which of the following is false regarding glucocorticoid-induced osteoporosis (GIO)? • Therapy for GIO only indicated in COPD patients on at least 7.5 mg/day chronically • Calcium citrate + Vit D and a bisphosphonate is a recommended regimen in a patient receiving at least 4 courses of prednisone per year • Calcium + Vit D supplementation is recommended in a COPD patient receiving Advair 500 • All of the above are true Answer: (D) Question 6 6) Antibiotics are indicated in a COPD patient who: • Has increased volume of sputum only with no other signs of infection • Has increased volume and mucopurulence of sputum • Has dyspnea, increased sputum, and sputum is more mucopurulent • Only b and c • Only a and b Answer: (D) Diabetes Health Maintenance Clinical Vignette A 54 y.o. white female with history of GERD, fibromyalgia and hypertension presents to your clinic complaining of fatigue, malaise for 3 months. She denies myalgias or arthralgias. She does not smoke or drink alcohol. Her medications include amitryptiline 50 mg qhs, HCTZ 25 mg qd, amlodipine 10 mg qd, and pantoprazole 40 mg qd. She reports unusual thirst and blurred vision. She denies family history of diabetes, and states her mother had an MI at age 43. BP- 154/ 92, P- 80, regular, calculated BMI- 34. On exam, she is well-appearing and anxious. Exam is otherwise unremarkable. A fasting blood sugar is 278, and you regretfully inform her she has a diagnosis of diabetes. Chem7 panel and CBC is WNL, U/A shows 1+ protein with a SG of 1.012 but is otherwise negative. A1c is pending. What is the patient’s goal blood pressure? (see next slide for answer) Clinical Vignette (2) • Answer: – 130/80 mmHg according to JNC VII guidelines – 125/75 if her proteinuria totals over 1g per day Vignette continued on the next slide Clinical Vignette (3) You correctly decide she needs better blood pressure control. Should you start another medicine or ask her to try lifestyle modification (diet and exercise)? (see next slide for answer) • Clinical Vignette (4) Answer: – With her bp of 154/ 92, you should start another medicine, or increase the dose of an existing medication (although this pt is on essentially maximal doses of her bp meds. With a blood pressures between 130-139/ 80-89, it is appropriate to recommend lifestyle changes up to 3 months, then if not successful add a bp agent. What class of antihypertensives should you strongly consider using in this pt? (see next slide for answer) Clinical Vignette (5) • Answer: – Given proteinuria, start an ACE-I. What other medication would you strongly consider in this patient to reduce her risk of CV events and why? (see next slide for answer) • Clinical Vignette (5) Answer: – ASA 75mg – 162 mg daily, because she has other risk factors for CV disease. What other labwork do you need to more definitely outline her CV risk? (see next slide for answer) Clinical Vignette (5) • Answer: – A fasting lipid panel, with strong consideration of placing her on a statin if LDL > 70. What other medication would you strongly consider in this patient to reduce her risk of CV events and why? (see next slide for answer) Diabetes Screening Case #1 Stacy G. is a 29 y/o male with a hx of heavy smoking who presents to your PM clinic as a new patient. He has a multitude of complaints but most concerning to you (and him for different reasons) is polyuria for several months as well as weight loss. You think he has diabetes, which of the following is appropriate to diagnose diabetes? • • • • • A. check a hemoglobin A1C and tell him he has diabetes when it returns at 7.4 B. check a chem 7 which reveals a BG of 218 mg/dL C. give him a 50g OGTT test D. wait until the following morning and check a fasting glucose and if >125 mg/dL have the test repeated at a later time. E. Don't do any testing because you know he will be noncompliant on his medications and will continue to eat Krispy Kreme doughnuts Case #2 Andy "Toughguy" W. is a 30 y/o male who you see for routine follow up of his diabetes which has been complicated by severe retinopathy w/ 20/400 vision in both eyes. He has missed several appointments and has not seen his opthalmologist. On exam you note his BP is 138/86 after being repeated on several occasions. He asks you if he should be treated for his BP and if so with what drug? • • • • • • • • • • • • • • • Yes, start lisinopril 10mg po daily Yes, start long-acting metoprolol 25mg po daily Yes, start chlorthalidone 10mg po daily Yes, start amlodipine 2.5mg po daily No, his blood pressure is at goal of <140/90 Case #3 Sascha T. is a 75 y/o patient with diet controlled diabetes, HTN, HL, PVD, and smoking. He comes to clinic with a list of things he wants you to "fix". However, he said his wife told him he can't multi-task with anything in life and wants to know what one thing will give him the best chance of living to 100. Which of the following measures will result in the greatest mortality benefit. A. Send him for his annual eye exam B. Tell him to stop smoking C. Increase his atorvastatin to get his LDL below 100 D. Take off his shoes, examine his feet, and suggest that he cut his 2" fungus laden toenails E. Tell him to eat a steak and baked potato with every meal Case #4 You have just finished your rotation on diabetes management when you see one of seven patients with diabetes scheduled to see you in continuity clinic. You feel a little guilty because you have been content with A1C's in the 8-9 range. Now you pull out your ADA guidelines on screening and management for diabetes. Which of these would meet standard of care as established by the ADA? Ordering your long-time 65 y/o diabetic patient their first pneumococcal vaccine Testing for microalbuminuria in patient with a random glucose of 400 mg/dL Checking A1C every six months on your diabetic patient who has been <7 for 3 years Performing a brief foot exam once a year on a diabetic who sees you every 2 months in clinic. Telling the patient to try the Ultimate Double Gravy Biscuit at Biscuitville so you can utilize "shock & awe" when he sees his blood sugar surpass your SAT score Final Question Which of the following is true of diabetics? • • They have similar rates of smoking than nondiabetic counterparts All diabetics should have a dilated eye exam at the time of diagnosis • • • Daily aspirin is recommended for all diabetics for primary prevention They are less likely to have an annual mammogram performed if indicated When seen at Academic centers like Duke, the majority (>50%) of the time their diabetic medications are titrated appropriately Foot, Wrist, Hand Question 1 1. Based on available data, which combination of clinical findings is most likely to have electrodiagnostic testing consistent with CTS? a. Hand pain in all digits, diminished thumb abduction, and diminished sensation to sharp. b. Pain in fourth and fifth digits only, positive Phalen sign, positive Tinel sign c. Positive Flick sign, positive close fist sign, positive square wrist sign (a-p diameter/mediolat dimension at distal wrist crease > 0.7) d. Asymptomatic 55 yo female, works in the logging industry. Answer 1. a. Correct. Each of these clinical findings are predictive of carpal tunnel syndrome confirmed by electrodiagnostic testing. b. Incorrect. This is an unlikely pattern of pain for CTS. Although classically used to diagnose CTS, the Phalen and Tinel signs have not been shown to be predictive of the electrodiagnosis in studies. c. Incorrect. These are potentially predictive of CTS but lack sufficient validation at this time. d. Incorrect. Although a middle aged female lumberjack may be at increased risk for CTS based on epidemiology, she is asymptomatic and electrodiagnostic testing would be inappropriate. If she did have a positive test, this would likely represent a false positive. Question 2 All of the following are associated with Carpal Tunnel Syndrome EXCEPT • Traumatic arthritis and hyperthyroidism • Diabetes Mellitus and corticosteroid use • Pregnancy and use of estrogens • Manufacturing work and amyloidosis • Female gender and h/o Colle’s fracture Answer • Correct – Neither of these conditions are associated with CTS. Inflammatory arthritis and hypothyroidism are. • - E. Each of these has been associated with CTS Question 3 Which of the following is best supported by evidence for the initial management for CTS? • Referral for surgery • Corticosteroid injections • NSAIDs • Wrist splints • Diuretics or Yoga • • • • • Answer Incorrect: Surgery is effective but is generally not done as initial therapy unless the pt presents with evidence of advanced disease (e.g. thenar atrophy). Incorrect: Has been shown to provide at least short term relief, but is generally only considered after more conservative measures have failed. Incorrect: Although typically used in practice, the use of NSAIDs has not been supported by evidence. Correct: Wrist splints provide relief of symptoms in most patients with CTS. Incorrect: Unlikely to be helpful. Question 4 When evaluating the sensation of the hand, the following anatomical areas correlate with which nerve? A) Pulp of index finger – ulnar nerve B) Pulp of the 5th finger – radial nerve C) Dorsal web space between the thumb and index finger – radial nerve D) Pulp of index finger – radial nerve Question 4 Answers A &D) Incorrect: The pulp of index finger is innervated by the median nerve. B) Incorrect: The pulp of the 5th finger is innervated by the ulnar nerve C) Correct: You are so smart! The dorsal web space between the thumb and index finger is innervated by the radial nerve. Question 5 A 65 y/o woman presents with pain in a few of her fingers. Physical exam reveals bony enlargement with little or no inflammation of the affected PIPs and DIPs. What is her most likely diagnosis. • • • • Rheumatoid Arthritis Psoriatic Arthritis Osteoarthritis Who cares? Refer to Rheumatology. Question 5 Answers • Incorrect: Rheumatoid arthritis rarely affects the DIPs and the joint exam would be consistent with inflammation. • Incorrect: Psoriatic Arthritis can affect both the DIPs and PIPs, but is also associated with inflammation. She would also likely have a hx of psoriasis or active lesions at the time of diagnosis. Nail changes would also provide a clue. • Correct: Osteoarthritis has little to no evidence of inflammation on physical exam and does affect both the PIPs and DIPs causing bony enlargement (Bouchards and Heberdens nodes). • Although Rheumatologists are nice people, you can probably handle this one on your own. Question 6 Which of the following is NOT a common causes of plantar fascitis (the most common cause of heel pain)? • • • • • Prolonged standing Obesity Poor flexibility of calf muscles or reduced ankle range of motion Too much stretching Lack of arch support Answer D. Too much stretching. Plantar and heel cord stretches is actually one of several ways to treat heel spur (plantar fascitis). Other treatments include orthoses, rest, NSAIDS, and even surgery. The other answers contribute to development of plantar fascitis. Question 7 A 47-year-old man fell from a ladder at work and presents to urgent care. He report 10/10 ankle pain and is convinces that he has fractured his ankle. He requests Percocet and a work excuse note. He has been ambulatory since the fall. Which of the following is the BEST next step? • Order an ankle serious to rule out fracture • Prescribe Percocet • Perform a careful ankle exam and focus on the tarsal zone • Write a work excuse citing unsafe work environment • Screen the patient for narcotic abuse Answer C. The best next step would be to exam the foot carefully for bony tenderness alone the poster and tip of both lateral and medial malleoli. If the patient does not have tenderness in these areas and since he is ambulatory, ankle x-ray would not be necessary. The other answer could be options depending on the specific situation, they would not be the next best step. Question 8 What of the following about Toe fractures is FALSE? A. Causes include crush injury, hyperabduction, and axial loading. B. They are the MOST common cause of foot fracture. C. They are never emergent. D. “Buddy taping” is the usual treatment. E. Point tenderness is present and may be accompanied by soft tissue swelling and tenderness. Answer C. Emergent referral for toe fractures are indicated for open proximal phalanx fractures, fractures associated with contamination or circulatory instability. The other answers are features of toe fracture. Question 9 Which of the following is NOT a risk factor for metatarsal fractures. • • • • • Hypertension Diabetes Sedentary lifestyle BZP use Osteoporosis Answer A. Hypertension is not a risk factor for metatarsal fractures. Diabetes, especially >25 years is on of the major risk factors. Other risk include sedentary lifestyle, BZP use, and osteoporosis. Repeat direct trauma is a common cause of stress metatarsal fractures. Question 10 When treating patients with metatarsal fractures, the following should be carefully considered EXCEPT. • • • • Early immobilization for 3-5 days Early weight bearing for 24 hours Follow-up exam should focus on pain and point tenderness Displaced fractures should be reduced with regional block • Stress fracture is usually treated by 4-8 weeks of cessation of inciting activity Answer B. Early weight bearing is discouraged for fractures in general and immobilization is used primarily to help with fracture healing and prevention of complications such as displacement or non-union. Early immobilization for 3-5 days is the general rule for metatarsal fractures. Follow-up exam should focus on point tenderness and follow-up x-ray should exam callus formation at the fracture site. Most stress fractures could be management by rest. However, 5 th metatarsal stress fracture require orthopedic referral due to high complication rate. Influenza Questions Your Uncle Fred is worried that this is going to be the year of the “really bad flu,” similar to 1918. You explain to him that pandemics of the flu are caused by: • Antigenic shifts from point mutations • Antigenic shifts from gene segment reassortment • Antigen drift from point mutations • Antigenic drift from gene segment reassortment D. Antigenic shift is caused by point mutations in RNA (leading to epidemics), while antigenic drift is caused by reassortment of gene segments leading to new HA or NA glycoproteins (leading to pandemics) Questions (T/F) Family members of a patient w/ influenza treated with Amantadine should be given prophylaxis w/ Amantadine. Answer: False. If a household contact has the flu and is treated w/ rimantadine or amantadine, there appears to be no benefit to other household members receiving postexposure prophylaxis, probably because resistant virus is transmitted. In contrast, this does not appear to occur w/ oseltamivir and zanamivir. Influenza vaccination in the elderly can: A. Reduce hospitalization B. Reduce Pneumonia C. Reduce stroke D. Reduce heart attacks E. All of the above. Answer: E Questions True or False: You should always test a patient presenting with flu-like symptoms for influenza prior to initiating treatment. Answer: False. During an outbreak of influenza it is more cost-effective to treat empirically. Questions Your Aunt Sally calls to tell you that she thinks that she has the flu. She complains of fevers, myalgias, and fatigue. Over the next 7 days, she does not seem to be getting better. In fact, Sally has now developed shortness of breath and worsening fevers. You tell your Aunt Sally that: • She is just experiencing a severe case of the flu. • She should see her doctor in the next few days. • She should go to the emergency department to be evaluated. Answer: C. In a patient w/ influenza who does not seem to be getting better and develops respiratory symptoms, you should suspect either bacterial or primary viral pneumonia, two potentially deadly complications, which require urgent medical attention. Kidney Stones 2. Which of the following factors is not associated with calcium stones • • • • • High uricosuria High Na diet High oxaluria High citraturia Alkaline pH Go to the next slide for the answer Answer: d. Uric acid acts as a nidus for calcium stones. High Na diet leads to increased urinary calcium. Oxalate binds to calcium in the urine and precipitates calcium-oxalate crystals if present at high concentrations. Alkaline pH precipitates calcium stones. Citrate is the most powerful inhibitor of calcium oxalate stones 3. True or False. In patients with calcium oxalate stones, decreasing calcium intake will lower urinary calcium excretion and will result in less stone formation. Go to the next slide for the answer Answer: False. Lowering calcium intake will result in less calcium chelating oxalate in the GI tract, more oxalate absorption and thus urinary excretion. Hyperoxaluria will cause more calcium stone precipitations 4. True/False: Potassium citrate is routinely used in patients with calcium oxalate stones and low urinary citrate. Go to the next slide for the answer • 4. Answer: False. Although citrate is a powerful inhibitor of calcium oxalate formation and needed in the urine to prevent stones, it also raises the pH which might cause more calcium stone precipitation, especially calcium phosphate. If the urine pH >6, it should be avoided. Knee Pain Questions: (Matching 1-6) 1.46 yo woman with R> L knee pain, gradually worsening over several weeks, worse with walking down stairs. No catching, no trauma. 2.50 yo woman with pain over the medial knee, particularly with crossing her legs. She has pain 2 cm inferior to the medial joint line. 3.30 yo man playing soccer, twisting motion of knee with foot planted, developed an effusion, pain and difficulty walking. 4.35 yo man with right knee pain, swelling and effusion. No similar prior history. Low grade fevers at home. 5. 72 yo man with long standing severe OA now with tenderness and swelling in the popliteal fossa. 6.67 yo man with h/o DM in the ACC with swollen right knee for 4 days, exquisitely tender with similar problem in right great two last year. 7.a.Septic joint b. ACL tear c. Anserine bursitis d. Patellofemoral syndrome e. Gout f. Baker’s cyst 1.D. This is a classic presentation of patellofemoral syndrome which is more common in women and in runners. The lateral compartment of the quadriceps is more developed than the medial, pulling the patella laterally. PE is often benign except for pain with palpation anteriorly over the patella, you may also notice a lateral riding patella. Treat with NSAIDS, strengthening of the medial quads with extension exercises- last 15 degrees of extension. 2.2.C. This presentation is suggestive of Pes Anserine bursitis. This can be managed for 6 weeks with NSAIDS, ice. If continued pain, steroid injections at the site of maximal tenderness- insert needle perpendicular to tibia, advance needle to bone, pull back a small amount, aspirate to ensure not in vessel and then inject 40 mg Depomedrol, 1 cc lidocaine. . 3.B. The concern here is for a ligamentous injury. If his lower legs was hit from behind while his foot was planted, you might think about ACL tear. Conversely, if the lower leg is struck on the anterior surface, such as in an MVA (against a dashboard) you may be more likely to see a PCL tear. You would look specifically for laxity on the anterior, posterior draw, and Lachman test. An orthopedics consult and likely MRI imaging of the affected knee should be pursued. 4.A. This would be concerning for infectious etiology, and you should consider GC. Would ask about pyuria, penile drainage, recent sexual contact. You should do a tap including cultures and gram stain. 5.F. This is most likely a Baker’s cyst which can be a complication of OA, degenerative changes. Would treat as you treat OA. May give joint injections. Do not inject or aspirate in the popliteal fossa. Ultrasound would confirm. 6.E. Recurrent monoarticular arthritis- typically limited to 5-10 days, is suggestive of gout. In this patient, making a crystal diagnosis would be helpful. In this scenario, you would need to tap anyway to r/o infectious causes. 7.54 yo man with blunt trauma to the right knee, acutely painful. There is no effusion or joint laxity and he is able to ambulate. Would you? A. Get plain films and treat with NSAIDs B. Look for tenderness or patella or fibula and get films only if tender C. Given his age, he needs films even though he can ambulate D. No films now, but if he continues to have pain, order MRI as it is much more sensitive. Answer is B. Using the Ottawa, there is no indication for plain radiographs for this patientneg LR 0.11 for fracture. Criteria include age > 55, fibula head tenderness, isolated patella tenderness, inability to flex knee to 90 degrees, inability to bear weight immediately or in ER (4 steps). Manage conservatively with Rest, Ice, Compression, Elevation, NSAIDS. If he continues to have pain at 10 days, plain films should then be obtained 4.8. 72 yo obese man with bilateral knee pain for several years, increasing pain, decreasing ability to walk, morning stiffness, and crepitus. What is the most likely dx and would you image? A.Rheumatoid Arthritis, imaging needed to evaluate for joint damage B.Osteoarthritis, imaging needed to evaluate extent of disease C.Osteoarthritis, imaging not needed as history and exam consistent with Diagnosis D.Parkinson’s with stiffness likely unrelated to knees, refer to neurology C. This presentation is c/w osteoarthritis. Based on clinical predictors alone (see slide 15- sens 95%, spec 69%) which are more sensitive and less specific then clinical plus radiographic findings (sens 91% and spec 86%), the probability that he has OA is 79% based on ACR criteria. There is currently no indication for plain films with initial management. Initial treatment should include APAP, then NSAIDS, resistance training, weight loss. If the above treatments are not effective, may then proceed to intra-articular steroids, consider arthroplasty. • 9. 72 yo man with long standing severe OA now with tenderness and swelling in the popliteal fossa. Your next step is A. Drain popliteal fossa B. Aspirate joint C. Rest, Ice, Compression, Elevation D. Xray and refer to ortho Answer 9: B This is most likely a Baker’s cyst which can be a complication of OA, degenerative changes. Would treat as you treat OA. May give joint injections. Do not inject or aspirate in the popliteal fossa. Ultrasound would confirm Management of Hypertension Cases A 87 y.o. AAM has never visited a physician in his life and comes to see you. His bp is 180/75. He states he has never had any health problems. Your workup of target end-organ damage, along with all bloodwork, is completely negative. (1) Would you start 1 or 2 agents? (2) What would be the first agent you would choose and why? Answers PAP (1) Would you start 1 or 2 agents? Although he falls under the category of stage 2 HTN (and therefore needs to be started on 2 agents), given his advanced age (and likely decreased metabolism), you could consider starting 1 agent, then bringing him back soon (within 2-4 weeks) to start a second agent. Ultimately, he will very likely need 2 agents. (2) What agent(s) would you choose and why? According to the SHEP trial, elderly patients with isolated systolic HTN had a significant decrease in stroke risk when patient were placed on chlorthalidone. You could therefore consider a thiazide diuretic as initial therapy. Questions: 1) A 28 y/o woman with no significant past medical history comes into your clinic to establish care. She is currently sexually active and has had 5 lifetime sexual partners . Her last Pap was 2 yrs ago and was normal. She has had 3 consecutive normal Paps. Does she need to be screened for cervical CA? if yes at what interval?. a) Yes, and screening should be yearly b) Yes, but in light of her prior normal Paps the interval can be decreased to q2-3 yrs c) No, since she’s had 3 consecutive normal Paps screening can be stopped. d) Yes, and since she has not been screened in the past 2 yrs she should be screened twice this yr then if normal resume yearly screens. 2) A 22 y/o woman presents for routine health maintenance in your clinic. She is a graduate student at Duke business school and her past med hx is only sig for h/o depression. She is on an SSRI and denies being currently depressed. She is not currently sexually active and denies prior sexual activity. As part of your routine heath maintenance does she need screening for cervical cancer? If yes why? a) No she does not need screening for cervical cancer since she’s not currently sexually active b) No, she does not need screening since she has never been sexually active. c) Yes, although she is not currently sexually active, her sexual history may be incomplete d) Yes , since every adult woman should be screened yearly regardless of sexual history 3) A 30 y/o woman with h/o HTN presents the acute care clinic with chief complaint of increased vagina discharge. She denies fever or chills or any other associated symptoms. She has not been sexually active for 8mths but has had 15 lifetime sexual partners. She has always used barrier protection with intercourse. As part of your physical exam you performed a pelvic exam which revealed copious discharge from the vagina but generally normal appearing cervix except from a small spot (<1cm) on the posterior cervix which appeared friable bleed easily as you were obtaining culture samples. Which of the following is the most appropriate next step. a) b) c) d) Evaluate her for possible STD and refer to her PCP for further evaluation since this is an acute care visit. Evaluate her for possible STD and screen her for cervical CA by performing a Pap. Evaluate her for possible STD and refer her to a gynecologist for biopsy of the cervical lesion Evaluate her for possible STD and titrate her blood pressure meds if her BP is not at goal. Answers: 1) A is correct. Based on ACS screening recommendation B is incorrect because reducing frequency of screening is recommended in those ages 30 or older. C is incorrect because cessation of screening after 3 consecutive normal pap is recommended only in those over 65y/o. D is incorrect because it describes the screening recommendation for pts with HIV after initial diagnosis. 2) C is correct. The rational was that in the US by age 21 most women are sexually active, also some women may have been victims of rape or sexual abuse and may not disclose this. A and B are incorrect because both USPTF and ACS recommend screening start at age 21. D is incorrect because not all adult women need screening. For instance continued screening those over 65 who have not been sexually active and have had previous normal Pap is not recommended. 3) C is correct. The sensitivity for Pap smear is about 60-80%, therefore a pt with visible lesion should have the lesion biopsied. A, B and C are incorrect because they do not include obtaining a biopsy. 9. A 23 year old with HIV (CD4 600 and VL 100), diagnosed 6 months ago, presents to the Health Department. She is not on HAART. She has a history of HSIL in 2003. What treatment should she have received for HSIL? 10. Being the industrious resident that you are, you perform a Pap smear since immunocompromised patients should be screened twice in the first year of diagnosis. The results return as atypical squamous cells of undetermined significance. What do you do next? 9. and 10. Answers 9. Colposcopy and endocervical curretage, unless a diagnostic excisional procedure was performed. 10. Immunosuppressed patients with ASC-US, regardless of CD4 count, HIV viral load, or antiretroviral therapy, should be referred for colposcopy. Pharm. Marketing Question 1 Congrats! You have been elected chief medical resident and have to manage noon conference lunches for the next year. During last year as a GI fellow you got to know the Astra Zeneca Drug Rep while at the AGA meeting. She calls and asks if she could sponsor a talk in Peptic Ulcer Disease to your residents. She offers to bring lunch, pens, mugs, and a stack of tickets to go see Justin Timberlake at the RBC Center in Raleigh. Question 1 (cont.) Based on what you know about Duke’s Rules you decide to tell her: A) Sure come on down, the interns are hungry, my ACR stole all my pens, and Justin is dreamy. B) Thanks, but I can’t have you do the talk or pass out gifts. If you want to buy us lunch we may be able to work things out with my boss. C) No way! After Janet Jackson’s wardrobe malfunction, I wouldn’t feel Justified. Besides, couldn’t you use that money to pay for Malaria drugs in Africa? Answer 1 The answer is B. According to Duke rules, the drug rep cannot bring gifts. She may sponsor lunch, if the program director and chair agree. Wouldn’t it be nice if the $11 billion spent by drug companies to advertise to us were spent on saving lives? Question 2 Your have just graduated from your Allergy and Immunology fellowship and finally have to work for a living. You move to Columbus, OH where the Buckeye Allergens are high enough to support your career in treating allergic rhinitis. The Schering representative drops by your office and notices that your golf clubs are looking kind of ratty. He offers to hook you up with a new set of clubs and a membership at the Country Club in exchange for your advice on the advantages of Clarinex. Question 2 (cont.) Based on what you know about the ACP and PhRMA’s guidelines on drug marketing you tell him: A) Could you please arrange for a 3PM tee time Monday-Friday I like to get a game in after a hard day in the office. B) My golf game is kind of weak, could you throw in a couple of lessons. C) Sorry I can’t take your bribe, ahem, gift. Answer 2 The answer is C. Gifts should be of an educational nature and should benefit patient care. PhRMA’s voluntary guidelines recommend that the value of gifts not exceed $100. The ACP says that docs “should not accept gifts, hospitality, services, and subsides form industry if acceptance might diminish or appear to others to diminish the objectivity of professional judgment.” Questions 3, 4, and 5 background You’ve just finished Gen Med Duke as an intern and have CAD and 9090 to look forward to. As you try to figure out how much of your well earned paycheck to invest in PfizerMerckSchering and Co, you try to remember how these companies spend their money. Questions 3, 4, and 5 Match the following numbers with the correct description: $11bn Amount of total revenue spent on Research and Development 14% Amount of total revenue that is diverted to profits 17% Amount of total revenue spent on advertising drugs Answers 3, 4, and 5 Answers • $11Bn is spent on marketing drugs each year • 14% of drug company revenue is spent on research and development • 17% is spent on profits Pre-op Assessment Quiz • Question One: – Question: A 76 year-old man with history of CAD s/p CABG (3 years ago), HTN, DM2, CVA, CRI, and newly diagnosed lung mass was sent to the cardiology clinic by the surgeon for “cardiac clearance” for resection of the mass. Patient reports that he had been doing well and in his USOH, and the mass was discovered on a recent CXR. What is the most appropriate recommendation for this pt? • • • • – A) Pt will need at least a noninvasive test prior to the surgery B) Pt may proceed with the surgery without further cardiac evaluation C) Pt will need a coronary angiogram prior to the surgery D) The surgery should be delayed until he is on optimal medical regimen Answer: B. Pt may proceed with the surgery without further cardiac evaluation. Pt had recent revascularization procedure (within 5 years – CABG 3 years ago), and has not had recurrence of symptoms. Therefore, he can proceed to noncardiac surgery without any further cardiac evaluation. Pt still need to continue medical therapy and postoperative risk stratification and risk factor modification. Quiz continued • Question Two: – Question: As the cardiology consult resident, you are seeing a 72 year-old woman with history of DM2, COPD, and on-going tobacco abuse who was admitted with a fractured pelvis after a fall at home. The patient is a resident at an ALF and fell when she tripped over some furniture. She reports that she has had some difficulty with worsening fatigue and DOE, and she can barely walk across the room because of her symptoms. What is the most appropriate recommendation for this pt awaiting an orthopedic procedure? • • • • A) Pt will need at least a noninvasive test prior to the surgery B) Pt may proceed with the surgery without further cardiac evaluation C) Pt will need a coronary angiogram prior to the surgery D) The surgery should be delayed until she is on optimal medical regimen and has stopped smoking – Answer: A. Pt should have at least a noninvasive cardiac evaluation given that she has at least one intermediate clinical predictor (DM) and poor functional capacity (METS<4). If low risk on the noninvasive test, then she may proceed to the OR; but if high risk, she may need more invasive testing such as coronary angiography. Quiz continued • Question Three: – You are asked to evaluate Mr. L, a 65 year old male with known COPD, in pre-op clinic preceding planned resection for a 2 cm right upper lobe nodule. Which of the following statements is FALSE: •A) If Mr. L’s FEV1 is 40% predicted, he should undergo quantitative V/Q scanning and possibly exercise testing prior to surgery •B) If Mr. L’s FEV1 is 50% predicted, he can proceed to surgery without further testing so long as lobectomy is not planned •C) If Mr. L’s FEV1 is 90% predicted with a normal DLCO and MVV, he can proceed to surgery including lobectomy without further testing •D) If Mr. L’s FEV1 is 2.2L, but his DLCO is only 40% predicted, he should undergo further testing prior to surgery – Answer: B – If Mr. L has an FEV1 of 50% predicted, he shouldn’t go directly to surgery – instead, he should undergo quantitative V/Q testing and possibly exercise testing prior to surgery for further risk stratification Quiz continued • Question Four: – Question: Which of the following is NOT a significant risk factor for the development of postoperative pneumonia, based on the VA study outlined above? •A) Thoracic surgery •B) Age greater than 70 •C) History of inhaler use •D) Receipt of general anesthesia – Answer: C – there is no evidence that a history of inhaler use is directly related to risk for post-op PNA, although COPD has been shown to be a risk factor in various smaller studies. Quiz continued • Question Five: – Question: Mr Green is a 69 yo healthy male scheduled to have CABG in 2 weeks. You are asked to asses his bleeding risk. How would you asses him? •A) History alone •B) History and physical exam •C) PT/PTT/platelets •D) All of the above – Answer: D. CABG is a high-risk surgery, so he will need a thorough evaluation prior to the procedure. Quiz continued • Question Six: – Question: Mr. Smith is a 68 year old male on Coumadin for a prosthetic mitral valve. He is scheduled to have an inguinal hernia repair. How would you manage his coumadin pre/post-op? •A) Stop Coumadin 3 days pre-op, no need for bridge. Restart Coumadin 3 days post-op •B) Stop Coumadin 3 days preop, bridge with heparin when INR<2.5, restart heparin ASAP post-op, and then restart Coumadin •C) Continue Coumadin through surgery •D) Stop Coumadin one day prior to surgery and do not resume until 1-2 weeks post-op – Answer: B. This patient is at high risk for ATE despite the low-risk nature of the surgery and needs a heparin bridge for his procedure. • Question Seven: – Question: Ms. Apple is a 28 year old female undergoing thyroidectomy in one week. Pre-op labs show a PTT of 68, INR of 1.1, and a normal CBC. She give no history of abnormal bruising or bleeding. Your next step is: •A) Proceed with surgery Consult hematology for further workup •C) Proceed with surgery after 4 units FFP •D) Proceed with surgery after 5 mg of Vitamin K SQ x1 •B) – Answer: B. This patient has a high-risk surgery (head and neck) and therefore needs further workup (i.e. mixing study, etc.). • Question Eight: – Question: What aspect of history, physical or laboratory studies is associated with increased risk of post-operative wound infections? •A) Baseline hemoglobin A1c •B) History of retinopathy •C) Preoperative glucose level •D) Use of insulin – Answer: Preoperative blood glucose > 200 has been associated with increased risk of deep sternal wound infections in post-CABG patients (found to have OR of 10.2). Shingles 1. Which of the following is not a risk factor for shingles? A. HIV B. Advanced age C. Malignancy D. Obesity E. Chronic illness 1. Answer: D Immune suppression and advanced age are the two major risk factors for shingles. 2. A. B. C. D. What’s the cumulative life time incidence of shingles? 0-10% 10-20% 20-30% 30-40% E. 40-50% 2. Answer: B The cumulative life time incidence of shingles in the USA is between 10-20%. 3. Which of the following is not a recognized complication of VZV infection? A.Acute retinal necrosis B.Herpes zoster ophthalmicus C.Aseptic meningitis D.Herpes zoster esophagitis E.Herpes zoster oticus 3. Answer – D. Herpes zoster esophagitis is not a recognized complication of VZV infection. All others are known complications. 4. One of your clinic patients presents with findings suggestive of possible VZV. You decide to perform a scraping of one of the lesions to send for further testing. What is the preferred test to help confirm the diagnosis? A.Tzanck smear B.DFA C.PCR D.Serologic testing E.Viral culture 4. Answer – B. DFA. PCR is the most sensitive method available, but it is still very expensive and not widely available. Both methods are now preferable to the old standard Tzanck smear. Culture is difficult and impractical. It may take up to 3 wks for results. 5. What treatment should be used for uncomplicated herpes zoster? A.Steroids alone B.IV acyclovir C.Foscarnet D.Acyclovir and steroids E.VZV Vaccine 5. Answer D. Out of the list of possible answers, an antiviral such as acyclovir and steroids would be the best for treatment of an episode of herpes zoster. Steroids should not be used alone. Foscarnet is reserved for acyclovir-resistant zoster. VZV vaccine would be good for prevention of future episodes of shingles. 6. What has been shown to be useful for pain control in herpes zoster? A.NSAIDs B.Steroid cream C.Short-acting opioids D.Tricyclic antidepressants E.C and D 6. Answer E. Opioids, either short-acting such as percocet or vicodin or long-acting such as a transdermal fentanyl patch are useful. Topical lidocaine patches have also been shown to be useful. NSAIDs or steroid creams have not been shown to be helpful with pain control. Hyperlipidemia •A 54 y.o. WM with PMH of CAD s/p MI 3 years ago presents to your office to establish a new PCP. His bp is 156/92, fasting lipid panel: LDL- 167, HDL- 34, TG- 245. (1)What is his goal LDL-c, given the above data? (2)What are his other CV risk factors? (3)What is your first step in management of his hyperlipidemia? (4)Would you treat his triglycerides? (5) By how much would you expect his lipids to change, if you decide to start a statin? (1)What is his goal LDL-c, given the above data? Goal LDL-c is 100, given his past history of CAD. (2)What are his other CV risk factors? age>45, hypertension, low HDL (<40). (3)What is your first step in management of his hyperlipidemia? Start a statin. (4)Would you treat his triglycerides? Treat his LDL first, recommend diet and exercise changes. This alone may correct his high TG;s. If they remain high, could consider niacin or a fibrate. (5) By how much would you expect his lipids to change, if you decide to start a statin? On average, statins lower TG’s by 20% and raise HDL by 5%. They lower LDL by 30-60% •A 62 y.o. AAF presents with hyperlipidemia but no other past medical history. She has never smoked, reports no FH of premature CAD, BP= 124/78. Her fasting lipid panel: LDL-c: 178, HDL: 55, TG- 180. (1)What is her goal LDL-c? (2)What is the first step in managing her lipids? (1)What is her goal LDL-c? She has 1 known additional risk factor, her age. Her goal is therefore 160. (2)What is the first step in managing her lipids? You can suggest lifestyle modifications, but if these fail, starting a statin is appropriate. •You have a 52 y.o. WM with type 2 DM, previous MI, HTN and a fasting lipid panel: LDL-c: 99, HDL: 39, TG- 280. He is a smoker. He asks you if his cholesterol is “good”. What do you tell him? (1)“Your cholesterol is fine.” (2)“Your cholesterol is almost at goal, you need to try diet and exercise.” (3)“Let’s talk about starting a new medication.”•The patient’s official LDL-c goal is <100, given his history of CAD or even given his diabetes alone. However, this patient is at extremely high risk for another CV event. The Heart Protection Study and PROVE IT suggested benefit to lowering LDL-c to levels even when already around or less than 100. Other studies are underway to determine if lowering LDL to very low levels has additional benefit. •In this particular patient, starting a statin is reasonable. Some recent publications are suggesting an LDL goal of <70 in such high-risk patients. (Grundy et al. Circulation. 2004; 110: 227-239) QUESTION # 1 True or false? The number of people smoking in the U.S. is declining overall, but Joe Camel ads have done their job and adolescents are smoking more than ever. False. The numbers of people smoking overall AND adolescent smokers are both down, with 22% for both groups in 2003, from peaks of 42% of adults in the 70’s and 36% of adolescents in 1997. QUESTION #2 True or false? People know smoking is bad for them, but the majority of American smokers have tried to quit and just haven’t been able to kick the habit. QUESTION #2 True or false? People know smoking is bad for them, but the majority of American smokers have tried to quit and just haven’t been able to kick the habit. True. 70% of American smokers have tried to quit, 46% in the past year. Only 7% are still abstinent one year out and most need 2-3 attempts to successfully quit. Smokers “in remission” need to be reminded if and when they relapse that most smokers fail several times before they succeed at quitting. QUESTION #3 True or false? Clinical practitioners are fairly attentive to providing smoking cessation counseling. 70% of smokers go to the doctor yearly and the majority of them gets some form of counseling. QUESTION #3 True or false? Clinical practitioners are fairly attentive in providing smoking cessation counseling. 70% of smokers go to the doctor yearly and the majority of them gets some form of counseling. False. Of all visits to clinicians by smokers, in only about 15% was some form of smoking counseling given and only in 3% were patients offered follow-up to specifically assist with cessation. Given that smoking cessation counseling is “dose-responsive” and quantity DOES mean quality, smoking needs to be addressed at every visit. Smoking cessation interventions are moreover both efficacious and cost-effective even when compared to other preventative measures such as BP and lipid screening. QUESTION #4 The 5 A’s refer to counseling that should be provided to pts who are ready or not ready to quit smoking? What do the A’s stand for? QUESTION #4 The 5 A’s refer to counseling that should be provided to pts who are ready or not ready to quit smoking? What do the A’s stand for? The 5 A’s are for people ready to quit. They are: Ask about smoking, Advise pts to quit with specific statements regarding benefits of quitting and risks of not, Assess their willingness to quit, Assist with doing so (meds, counseling, etc.), and Arrange close follow-up to help prevent relapse QUESTION #5 Similarly, the 5 R’s refer to counseling that should be provided to smokers not currently willing to quit. What do the R’s represent? QUESTION #5 Similarly, the 5 R’s refer to counseling that should be provided to smokers not currently willing to quit. What do the R’s represent? Relevance to the individual, Risks of continuing to smoke, Rewards of quitting, Roadblocks to quitting, and Repetition at each opportunity, reinforcing the need to quit. QUESTION #6 Bupropion is an effective agent for smoking cessation resulting in an approximate doubling of successful cessation attempts, but it’s commonest side effect is: • • • • Xerostomia Decreased libido Insomnia You grow hair where you don’t want it QUESTION #6 Bupropion is an effective agent for smoking cessation resulting in an approximate doubling of successful cessation attempts, but it’s commonest side effect is: C. Insomnia Approximately 30-40% of patients report problems with insomnia, which can be helped by taking it earlier in the day. Xerostomia is also fairly common at around 10%, and seizures are a relatively uncommon problem (0.01%) but pts with seizure or eating disorders should avoid bupropion because it can lower the seizure threshold. QUESTION #7 Transdermal nicotine patches are also associated with insomnia in some users. All EXCEPT which of the following can be done to avoid that problem? • • • Remove the patch prior to bedtime Change to a specially formulated 16h patch Add paroxetine, a 2nd line agent in smoking cessation, which can beneficially cause sedation and may fix the problem • All these answers look great. Let’s move on. QUESTION #7 Transdermal nicotine patches are also associated with insomnia in some users. All EXCEPT which of the following can be done to avoid that problem? C. Add paroxetine, a 2nd line agent in smoking cessation, which can beneficially cause sedation and may fix the problem. Despite success with the antidepressants bupropion and nortriptyline, paroxetine and SSRI’s in general have failed in numerous RCT’s to assist in smoking cessation. Paroxetine is hence not a 2nd line agent in smoking cessation. Given that only certain anti-depressants work, it seems that some mechanism beyond the anti-depressant effect is operating to help pts to quit smoking. QUESTION #8 True or false? Nicotine replacement in any form and bupropion have independently been shown to help smokers to quit. Given together, the effects are even more powerful and they should both be prescribed when possible. QUESTION #8 True or false? Nicotine replacement in any form and bupropion have independently been shown to help smokers to quit. Given together, the effects are even more powerful and they should both be prescribed when possible. False. Several studies have been performed, and the bupropion alone, nicotine alone, and combination arms of available trials show similar effects. Nicotine and bupropion are not additive prescribing both is generally not advisable given the increased potential for side effects. One agent or the other should be chosen based on individual pt characteristics (e.g. background depression, etc.). QUESTION #9 Which of the following is true? • Clonidine is as somewhat effective in helping smokers to quit but is not first line because of lesser efficacy and greater side effects as compared to bupropion, • Benzos have been demonstrated to help smokers to quit by “taking the edge off” their cravings, • Nortriptyline is as effective as bupropion but only second line because of greater side effects, • Bupropion is not effective in schizophrenics, probably because it negatively interacts with the dopaminergic neural pathways. QUESTION #9 C. Nortriptyline is as effective as bupropion but only second line because of greater side effects. The other statements are false: clonidine and nortriptyline both seem to be as effective as bupropion but remain second line because of greater side effects and less available efficacy data. Benzos (as well as beta blockers, naloxone, and others) have not been shown to be helpful in cessation. Lastly, bupropion HAS been effective specifically in trials involving schizophrenics. QUESTION #10 “Doc, I’m going to get fat and depressed. Why would I want to quit smoking?” How do you respond? QUESTION #10 “Doc, I’m going to get fat and depressed. Why would I want to quit smoking?” How do you respond? The average weight gain is about 10 lbs. and the health benefit is clearly worth the trade-off for the weight gain. Many people have mild mood lability but depression can occur and those pts with a predisposition or history may do better on nortriptyline or bupropion. In general, acknowledge that there are “hazards” to smoking cessation but that they are surmountable and worth the effort. Travel Medicine Quiz Question #1: A 26 year old female who recently relocated to the U.S. from Honduras 6 months ago presents to the emergency department with a three day history of fever, abdominal pain and vomiting. She reports that she was treated for malaria 9 months ago with chloroquine in El Salvador when she presented with similar symptoms. A thick and thin smear obtained in the ED reveal plasmodium vivax, 1% parasitemia. What is the most likely explanation for this patient’s recurrence of malaria? • • • • • She did not complete her full course of chloroquine in El Salvador She caught malaria from her cousin who is visiting her from El Salvador She had reactivation of liver hypnozoites from the first episode of malaria She was reinfected by a mosquito carrying malaria here in Durham There is no way she has malaria- the ED is wrong again. Quiz Question #2 Referring to the patient in question #1, what is the most appropriate treatment for her illness? • Chloroquine 600mg PO x1, then 300mg PO daily x3 days • Chloroquine 600mg PO x1, then 300mg PO daily x3days, followed by primaquine 15mg PO daily x14 days • Quinidine 10mg/kg IV over 1-2 hrs, then 0.02mg/kg/min IV followed by doxycycline 100mg PO/ IV Q12hrs • There is no treatment available that will cure her recurrent malaria Quiz Question #1&2: Explanation Correct answer #1: C Correct answer #2: B Explanation: P. vivax and P. ovale remain dormant in the liver in hypnozoite form. This form is not eradicated by treatment with chloroquine alone, so this patient was not adequately treated during her 1st episode 9 months ago. Correct treatment would entail chloroquine (El Salvador is not an area with chloroquineresistant malaria) followed by primaquine to eradicate liver hypnozoites to prevent another recurrence. In addition, she should be tested for G6PD deficiency prior to use of primaquine as this medication can cause hemolysis in G6PD-deficient patients. Quiz Question #3: A 30-year HIV positive male recently returned from a trip to sub-Saharan Africa. He did not take chemoprophylaxis prior to his trip. His sister notices that he has had a high fever and is developing altered mental status and rushes him to the Duke Emergency Department. Upon presentation, the patient is febrile to 39.5C. He is only oriented to person and has a generalized seizure shortly after presentation. Thick & thin smears reveal banana-shaped gametocytes within red blood cells. What plasmodium species is this patient infected with? • Plasmodium falciparum • Plasmodium vivax • Plasmodium ovale • Plasmodium malariae Question #3 Explanation Answer: A Explanation: This patient is having symptoms c/w cerebral malaria. This can occur in patients infected w/ p. falciparum. Clinical findings consist of an altered level of consciousness and seizures. Risk factors include HIV infection, pregnancy, age (old or young), prior splenectomy. Patients living in endemic areas are much less likely to get cerebral malaria even if infected w/ P. falciparum than non-immune individuals. It is universally fatal if untreated and is associated with 20% mortality with treatment. Quiz Question #4 A 20-year old female college student presents to the acute care clinic for evaluation of jaundice. She recently returned from a Spring Break trip to Cancun, Mexico. On examination she is grossly jaundiced and has appreciable hepatomegaly on exam. Laboratory data is significant for an AST of 1200, ALT 1800, total bilirubin 8.2, INR 1.1. What laboratory test would help to identify the most likely diagnosis? • Anti-hepatitis C virus antibody • Hepatitis B surface antibody • Monospot • IgM anti-hepatitis A virus antibody • IgG anti-hepatitis A virus antibody Quiz Question #5: Referring to the patient in question #4, what is the most appropriate treatment at this time? • Supportive care only • Doxycycline 100mg PO BID x7 days • Pegylated interferon alone • Pegylated interferon plus ribavirin Quiz Question #6 Referring to the patient in question #4, what is the most likely outcome from this illness? • Fulminant hepatic failure • Chronic infection with resultant cirrhosis over time • Resolution without permanent hepatic damage • It depends on the treatment used Questions #4-6 Explanations Question #4 Answer: D Question #5 Answer: A Question #6 Answer: C Explanation: This student most likely has acute hepatitis A virus infection. This is transmitted primarily by fecal-oral route and is common in areas with poor sanitation. In patients with appropriate clinical findings, the diagnosis can be confirmed by an elevated hepatitis A virus IgM antibody level. The vast majority of cases resolve with AST/ ALT levels returning to normal within 3 months (85%) and treatment is supportive. Quiz Question #7 A 30-year old male presents to your clinic for evaluation prior to a trip to Central America. He wants to avoid getting traveler’s diarrhea during his trip and is wondering if there is anything he can do to prevent this. What advice do you offer? • Only drink bottled water and you should be fine. • Salads are the safest food to eat while dining out. • Only eat food that is thoroughly cleaned and recently cooked and concentrate on drinking carbonated beverages. • There is nothing you can do to prevent traveler’s diarrhea. Quiz Question #7 Explanation Correct answer: C Explanation: Prevention is key while traveling to avoid traveler’s diarrhea. Bottled water is not always safe and can come from a contaminated source. In addition you should avoid eating fresh vegetables or salads at restaurants- only eat those that are cooked or fruits/ vegetables you can peel yourself. Carbonated beverages are a safe drink if you make sure to verify the presence of carbonation upon opening. GERD Question 4 Andy W., a 31 y.o old computer graphic designer, presents to his primary care physician for annual visit. He reports a chronic cough present for >2months but no heartburn. Chest x-ray and physical exam are unrevealing. Which of the following symptoms is NOT suggestive of Gastroesophageal Reflux Disease? • • • • • Hoarseness Dental Erosions Steatorrhea Chest pain Odynophagia Question 4 C. Steatorrhea is not classically associated with GERD. The other symptoms mentioned are atypical manifestations of the disease. Heartburn and regurgitation are the most common complaints. In patients with atypical symptoms, endoscopic findings of esophagitis are less common and ambulatory 24-hour pH monitoring and/or trial of PPI therapy may be required to confirm the diagnosis. Question 5 Of the following four patients, who is most likely to benefit from screening for Barrett’s Esophagus? • • • • 35 55 55 60 y.o y.o y.o y.o white male with GERD for 1 year asymptomatic on PPI therapy white female with GERD x 5 years asymptomatic on PPI therapy black male with reflux symptoms x 6 months not yet on PPI therapy white male with GERD x 10 years asymptomatic on PPI therapy Question 5 D. Screening for Barrett’s esophagus is controversial. There is no evidence of mortality benefit with regular screening. However, because Barrett’s is a premalignant state, identifying patients with Barrett’s may benefit that patient. Risk factors include white race, male gender and duration of GERD symptoms. Question 6 Nadia, a 30 y.o black female, has a 6 month history of heartburn that has not improved after 2 months of maximal PPI therapy and lifestyle modification. She denies any dysphagia, weight loss or anorexia. Which would be the next appropriate step in her management? • • • • • Barium Swallow Surgical Fundoplication Upper Endoscopy with biopsy Addition of H2 blocker Ambulatory 24-hour Esophageal pH monitoring Question 6 E. Ambulatory esophageal pH monitoring. In patients who do not respond to PPI therapy, pH monitoring while on therapy will help confirm the diagnosis of GERD. Combination therapy with PPI and H2 blocker has not been shown to be better at controlling symptoms than single-agent therapy, though there is evidence that addition of an H2 blocker to maximal PPI therapy may help decrease nocturnal acid secretion (Xue S et al. Aliment Pharmacol Ther. 2001 Sep;15(9):1351-6) Sinusitis 1. 43 yo woman presents with fatigue, rhinorrhea, left facial pressure, mild pharyngitis, left maxillary toothache and postnasal drip for the past 3 weeks. She has felt feverish, but has not taken her temperature. She uses an oral antihistamine for allergic rhinitis. She has no allergies to antibiotics. On PE, she has an oral temp of 37.4C. There is mucopurulent discharge from the left hostril, tenderness over the left maxillary sinus, mildly erythematous tympanic membranes, poor transillumination of the left maxillary sinus, no cervical adenopathy and clear lungs. Which one of the following therapies is most appropriate for this patient? A) B) C) D) E) Intranasal glucocorticoids Oral decongestant Antihistamine Amoxicillin-clavulanate Amoxicillin Answer: E Amoxicillin This pt has acute sinusitis, given symptoms > 1 week, unilateral or bilateral purulent rhinorrhea, local pain and maxillary toothache. Acute sinusitis is defined as having symptoms lasting up to 4 weeks, chronic sinusitis greater than 12 weeks duration. Other therapy for rhinitis includes administration of intranasal glucocorticoids and intranasal decongestants. Patients can have multiple episodes of acute sinusitis. Allergic rhinitis may predispose and should be addressed. Antihistamines should be continued for the pt’s underlying allergic rhinitis, and the first choice of treatment is antibiotics. Treatment with amoxicillin or TMP-SMX is successful in 90% of patients and should be first line therapy. If antibiotics are used, choosing the agent with narrower coverage is consistent with the need to avoid antibiotic resistance. In pts with acute sinusitis, 69% had resolution or improvement without antibiotics by 14 days. Recommendations on the duration of therapy vary, with data showing that 3 days of therapy is as effective as 10 days for acute maxillary sinusitis. This patient does not have chronic sinusitis. Therefore, therapy with amoxicillinclavulanate is not appropriate. Regarding possible imaging studies, plain films of the sinuses are not indicated; CT scan of the sinuses would be the imaging test of choice, but it is reserved for patients who have sinusitis or who have failed to respond to treatment. 2) A 27 yo man presents with 4 days of malaise, fatigue, and yellow discharge from his right nostril, along with sneezing, mild sore throat, congestion, dry cough, and myalgias. He wants relief from his symptoms because he must travel by plane in 3 days. He smokes one pack of cigarettes per day. On physical examination, his temperature is 37.4C. There is no facial tenderness, and normal transillumination of his sinuses, yellow rhinorrhea from right nostril, mild pharyngeal erythema, no cervical adenopathy and clear lungs. Which of the following would be appropriate for this patient? A) B) C) D) E) TMP-SMX, double-strength therapy Pseudoephredrine therapy Amoxicillin-clavulanate therapy Sinus radiography Azithromycin therapy Answer: B Pseudoephedrine therapy This patient does not meet the criteria for sinusitis. His symptoms have lasted less than 7 days, and he likely has a viral URI. Other than unilateral purulent discharge, he does not have specific criteria for sinusitis. Systemic adrenergic agonists may play a role, as may nasal glucocorticoids, guaifenesin, oral hydration or nasal saline spray. Patients with controlled hypertension may use short-term adrenergic agonists or decongestants. Smoking cessation should also be stressed in this patient. Antibiotics are over-prescribed for colds, URI and bronchitis. In one study, more than 50% of patients who presented with any of these three conditions was prescribed an antibiotic, even though antibiotics have little to no benefit in these conditions. Ipratropium bromide has been shown to decrease nasal discharge and sneezing, but routine use of this medication is questioned because of cost and because it does not releive many other symptoms related to the common cold. Sinus radiography is not indicated win the evaluation of uncomplicated viral URI. Nodules Question: A 42 y/o woman presents for evaluation of a 2.8-cm left adrenal mass. She was seen in the ER 1 week ago for abdominal pain. CT scan shows only the adrenal mass. Physical examination, vital signs, and review of systems are all normal. Medical history and family history are unremarkable. What is the first step in management of this patient? A) B) C) D) E) Reassure the patient and suggest follow-up CT scan in 6 months Arrange CT-guided needle biopsy of the mass Order plasma and urine hormone work-up Consult a general surgeon to have the mass removed Order ultrasonography or MRI Answer: C) The first step in management is an evaluation of serum and urine hormone levels to determine whether the mass is functional or nonfunctional. If it is nonfunctional, follow-up CT and repeat hormone testing at 6-12 months are indicated to ensure the mass is not enlarging or beginning to produce hormones. At 2.8 cm, the mass has a low malignant or functional potential, and therefore there is no immediate indication for removal of the mass, biopsy, or further imaging. (MKSAP-13) Questions: 1. A 42-year-old woman presents with a palpable mass on the left side of her neck. She has no neck pain and no symptoms of thyroid dysfunction. Physical examination reveals a solitary, mobile thyroid nodule, 2 cm by 3 cm, without lymphadenopathy. The patient has no family history of thyroid disease and no history of external irradiation. What is the best first step in evaluation? A) Check TSH B) Order a thyroid ultrasound C) Refer for thyroid surgery D) Check serum calcitonin level 2. A 37 y/o asymptomatic woman presents for a routine physical examination. Physical examination reveals a 2-cm right-sided thyroid nodule that is firm, nontender and moves with swallowing. The rest of the physical exam is unremarkable, including normal reflexes and absence of tremor. The TSH level is 1.8. She is referred for fine-needle aspiration biopsy of the thyroid nodule. Which of the following is true regarding interpreting the cytologic results of thyroid FNA biopsy? A) Follicular carcinoma can be accurately diagnosed B) Most FNA biopsy specimens reveal malignant cells C) Follicular adenoma can be accurately diagnosed D) Papillary carcinoma can be accurately diagnosed E) Cystic nodules are more likely than solid nodules to provide diagnostic material. Answers: 1. A) All patients with a thyroid nodule should have a TSH checked, followed by either an FNA if the result is normal or high, or a radionuclide scan if low. A thyroid ultrasound does not avoid the need for a FNA, so it should not be ordered without a plan for simultaneous biopsy. Tissue is preferred prior to surgery (even for high risk patients, where the pathology may guide surgical approach). A serum calcitonin level would be important to order with the TSH if the patient had a family history of medullary thyroid cancer or MEN-2. (source: Hegedus, NEJM 2004) 2. D) When adequate samples are obtained from FNA (less likely with cystic lesions), approximately 85% of nodules are benign adenomatoid, cellular, or cystic. A certain proportion can be characterized as papillary cancers. However, FNA biopsy cannot distinguish between malignant and benign follicular neoplasms because these entities are cytologically identical. Thus, in many cases, patients with papillary carcinoma or follicular neoplasm on FNA biopsy are referred for surgery (source: MKSAP-13) Questions: 1. A 62 y/o woman is evaluated because of abnormal results on chest radiograph. She smokes 1 pack of cigarettes per day, with a 50-pack-year history. She has a morning cough productive of small amounts of yellow sputum. She has hypertension, for which she takes metoprolol, and type 2 diabetes mellitus, which is managed with diet and metformin therapy. Her BMI is 30. Her BP is 145/90 mmHg. Chest radiograph shows a 1.5cm nodule in the left upper lobe; no previous radiographs are available for comparison. Which of the following should be measured before sending this patient for a PET scan to evaluate the nodule? A) Serum sodium B) Blood pressure C) Serum creatinine D) Serum glucose 2. A 38 y/o woman who has never smoked is evaluated because of a well-circumscribed nodule in the right lower lobe, which was discovered on a chest radiograph during a routine physical examination. There is no family history of cancer, the patient has never had cancer herself, and the lesion is completely calcified. A CT scan of the chest done 2 years ago showed a 0.8cm nodule in the right lower lobe. Another CT scan is ordered, and it shows the nodule is eccentrically calcified and has grown. What is the next best step in this patient’s management? A) Lobectomy B) Transthoracic needle aspiration C) PET scan D) Remove the nodule Answers: 1. D) PET scanning uses 2-fluoro-2-deoxy-D-glucose (FDG) as the positron emitter and measures the relative concentration of the agent in the nodule. Because FDG competes with glucose for uptake into the nodule, elevated serum glucose can lead to a false-negative test. It is, therefore, important that patients with diabetes mellitus have good serum glucose control before PET scanning. The cell type of the tumor is not important in the imaging, and lesions larger than 1 cm can be assessed by PET scanning. Blood pressure control, has no influence on PET imaging, and the study is not potentially nephrotoxic because it does not use radiocontrast agents. ( MKSAP-13) 2. D) This patient likely has a benign granuloma, which is growing. The characteristics of the nodule, well-circumscribed, lower lobe location make it less likely to be a malignancy. In addition, the patient’s young age, the fact that she has never had cancer, and the fact that she is a nonsmoker also make cancer unlikely. The nodule should be removed. TTNA is unhelpful because a negative aspirate would not rule out the clinical suspicion of cancer. A PET scan would be a reasonable option if the lesion were larger; PET scanning cannot discriminate well is the lesion is less than 1cm. Lobectomy is too extensive if the lesion is not malignant. Removal of the nodule allows for minimal resection; if the frozen section at the time shows cancer, then a formal lobectomy can be accomplished during the same surgery. (MKSAP-13) Hypothyroidism Question 1 • Subclinical hypothyroidism – – – – – Is associated with an elevated TSH and normal T4 Is usually asymptomatic May progress to overt hypothyroidism May not require treatment All of the above • E. All of the Above Answer: Question 1 Subclinical hypothyroidism is defined by an elevated TSH, but a T4 within the normal range. Patients may have mild or no symptoms. Some patients with subclinical hypothyroidism will progress to overt disease; estimates are from 320%. Progression is more common in patients with higher TSH levels and positive thyroid antibodies. Treatment of subclinical hypothyroidism is controversial and needs to be tailored to the individual patient. Patients with only mild elevations in TSH and no symptoms probably do not need treatment. Question 2 • 64 year old female with hypertension and hyperlipidemia presents with complaints of mild fatigue, constipation and edema. Exam is normal. TSH is 11µIU/ml (0.34-5.66). Free T4 is 0.82ng/dl (0.52-1.21). Antithyroid peroxidase antibodies are positive. Current medications are HCTZ and atorvastatin. What is your next step in her management? a. Watchful waiting b. Initiate therapy with levothyroxine c. Pituitary imaging d. Refer to an endocrinologist Answer: Question 2 • B. This patient has subclinical hypothyroidism, with an elevated TSH and normal T4. Although treatment of subclinical hypothyroidism is controversial, there is general agreement that patients with TSH > 10µIU/ml should be treated. Further arguing for treatment in this patient are her positive auto-antibodies, which also place her at increased risk for progression to overt disease. Her labs are not consistent with central hypothyroidism, which is associated with low T4 and low, normal or modestly elevated TSH, therefore, imaging of the pituitary is not indicated. In the absence of other endocrine disorders or complicating factors such as ischemic heart disease, she does not need to be referred to an endocrinologist. Question 3 • A 32 year old female presents with complaints of fatigue, headache, dry, coarse skin and amenorrhea. She has no other medical problems and takes no medications. TSH is 0.1µIU/ml (0.34-5.66). Free T4 is 0.2ng/dl (0.521.21). What is your next step in her management? – Initiate therapy with levothyroxine – Check for antithyroid antibodies – Reassure her and repeat TSH and free T4 in 6 months – Pituitary imaging Answer: Question 3 • D. The presence of low T4 and low or normal TSH, particularly when combined with other symptoms of pituitary dysfunction, is suggestive of central hypothyroidism. Anti-thyroid antibodies are helpful in primary hypothyroidism, not central. This patient will likely need to be treated with levothyroxine, but the next step should be to image her pituitary to evaluate for an adenoma, the most common cause of central hypothyroidism. Question 4 • You have just diagnosed primary hypothyroidism in your 89 year old nursing home patient with CAD, chronic stable angina, DM2, hypertension, hyperlipidemia, osteoporosis and BPH. He weighs 60kg. You initiate the following therapy and follow up: a. Levothyroxine 12.5mcg daily; repeat TSH in 6 weeks b. Levothyroxine 100mcg daily; repeat TSH in 6 weeks c. Levothyroxine 12.5mcg daily; repeat TSH in 6 months d. Levothyroxine 100mcg daily; repeat TSH in 6 months Answer: Question 4 • A. The mean Levothyroxine dose is 1.6-1.8mcg/kg/day. While younger, healthy patients may be started on the full dose immediately, the rule with older patients and those with ischemic heart disease is to start low and go slow. That would be particularly true in this patient, as therapy may worsen his angina. Monitoring of TSH should be done every 4-6 weeks after initiating therapy or changing the dose. Once stable, monitoring may be done annually or when symptoms suggest under or over-replacement. Question 5 • Which of the following lab abnormalities may be seen with hypothyroidism? – Hyperkalemia – Hyperglycemia – Hypomagnesemia – Hypercholesterolemia – Hypernatremia Answer: Question 5 • D. Hypothyroidism is present in 4-14% of patients with hypercholesterolemia. The typical pattern is elevation in total and LDL cholesterol. Treatment of hypothyroidism may reduce lipid levels, especially in patients with TSH > 10. There is no available data on whether these reductions are clinically significant. Other lab abnormalities associated with hypothyroidism are hypoglycemia, hyponatremia, hyperprolactinemia, hyperhomocysteinemia and elevated CK. Question 6 • You see a 28 year old female with autoimmune thyroiditis and subsequent hypothyroidism in clinic. She has been asymptomatic on 125mcg levothyroxine for 3 years. She is now 4 weeks pregnant. When should you check a TSH? – At least once each trimester – 6-8 weeks postpartum – 4-6 weeks after any dosage change – At 4-6 weeks gestation – All of the above Answer: Question 6 • E. Hypothyroidism in pregnancy is associated with increased complications including preeclampsia, premature delivery and increased perinatal morbidity and mortality. T4 requirement increases during pregnancy. To ensure maternal euthyroidism, TSH should be checked early (4-6 weeks), at least once each trimester, and 6-8 weeks postpartum. As with non-pregnant persons, TSH should also be checked 4-6 weeks after any change in the dose of levothyroxine. Depression Questions • Matching – – – – – Dysthymic – 2 years of low-grade symptoms Bereavement – Loss of a loved one Pathologic Grief – Excessive worthlessness or suicidality Melancholia – Particularly amenable to ECT Depression NOS – Hypersomnia and weight gain True/False – Hypercalcemia has been associated with depression. True. – A man who recently lost his wife is undergoing a standard grief reaction with frequent thoughts about his wife, frequent crying, occasional visual or auditory hallucinations, and intense guilt and worthlessness. False. => The statement is false as this patient is feeling intense guilt and worthlessness, which are signs of pathologic grief and must be considered as a major depressive disorder with PTSD symptoms. – – – Depression increases mortality at 1 year post-MI. True. 12-20 weeks of psychotherapy has been shown to be as effective as long-term maintenance pharmacotherapy in the treatment of major depressive disorder. True. Initial laboratory testing should include TSH, CBC, Folate, and ECG. - False => The statement is false as a CBC is not part of a routine laboratory examination for depression. Electrolytes are the missing component of this list and must be checked whenever depression is being evaluated. Questions • • Which of the following criteria is not exactly relevant to the diagnosis of major depression: A) 2 weeks of persistent anhedonia B) Significant loss of weight C) Intermittent crying spells for 4 days D) Active suicidal ideation E) Early morning awakenings => Answer is C, when sadness is present it needs to be most of the time for at least at least 2 weeks Which of these antidepressants is most likely to have drug interactions? – – – – – Fluvoxamine – CYP450 1A2 Fluoxetine – CYP450 2D6 Nefazodone – CYP450 3A4 Paroxetine – CYP450 2D6 Fluvoxamine – CYP450 2C9 Answer: Fluvoxamine has multiple pathways in CYP450 that are affected making it more likely that alternative metabolism will occur. This makes it most likely to have drug interactions. Questions • • Which of the following side-effects is NOT applicable with TCAs: A) Bladder obstruction B) Weight gain C) Sedation D) Increased anxiety at onset of treatment E) QTc prolongation => Answer is D, though in theory possible especially with tertiary amines, in practice much less likely probably because of the overall sedative properties of such molecules Which of the following side-effects is NOT applicable with SSRIs: A) Nausea B) Weight gain C) Delayed orgasm D) Increased anxiety at onset of treatment E) Hyperthermia => Answer is B, quite unlikely (significant weight loss is also improbable) Questions • • Elderly man on Coumadin, now depressed, which SSRI is, in theory, the least likely to interfere with his INR: A) None B) Citalopram C) Setraline D) Fluoxetine E) Paroxetine => Answer is A, the only pathway not implicated in either S-warfarin and R-warfarin metabolism is CYP450 2D6. However, all SSRIs are involved with at least another pathway. In practice, the least likely is sertraline (though monitor INR closely) while fluvoxamine is the worst choice (not recommended) Which of the following SSRIs is the least bound to protein and thus least likely to displace other medications (which matters in polymedicated elderly patients): A) Paroxetine B) Citalopram C) Setraline D) Fluoxetine => Answer is B, about 50%,, all others >95% (fluvoxamine: 77%) Questions • Middle-age obese patient with long history of insomnia, smoking and hyperlipidemia well controlled on a statin is now depressed for one month and needs to be started on an antidepressant. Which of the following choices is the best and why? Note, patient is also being worked up for suspected CAD: A) Nefazodone because he also complains of prior sexual dysfunction on fluoxetine several years ago B) Mirtazapine would better target the insomnia C) Low dose of amitriptyline is cheaper & with less side effects (50 mg ) D) Sertraline started at 50 mg daily because it is easy to prescribe E) MAOI because of its mighty power => Answer is D, though presents a theoretical risk of interaction with the statin (via CYP450 3A4) is the best choice especially in a CAD patient. Nefazodone puts Pt at risk for rhabdomyolysis, while mirtazapine might precipitate a diabetes mellitus secondary to weight gain, low doses of any TCA are likely ineffective, and MAOI should not be a first – line agent. On sertraline, Pt may however develop delayed orgasm and bupropion might be a better alternative and latter be helpful in smoking cessation Menopause 1. Your clinic patient, Ms. M, is a 45 year old woman who would like to know when to expect menopause. She has a history of hypertension and she smokes 1 pack per day. She reports that her cycles are regular. She has 3 children, all of whom are healthy. Her mother had menopause at age 52. Which of the following factors are linked to early menopause? A. Patient’s mother had menopause at age 52 B. Patient has had 3 children C. Her tobacco use D. Hypertension 2. Which of the following factors are good predictors (LR+>10) for the onset of menopause? A. Hot flashes B. Elevated FSH C. Vaginal dryness D. Depressed mood E. None of the above 3. In the Women’s Health Initiative, estrogen-progesterone therapy was found to decrease the risk of which of the following end points? A. Stroke B. Hip fractures C. Breast cancer D. Coronary artery disease E. Pulmonary embolism Answers: 1. Answer: C Smoking has been shown to correlate to early menopause. Patient’s develop menopause 1-2 years earlier than non-smokers. 2. Answer: E None of the above In a systematic review, there is not a single symptom or laboratory finding that can accurately predict the presence of menopause. The diagnosis must be made clinically with good judgment! 3. Answer: B Hip fractures Combined estrogen replacement therapy has been shown to effectively reduce the risks of osteoporosis, however it has been shown to increase one’s risk for all of the other listed end points. As a result, bisphosphonates and calcium should be used for osteoporosis risk reduction. Obesity 1. You are seeing a 38 year old man for a routine yearly physical. He has no complaints, however he notes that he has become less physically active over the past several years and feels quite “out of shape”. You are relieved that he broached this subject because you have been wanting to discuss the issue of his weight for years. You also have been wanting to broach the issue of smoking cessation with him, however he remains quite elusive on this issue. The patient is 165cm tall and weight 90kg giving him a BMI of 34. His waist circumference is 103cm. Your recommendations to him should be: a) Drink 3 less regular sodas per day and walk for 30 minutes 3 times a week working up to 45min 5 days per week. b) He cannot lose weight until he begins an exercise program, so have him start 3 times per week for 30 minutes per session of aerobic activity. Do not have him change his diet at the same time as that would be too many changes at the same time. c) Make him quit smoking first. This is his biggest risk factor and there is no way he could do cardiovascular exercise while he is still smoking. d) Initiate a balanced diet of 55%carb, 30% fat, and 15% protein and give the patient a goal of 1lb wt loss per week. Encourage the patient to start walking several times per week and increase as tolerated. e) Recommend a low carb diet such as Atkins for as long as the patient can adhere to this diet with the goal of rapid weight loss and then change to a more sustainable diet once he has reached his goal weight. 2. You are seeing a 42 year old obese male police officer for routine follow up. The patient is 6’1” and weighs 280lbs. He reports his frustration that the diet and exercise regimen you discussed at your last visit were not effective in weight loss. He initially lost 3 pounds in the first month, but has lost no weight since that time. He feels increasingly worried about his ability to perform his duties as a police officer with this degree of obesity and inquires about pharmacologic agents to assist with weight loss. You should recommend: a) Orlistat because of the beneficial lipid profile of this agent. b) That the patient wait until Accomplia comes to the market. c) Silbutrimine because it is currently on the market and you feel that this patient’s main problem with weight loss is a low metabolic rate. d) Re-address the diet (re-enforcing that the frequent donut breaks are not recommended) and exercise regimen to assure that he is actually understanding and following your advice. Only after he fails a second attempt should you begin to discuss pharmacologic therapy. 3. Which of the following is not a true statement? a) Being in the United States is a risk factor for obesity. b) The elderly, above age 75, are LESS likely to die from obesity related illness. c) Obese patients have a lower basal metabolic rate than non-obese patients. d) Lower income and lower educational levels are risk factors for obesity. THE FOLLOWING QUESTIONS HAVE NO RIGHT OR WRONG ANSWERS, BUT ARE DESIGNED TO STIMULATE DISCUSSION AT THE END OF THE PRESENTATION. 4. Which of the following reasons plays the greatest role in why you would not address the issue of weight loss with every obese patient you see in your clinic each and every visit? a. You are too busy discussing the complications of the patient’s obesity such as DM, HTN, hyperlipidemia, and OSA that you do not get the opportunity to address weight loss as well during the time scheduled for the clinic visit. b. You do not feel that your patient would be willing to take your advice. c. While you have your own ideas about suggestions you could give your patient for weight loss (ex: less fried chicken and sweet tea – you have to love the south!), you are not familiar with any well designed clinical trials that show effectiveness of any advice that you may give your patient in clinic. d. Lack of recognition that obesity is a major medial problem in the patient. (While we may all think about a patient’s obesity while we are addressing their other problems, when it comes down to our notes – are we including it in the problem list and specifically addressing it in our assessment and plan at each visit?) e. You assume that it must be obvious to the patient that obesity is creating a risk to their health, and they would bring it up to you if they felt that they needed and were willing to accept your advice. f. All of the above. g. None of the above. h. Other – explain. 5. If you have not prescribed medications for weight loss for your obese patients, what is the reason: a. Lack of ability for the patient to pay for the medication. b. Unfavorable side effect profile of these medications. c. Lack of confidence in safety data of these medications considering FenFen. d. Lack of familiarity with these medications. e. Patient’s unwillingness to take these medications. f. Fear of adding one more agent to your patient’s list of medications that already numbers 15. g. You have not had the time (or other reason above) to counsel the patient on non-pharmacologic means to lose weight, therefore the patient has not yet failed this to warrant being tried on a medication. h. All of the above i. None of the above j. Other – explain. EXPLANATIONS: 1. D. With a BMI of 34, his weight loss goal should be one pound per week or a calorie deficit of 500. However with a BMI of 35 he would need 1-2 pounds or a calorie deficit of 500-1000. Drinking 3 less regular sodas per day, assuming he is drinking this much soda will bring him to a calorie deficit of less than 500 daily. The days he walks he may have a 500 calorie deficit, but this is also assuming that he does not substitute the sodas for another source of calories. An exercise program alone will not create a 500 calorie deficit daily. Exercise is important, but it helps to insure that weight is not re-gained rather than initiate weight loss by itself. The patient does not have the desire or motivation at this time to quit smoking. Use this opportunity while the patient is interested in trying to lose weight to work on weight loss. The goal is not rapid weight loss, it is sustained 1 pound per week on a regimen that the patient will likely continue after at goal weight, therefore recommending Atkins or a diet the patient is not likely to be able to adhere to would not be a good plan. The best plan at this time is to recommend a balanced, sustainable diet with an exercise regimen that can be escalated and a goal of 1lb/week weight loss. 2. D. Most patients who fail diet and exercise for weight loss are not following the recommendations appropriately. Whether this is lack of understanding on the patient’s part or inadequate explanation by the physician, this should be readdressed to determine why it did not work and the patient should be given another attempt before initiating pharmacologic therapy. 3. C. Obese patients do not have slower metabolic rates than non-obese patients. The other statements are true. Allergy Testing Questions on Allergy Testing. 1) What in the world is a hymenoptera? a) b) c) d) A snake A spider A hysterical woman An order of insects Answer: (d) Hymenoptera is one of the larger orders of Insects, comprising the sawflies, wasps, bees, and ants. The name comes from the membranous wings (Greek hymen = a membrane), of which most forms have two pairs. 2) Inspection of the nares is an important part of the complete physical exam for a patient with suspected allergic rhinitis. If you observed bilateral nasal polyps on exam, what would your differential diagnosis be? a) Cystic fibrosis b) c) d) e) f) g) Asthma Chronic allergic rhinitis Aspirin sensitivity Chronic sinusitis Meningocoele in a child All of the above Answer: (g) Nasal polyps are yellowish, grey, pedunculated sacs which cause progressive nasal obstruction, and most are bilateral and originate from the ethmoid sinuses. Analysis of a polyp reveals a grossly edematous submucosa with a cellular infiltrate of plasma cells, lymphocytes, macrophages and eosinophils. Polyps also contain high levels of histamine. On exam, polyps are insensitive if probed and mobile; turbinates are sensitive and fixed. A unilateral polyp should be assumed to be neoplastic until proven otherwise. All unilateral polyps and suspicious-looking polyps should be biopsied and sent for histological examination. Note that neoplasia may also occur in bilateral polyps. Samster’s triad refers to the clinical syndrome of asthma, aspirin sensitivity, and nasal polyps, and occurs in up to 8% of patients with nasal polyps. QuickTime™ and a TIFF (LZ W) decompressor are needed to see t his picture. 3) When should referral of a patient with allergic rhinitis be considered? a) refractory to treatment e.g. 6 weeks with nasal steroids b) unilateral nasal symptoms c) nasal perforation, ulceration or collapse d) serosanguinous discharge e) high nasal cavity crusting f) recurrent cellulitis g) all of the above Answer: (g) All of the above warrant consideration for referral from our primary care clinic. Urgent referral, of course, is required for periorbital cellulitis. 4) The amount of IgE response detected on in vitro RAST, or radioallergosorbent testing, directly correlates to the severity of symptoms in the patient. True or false? Answer: (False) These tests are in vitro and results correspond to the concentration of specific IgE in the patient's serum. They do not reflect the amount of mast cell fixed antibody and are not a marker of the severity of reactions the patient has or will experience in the future. The result is a marker of exposure and IgE response only. RAST tests for the type 1 IgE mediated hypersensitivity reaction by incubating the patient's serum with a solid phase allergen: the amount of allergen-specific IgE is thus quantified with radiolabelled anti-IgE. 5) A patient who presents to clinic complaining of symptoms of rhinitis on exposure to cigarette smoke deserves an explanation that this is caused by a Type I IgE mediated hypersensitivty reaction which leads to release of histamine from mast cells. True or false? Answer: (False) There are many types of non-allergic rhinitis, and vasomotor rhinitis is one of them. This rhinitis does not depend on the presence of IgE and is not due to an allergic reaction. Symptoms can be triggered by cigarette smoke, other pollutants, strong odors, alcoholic beverages, temperature/humidity changes, or even changing position at night. Non-allergic rhinitis can also be caused by blockages in the nose, a deviated septum, infections, and over-use of decongestant medications. This is a chronic problem and for those who suffer from it, and not all of the above stimulants are easy to avoid. For acute relief, oral decongestants or nasal corticosteroids can be used for non-allergic rhinitis, as well. 6) RAST can be used in patients who may have: a) contact dermatitis b) food allergy c) inhalant allergens d) occupational allergens e) venom allergens f) PCN allergy g) b-f Answer: (f) Allergic contact dermatitis is a cell-mediated, type IV hypersensitivity reaction; RAST is inappropriate for testing for contact dermatitis. Using RAST, only one sample of serum can be tested for many different allergens: -- food - peanuts; tree nuts including walnut, almond, hazelnut; eggs; milk; shrimp; prawns -- inhalant allergens – pollens, dust mite, pet dander -- occupational allergens - latex -- venom - wasps, bees, etc -- drug - penicillin 7) Once it has been decided that a patient needs allergy testing, RAST can be used for: a) Allergy testing from the primary care clinic, when the patient does not have time for referral -- RAST is an easy blood test which involves taking only one sample of serum from the patient in PCP clinic. b) Patients who cannot discontinue use of beta-blockers or TCA antidepressants for the purpose of undergoing skin allergy testing. c) Skin conditions which preclude accurate reading of skin tests, such as severe eczema or dermatographia d) History or suspicion of anaphylaxis in which skin testing could be hazardous Answer: (b, c, and d) RAST is not better than skin testing, however it is much more expensive. Indications for RAST testing include: -- inability to discontinue use of medications that could interfere with the skin response, such as antihistamines, topical corticosteroids, clonidine, tricyclic antidepressants, or phenothiazines -- inability to discontinue use of medications such as beta blockers that will interfere with the need to treat adverse systemic reactions which can occur on skin testing -- cases in which anaphylaxis is suspected and skin testing may be hazardous -- cases in which skin testing will not be accurately interpreted due to skin conditions