Antenatal Assessment/Changes at birth
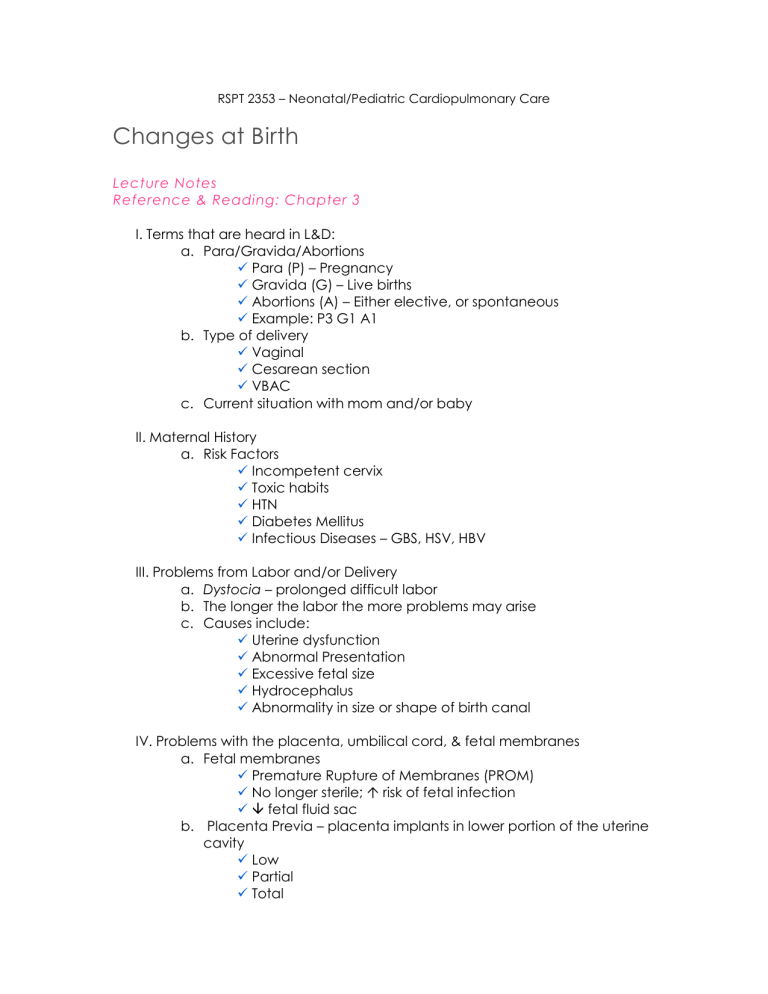
RSPT 2353 – Neonatal/Pediatric Cardiopulmonary Care
Changes at Birth
Lecture Notes
Reference & Reading: Chapter 3
I.
Terms that are heard in L&D: a.
Para/Gravida/Abortions
Para (P) – Pregnancy
Gravida (G) – Live births
Abortions (A) – Either elective, or spontaneous
Example: P3 G1 A1 b.
Type of delivery
Vaginal
Cesarean section
VBAC c.
Current situation with mom and/or baby
II.
Maternal History a.
Risk Factors
Incompetent cervix
Toxic habits
HTN
Diabetes Mellitus
Infectious Diseases – GBS, HSV, HBV
III.
Problems from Labor and/or Delivery a.
Dystocia – prolonged difficult labor b.
The longer the labor the more problems may arise c.
Causes include:
Uterine dysfunction
Abnormal Presentation
Excessive fetal size
Hydrocephalus
Abnormality in size or shape of birth canal
IV.
Problems with the placenta, umbilical cord, & fetal membranes a.
Fetal membranes
Premature Rupture of Membranes (PROM)
No longer sterile; risk of fetal infection
fetal fluid sac b.
Placenta Previa – placenta implants in lower portion of the uterine cavity
Low
Partial
Total
c.
Abruptio Placentae –
A normally attached placenta separates prematurely from uterine wall
Most common cause is Preeclampsia or eclampsia (PIH)
Many risks involve for both mother, fetus & at delivery d.
Umbilical Cord Problems
Prolapsed cord – the umbilical cord presents in the cervix into the birth canal before the baby
Nuchal cord – the umbilical cord wraps around the baby’s neck
( http://www.merckmedicus.com/pp/us/hcp/framemm.jsp?
pg=www.merck.com/mmhe/sec22/ch261/ch261c.html
)
Cord knot – also called a true knot; a knot is made in the umbilical cord
( http://www.mercksource.com/pp/us/cns/cns_hl_dorlands.js
pzQzpgzEzzSzppdocszSzuszSzcommonzSzdorlandszSzdorland zSzdmd_k_04zPzhtm#12472003
V.
Problems with Amniotic fluid (AFI) a.
Fluid within Amnion b.
Dynamic – constantly being replenished & absorbed c.
After 24-26 weeks gestation fluid is swallowed and replenished with fetal urine d.
P OLYHYDRAMNIOS – too much amniotic fluid present
CNS malformations
Orogastric malformations
Down syndrome
CHD
IDM e.
O LIGOHYDRAMNIOS – scant or decreased amount of fluid
Defect in urinary system – usually renal dysplasia or urethral stenosis
Potter’s syndrome
Implications include: lung Hypoplasia, asphyxia, and significant skeletal deformities
Presentation later in gestation – umbilical cord compression
VI.
Mode of Delivery a.
Vaginal most common b.
Forceps/ vaccum extraction c.
C-section – there are several risks involved:
Accidental cutting
TTN
VII.
Multiple Gestation – more than one fetus present
a.
Higher incidence of premature labor b.
Fraternal twins – separate placentas c.
Identical twins – shared placenta
VIII.
Antenatal Assessment a.
Ultrasound b.
Amniocentsis – Performed to run for a variety of tests
Routinely done on mothers over 35
Not common practice because of risks involved
Tests that can be performed:
1.
L/S ratio – a.
Determines lung maturity b.
compares amount of lecithin to sphingomyelin in amniotic fluid c.
lungs considered mature when L/S ration reaches 2:1
2.
Shake test – a.
Amniotic fluid mixed with ethanol b.
15 minutes later if there is a ring of bubble present, there is enough protein – lungs are mature
3.
Alpha-fetoprotein a.
Alpa-fetoprotein peaks in 12 th week and then decreases b.
If there is a break in fetal skin AFP will be present c.
High level usually indicates neural defect d.
Low level indicates Down Syndrome c.
Nonstress Test and Contraction stress test
FHR is monitored with fetal movement (NST) or with induced contractions (CST)
Reactive NST - FHR with movement or contraction
CST
1.
Negative – no late decals
2.
Positive – late decals w/ each contraction
3.
Suspicious – some late decals w/ some contractions d.
Biophysical Profile (Table 3-1)
Determines fetal risk
Tests: fetal breathing, fetal movement, fetal limb tone, NST, amniotic fluid volume e.
Fetal Heart Rate Monitoring
Important reading along with variability
Good indicator of what is going on with fetus during labor
Three ways to monitor:
1.
External abdominal transducer
2.
Electrodes on abdomen
3.
Spiral electrode
Uterine contractions are monitored with a tocodynamometer
Fetal Heart Patterns
1.
Baseline
2.
Variability – changes with CNS depression, fetal sleep, narcotic or sedative use, etc.
3.
Bradycardia - <100bpm or a maintained 20 bpm drop from baseline
4.
Tachycardia – consistenly above 180 bpm; usually maternal fever
5.
Accelerations – FHR exceeds 160 bpm for <2 minutes; good sign
6.
Decelerations – FHR drops below 120 bpm for <2 minutes a.
Early (Type I) drops during contraction – benign b.
Late (Type II) don’t follow contractions – uretoplacental insufficiency during contractions c.
Variable (Type III) independent of contractions
– secondary to umbilical cord compression
IX.
High risk conditions a.
Premature labor – Prevention is better!
Tocolysis – process of stopping labor
1.
Pharmacological – β -sympathomimetic (terbutaline & ritodine); anti-convulsant (magnesium sulfate)
Identification of risks for premature labor
Bedrest-
1.
Light-duty
2.
Bedrest (home or hospital)
3.
Trendelenburg b.
Postterm Pregnancy
Increased risk for:
1.
Large size
2.
Meconium aspiration
3.
Obstetrical trauma
Labor often induced
X.
Adaptation to Extrauterine Life a.
The first breath – Three things that influence the initiation of the first breath
Chemoreceptors detect changes in PaO2 & PaCO2 stimulate the baby to breathe
Thoracic recoil and baby leaves vaginal canal
Abrupt change in environment b.
Change from fetal to adult circulation
Changes in circulatory Pressures
1.
Umbilical cord is clamped, forcing blood to lower extremities, raising arterial blood pressure
2.
Initial breathing causes ↓ pulmonary vascular resistance (FRC & ↑PaO2)
Closure of fetal shunts
1.
With ↑ pressures in L heart foramen ovale closes
2.
Ductus arteriosus closes with the absence of prostaglandins (smooth muscle constricts)
3.
Umbilical arteries & veins constrict & become ligaments
4.
Ductus venosus also constricts & becomes ligament