Oversight and Competency Goals by Year of Clinical Training
advertisement

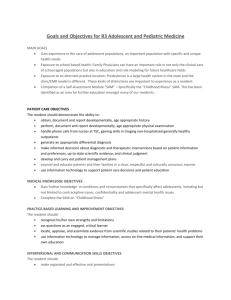
Oversight and Competency Goals by Year of Clinical Training As outlined in greater detail in the table below listing competencies by year of clinical training, residents will be given increasing levels of supervised independence as they proceed through the residency program. Specifically, they will be supervised by the attending physician, with feedback given by the attending at the half-way point and at the endpoint of every rotation and by the Associate Program Directors/Program Director at every 6-month follow-up evaluation. For residents in the first 2 clinical years, the length of rotations is 3 months. Each rotation will be devoted to one (or occasionally two) disease sites. Residents in their final clinical year may elect rotations of 1.5 months in specific disease sites or in the use of advanced technologies at the discretion of the Residency Program Directors. In the first year, residents will primarily be in the role of apprentices and will be involved in decisions surrounding all aspects of care, including patient evaluation and treatment plan development. In the second year, residents will be expected to demonstrate to the attending physician competency in several realms, including team communication, radiation treatment plan evaluation and patient work-up, without the need for attending intervention. However attending oversight will remain in place. The third year is research-based, however residents are expected to attend morning conferences, perform simulations on services without residents and take overnight call. All of these activities will be under the continued supervision of the attending physician. In the final year of training, residents will be expected to independently evaluate treatment plans and make modifications prior to finalization; to work up and develop treatment recommendations for both palliatively and definitively treated patients; and to function independently within the treatment team, including making decisions regarding psychosocial, dietary and other appropriate support-service involvement. The resident is expected to continue to develop progressive competency in disease sites covered by rotations done in the first two clinical years. This is accomplished by attendance and participation in morning case conferences, the summer didactic series and other teaching sessions and will be assessed by the annual in-service examination and by competency displayed in discussions during morning conferences. One of the strong points of HROP is the multiplicity of experts at the different sites. The variation of opinions by these experts provides an even greater attention to the evidence underlying clinical decision-making, which forms a key aspect of life-long practice-based learning and improvement. The content of the disease-specific rotations at the different sites does differ and compensation for these differences is accomplished by attendance and participation in morning case conferences, the summer didactic series and other teaching sessions and will be assessed by the annual in-service examinations and by competency displayed in discussions during morning conference. Competency Goals Patient Care Clinical Year 1 • The resident will become familiar with his/her role as health care provider to patients with cancer and their families. • The resident will learn the Clinical Year 2 • The resident will become competent in making appropriate cancer management Clinical Year 3 • The resident will show independence in making and implementing appropriate cancer Medical Knowledge components of a thorough oncologic history and PE. • The resident will become familiar with making appropriate cancer management recommendations, including writing appropriate consultation notes on patients s/he has evaluated. • The resident will learn to recognize signs and symptoms of an oncologic emergency and recommend appropriate care. • The resident will learn the fundamentals of cancer biology and of radiation physics with special emphasis on treatment planning. • The resident will become familiar with the rudiments such as staging and natural history of the common malignancies. • The resident will learn the acute toxicities of radiation treatment and their management. • The resident will learn the “tolerance” doses of the various organs to radiation treatment. • The resident will become knowledgeable regarding anticipated treatment outcomes so that these can be discussed with the patient, family and other involved physicians. • The resident will become competent in the palliative management of cancer patients including pain-medication management and delivery of palliative radiation therapy for compression syndromes, hemorrhage and other urgent distressing symptoms. • The resident will learn the fundamentals of CT-based and MRbased anatomy to define target volumes and critical normal tissues. • The resident will learn these technical skills: lymph node examination; urinary recommendations. • The resident will become competent in working with physicists in devising treatment plans. management recommendations and planning in the simulator (under appropriate supervision). • The resident will become familiar with alternative forms of cancer treatment, including surgery and systemic therapy, as well as the benefits and toxicities of combined modality treatment. • The resident will develop a solid foundation in the physics and biology of radiation therapy and the biology of cancer. • The resident will become familiar with the evaluation of diagnostic studies (pathology and radiology) related to cancer management. • The resident will learn these technical skills: how to check set-ups on the machine and problem-solve for difficult set ups; how to appreciate which cases are appropriate for IMRT versus a 3-D conformal plan or a 2-D plan. • The resident will become thoroughly familiar with the likelihood of the long-term potential toxicities of radiation related to dose and volumes. • The resident will demonstrate a strong working knowledge of all the options, as well as their risks and benefits, in the management of common malignancies, with emphasis on the use of radiation therapy. • The resident will become conversant with the major clinical studies regarding common malignancies. • The resident will have a thorough knowledge of medical physics and cancer biology, particularly as they relate to radiation therapy. • The resident will learn the specific technical skills for Practice-based Learning and Improvement Interpersonal and Communication Skills catheterization and insertion of rectal tubes and vaginal markers; AP-PA set-up using SSD and isocentric technique; calculation of radiation doses using equivalent square, phi and psy tables; wholebrain set-ups; 3- and 4-field setups; opposed oblique set-ups; interpretation of dose-volume histograms; radiation safety procedures and reviewing port films. • The resident will learn the specific technical skills for his/her rotations in the first year. • Morning case conference occurs 2-3 times a week during the nonsummer months. The resident will learn to competently present cases at these conferences, identifying both the critical issues of the case and the pertinent literature bearing on these issues. The resident will present cases over his/her 3 clinical years and this approach to cases will form a key aspect of life-long practice-based learning and improvement. • The resident will also learn how to competently present at Journal Club, Mortality and Morbidity Conference, chart rounds, diseasespecific courses, resident seminars and other opportunities for critical literature review. • The resident will become familiar with his/her role as consultant, including the preparation of concise and specific consultation notes. • The resident will become familiar with the ‘team’ aspect of radiation oncology, in which the physician works effectively with physicists, dosimetrists, nurses, therapists, other health-care providers and administrative and secretarial staff. • The resident will develop • The resident will learn the specific technical skills for his/her rotations in the second year his/her rotations in the third year • The resident will be able to critically evaluate clinical studies in regard to their design, use of statistics and the validity of their conclusions. • The resident will complete an original research project. • The resident will function effectively with the ‘team’ aspect of radiation oncology, in which the physician works effectively with physicists, dosimetrists, nurses, therapists, other health-care providers and administrative and secretarial staff. • The resident will function effectively in dealing with difficult situations common in oncology, such as the dying patient, the newly relapsed patient and the hostile patient. • The resident will function effectively with the ‘team’ aspect of radiation awareness and respect for different cultural backgrounds and ethnicities in order to provide sensitive and effective care. • The resident will learn to provide clear and concise off-service notes to facilitate patient care. Professionalism Systems-based Practice • The resident will have the conviction to be a Radiation Oncologist. • The resident will record duty hours in a timely fashion. • The resident must consistently protect patient confidentiality. • The resident will enter notes into the electronic medical record within 24 hours of seeing a patient and promptly sign off on these notes. • The resident will treat patients/families with utmost respect and maintain patient confidentiality at all times. • The resident will maintain collegial relations with all staff and providers across disciplines. • The resident will demonstrate a commitment to providing patients with the best possible care through continuous learning and self improvement. • The resident will be open to receiving feedback and willing to provide it when appropriate. • The resident will become familiar with multidisciplinary cancer care, including effectively communicating with medical and surgical oncologists to develop a unified and complete treatment plan. • The resident will learn to use the • The resident will be able to acknowledge areas that require further work and set up a plan to address them. The resident will be able to discern when consultation with social work or psychiatry services, dieticians or other services are needed. oncology, in which the physician works successfully with physicists, dosimetrists, nurses, therapists, other health-care providers and administrative and secretarial staff. The resident will effectively communicate with referring physicians. • The resident will develop clear and thoughtfully considered career goals. • The resident will develop a deep understanding of the ethics of curative therapy and end-oflife care. The resident will be able to follow through on recommendations from support services listed in the column for year 2 and make electronic medical record to obtain medical information. • The resident will become proficient in the use of electronic radiation oncology prescription writing and documentation for compliance. appropriate recommendations with the oncology team. • The resident will become familiar with the use of databases for research projects. • The resident will develop an understanding of the economics of practice, and in particular, with the appropriate use of cutting-edge technology and fractionation.