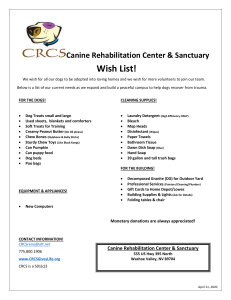
Supplementary Methods Eligibility. Dogs with spontaneously
advertisement

Supplementary Methods Eligibility. Dogs with spontaneously occurring osteosarcoma presenting for treatment to a participating center (the Animal Cancer Center at Colorado State University or the University of Minnesota Veterinary Medical Center) were screened for eligibility and owner consent. Eligibility required a diagnosis of stage-I or stage-II primary appendicular osteosarcoma, substage-a or substage-b. Stage-I disease is restricted to the endosteum with no detectable metastases based on physical exam and radiographic findings, and stage-II disease is present outside the periosteum with no detectable metastases based on physical exam and radiographic findings. Substage-a tumors have low-grade histologic appearance and substage-b tumors have high-grade histologic appearance. Additional eligibility criteria included age between 2 - 12 years; either sex (neutered or sexually intact); any breed (including mixed-breeds); body weight >20 kg; adequate performance and constitutional health status to tolerate biopsy, gene therapy, and 10-day delay for standard-of-care, no known distant metastatic disease, and no other pre-existing acute or chronic disease that would knowingly preclude a one-year lifespan. Diagnostic tests to screen for eligibility included medical history, physical exam, complete blood count (CBC), serum biochemical profile, urinalysis, chest radiographs for metastasis evaluation, and in some cases, whole body nuclear bone scan. Among the laboratory and clinical indices required for eligibility were transaminases not exceeding 3X normal, total bilirubin not exceeding 1.5X normal, creatinine not exceeding 2X normal, at least 2,500 neutrophils/µl, 75,000 platelets/µl, and a hematocrit of 28%. Owners were offered participation in the trial as one treatment option available for their dogs. Owners who chose to enroll their dogs in the study were given additional educational materials describing the procedure and possible outcomes, and they were required to provide informed consent. They also agreed to follow-up with study investigators through first recurrence of disease. Comparison population (contemporary controls). The study had a single arm. To assess efficacy against a contemporary control population treated with the standard of care, we analyzed the outcome for every dog that was diagnosed with appendicular osteosarcoma at the Animal Cancer Center (Colorado State University) and that received the same therapy (limb amputation with adjuvant carboplatin chemotherapy) during the study enrollment period. Sixty-two dogs were identified that met these criteria. The demographics of this contemporary comparison cohort (“standard of care”) are shown alongside the study cohort in Table S1. Derivation and validation of cultured osteosarcoma cells. Ex vivo osteosarcoma cell cultures were derived as described 30, 36. Briefly, two Jamshidi needle biopsy samples obtained at staging from each dog were placed in 10 ml of DMEM media supplemented with 10% FBS for transport to the laboratory. The samples were maintained at 4C until processing. A large enough portion that was grossly representative of the biopsy was prioritized for histopathologic analysis and transferred to 5 ml of neutral buffered formalin for paraffin embedding. The remaining material (usually ~2 mm in length x 4 mm diameter) was rinsed in sterile phosphate buffered saline solution and disaggregated into single cell suspensions. Debris was removed by passing sequentially through 500and 200-µm mesh filters; cells were then placed in a 4-cm2 culture dish at a density of 1 x 106/ml in DMEM/FBS and cultured at 37C in a 5% CO2 atmosphere. Cells were allowed to reach ~80% confluence, at which time they were passed to a 10-cm2 culture dish, and then again to a 25-cm2 culture flask. Our success rate for expansion beyond one passage using this method is approximately 50%. By the second passage, the cultures were homogeneous and consisted of large polygonal to plump spindloyd or slightly rounded cells. Cells in logarithmic growth from the third passage were detached, washed, and suspended in 90%FBS/10% DMSO for cryopreservation in liquid nitrogen. We have shown previously that this method yields cells of osteoblastic origin based on retained alkaline phosphatase activity and osteocalcin expression by the third passage, and we have documented stability in culture for 30 passages with no noticeable changes in morphology or loss of alkaline phosphatase expression. Cell lines that we have derived in this manner are tumorigenic in vivo, and when injected orthotopically into nude mice, they metastasize spontaneously to the lungs 40. Genome wide gene expression signatures of cultures derived in this manner also are consistent with osteogenic origin and describe predicted biological behaviors of the tumors 30. We recovered viable cells for RNA analysis from 15 dogs in the study, and could not detect any apparent bias in these samples (Table S5). We confirmed that the cells conformed to expected expression patterns of the 10 genes identified in the RNA isolation section of the methods, selected from a conserved prognostic signature 30, in 10 of the samples from this study, and subsequently evaluated expression of Fas and GAPDH mRNA in all 15. Manufacturing of Ad-FasL. The viral clone used for these studies has been described previously 13, 17. For this large-scale preparation of Ad-FasL, HEK 293-crmA cells (stably transformed with the cowpox virus crmA gene) were grown in 200 10-cm dishes and infected with Ad-FasL. When the cytopathic effect was nearly complete (36-48 hr after infection), non-adherent and weakly adherent cells were collected, medium was neutralized to a pH between 7.5 and 8 by addition of 1 M HEPES/0.9 M NaOH, cells were centrifuged at low speed, and placed through three rounds of freezing and thawing. Infectious virus was purified from supernatants cleared of cell debris using routine CsCl banding methods and concentrated in stabilization buffer containing 50% v/v glycerol. Ad-FasL was vialed under sterile conditions in a GMP-compliant facility and stored at 80°C. Release assays. Vials were selected randomly from the lot for aerobic culture and activity assays. Activity of Ad-FasL was standardized in a bioassay measuring apoptosis of Fassensitive OSCA-32.3 canine osteosarcoma cells 29 under limiting dilution conditions (MOI<0.001). Stability was tested in material stored at -80C, -20C, 4°C, room temperature or 37°C. Reduced Ad-FasL activity was only seen in samples stored at >4°C for over 6 months, or at 37°C for 3 days. Experimental treatment protocol. Immediately prior to injection of Ad-FasL, core biopsies were obtained for histopathologic confirmation and to establish primary tumor cultures. Biopsy and injection procedures were done using fluoroscopic radiographic guidance (Fig. S3). A 4-inch, 8-gauge or 11-gauge Jamshidi needle was used to obtain tumor biopsies using routine procedures. Briefly, dogs were anesthetized, prepared and draped for surgery; the needle was advanced through the tumor taking care not to penetrate the opposite cortex. The first sample was taken in the proximal portion of the tumor and a second biopsy was done parallel to the first in the distal portion of the tumor with a minimum of 0.5 cm separating both sites. Images were recorded to aid in histopathologic orientation after tumor removal, and 0.3 ml of sterile New Methylene Blue was injected into the proximal biopsy tract using an 18-gauge needle for subsequent tracking. Ad-FasL (0.3 ml) was injected in the distal biopsy tract using the same technique. Dogs had a light bandage placed over the site and were monitored post operatively for pain or other adverse events. All dogs received a non-steroidal anti-inflammatory (Deracoxib) and tramadol on an as needed basis for pain control. Except for the first 5 dogs treated, which remained hospitalized for 48 hr to evaluate viral shedding, all dogs were treated on an outpatient basis and returned home to their owners the same day. Environmental monitoring. Ad-FasL is built on the a replication-defective Ad5 platform. The unlikely possibility that there was viral shedding into the environment was monitored in the first five dogs enrolled. Because adenoviruses target the small intestine, where persistent infections lasting from days to weeks occur following infection and virus growth at the primary site of infection, rectal swabs were collected. For adenovirus type 5 (the serotype used to construct the Fas ligand-encoding vector), the initial site of infection in humans is in the pharyngeal epithelium. Therefore, buccal swabs were collected. Swabs were obtained from each dog prior to administration of Ad-FasL, and 4, 24, and 48 hours after treatment. Swabs were stored at 0°C in mammalian cell culture medium supplemented with antibiotics until testing. HEK293-crmA plates, which are resistant to Fas ligand because of inhibition of caspase activity by crmA were plated at approximately 40% confluence in medium containing anti-bacterial and anti-fungal antibiotics in 24-well plates. The day after plating of the cells, total medium (approximately 200-250 µl) was taken from 15 ml tubes containing the buccal and rectal swabs from the five treated dogs and added to the cells. The cells were then incubated at 37°C in the presence of 5% CO2 for 9 days. The wells were examined each day for the appearance of cytopathic effect resulting from virus growth. HEK293-crmA cells infected with Ad-crmA (e.g., for a plaque assay) produce clearly apparent cytopathic effect within 4-5 days. Dose finding rationale. The initial rate of systemic adverse events for the treatment considered acceptable was set at 30% 25. The lowest dose for the study was set at an equivalent of 1/50th of the mouse LD10, expressed as viral particles (pfu) per unit of mass or area. Data from our laboratories place the mouse LD10 Ad-FasL at >1 x 108 pfu per mouse (RCD, DB, JS, unpublished), but only when FasL is given intravenously. This dose would be approximately 5 x 109 pfu/kg; therefore 1/50th of the mouse LD10 (intravenous) would be equivalent to 1 x 108 pfu/kg. The accepted conversion factor published by the NIH Developmental Therapeutics Program (body surface area) from mouse to dog is 1/6th, from which, we determined a lowest dose (i.e.. “Dose 1”) of 1.6 x 107 pfu/m2 to build the schedule for escalation (Table S2). A number of considerations particularly noteworthy: in mice, administration of AdFasL using doses >100-times the intravenous LD50 are completely safe when administered using any route other than the intravenous or intraperitoneal. When administered through the intravenous or intraperitoneal routes, death is due to liver failure precipitated by Fas-mediated apoptosis 3, 4. Although intratumoral administration in osteosarcoma had the potential to reach the bone marrow, we anticipated that reduced blood flow and increased interstitial pressure at the tumor site 32 would retain the AdFasL at or near the site of administration and largely avoid systemic distribution. We also predicted that the virus would interact with cells immediately at the site of injection, reducing the chance that significant titers would even have access to the blood. Dose escalations used geometric increases (doubling the dose) to a maximum of 2.0 x 109 pfu/m2. A previous study that administered a replication-deficient adenovirus into the prostate gland of normal dogs at this dose showed no local (urinary system) or systemic toxicity associated with the adenovirus 31. We used a dose escalation method with clearly defined rules to establish a reasonable dose range as a means to provide measures of safety (primary endpoint) and estimates of efficacy (secondary endpoints) to go on to the next phase. We designed the dose finding using a standard testing approach with 3 dogs per dose. Assuming 6 potential doses, we used the following escalation rule: We started at the 4th dose. If there was no toxicity in the first three cases, escalation occurred to the next dose with the next 3 dogs. If one of the three dogs experienced a toxic event, that cohort would be expanded with the next 3 dogs and continued until a decision was made (up or down). If two or more dogs experienced a toxic event, dose was to be de-escalated to the next lower dose for the next 3 dogs. Three consecutive de-escalations or one immediate fatality would lead to stopping the study. Toxicity Monitoring. Toxicity or severe adverse events were evaluated using a scale from grade 1 to grade 5 for constitutional symptoms, respiratory events, cardiac events, hematological (blood, bone marrow, hemostatic, vascular) events, gastrointestinal and other metabolic events as established in the Veterinary Cooperative Oncology Group (VCOG) Common Criteria for Adverse Events 26. Unacceptable severe adverse events were considered those that were life threatening (grades-4 or-5) or that significantly impact quality of life (grade-3 toxicity in >2 categories). Grade 1-2 events, or grade 3 in <2 categories that were not life-threatening or did not significantly impact quality of life were considered acceptable. Toxicity was evaluated on days 3, 7, and 10 as described in Table S3. Quality of life. Quality of life was assessed by the owners based on surveys completed on days 1, 3, 7, and 10. Owners were asked nine questions concerning appetite, activity, and general health. They were asked to answer each question based on change from their previous visit, with answers including five categories (greatly decreased, decreased, no change, increased, and greatly increased). No change was scored as 0; greatly decreased was scored as -2; greatly increased scored as +2. A cumulative positive score indicated an increase in quality of life and a cumulative negative score indicated a decrease in quality of life parameters assessed. Histopathologic evaluation. The entire tumor specimen from each amputated limb was available for analysis. Samples were placed in formalin for 24 hr, at which time they were transferred to a formic acid-based bone decalcifier (1414A, Decal Chemical Corp, Tallman, NY) and processed using routine protocols. One ACVP-boarded pathologist (EJE) evaluated and scored all criteria. A hematoxylin and eosin-stained section of each sample was evaluated to confirm the diagnosis. Tumor sections from the pre-treatment biopsies and from the tumors isolated after limb amputation were scored for overall cellularity, tumor osteoid, general inflammation, lymphocyte numbers, neutrophil infiltration, tumor necrosis, and tumorassociated fibrosis. Each section was assigned a subjective score of 0-3 for each category, where 0 = none seen and where 1 to 3 were graded from minimal (1) to moderate (2) to abundant (3) using pathological criteria applicable to the tissue in question. Two pre- treatment biopsy samples and nine samples from dogs that underwent routine amputation without Ad-FasL treatment were used to establish basal values in untreated dogs. Immunohistochemistry. Immunohistochemistry (IHC) was done using standard protocols. Briefly, 4-µm sections were cut from formalin fixed-paraffin embedded samples and mounted on positively charged slides. The sections were deparaffinized and then rehydrated with descending alcohol concentrations to buffer. Heat-induced epitope retrieval with citrate buffer, pH 6.0 (CD3, Pax5, Fas) or EDTA buffer, pH 8.0 (Caspase-3 active) for 30 minutes was followed by endogenous peroxidase blocking with 3% hydrogen peroxide and incubation with the primary antibody at room temperature for 10 hours. Primary antibodies with known cross-reactivity to the corresponding homologous canine antigen were used, and included polyclonal rabbit anti-human CD3 (A0452, Dako, Carpinteria, CA), monoclonal mouse anti- human Pax5 (610862, BD Bioscience Pharmingen, San Jose, CA) and polyclonal rabbit anti-human Caspase-3 active (AF835, R&D Systems, Minneapolis, MN). An anti-Fas antibody that performed robustly to stain the canine protein was not available. We thus selected from a panel of antibodies that were known to perform well both in immunoblotting and IHC assays in the primary target species against which they were developed (human/mouse) for further evaluation. We tested two antibodies against cell lines from the target species that expressed Fas antigen (e.g., Jurkat and Kit-225 human T cell leukemias) as well as against canine cell lines that we had documented as having detectable Fas mRNA expression (e.g., TLM-1 melanoma, 25). Monoclonal rabbit anti-Fas antibody C18C12 (4233 Cell Signaling Technology; Danvers MA) recognized major bands of the same molecular weight (44 kDa) in the human and canine samples. We then assessed its reactivity in formalin-fixed and paraffin embedded canine lymph nodes, where we noticed staining in paracortical T cells, germinal center B cells, and granulocytes, where it had the strongest intensity. This antibody was then used to stain pre-treatment biopsies from dogs in this study at a 1:100 dilution and using heat-induced epitope retrieval with citrate buffer. A pre-diluted, dual link polymer HRP secondary antibody (K4061, Dako, Carpinteria, CA) and DAB kit (K3467, Dako, Carpinteria, CA) was utilized to detect the immunoreactive complexes. The slides were counterstained with Mayer's hematoxylin. Image analysis. For each sample, images were taken using an Axioplan 2 imaging scope coupled with an AxioCam HRc camera (Carl Zeiss, Thornwood, NY). The “hotspot” analysis method was used for quantification. This analysis was selected because parts of each tumor section contained acellular areas that would interfere with overlapping field methods. The hot spots analyzed represented most or virtually all the cellular areas detectable in the sections. Images were taken at the “hotspots” after a complete scan of each section. Image analysis was performed using AxioVision 4.3 software (Carl Zeiss). For each image, the total area of DAB-stained nuclei and the total area of all nuclei were determined. These values were used to determine the percent stained cells for each image. Measured values from images from five independent areas were combined to give means ± S.D. for each tissue section. One of the eight samples stained for Fas expression was done in duplicate as an additional step for quality control, and the staining in the duplicate samples was indistinguishable. To score Fas staining, we used a conventional semiquantitative scale ranging from 0 to 4+ where 0 was no different from background, 1 - 3 had increasing levels of membrane and cytoplasmic staining, and 4+ was equivalent to that seen in neutrophils, which were present in every tissue section (Fig. S2). Reference 1. Wolfe TD, Pillai SP, Hildreth BE, 3rd, Lanigan LG, Martin CK, Werbeck JL et al. Effect of zoledronic acid and amputation on bone invasion and lung metastasis of canine osteosarcoma in nude mice. Clin Exp Metastasis 2011; 28(4): 377-89.