3. Personal Transferable Skills - Education Programmes
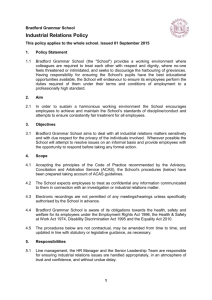
advertisement

http://www.educationprogrammes.bradford.nhs.uk/ Dear Applicant Re: Postgraduate Diploma in Gastroenterology for Practitioners with a Special Interest Thank you for your enquiry related to the Postgraduate Diploma in Gastroenterology for Practitioners with a Special Interest. This document contains information about the above course, an application form for the programme, and information for your future mentor, should you decide you wish to take this application further. This Postgraduate Diploma is designed to encourage the development of the specialist practitioner role by establishing collaborative clinical work-based training between the Practitioner and the Consultant. As it comprises a large element of work-based learning, you do not need to be Bradford based to participate in the course. The award made upon successful completion will either be a Postgraduate Diploma, in which case student completes one service improvement and three clinical modules, or a Postgraduate Certificate, when the service improvement module and one or two clinical modules are taken. The cost for the Diploma is £4,500, the cost for the 60 credit Certificate is £2,250, and the cost for an individual module is £1,125. The awarding institution is the University of Bradford. Should you require any further information regarding the programme after you have read this pack, please contact us by email on psi@bradford.nhs.uk with your query. Should you wish to apply for a place on the course, you should approach a mentor of your choice. Your completed application form, together with the letter of support from your chosen mentor as well as a copy of your mentor’s CV should then be returned to: Belinda Perfitt Education Programmes Team NHS Airedale Bradford and Leeds Douglas Mill Bowling Old Lane Bradford BD5 7JR All documents are required prior to the start date of the course. Should you be unsure of whether you meet the requirements to join the programme, please contact the course team on psi@bradford.nhs.uk for advice. We look forward to hearing from you in the near future. Belinda Perfitt Education Programmes Manager Programme Aims The programme is intended to: develop wider specialist knowledge and skills to enable you to practice gastroenterology at a higher level and to deal with complex clinical situations systematically; develop a thorough understanding of the role and responsibilities of consultant specialists and the multidisciplinary team in secondary care and to establish appropriate relationships with these professionals; position you at the forefront of your area of gastroenterology care to develop and establish the most appropriate integrated care pathways between primary and secondary care for the patient within current NHS guidelines; engage you in life-long learning through the enhancement of key skills, a thorough knowledge of critical appraisal and reflective practice; provide you with transferable nationally recognised training in gastroenterology. Programme Learning Outcomes Critically review and use current and emerging knowledge of the pathophysiology and epidemiology of gastroenterological disorders and their complications. Triage and appropriately refer patients whose symptoms may be due to gastroenterological disorders and their complications. Undertake appropriate investigations for patients presenting with symptoms of gastroenterological disorders and their complications and interpret the results accurately. Diagnose and appropriately manage patients who present with gastroenterological disorders and their complications, by means of clinical interventions. Undertake appropriate evaluation and preventative management of patients with gastroenterological disorders, addressing lifestyle and other related issues. Map and reflect on the entire patient pathway, and appropriately apply service improvement methods to make improvements where necessary to the delivery of care. Work autonomously and collaboratively, in a multidisciplinary context. Critically appraise and update clinical knowledge. Use information technology as a medium for communication and presentation of data. Course Dates These are the provisional dates of the teaching and assessment days, and an indication of the time available for your placement. Attendance at the teaching days is mandatory, unless mitigating circumstances prevent it. Dates 18 October 2012 19 October 2012 20 October 2012 to 17 April 2013 18 April 2013 19 April 2013 20 April 2013 to 16 October 2013 17 October 2013 18 October 2013 19 October 2013 to April 2014 Element of course: Introduction and Applied Modular Assessment Day Methodologies Module for 9.00 am to 5.00 pm new starters 9.00 am to 5.00 pm Modular teaching 9.00 am to 5.00 pm Hepatobiliary Work-based placement - one session per week for at least 14 weeks Introduction and Applied Modular Assessment Day Methodologies Module for 9.00 am to 5.00 pm new starters 9.00 am to 5.00 pm Work-based placement - one session per week for at least 14 weeks Modular teaching 9.00 am to 5.00 pm Upper GI Introduction and Applied Methodologies Module for new starters 9.00 am to 5.00 pm Work-based placement - one session per week for at least 14 weeks Modular teaching 9.00 am to 5.00 pm Lower GI Location: Bradford Bradford Locality Further dates will be provided with as much notice as possible. June 2012 © NHS Bradford and Airedale The Curriculum The Postgraduate diploma consists of four modules, three of which are clinical modules which last for 6 months each, and the Applied Methodologies module which runs alongside the clinical modules over a period of 18 months. Each module is worth 30 credits and consists of 300 hours to cover lectures, seminars, directed study and other work. The entire programme can be completed in 18 months, but practitioners may stagger the modules over a period not exceeding 3 years, other than in exceptional circumstances, when this could be extended to 5 years. The Postgraduate Certificate consists of the Applied Methodologies module and one or two clinical modules. The clinical modules taught alongside the Applied Methodologies module in this programme are the following: Assessment, Diagnosis and Management of Upper Gastrointestinal Disorders Assessment, Diagnosis and Management of Lower Gastrointestinal Disorders Assessment, Diagnosis and Management of Hepatobiliary Disorders An outline syllabus and learning outcomes for each of the modules is given below. Assessment, Diagnosis and Management of Upper Gastrointestinal Disorders Outline syllabus Epidemiology and pathophysiology of Upper GI disorders Differentiation between the varied presentations of Upper GI disorders Critical appreciation of the principles of screening for and diagnosis of Upper GI disorders The appropriate use and delivery of Endoscopy Services Dyspeptic disorders including reflux disease, H Pylori, gall stones Nausea, vomiting and oral lesions Iron deficiency anaemia Gastrointestinal Haemorrhage Reviewing and referral (gateway) Upper GI cancers Learning Outcomes In successfully completing this module, you will be able to: 1. Knowledge and Understanding a. Synthesise the current evidence for the epidemiology and pathophysiology of Upper GI disorders and differentiate between the varied presentations of Upper GI disorders. b. Synthesise the evidence and show an advanced critical appreciation of the principles of screening, diagnosis and the full range of treatment, management and monitoring options for Upper GI disorders. 2. Discipline Skills a. Clinically interpret the result of upper gastrointestinal investigations and upper gastrointestinal endoscopy and appropriately manage and/or refer the outcome. b. Understand the breadth and presentation of various dyspeptic disorders such as reflux disease, H pylori and gall stones. c. Undertake assessment, investigate, diagnose and manage causes of oral lesions. d. Undertake assessment, investigate, diagnose and manage causes of dysphagia. e. Undertake assessment, investigate, diagnose and manage causes of nausea and vomiting. f. Undertake assessment, investigate, diagnose and manage iron deficiency anaemia and related disorders. g. Undertake assessment, investigate, diagnose and manage gastrointestinal haemorrhage. h. Investigate, diagnose and appropriately manage or refer patients with GI cancers. i. Refer patients appropriately for a second opinion for a range of Upper GI disorders. j. Practise evidence based medicine. 3. Personal Transferable Skills a. Practise critical effective problem solving skills. b. Utilise effective team working skills with colleagues and peers. c. Communicate effectively with patients, consultants, other hospital staff, peers and trainers. Assessment, Diagnosis and Management of Lower Gastrointestinal Disorders June 2012 © NHS Bradford and Airedale Outline Syllabus The epidemiology and pathophysiology of Lower GI disorders Differentiation between the varied presentations of Lower GI disorders Critical appreciation of the principles of screening for and diagnosis of Lower GI disorders The appropriate delivery of Endoscopy Services Irritable Bowel Syndrome Inflammable Bowel Disease and manage or refer appropriately Stomas Coeliac Disease Diverticular Disease Wind Reviewing and referral (gateway) Lower GI cancers Anal lesions Rectal bleeding Learning Outcomes In successfully completing this module, you will be able to: 1. Knowledge and Understanding a. Synthesise the evidence for the epidemiology and pathophysiology of Lower GI disorders and differentiate between the varied presentations of Lower GI disorders. b. Synthesise the evidence and show an advanced critical appreciation of the principles of screening, diagnosis, and the full range of treatment, management and monitoring options for Lower GI disorders. 2. Discipline Skills a. Clinically interpret the results of lower gastrointestinal investigations and lower gastrointestinal endoscopy and appropriately manage and/or refer the outcome. b. Investigate, diagnose and appropriately manage or refer patients with diarrhoea and constipation. c. Understand the breadth and presentation of Irritable Bowel Syndrome and manage or refer appropriately. d. Understand the breadth and presentation of Inflammatory Bowel Disease and manage or refer appropriately. e. Investigate, diagnose and appropriately manage or refer patients with Coeliac Disease. f. Investigate, diagnose and appropriately manage or refer patients with Diverticular Disease. g. Investigate, diagnose and appropriately manage or refer patients with Lower GI cancers. h. Investigate, diagnose and appropriately manage or refer patients with less common causes of rectal bleeding. i. Investigate, diagnose and appropriately manage or refer patients with anal lesions. j. Practise evidence-based medicine. 3. Personal Transferable Skills a. Practise critical effective problem solving skills. b. Utilise effective team working skills with colleagues and peers. c. Communicate effectively with patients, consultants, other hospital staff, peers and trainers. Assessment, Diagnosis and Management of Hepatobiliary Disorders Outline Syllabus The epidemiology and pathophysiology of Hepatobiliary disorders Presentations of Hepatobiliary disorders Principles of screening for and diagnosis of Hepatobiliary disorders Treatment, management and monitoring options for Hepatobiliary disorders Endoscopy services Liver disease: Non invasive liver screening (NILS) Abnormal Liver Tests: Alcohol related Fatty liver disease Cholangio pancreaticogrophy June 2012 © NHS Bradford and Airedale MRCP Hepatitis C Jaundice Pancreatic Disease Alcohol Strategies Learning Outcomes In successfully completing this module, you will be able to: 1. Knowledge and Understanding a. Synthesise the evidence for the epidemiology and pathophysiology of Hepatobiliary disorders and differentiate between the varied presentations these disorders. b. Synthesise the evidence and show an advanced critical appreciation of the principles of screening, diagnosis, and the full range of treatment, management and monitoring options for Hepatobiliary disorders. 2. Discipline Skills In successfully completing this module, you will be able to: a. Clinically interpret the results of Hepatobiliary investigations and appropriately manage and/or refer the outcome. b. Understand the breadth and presentation of liver disease (including alcohol related) and to manage or refer appropriately. c. Understand the breadth and presentation of billiary and pancreatic disease and to manage or refer appropriately. d. Investigate, diagnose and appropriately manage or refer patients with abnormal liver tests. e. Investigate, diagnose and appropriately manage or refer patients with viral hepatitis. f. Investigate, diagnose and appropriately manage or refer patients with jaundice. g. To review and implement relevant alcohol strategies and manage hazardous drinking behaviour. h. Practise evidence based medicine. 3. Personal Transferable Skills In successfully completing this module, you will be able to: a. b. c. Practise critical effective problem solving skills. Utilise effective team working skills. Communicate effectively. June 2012 © NHS Bradford and Airedale APPLIED METHODOLOGIES Outline syllabus Critical appraisal research design, qualitative, quantitative, randomised, non-randomised, prospective and retrospective & levels of evidence research analysis statistical analysis research evaluation Process Mapping Current improvement techniques PDSA methodology (Plan Do Study Act) Capacity and demand management including batching and carve out Process mapping / pathway redesign Patient involvement techniques Policy context of involving patients Types of patient involvement Methods of patient involvement including qualitative and quantitative methods Clinical Audit Common approaches, national guidance Reflective model eg. Rolfe 2001 Learning outcomes In successfully completing this module, you will be able to: Knowledge and Understanding a. Critically evaluate clinical research within their area of special interest and understand the implications of it in practice. b. Critically analyse your service in relation to the whole patient pathway, clinical governance and methodologies for change. c. Critically evaluate the evidence and methodologies for patient involvement in healthcare delivery. Discipline skills a. Reflect on and apply the above knowledge to their specific area of clinical practice. Transferable skills a. Reflect on their current practice, as it relates to service improvement. b. Communicate effectively by use of C&IT, particularly in the area of electronic communication and data presentation. Learning and Teaching Methods Your programme of study will start with two teaching days in Bradford (one for the Applied Methodologies module, one for your first clinical module), followed by your clinical attachment and directed study for at least 14 weeks (clinical modules). Alongside this, your directed study for the Applied Methodologies module will begin, for up to 18 months. For your clinical modules only, you will return to Bradford after placement for an assessment day, followed by the next clinical module teaching day. A large proportion of your study will be work-based learning. This learning is undertaken in your locality, under the supervision of a clinical mentor. Mentors are GMC registered consultants in gastroenterology whose names appear on a national register of practitioners. Your clinical mentor will receive a specific Mentor Guide which is included in this pack, as well as advice and support from the course management team. The tasks for your directed study on clinical attachment are as follows: the development and fulfilment of a programme of activities with your mentor, in order to fulfil clinical competence-based learning outcomes; recording your placement cases using a reflective learning diary, to record your learning progress and learning needs; obtaining essential background information to the module studied to inform your practice and the preparation of assessed work, through guided reading in the form of lists and website references; discussions concerning your June 2012 © NHS Bradford and Airedale learning needs and possible solutions through scheduled meetings with your mentor (eg. advice, further reading, alteration of elements of your programme). The Applied Methodologies module involves working within your healthcare community to apply three different methodologies. Directed study comprises researching and reading information, planning, preparation and application of these. Peer learning is encouraged through peer contact in Bradford, and through participation in “Blackboard”, the virtual learning environment accessed via the University of Bradford website. It is anticipated that you will continue to work in your normal practitioner setting during the period of study, and it is expected that ongoing learning will be applied in this context. Assessment You will be assessed in a variety of ways, including written case studies and oral presentations; however, there will be no formal written exams. Verification of clinical competence must be indicated by your consultant-mentor's signature on assessment day. Clinical competence is a pass/fail element, with no mark attached to it. All written work and the critical appraisal presentation must be presented on assessment day, in order for you to progress to the next module. All assessment tasks must be passed by attaining 40% of the full marks. Masters level marking criteria will be made available to you to help you check your work. One opportunity to resubmit work along the same lines as the sessional assessment will normally be allowed. The standard thresholds of distinction (minimum of 70% overall average) and merit (60-69% overall average) will apply for marked work of an exceptional nature for the award of the Postgraduate Diploma and Postgraduate Certificate. Participants who succeed in one module only, and who do not qualify for one of the above awards, shall be eligible for the award of a Certificate of Continuing Education. Admission Requirements The application process is divided into two parts: 1. Submission of an application form indicating that you meet the professional/educational criteria. 2. Submission of letters of support showing suitability for you to undertake this course of study. To be accepted onto the Diploma or Certificate, and to benefit from this course of study, you must meet the admission requirements for Masters level, as outlined by the University of Bradford, in addition to those required by NHS Bradford and Airedale. You should be a registered practitioner (GMC, NMC or HPC as appropriate) who falls within the following groups: General practitioner; specialist nurse; nurse practitioner; nurse consultant; clinical assistant; other suitably qualified registered primary care practitioner. GPs are additionally required to provide their GP Qualification details and GMC registration number, and to show an interest or a background in gastroenterology. It is desirable, but not essential, for GPs to be Members of the Royal College of General Practitioners. If you are not a GP, you must have, and provide evidence of a Gastroenterology-related Diploma or equivalent; several years' experience in gastroenterology; and 2-3 years post-qualifying practitioner experience. It is desirable for candidates to have experience in post-graduate education. All applications will be judged on their own merit and prior learning experience. While making your application for the programme, you must obtain support from your local NHS hospital trust consultant in gastroenterology (GMC Registered) for mentorship and the provision of a placement. Without this evidence of support, you cannot be admitted on to the programme. Should you be unsure of whether you meet the requirements to join the programme, please contact the course team on psi@bradford.nhs.uk for advice. We can admit up to 12 participants per clinical module, with entry points in October and April. Student support and guidance The course study guide which will be issued to you at the beginning of the programme will support you in all aspects of work-based learning and assessments. Tutor support will be provided by a system of email queries, initially. Peer support is available to assist you with your clinical questions through participation in “Blackboard”. It is anticipated that a significant amount of discussion relating to cases, working arrangements, progress and approaches to study will result from this group. Support you can expect from your mentor is outlined within the mentor guide. The guide also enables mentors to understand the support they will receive automatically, and can gain if required, from the course tutors. You are invited and encouraged to express your opinions about the course structure, materials, process etc throughout your training, and will have a formal feedback opportunity after the first module is completed. Thereafter, participants may nominate a number of student representatives to join the Course Management Committee and they may offer feedback through this committee. Each individual student is June 2012 © NHS Bradford and Airedale also asked to complete paper-based evaluation forms for end of unit (module) and stage (course) evaluation from the University of Bradford. You are also made aware of your responsibilities in the participant study guide: taking responsibility for organising your own learning, ensuring your placement arrangements are acceptable; returning course forms/assessment submissions on time; attendance at the first teaching day and the concluding assessment day for each clinical module and at the initial teaching day for the core module; patient confidentiality; working to a professional code of conduct; and alerting the course tutors to problems which will affect your training. Disclaimer Changes in the above specification may be made at any time by NHS Bradford and Airedale, but notification will be made to you as appropriate. Elements of the programme are subject to University conditions including its status as an approved course. The University reserves the right to alter or withdraw these elements at any time, and notification will be made to you by NHS Bradford and Airedale should this occur. Students with Disabilities We endeavour to make our course accessible to everyone. Please indicate below if you require any information to be presented in a different format (please specify): June 2012 © NHS Bradford and Airedale APPLICATION FORM Postgraduate Diploma in Gastroenterology for Practitioners with a Special Interest First name ________________________________________________________________________ Last name ________________________________________________________________________ Title _________________________________ Date of Birth _____________________________ Home Address ___________________________________________________________________ ________________________________________________________________________________ _________________________________________________________________________________ ______________________________________ Post Code __________________________________ Profession _______________________________________________________________________ Telephone (please specify work or home) Landline __________________________________________________________________________ Mobile ___________________________________________________________________________ email address (PLEASE WRITE CLEARLY)_____________________________________________ Professional Qualifications _________________________________________________________________________________ Other relevant Postgraduate Qualification(s) or Experience _________________________________________________________________________________ GP registration number, Nursing and Midwifery council PIN or other professional registration number (if relevant) _________________________________________________________________________________ Briefly outline your interest in working as a PwSI or in developing specific clinical skills. Include current/planned activities as appropriate. _________________________________________________________________________________ _________________________________________________________________________________ Details of the hospital you will link your clinical training to Hospital name _____________________________________________________________________ Address ____________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ June 2012 © NHS Bradford and Airedale Details of the registered consultant who will act as your mentor Name ___________________________________________________________________________ Postal address _____________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ Telephone number __________________________________________________________________ For invoicing purposes, please note the following: Contact name: _____________________________________________________________________ Address __________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ Email address: _____________________________________________________________________ Telephone number: _________________________________________________________________ Please circle the programme of study for which you wish to register A) Diploma: 3 clinical modules and Applied Methodologies (AM) (£4,500) B) Certificate: 2 clinical modules and AM (£4,500) (see next question) C) Certificate: 1 clinical module and AM (£2,250) (see next question) D) Single module (£1,125) (see next question) For the Certificate or single module only, please circle the module(s) you wish to study i Assessment, Diagnosis and Management of Upper Gastrointestinal Disease ii Assessment, Diagnosis and Management of Lower Gastrointestinal Disease iii Assessment, Diagnosis and Management of Hepatobiliary Disorders iv Applied Methodologies Indicate your preferred start month and year (October or April). Please note that we cannot guarantee your start date or the order in which clinical modules are undertaken. Places will be allocated with priority to diploma students. Please outline below any information you wish to give to support your application. If you wish to stagger your modules across more than 18 months, please refer to that and the factors influencing your planned study, ie consultant availability, personal circumstances, service delivery commitments. _________________________________________________________________________________ _________________________________________________________________________________ June 2012 © NHS Bradford and Airedale _________________________________________________________________________________ _________________________________________________________________________________ Non-native English speakers: As the assessment elements of the postgraduate diploma require a substantial amount of written work at masters level, in accordance with regulations from the University of Bradford we ask that non-native speakers complete an IELTS English Language Exam before they begin their studies. Please indicate here if you have completed the IELTS exam and if so also include your result (further details can be found at www.ielts.org) __________________________________________________________________________________ Please indicate where you heard about our course: Article (please specify which) __________________________________________________________ Advertisement (please indicate where this was) ____________________________________________ Website ___________________________________________________________________________ Other _____________________________________________________________________________ Please ensure that the following completed letters of confirmation have been attached to this form. i. Consultant Mentor ii. Mentor’s CV Please note that in order to confirm your place and start date the completed documentation as detailed above would need to be received one month prior to your requested start date. Should you be unsure of whether you meet the requirements to join the programme, please contact the course team on psi@bradford.nhs.uk for advice. June 2012 © NHS Bradford and Airedale EQUAL OPPORTUNITIES INFORMATION (confidential) Course applied for: Start date 1. Please tick the appropriate age range 20 – 30 __ 30 – 40 __ 40 – 50 __ 50 – 60 __ over 60 __ 2. Please note your gender __________ 3. Please note the number of years you have been qualified 4. Please note the number of years you have been practicing _______ 5. Please note your ethnicity _______________________________________ 6. Do you consider yourself to be disabled? yes/no 7. If you have answered yes to the previous question, please provide further details of your disability ______________________________________________________________ 8. Please note any further comments you wish to make _______ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ June 2012 © NHS Bradford and Airedale NOTES AND COSTS Practitioners to undertake the course A Postgraduate Diploma costs £4,500 (all 4 modules) A 90 credit Postgraduate Certificate costs £4,500 (2 clinical modules and AM) A 60 credit Postgraduate Certificate costs £2,250 (1 clinical module and AM) A single 30 credit module costs £1,125 In undertaking this course, the candidate is making a commitment to update their professional knowledge after the course is finished. This will probably occur through the professional appraisal process, and is required by the University to retain a valid award. Travel For a full course, this will require 3 trips of two days and a last single day to Bradford. Accommodation For a full course, 3 overnight stays, unless local to Bradford (Possibly 8 if the candidate cannot travel to Bradford to commence a taught day at 9.00am). Time: Locum cover / backfill costs for at least 14 clinical sessions per module, and two days attendance per clinical module and one for introduction/AM module. Personal study above these sessions is an issue for local agreement and the module descriptors give information regarding time allocation for study. June 2012 © NHS Bradford and Airedale Dear Consultant Re: Postgraduate Diploma/Certificate for Practitioners with a Special Interest in Gastroenterology The practitioner presenting you with this letter wishes to apply for the above-named course. It is mainly a competence-based course and seeks to extend the training of the Practitioner with a Special Interest (PwSI) to an advanced level. This complies with developments and guidance issued through the Modernisation Agency and the Royal College of General Practitioners and advice from the Royal College of Physicians. In order for them to be selected, they must undertake to work with a named mentor, who is a consultant in Gastroenterology at their local NHS trust hospital. They have chosen you to mentor them for the duration of the course, and you must therefore understand the commitment you are undertaking, if you choose to support them. You should consider whether you are prepared in principle to support this individual for training at a more advanced level in Gastroenterology. If you know them already, this judgment should be made on the basis of your information regarding their professional capability to be trained in this manner. If you do not know them, you may wish to speak to them about their professional background, current interests in Gastroenterology and future plans. Advanced Nurse Applicants Our experience from these practical, clinical courses so far is that many secondary care nurses achieve well in the Diploma. However, some nurses may have difficulty in accessing patients for the modules which are outside their area of practice. They may also require prior training in clinical history taking and physical examination. Please can you discuss these areas with the applicant and ensure that you are satisfied that they will be able to undertake the Postgraduate course. During their training, you will engage in creating a programme of activities with them. This will identify their learning needs and permit them to acquire the knowledge and experience, and perform the skills required for their workbased learning in gastroenterology. The practitioner has a copy of the syllabus and learning outcomes for the modules they plan to undertake, as well as a mentor guide, a copy of which you should receive. For each clinical module the candidate will need at least one session per week to train in the work-based clinical attachment within the hospital over a minimum of a 14 week period. During this time, as a mentor, you and members of your team will be observing the candidate's work with patients, offering advice, support and opportunities for learning by reflection. Time to discuss problems and to offer constructive feedback should be part of this process. During and at the end of the training, you will assess the clinical and professional competence of the candidate. Your signature of competence against the modular learning outcomes and the agreed programme will carry great weight in the overall assessment of the candidate. Together with the outcome of their course work, he or she will pass or fail the course on this signature. Ultimately, the benefits of working in this mentoring relationship will affect your service directly, as patient access in gastroenterology is improved. Please give your worthy consideration to this matter and fill in the attached response form accordingly. You may wish to inform the candidate of your response separately. If you are willing to act as a mentor, to comply with the University of Bradford regulations, please could you attach a copy of your CV to this letter, or email it directly to belindajane.perfitt@bradford.nhs.uk . Yours faithfully Belinda Perfitt Education Programmes Manager June 2012 © NHS Bradford and Airedale CONSULTANT RESPONSE OF SUPPORT Please complete the form below and send to: Belinda Perfitt PwSI team NHS Bradford and Airedale Douglas Mill Bowling Old Lane Bradford BD5 7JR I (name) ………………………………………………………………………………………. GMC Number …………………………………………………………………………………. of the (name and address of hospital) ……………………………………………………. …………………………………………………………………………………………………. …………………………………………………………………………………………………. Telephone contact number .………………………………………………………………… Email address ……………………………………………………………………………….. am willing to support (candidate's name):………………………………….………….. and recognise their suitability for participation in the Postgraduate Diploma/Certificate in Gastroenterology for Practitioners with a Special Interest, having discussed their clinical experience and their experience/training in diagnosis, clinical history taking and physical examination, for the module (s): Applied Methodologies Assessment, Diagnosis and Management of Upper Gastrointestinal Disease Assessment, Diagnosis and Management of Lower Gastrointestinal Disease Assessment, Diagnosis and Management of Hepatobiliary Disorders I am willing to engage in the creation of the learning programme, to offer mentor observation, advice, support and opportunities for learning by reflection, and to assess the clinical competence of the candidate. I have forwarded a copy of my CV to The Education Programmes Team Co-ordinator. Signed:………………………………………………. Date:…………………………………………… Hospital June 2012 © NHS Bradford and Airedale Information To Advanced Level Nurses Regarding: POSTGRADUATE AWARDS FOR PRACTITIONERS WITH A SPECIAL INTEREST (Bradford) The following advice is available to help direct your study options. Pre-Entry Advice: 1. You will need to be working at a level of advanced practice in order to be able to clinically assess patients to achieve the competencies. 2. In order to start the course with the clinical assessment skills necessary, you are strongly advised to attend short courses or gain experience in diagnosis/differential diagnosis and clinical examination (ie. before the diploma begins). M&K currently offer a three day course on Clinical History Taking and Physical Examination; similar courses may also exist elsewhere. You may be able to spend time alongside a general practitioner to gain practical experience of diagnosis skills, use of a stethoscope etc. Entry Advice 1. You may wish to enrol in the first instance for the 60 credit Postgraduate Certificate (the Applied Methodologies module and the clinical module which relates to your specialist area), with the option of expanding your studies to the two clinical module Certificate (with Applied Methodologies), or to the Diploma (Applied Methodologies and three clinical modules), as appropriate. These additional clinical modules would be agreed with the course team, subject to the complete submission of work each assessment day for the previous module. These could be paid for separately, at an agreed time before the start of each new module. 2. You are free to enrol on the Diploma from the outset, if you have every intention of studying for it, in which case the whole fee should be paid at the beginning of the course as normal. 3. For those taking the Diploma it is best to start your course with the module relating to your own specialist area. There are fewer issues to overcome in your own clinical area, whilst you get used to the structure and demands of the course. This is the recommendation of all the secondary care based nurses in the pilot groups and we would therefore recommend this pattern as beneficial, whether you are working in secondary or primary care. 4. Often, specialist nurses cannot find time to attend clinics outside their specialist area. It can also be an issue within the specialist area itself, as there are usually restrictions to your location. Therefore, a letter is available to give to your nurse manager, in order to establish whether an agreement can be obtained for you to visit and work outside your clinic for placement sessions. This agreement should be established at the outset, so that you do not get into difficulties with your studies during the course. 5. You may also wish to obtain designated support in the form of free time/designated study time. Without this, there can be pressures on studying due to catching up ordinary workloads. 6. Where you are expecting to study more than one clinical module, you should plan for studies in future modules whilst you are studying your first clinical module. This will require talking to colleagues within those areas and asking the mentor to negotiate suitable clinics. 7. To make the most of your programme of study, you are likely to need negotiation skills and to be proactive in your approach. You will need to ensure that placement session times are made available and that support with workload is received. 8. The Diploma programme can be extended to a Master of Science award. Any successful graduate from the diploma programme is eligible to undertake this programme of study, providing other entry criteria can be met. Please email us on psi@bradford.nhs.uk for more information. June 2012 © NHS Bradford and Airedale Letter for Nurse Managers: Nurse Manager c/o Nurse applicant for Postgraduate Diploma in Gastroenterology for Practitioners with a Special Interest Dear Sir/Madam Re: Postgraduate Certificate/Diploma for Practitioners with a Special Interest We are glad to accept the application for your nurse practitioners/nurse consultants/specialist nurse onto our Postgraduate Certificate and Diploma programme. Having undertaken pilots for similar nurses on these courses, we are conscious that successful training requires the following: Time out of their own clinic/work to undertake the mandatory 1 session per week on “placement” within the hospital and other appropriate clinics for a minimum of 14 sessions per clinical module. Recognition that even within their specialist area, there will be need to observe and be involved in other related areas to gain a breadth of experience, also necessitating cover for their ordinary work Consultant supervision/observation of nurses working “hands on” with patients in areas within, but particularly outside their specialism is vital. This enables nurses to gain the experience required for Postgraduate level, to demonstrate clinical competence in diagnosis, investigation and management of other conditions, rather than be judged by what their service may require. Other elements of support which would significantly enhance the training opportunity would include time given for the nurse to pursue supporting academic studies (preparation of written clinical cases, guided reading and journaling, and the preparation of presentation of clinical papers), and for discussion with the supervising consultant specialist. As line manager to this applicant, would you discuss with him/her the possibilities of ensuring the above as they relate to the programme of study undertaken. By all means, contact me by email on belindajane.perfitt@bradford.nhs.uk in order to discuss issues surrounding the viability of study or the best approach to it. Yours sincerely Belinda Perfitt Education Programmes Manager June 2012 © NHS Bradford and Airedale Hospital Manager - RESPONSE OF SUPPORT (for secondary care nurses) Please fill in the form below and send to: Belinda Perfitt Education Programmes Team PwSI Bradford and Airedale teaching Primary Care Trust Douglas Mill Bowling Old Lane BRADFORD BD5 7JR I (name and position):……………………………………………………………….. of the (name of Hospital) :……………………………………………………………….. am willing to support (candidate's name): …………………………………….……… for participation in the Postgraduate Diploma/Certificate in Gastroenterology for Practitioners with a Special interest For the module (s): Applied Methodologies Assessment, Diagnosis and Management of Upper Gastrointestinal Disease Assessment, Diagnosis and Management of Lower Gastrointestinal Disease Assessment, Diagnosis and Management of Hepatobiliary Disorders We hereby commit support time for study and practical clinical experience as is necessary for the above candidate (once accepted onto the course) to complete the Postgraduate Award. Further comments (please indicate any further support offered, information about the candidate etc) Signed:……………………………………………… Hospital stamp/authenticating mark June 2012 Date………………………… © NHS Bradford and Airedale MENTOR GUIDE Postgraduate Diploma in Gastroenterology for PwSI List of Contents Page number Introduction 1 What we ask of you Roles of mentor and assessor 1 What is in the course 2 Establishing the learning programme Four stage process Clinical competence forms 6 Student learning, reflection and discussion 10 Assessing clinical competence How to sign a student off 11 What we can do for you Bradford-based support Contact details June 2012 13 © NHS Bradford and Airedale June 2012 © NHS Bradford and Airedale Introduction Thank you for your interest in being a mentor for a student on the Postgraduate Diploma in Gastroenterology for PwSI. This course is one of a series of NHS run courses which provides accredited competence based training for Practitioners with a Special Interest. If you require further information about the course, your student has a comprehensive study guide. Alternatively, contact us by email: psi@bradford.nhs.uk. Your feedback about the course is very valuable to us, and will be welcomed in any form throughout the programme. As a consultant your help is needed to ensure that your student, who will learn locally in your clinics, is adequately trained to an agreed level of competence. It is our expectation that following the course, the collaborative relationship between yourself and your student will continue. What we ask of you You will have two roles within the programme. Mentor Assessor Mentor role We anticipate that all mentors will be GMC registered specialists and that you have been through a recognised body for training to undertake mentorship. We draw your attention to the fact that whilst you are called upon to direct and assess the overall programme, other clinicians may be involved with the provision of training activities for the student. There are four main tasks as mentor: 1 2 3 4 establish and oversee a learning programme with your student based on mandatory learning outcomes and their learning needs; encourage your student to develop their skills and knowledge by reflection, reading and discussion about cases, with you and other colleagues; provide time in which to discuss cases and reflect on learning; provide opportunity for hands-on work. Assessor role This role requires you to: Assess the student’s clinical competence given the appropriate opportunities. All of these roles are outlined with examples in the next sections. ____________________________ 12/02/2016 1 NHS Bradford and Airedale The Award The Postgraduate Diploma for Practitioners with a Special Interest is a masters level award. The candidate can gain credits for each module undertaken towards a full award (Diploma), a semiaward (Certificate) or a credited transcript of work. The value of each module is 30 masters level credits. This approximates to 300 hours total learning time for the participant per module, 70 hours or more of which is undertaken on practical placement in clinic across a minimum of 14 sessions. The Modules There are four modules on the diploma course. Three of these are concerned with clinical competence, based on a series of learning outcomes which are listed below, and will be undertaken in the student’s locality on placement in your hospital. Each takes six months to complete. The fourth module (Applied Methodologies) is a written module relating to service improvement and is studied throughout the 18 month period. In addition to work-based learning, the course includes teaching and assessment days in Bradford at the beginning and end of every module, guided reading lists to support learning and an interactive virtual learning environment on the University of Bradford website. The Training Programme On the clinical attachment with you, the student will develop, run and evidence their training programme. The training programme is based on a series of mandatory learning outcomes to which you and the student will attach appropriate activities. The Procedures The course has been developed by The Education Programmes Team at NHS Bradford. Accreditation is provided by the University of Bradford. The teaching, learning and assessment criteria are all in line with University of Bradford regulations and come under the University quality control procedures. Course contents The Curriculum The Postgraduate diploma consists of four modules, three of which are clinical modules which last for 6 months each, and the Applied Methodologies module which runs alongside the clinical modules over a period of 18 months. Each module is worth 30 credits and consists of 300 hours to cover lectures, seminars, directed study and other work. The entire programme can be completed in 18 months, but practitioners may stagger the modules over a period not exceeding 3 years, other than in exceptional circumstances, when this could be extended to 5 years. The Postgraduate Certificate consists of the Applied Methodologies module and one or two clinical modules. The clinical modules taught alongside the Applied Methodologies module in this programme are the following: Assessment, Diagnosis and Management of Upper Gastrointestinal Disorders Assessment, Diagnosis and Management of Lower Gastrointestinal Disorders Assessment, Diagnosis and Management of Hepatobiliary Disorders An outline syllabus and learning outcomes for each of the modules is given below. Assessment, Diagnosis and Management of Upper Gastrointestinal Disorders Outline syllabus Epidemiology and pathophysiology of Upper GI disorders Differentiation between the varied presentations of Upper GI disorders Critical appreciation of the principles of screening for and diagnosis of Upper GI disorders __________________________ 12/02/2016 2 © NHS Bradford and Airedale The appropriate use and delivery of Endoscopy Services Dyspeptic disorders including reflux disease, H Pylori, gall stones Nausea, vomiting and oral lesions Iron deficiency anaemia Gastrointestinal Haemorrhage Reviewing and referral (gateway) Upper GI cancers Learning Outcomes In successfully completing this module, you will be able to: 1. Knowledge and Understanding c. Synthesise the current evidence for the epidemiology and pathophysiology of Upper GI disorders and differentiate between the varied presentations of Upper GI disorders. d. Synthesise the evidence and show an advanced critical appreciation of the principles of screening, diagnosis and the full range of treatment, management and monitoring options for Upper GI disorders. 2. Discipline Skills k. Clinically interpret the result of upper gastrointestinal investigations and upper gastrointestinal endoscopy and appropriately manage and/or refer the outcome. l. Understand the breadth and presentation of various dyspeptic disorders such as reflux disease, H pylori and gall stones. m. Undertake assessment, investigate, diagnose and manage causes of oral lesions. n. Undertake assessment, investigate, diagnose and manage causes of dysphagia. o. Undertake assessment, investigate, diagnose and manage causes of nausea and vomiting. p. Undertake assessment, investigate, diagnose and manage iron deficiency anaemia and related disorders. q. Undertake assessment, investigate, diagnose and manage gastrointestinal haemorrhage. r. Investigate, diagnose and appropriately manage or refer patients with GI cancers. s. Refer patients appropriately for a second opinion for a range of Upper GI disorders. t. Practise evidence based medicine. 3. Personal Transferable Skills d. Practise critical effective problem solving skills. e. Utilise effective team working skills with colleagues and peers. f. Communicate effectively with patients, consultants, other hospital staff, peers and trainers. Assessment, Diagnosis and Management of Lower Gastrointestinal Disorders Outline Syllabus The epidemiology and pathophysiology of Lower GI disorders Differentiation between the varied presentations of Lower GI disorders Critical appreciation of the principles of screening for and diagnosis of Lower GI disorders The appropriate delivery of Endoscopy Services Irritable Bowel Syndrome Inflammable Bowel Disease and manage or refer appropriately Stomas Coeliac Disease Diverticular Disease Wind Reviewing and referral (gateway) Lower GI cancers Anal lesions __________________________ 12/02/2016 3 © NHS Bradford and Airedale Rectal bleeding Learning Outcomes In successfully completing this module, you will be able to: 1. Knowledge and Understanding a. Synthesise the evidence for the epidemiology and pathophysiology of Lower GI disorders and differentiate between the varied presentations of Lower GI disorders. b. Synthesise the evidence and show an advanced critical appreciation of the principles of screening, diagnosis, and the full range of treatment, management and monitoring options for Lower GI disorders. 2. Discipline Skills d. Clinically interpret the results of lower gastrointestinal investigations and lower gastrointestinal endoscopy and appropriately manage and/or refer the outcome. b. Investigate, diagnose and appropriately manage or refer patients with diarrhoea and constipation. c. Understand the breadth and presentation of Irritable Bowel Syndrome and manage or refer appropriately. d. Understand the breadth and presentation of Inflammatory Bowel Disease and manage or refer appropriately. e. Investigate, diagnose and appropriately manage or refer patients with Coeliac Disease. f. Investigate, diagnose and appropriately manage or refer patients with Diverticular Disease. g. Investigate, diagnose and appropriately manage or refer patients with Lower GI cancers. h. Investigate, diagnose and appropriately manage or refer patients with less common causes of rectal bleeding. i. Investigate, diagnose and appropriately manage or refer patients with anal lesions. j. Practise evidence-based medicine. 3. Personal Transferable Skills a. Practise critical effective problem solving skills. e. Utilise effective team working skills with colleagues and peers. f. Communicate effectively with patients, consultants, other hospital staff, peers and trainers. Assessment, Diagnosis and Management of Hepatobiliary Disorders Outline Syllabus The epidemiology and pathophysiology of Hepatobiliary disorders Presentations of Hepatobiliary disorders Principles of screening for and diagnosis of Hepatobiliary disorders Treatment, management and monitoring options for Hepatobiliary disorders Endoscopy services Liver disease: Non invasive liver screening (NILS) Abnormal Liver Tests: Alcohol related Fatty liver disease Cholangio pancreaticogrophy MRCP Hepatitis C __________________________ 12/02/2016 4 © NHS Bradford and Airedale Jaundice Pancreatic Disease Alcohol Strategies Learning Outcomes In successfully completing this module, you will be able to: 1. Knowledge and Understanding a. Synthesise the evidence for the epidemiology and pathophysiology of Hepatobiliary disorders and differentiate between the varied presentations these disorders. b. Synthesise the evidence and show an advanced critical appreciation of the principles of screening, diagnosis, and the full range of treatment, management and monitoring options for Hepatobiliary disorders. 2. Discipline Skills In successfully completing this module, you will be able to: i. Clinically interpret the results of Hepatobiliary investigations and appropriately manage and/or refer the outcome. j. Understand the breadth and presentation of liver disease (including alcohol related) and to manage or refer appropriately. k. Understand the breadth and presentation of billiary and pancreatic disease and to manage or refer appropriately. l. Investigate, diagnose and appropriately manage or refer patients with abnormal liver tests. m. Investigate, diagnose and appropriately manage or refer patients with viral hepatitis. n. Investigate, diagnose and appropriately manage or refer patients with jaundice. o. To review and implement relevant alcohol strategies and manage hazardous drinking behaviour. p. Practise evidence based medicine. 3. Personal Transferable Skills In successfully completing this module, you will be able to: d. e. f. Practise critical effective problem solving skills. Utilise effective team working skills. Communicate effectively. __________________________ 12/02/2016 5 © NHS Bradford and Airedale Establishing the learning programme This section covers the development, running and evidencing of the training programme. The use of clinical competence forms These forms are used to plan, and later assess the learning which has taken place for your student. There is one clinical competence form for each learning outcome to be undertaken on clinical attachment for each of the clinical modules. There are two types of forms: training programme forms evidence forms All activities are to be recorded by the student on the training programme form. Towards the end of the module, students will complete their evidence forms to show how their learning programme has been achieved. With your student, you will agree a training programme for his/her clinical attachment sessions, to be documented on each form. The forms are then used as an active training document to inform the initial and continued training programme whilst on clinical attachment and as such, must always be made accessible to you, as mentor, and to any relevant clinician with whom your student is working. The evidence form is to be used to document the ways in which the training programme has been fulfilled. Here, comments and signatures will be required from you as mentor and other members of staff to authenticate the training under each learning outcome. Finally, you will decide whether to sign the student off as 1) competent, 2) not yet competent and requiring an extension of time or 3) not competent, despite having had opportunity to become so. This will be based on your and others’ experience and assessment of working with the student. These forms provide the greatest part of the student’s summative assessment for the module, because on this element alone they can pass or fail the module. This process is undertaken in four stages, as described below. Stage One: Induction/Preparation Explain the practical hospital details affecting the student, in particular lines of communication/ your whereabouts and procedures in case of emergency situations. Please cover appropriate aspects of: occupational health and safety indemnity cover dealing with emergencies patient confidentiality The student will prepare suggested activities for the training programme. Stage Two: First meeting Meet with the student to discuss the learning outcomes and his/her proposals for training activities to fulfil those, using the training programme forms. Together, devise a programme of activities covering each learning outcome which is satisfactory to __________________________ 12/02/2016 6 © NHS Bradford and Airedale you and your student, and which covers the essential requirements stated above. These activities should include: The types of clinic to be attended The types of patient cases to be seen Other types of input eg. Meetings, visiting or shadowing relevant staff; external input; tutorials by a mentor or hospital team member etc The student should write up the proposed activities on the forms and should send a copy of the form signed by you, to the Education Programmes Management Team, by post within 2 weeks of commencement of each of the clinical modules. Plan when and where (eg specialist clinic) the student will start their clinical attachment, and when and where you can be located. You should expect to meet most clinic sessions and the student should certainly be adequately supervised when you are not available. There are a number of models which can be followed to ensure that your student gains sufficient experience to become competent. These include; observing you in clinics, working hands on with you in your clinics and ultimately seeing patients on their own. NB Students may work with more than one consultant colleague, but for the purposes of the course, they should consider only one consultant to be their mentor, and this is the individual whose name appears on the initial letter of support, and who will sign their evidence forms. Stage Three: Once activities have started Your oversight will be required for the following student activities: Practical activities as they work through their training programme Recording cases of note in their clinical learning diary. Seeing you and/or another team member as appropriate, each session Obtaining signatures/comments as appropriate for work done. Obtaining evidence (copies or originals) as appropriate for work done. Stage Four: Evidencing the learning outcomes When a learning outcome has been completed, the task of writing up evidence is to be undertaken by the student. Using the evidence form for each learning outcome, ensure that the following evidence is included by the student to show they have fulfilled their learning activities: A list showing how many patients have been seen for each learning outcome. Reference to other areas of the activities shown on the student’s initial training programme which have been fulfilled. Description of other activities undertaken to support the student’s learning not listed on the initial training programme. Where activities from the student’s initial training programme have not been fulfilled, justification or explanation: where these are rarer conditions which have not been seen, you should indicate clearly your opinion of the student’s ability to manage such a condition. __________________________ 12/02/2016 7 © NHS Bradford and Airedale CLINICAL COMPETENCE FORM TRAINING PROGRAMME Name: TO BE COMPLETED BY STUDENT Learning Outcome: AS PER THE MODULE DESCRIPTOR Self Developed Learning Outcome (optional): TO BE COMPLETED BY STUDENT Training programme outline: TO BE COMPLETED BY STUDENTS To include CLINICS CLINICAL ACTIVITIES OTHER ACTIVITIES Confirmation that this training programme outline aims to fulfil the above learning outcome Please sign only when this programme is confirmed between student and mentor: Mentor name: Mentor signature Date: YOUR NAME YOUR SIGNATURE For use by NHS Bradford and Airedale only: checked by ……………………………………………. Date………………………………………….. __________________________________ 12/02/2016 8 © NHS Bradford and Airedale EVIDENCE Name: TO BE COMPLETED BY STUDENT Learning outcome: AS PER THE MODULE DESCRIPTOR Evidence of activities undertaken for this training programme listed below (see handbook section 4 for instructions on completion) Activity Type of patient No of patient cases Reading materials eg guidelines To be completed by mentor only I am satisfied that in the above learning outcome ……………………………………………………………….……… (student’s name) A Is competent B requires and extension of time to become fully competent C Is not competent Signature of Mentor (please sign one box only) YOUR SIGNATURE IN ONE BOX ONLY Mentor’s Name (please print) PRINT YOUR NAME HERE YOUR SIGNATURE IN ONE BOX ONLY Date: …………………………………………… YOUR SIGNATURE IN ONE BOX ONLY For use by NHS Bradford and Airedale only: checked by ……………………………………………. Date………………………………………….. __________________________________ 12/02/2016 9 © NHS Bradford and Airedale Student learning, reflection, and discussion about cases 1 Aims of your discussions structured time for the student to discuss cases/problems arising in clinic; regular constructive feedback for the student; encouragement to self-appraisal, helping the student to reflect on his/her practice and the relevant evidence base confidential and focussed discussion of relevant patient cases. You and your student should arrange contact time throughout the module in the way which best suits you both. This could include: during consultation: formative discussion held in consultant’s office about diagnosis and choice of management of patients during clinic; regular planned debriefing of 10 minutes to half an hour every session or every fortnightly session, at the end of each clinic; pre-arranged discussions or specially organised tutorial sessions. 2 Areas for discussion feedback on student’s progress issues arising out of cases seen or observed in your clinics; issues arising out of cases seen in general practice; interesting cases seen by consultant; learning from wider reading or new clinical updating; in depth learning about a topic which requires more input; encouraging the student to complete their learning diary (here they must record a minimum of 14 cases which provide learning and/or action points) as soon after clinical experience as they can and to focus on their understanding, knowledge and skills, and identify how these are changing. 3 Guided reading Students will mainly read around their immediate coursework / assessed work requirements. Please make your student aware of wider areas of knowledge from the reading list, or your own sources. THINGS MENTORS AND STUDENTS SAY ABOUT CLINICAL ATTACHMENT 1 Student feedback continuously confirms that that the most effective form of training was hands-on experience. This was expressed by very experienced practitioners, and those with less clinical experience. 2 All mentors visited made efforts to select the most appropriate patient cases for trainees to see. 3 Mentors want trainees to see them in between every, or most patients with proposed diagnoses and management plans. 4 PwSIs want to see their mentor for every patient/most cases due to the learning opportunity this represents and in light of their own understanding that their knowledge is limited. 5 PwSIs want to be entrusted with patients in order to gain confidence, and recognise where the limitations of their knowledge lie. 6 Mentor and PwSI discussion about patients highlights gaps in PWSI knowledge. 7 As students work in the hospital longer, they know staff better so hospital mechanisms __________________________________ work better. 12/02/2016 10 © NHS Bradford and Airedale Assessing clinical competence Assessment is continuous throughout the clinical attachment and can be done in a number of ways, for example: observation and note taking discussion about cases/perspectives/the fulfilment of learning needs looking at the clinical competence form (comments and signatures from other staff etc) examples of evidence and clinical pieces of work presented by the student reference to the learning diary Assessing learning outcomes individually Each learning outcome must be assessed during the clinical attachment. This covers both clinical and transferable key skills. Please refer to the student's Clinical Competence Forms for details. Ongoing sign-off of competence Please check comments and signatures from other members of staff who may have signed off clinical competence for individual activities. Please also check the evidence being presented by the student to support his/her competence, before you sign him/her off. You can also sign off clinical activities, but only you may sign for the final satisfaction of clinical competence in a given learning outcome (see overleaf). It is likely that sign-off will occur throughout the clinical attachment rather than just at the end, as individual outcomes are completed. Week 20 progress You and the student will be contacted separately by email to establish if there are any anticipated problems in the student’s progress. Learning diary sign-off Please sign the learning diary which records a minimum of 14 cases seen. This can be signed throughout clinical attachment following your discussions and at the end of clinical attachment when the record is complete. Information about other student assessed work During the clinical attachment your student will prepare two case studies and critical appraisal of a clinical paper. The case studies will be submitted as written pieces of work, the critical appraisal as a presentation. Before the assessment day at the end of the module, it would be helpful to your student for you to read and comment on the written work and to watch the presentation. __________________________________ 12/02/2016 11 © NHS Bradford and Airedale Final sign-off (verification) of clinical competence You may sign off a student in three ways. The three options shown on each clinical competence evidence form are explained below. Option 1 Competent. You have observed the student undertaking appropriate activities relating to this outcome and are satisfied that they are competent within this area. Please note that competence should be assessed purely on the student’s ability as you record it from extensive and appropriate observation of them on placement. Following the course, continued competence will rely on the nature of the working arrangement within the healthcare network. Option 2 Requires an extension of time to become fully competent. This option should be used for students who are clearly capable, but who, through lack of opportunity or other mitigating circumstances, require more time to fulfil their learning outcomes adequately. This extension will be for 8 weeks in the first instance, but can be reviewed thereafter, as long as progress continues to be made. Option 3 Is not competent. This option should be used for students who have had sufficient opportunity to demonstrate clinical competence, but who have failed to do so within a certain element. Any student in this category will automatically receive 8 further weeks to redeem their situation. Thereafter they will be deemed to have failed the module. Please note: The participant passes or fails the course on the basis of your signature for each outcome. __________________________________ 12/02/2016 12 © NHS Bradford and Airedale What we can do for you Our support to you Please use this manual as guidance to assist you in making the training process smooth for both you and your student. If you have any questions or concerns please contact us. Problems which arise for the student which may affect their training, the fulfilment of competency criteria or their performance, should be addressed to the student first. Please take appropriate steps to avert or resolve the problem at this level. (You may wish to make a record of the issue for your final comment, if appropriate.) In the event that these issues cannot be resolved, or if serious concerns are raised eg. about professional misconduct or incompetent practice, please contact us. Contact details The Education Programmes Manager and the course tutors can be contacted in the first instance at psi@bradford.nhs.uk. All clinically based requests will be forwarded to the appropriate tutor. The postal address for course returns is: Education Programmes Manager, NHS Bradford and Airedale, Douglas Mill, Bowling Old Road, Bradford, BD5 7JR. Definitions The following terms are explained below: Competence: skill demonstrated by the participant in fulfilling a task effectively and safely Verification of competence: proof of the above skills, indicated by mentor signature Student: candidate who has been accepted onto the course Mentor: consultant specialist in local hospital Course Tutor: clinical tutor based in Bradford, responsible for the delivery of this module Education Programmes Manager Manager (Bradford) overseeing course delivery Preparation for clinical attachment Week 1 Weeks 1- 26 End of module Complete and send mentor agreement letter Set date for the week following your student’s clinical teaching session in Bradford to plan the training programme. Meet with student to plan the training programme (learning for the clinical competencies). Training fully underway. You will be contacted at weeks 8, 16 and 20 by email (as will the student) regarding progress Student completes evidence sheets for clinical competency sign off by Mentor __________________________________ 12/02/2016 13 © NHS Bradford and Airedale