PMS - aaronsworld.com
advertisement
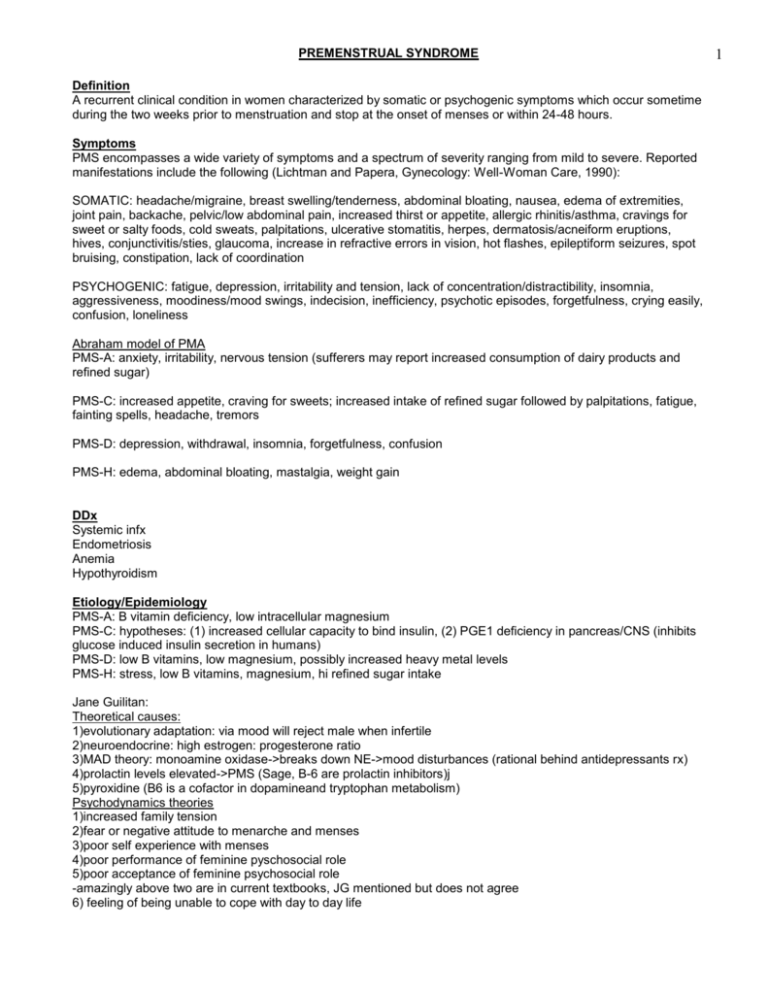
PREMENSTRUAL SYNDROME Definition A recurrent clinical condition in women characterized by somatic or psychogenic symptoms which occur sometime during the two weeks prior to menstruation and stop at the onset of menses or within 24-48 hours. Symptoms PMS encompasses a wide variety of symptoms and a spectrum of severity ranging from mild to severe. Reported manifestations include the following (Lichtman and Papera, Gynecology: Well-Woman Care, 1990): SOMATIC: headache/migraine, breast swelling/tenderness, abdominal bloating, nausea, edema of extremities, joint pain, backache, pelvic/low abdominal pain, increased thirst or appetite, allergic rhinitis/asthma, cravings for sweet or salty foods, cold sweats, palpitations, ulcerative stomatitis, herpes, dermatosis/acneiform eruptions, hives, conjunctivitis/sties, glaucoma, increase in refractive errors in vision, hot flashes, epileptiform seizures, spot bruising, constipation, lack of coordination PSYCHOGENIC: fatigue, depression, irritability and tension, lack of concentration/distractibility, insomnia, aggressiveness, moodiness/mood swings, indecision, inefficiency, psychotic episodes, forgetfulness, crying easily, confusion, loneliness Abraham model of PMA PMS-A: anxiety, irritability, nervous tension (sufferers may report increased consumption of dairy products and refined sugar) PMS-C: increased appetite, craving for sweets; increased intake of refined sugar followed by palpitations, fatigue, fainting spells, headache, tremors PMS-D: depression, withdrawal, insomnia, forgetfulness, confusion PMS-H: edema, abdominal bloating, mastalgia, weight gain DDx Systemic infx Endometriosis Anemia Hypothyroidism Etiology/Epidemiology PMS-A: B vitamin deficiency, low intracellular magnesium PMS-C: hypotheses: (1) increased cellular capacity to bind insulin, (2) PGE1 deficiency in pancreas/CNS (inhibits glucose induced insulin secretion in humans) PMS-D: low B vitamins, low magnesium, possibly increased heavy metal levels PMS-H: stress, low B vitamins, magnesium, hi refined sugar intake Jane Guilitan: Theoretical causes: 1)evolutionary adaptation: via mood will reject male when infertile 2)neuroendocrine: high estrogen: progesterone ratio 3)MAD theory: monoamine oxidase->breaks down NE->mood disturbances (rational behind antidepressants rx) 4)prolactin levels elevated->PMS (Sage, B-6 are prolactin inhibitors)j 5)pyroxidine (B6 is a cofactor in dopamineand tryptophan metabolism) Psychodynamics theories 1)increased family tension 2)fear or negative attitude to menarche and menses 3)poor self experience with menses 4)poor performance of feminine pyschosocial role 5)poor acceptance of feminine psychosocial role -amazingly above two are in current textbooks, JG mentioned but does not agree 6) feeling of being unable to cope with day to day life 1 PREMENSTRUAL SYNDROME Etiology/Epidiemology (cont) Affects 40-90 % of menstruating females and 5-10 % are severely affected (DB) Most common in the 30-40 year age range (DB) Abraham found the following characteristic of the diet of PMS patients: (DB) 62% higher in refined CHO 275% higher in refined sugar 79% higher in dairy products 78% higher in sodium 53% lower in iron 77% lower in magnesium 52% lower in zinc Pathophysiology PMS-A: high serum estrogen (decreased hepatic clearance), low serum progesterone PMS-C: increased carbohydrate tolerance, low red cell magnesium PMS-D: low serum estrogen, high progesterone, elevated adrenal androgens PMS-H: high sodium and water retention, high serum aldosterone, decreased dopamine at renal level Key PE Weight Blood pressure Heart and lung assessment Breast and pelvic exam Key Lab Pap smear w/ maturation index (from upper lateral 1/3 vagina) -could measure estrogen levels just b/f her period; estrogen levels should be low; positive test if estrogen high (JG) CBC: to r/o systemic infx and anemia Thyroid studies W/U, Strategy 1. Evaluate liver and bowel function. 2. Diet diary. 3. PE to r/o other disease. 4. Key labs + maturation index if needed. 5. Determine level of impairment, assess risk of suicide/homicide. 6. Once sx resolved, maintain with multiple and good diet (JG) 7. It takes a couple cycles to notice improvement; some take up to 6-8 months; 1 month for every year you had the condition (JG) 8. if alcohol increases symptoms: think B6 def. and malnutrition (JG) 2 PREMENSTRUAL SYNDROME TX PROTOCOLS Nutrient Considerations 1. Lipotropic factors (normalize estrogen metabolism) 2. Folate 3. Vit B6: -200 mg qd days 1-14; 400 mg qd days 15-menses (decreases edema, works w/ Mg) -100-200 mg QID (DB) -using pyridoxine with magnesium and/or in the context of a multiple vitamin-mineral supplement is far more successful (DB) 4. Magnesium: - 500 mg qd days 1-14; 1000 mg qd days 15-menses (divided doses; watch laxative effect) -400 to 600 mg/day (DB) -Check Mg deficiency (AJCN 34:2364 6 1981 Nov) 5. B complex (estrogen breakdown, proper liver function) 6. Vit C 7. Vit E: -400-1200 IU (decreases breast tenderness/congestion) (JG) -keep on dose until sx gone or down to a minimal level (JG) 8. Zinc, Calcium 9. PABA 10. Choline 1 gram 11. Inositol 500 mg 12. Dessicated liver 13. Cu, Se, Cr, Fe 14. Tyrosine 500 mg bid-qid (type D) 15. Lugol's Solution weekly (Bruce Dickson) 16. Vitamin A - 100,000 - 300,000 I.U./day for second half of cycle (DB) Dietary Considerations 1.Anti-Estrogenic diet 2. Phytoestrogens ---> dietary (e.g. soy) (DB) 3. Avoid raw goitrogens 4. Avoid oranges (increases 5-beta reductase) (BM) 5. Diet: 70% CHO, 15% protein, 15% fat 6. EFAs: Flax oil, EPO, Sunflower, or cod liver oil: 3 T/day -delta-6-desaturase activity is impaired in pts with PMS (DB) 7. Small frequent meals 8. Decrease sugar (depletes B vitamins & magnesium) 9. Brewer's yeast 1-2 T qd 10. Kelp (iodine for thyroid fxn) 11. Bran 12. Decrease refined/processed food, EtOH 13. Eliminate methylxanthines (coffee, tea, cola, chocolate) 14. Decrease or eliminate red meat/dairy (contain hormones, pro-inflammatory) 15. Decrease salt (assoc w/ increased magnesium excretion) - to at least 3 grams/day three days before menses (DB) 16. Reduce dairy products - dairy products impair the absorption of magnesium(Ca:Mg ratio higher in PMS-A pts) (DB) Botanicals 1. Phytoestrogens: Angelica, Medicago, Leonurus, Glycyrrhiza, Soy, Cimicifuga (JG) 2. Hypericum (type D)- avoid tyramine containing foods (JG) 3. Progesterone cream (JG) 4. Smilax, Dioscorea, Hydrastis, Collinsonia, Equisetum 5. Vitex agnus-castus, Angelica sinensis (DB) 6. phytoprogesterones ¿ (JG) 3 PREMENSTRUAL SYNDROME Homeopathy Bovista, Borax Physical Medicine Exercise - 20-30 min. 3-4 times weekly has been shown to increase progesterone (DB) Oriental Medicine Psychology 1. Stress Reduction (DB) 2. reframing; discussing positive effects it can offer (JG) Other 1. Increase exercise, decrease body fat (adipose stores estrogen) (JG) 2. Sunlight 1 hour/day 3. Menstrual chart 4. Allopathic: BCP(inhibits ovulation so the rhythms of the estrogen do not happen), lithium, bromacryptin(lowers prolactin levels), B6, tranquilizers, diuretics, antidepressants (JG) 5. Reflexology - ear, hand, foot (DB) 6. Melatonin hypothesis (DB) 7. PMS-D (JG) -tyrosine(500mg 2-4 x day); precursor to serotonin; use B6(200-400 mg) which is a cofactor -hypericum as mood enhancer; JG uses standard extract 4