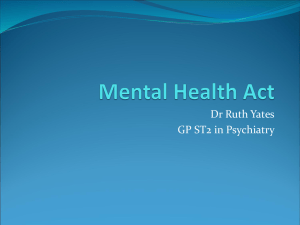
Hospital Managers` Handbook - Pennine Care NHS Foundation Trust
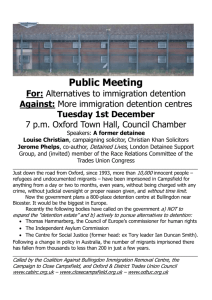
advertisement

Hospital Managers’ Handbook “It is the hospital managers who have the authority to detain patients under the Act. They have the primary responsibility for seeing that the requirements of the Act are followed. In particular, they must ensure that patients are detained only as the Act allows, that their treatment and care accord fully with its provisions, and that they are fully informed of, and are supported in exercising, their statutory rights.” Code of Practice (2008) Contents 1. Introduction 1 2. Principles of Mental Health 2.1 The Guiding Principles 2.2 The Human Rights Act 1998 2 3 3. Mental Health Act 1983 3.1 Informal Patients 3.2 Sections 4 4 4. Hospital Managers’ Hearings 4.1 When to Hold a Review 4.2 Prior to the Hearing 4.3 The Hearing 4.4 Procedure for Reviewing Detention or SCT 4.5 Criteria for the Decision 4.6 After the Hearing 11 11 13 15 16 17 5. Mental Health Review Tribunal 18 Appendixes Mental Health Act Team Contact Sheet Glossary – Key Words and Phrases Common Sections – Quick Reference Flowchart of Detention 19 20 36 37 1. Introduction The Mental Health Act 1983 (MHA) is the legislation that governs the formal detention, treatment and care of mentally disordered people in hospitals. The MHA has been amended by the Mental Health Act 2007. Pennine Care NHS Foundation Trust, in accordance with the MHA and the Code of Practice (Code) which offers guidance on how the Act should be applied, has appointed a Committee to undertake the duties required of ‘Hospital Managers’ within the meaning of the Act. The term ‘Hospital Managers’ refers to the Board of the NHS Trust with responsibility for detained patients. Legislation allows the Trust to establish a Committee comprising of Non-Executive Directors of the Trust and Associate Managers. The day-to-day duties are delegated to specific officers of the Trust, but only the Committee members are able to exercise the power of discharge. The terms Associate Managers or Managers throughout this handbook relates only to this Committee and not to the management team who work for Pennine Care. The Hospital Managers retain a responsibility for the performance of their delegated duties and as such must monitor and ensure these duties are carried out in accordance with the Act and good practice standards. Non-Executive Directors and Associate Managers are not personally liable for decisions taken about the discharge of detained patients; liability will rest with the Trust as a body. Pennine Care NHS Foundation Trust must ensure that the Committee is fully informed about the workings of the Act and the requirements placed on the Committee members both generally and specifically in relation to reviews of a patient’s detention. This handbook has been produced to assist Associate Managers with performing their duties and to act as a reference when carrying out review hearings with patients. This handbook should be read in conjunction with the Code and any other guidance that is provided. Training is available to the Hospital Managers and the information gained from this should also be considered additionally to the information contained within this handbook. Throughout this handbook we have included references, tips and further information in left hand margin which should assist and guide you. As the law changes constantly all reasonable efforts will be made to provide accurate and timely updates to this handbook. Page 1 2. Principles of Mental Health Section 118 of the Act While carrying out functions of the Act there are certain values and principles that must be considered and applied as far as possible. Chapter One of the Code 2.1 The Guiding Principles Before looking at the guiding principles in the Code it is useful to understand where the MHA, Code and Principles fit together. This can be summarised as follows; The MHA tells us what to do; The Code explains how to do it; and The Guiding Principles guide us in how to apply the MHA and Code in individual situations. The Code states that everyone who is working with the MHA must have regard to the guiding principles. As will become clear you may not be able to apply the guiding principles all the time but you should consider them when making decisions under the Act. The list of guiding principles that follows has been taken directly from Chapter 1 of the Code; Purpose Principle Decisions under the Act must be taken with a view to minimising the undesirable effects of mental disorder, by maximising the safety and wellbeing (mental and physical) of patients, promoting their recovery and protecting other people from harm Least Restriction Principle People taking action without a patient’s consent must attempt to keep to a minimum the restrictions they impose on the patient’s liberty, having regard to the purpose for which the restrictions are imposed. Respect Principle People taking decisions under the Act must recognise and respect the diverse needs, values and circumstances of each patient, including their race, religion, culture, gender, age, sexual orientation and any disability. They must consider the patient’s views, wishes and feelings (whether expressed at the time or in advance), so far as they are reasonably ascertainable, and follow those wishes wherever practicable and consistent with the purpose of the decision. There must be no unlawful discrimination Participation Principle Patients must be given the opportunity to be involved, as far as is practicable in the circumstances, in planning, developing and reviewing their own treatment and care to help ensure that it is delivered in a way that is as appropriate and effective for them as possible. The involvement of carers, family members and other Page 2 Para 1.7 Code, All decisions must, of course, be lawful and informed by good professional practice. Lawfulness necessarily includes compliance with the Human Rights Act 1998 people who have an interest in the patient’s welfare should be encouraged (unless there are particular reasons to the contrary) and their views taken seriously. These principles should inform your decisions not determine them. Through ongoing training and application Hospital Managers should be able to develop an ability to apply the principles as a whole and balance them dependent upon the decision to be made. 2.2 Human Rights Act 1998 (HRA) The Human Rights Act 1998 has been discussed with regard to the impact and duties it places on Hospitals and Hospital Managers. It should be noted that as long as they are working within the Code guidelines the requirements of the Human Rights Act are generally satisfied. A recognition of basic human rights should be achieved through the additional training but a brief explanation of the Articles most commonly associated with Mental Health are listed below for information; Article 2 - The Right to Life A person has the right to have their life protected by law. There are only certain very limited circumstances where it is acceptable for the state to take away someone’s life e.g. if a police officer acts justifiably in self defence. Article 3 - Protection from Torture and Inhuman and Degrading Treatment. A person has the absolute right not to be tortured or subjected to treatment or punishment, which is inhuman or degrading. Article 5 – Right to Liberty and Security A person has the right not to be deprived of their liberty – ‘arrested or detained’ – except in limited cases specified in the article (e.g where they are detained under the MHA) and provided there is a proper legal basis in UK law. This right has been central to many human rights based challenges brought by patients detained and treated under the Mental Health Act 1983. For further information on the HRA you may visit the Department of Constitutional Affairs website: http://www.dca.go v.uk/peoplesrights/humanrights/index.htm Article 8 - Right to a Private Life A person has the right to respect for their private and family life, their home and their correspondence. This right can be restricted only in specified circumstances. Page 3 3. Mental Health Act 1983 Para’s 4.9 – 4.24 of the Code 3.1 Informal Patients Hospital Managers do not conduct reviews of informal patients. MCA and DOLS are covered later in this handbook An informal patient can be a patient who has the capacity to consent to admission and does so or an incapacitated patient who lacks capacity to consent to admission and may be admitted using the Mental Capacity Act 2005 (MCA) and following April 2009, the Deprivation of Liberty Safeguards (DOLS). 3.2 Sections As the Hospital Managers carry out a high number of reviews across the Trust, the number and types of section they come across will vary. Although it would be impractical to list all sections within this handbook a brief guide to ‘common’ sections follows. Inpatient Sections Section 2 - Admission for Assessment This section lasts for up to 28 days and the criteria for detention is that the patient suffers from a mental disorder which warrants detention in hospital for assessment or assessment followed by treatment and that the patient needs to be detained in the interests of his own health or safety or for the protection of others. An Approved Mental Health Practitioner (AMHP) makes an application and two doctors need to complete medical recommendations (one must be section 12 approved) Patients may appeal to the Hospital Managers once at any time during the 28 days but they must appeal within the first 14 days to the Mental Health Review Tribunal. S.12 means the Doctor has undergone additional training in identifying mental disorder Section 3 – Admission for Treatment This admission is for up to 6 months which is then renewable initially for a further 6 months followed by periods of one year at a time for treatment of patient suffering from mental disorder that makes it appropriate for him to receive treatment in a hospital. It must also be necessary for the health and safety of the patient or for the protection of other persons that he should receive treatment and that appropriate treatment is available for him. An Approved Mental Health Practitioner (AMHP) makes an application and two doctors need to complete medical recommendations (one must be section 12 approved) Patients may appeal to the Hospital Managers at any time during the period of detention but they can only appeal once in each period of detention to the Mental Health Review Tribunal. Where the patient has recently had a hearing (either MHRT or Managers) the Associate Managers’ may refuse to consider his case if there hasn’t Page 4 been a significant change in his circumstances or condition. This prevents unnecessary hearings which may distress the patient and impact on those involved in their care. The Trust requires a Non-Executive Director to make the decision as to whether or not a hearing is held. Section 37 – Hospital Order Patient is sent to hospital by the courts following sentencing for a criminal offence. The criteria and the resulting admission work in the same way as a section 3 except for the appeal process. A s.37 patient cannot appeal to the MHRT in the first six months of a detention but can still appeal to the Hospital Managers. Section 4 – Emergency Admission for Assessment Admission for assessment in cases of emergency. This section lasts for a maximum of 72 hours and application is by an AMHP with recommendation by one doctor. The doctor must confirm that it is of urgent necessity for the patient to be admitted and that waiting for a second doctor would cause ‘undesirable delay’. There are no rights of appeal on these sections and their treatment is not covered by Part 4 of the MHA. Patients detained under section 4 CAN submit an appeal that would be heard upon conversion to a longer term detention Section 5(2) – Emergency Inpatient Doctors Holding Power Allows for patients already in hospital to be held for up to 72 hours by a doctor. Section 5(4) – Emergency Inpatient Nurses Holding Power Allows patient to be detained for up to 6 hours (by a nurse) to allow for the arrival of a doctor to carry out an assessment Section 135 (1) – Warrant to Search and Remove Allows that where there is reason to suspect that a person is suffering from a mental disorder and is: a. Being ill treated, neglected or not kept under proper control or b. Is unable to care for her or himself and lives alone an AMHP can apply to a magistrate for a warrant authorising a police officer with a doctor and an AMHP to enter any premises and remove the person to a place of safety. Once removed to a place of safety that person may be detained there for a period of up to 72 hours Section 135 (2) – Warrant to Retake an AWOL Patient Allows for the retaking of a detained patient, who is absent without leave, by forced entry if necessary to any premises where the patient is located and entry has been refused. Section 136 – Police Power to Detain Under this section if a police officer believes that a person in a public place is ‘suffering from mental disorder’ and is in ‘immediate need of care or control’ the police officer can take that person to a ‘place of safety’ for a maximum of 72 hours so that the person can be examined by a doctor and interviewed by an AMHP and any necessary arrangements made for the person’s treatment or care. Page 5 Community Sections s.17A was introduced by the Mental Health Act 2007 and replaces Supervised Discharge Section 17A – Supervised Community Treatment (SCT) Patients who have been detained under an unrestricted treatment section can be discharged into the community on a s.17A. This means a patient suffering from a mental disorder can live in the community whilst still subject to powers under the MHA. Patients on SCT are subject to a Community Treatment Order (CTO) which sets out conditions the patient is asked to keep to in order to ensure they receive the treatment they need. Applications are made by the patient’s Responsible Clinician and have to be approved by an AMHP. We will cover this Section in more detail later in the handbook (See Page 9). Section 7 – Guardianship For patients in the community guardianship allows their Responsible Clinician and other professionals to specify their place of residence. Initially for six months and then renewed for six months by the Responsible Clinician and yearly after that. The Local Authority manages the detention rather than Pennine Care. Other Sections / Status Part 4 - Treatment Part 4 of the Act allows some detained patients to be compulsorily treated if necessary. The emergency or short term sections are not subject to this. Chapter 23 of the Code Only treatment for mental disorder can be given using this part of the Act. Treatment may be given for the first three month period of detention and following this may only be given with the patients consent or second opinion. Part 4A – Treatment of a Community Patient (SCT) Part 4A provides authority to treat a community patient without their consent. S.64A – 64K authorise ‘relevant treatment’ to be given to a community patient who has not been recalled. This treatment may only be given if; The treatment is immediately necessary and the patient is capable and consents The treatment is immediately necessary and there is consent from someone authorized under the MCA to make decisions on the patients behalf The patient lacks capacity and force is not necessary to secure compliance Page 6 Emergency treatment needs to be given using force if necessary, to a patient who lacks capacity This treatment can only be provided where a Second Opinion Appointed Doctor (SOAD) has issued a certificate authorising the treatment. Section 17 – Leave of Absence Under section 17 of the Act, the Responsible Clinician may grant leave to the patient, subject to any conditions, which the Responsible Clinician considers necessary in the interests of the patient or the protection of other persons. Only the Responsible Clinician may grant leave. Section 20 – Renewal Sections 3, 37, 17A and 47 require the Responsible Clinician to complete a renewal form before the expiry of the section. This allows for the section to continue for a further period of either six or twelve months, dependent upon the length of time they have already been detained. Once a form has been completed the Hospital Managers are then obliged to review the continued detention. It is good practice for the review hearing to take place before the section expires but it may also take place following the expiry date. Section 18 – Absent Without Leave (AWOL) If a patient takes leave of absence from the hospital without a section 17 authorising this then the patient is classed as AWOL. If a SCT patient is recalled to hospital and does not return they are also classed as AWOL. Section 23 – Discharge Sections can be ended in a number of ways including Responsible Clinician discharges the patient before the end of the section Mental Health Review Tribunal discharges patient following review Hospital Managers discharge patient following review Nearest Relative discharges the patient Section 117- Aftercare It is the duty of the health authority & local social services to provide, in cooperation with relevant voluntary organisations and aftercare services. It is important that all patients who are subject to S117 are identified & records kept of them. Those subject to S117 are patients on (or have been on) S3, S37, S17A, S41, S47 & S48. Page 7 We will now expand on particular elements of the MHA which require further explanation and consideration. Chapter 3 of the Code Mental Disorder There is one broad definition of Mental Disorder within the meaning of the MHA which is ‘any disorder or disability of mind’. This applies to all sections. Where a patient has a learning disability, this must also be associated with abnormally aggressive or seriously irresponsible conduct to meet the criteria. Dependence upon alcohol or drugs is excluded and can not be considered a disorder or disability of mind. Chapter 6 of the Code Appropriate Treatment Test When a patient has been detained under a treatment section of the MHA there must be appropriate medical treatment available for their mental disorder. This is to ensure no-one is detained unless they are actually to be offered treatment for their mental disorder. Medical treatment for mental disorder means medical treatment for the purpose of alleviating, or preventing a worsening of, a mental disorder or one or more of its symptoms or manifestations Medical treatment also includes nursing, psychological intervention and specialist mental health habilitation, rehabilitation and care. ‘The appropriate medical treatment test requires a judgement about whether an appropriate package of treatment for mental disorder is available for the individual in question. Where the appropriate medical treatment test forms part of the criteria for detention, the medical treatment in question is treatment for mental disorder in the hospital in which the patient is to be detained. Where it is part of the criteria for SCT it refers to the treatment for mental disorder that the person will be offered while on SCT.’ (Para 6.9 Code) Supervised Community Treatment (SCT) As stated earlier this allows a patient to receive the care and treatment they need for their mental disorder in the community rather than in hospital. To be eligible for SCT the patient must have been detained on one of the treatment sections when the application for the CTO was made. Each time a period of Section 17 leave is granted to a detained patient for more than seven consecutive days, their Responsible Clinician must consider whether it would be appropriate for the patient to be on SCT rather than an inpatient. The patients Responsible Clinician may specify conditions to be applied by the CTO. The only limitation on these conditions is that they are ‘necessary or appropriate’ for; Page 8 Ensuring the patient receives medical treatment Preventing the risk of harm to the patient’s health or safety Protecting other persons Once on a SCT the patient may be recalled to the hospital for up to 72 hours or the CTO can be revoked and the patient would revert to the section he was on immediately prior to discharge. The Responsible Clinician can recall the patient if he is of the opinion; Chapter 8 of the Code The patient requires medical treatment in hospital for his mental disorder; and There would be a risk of harm to the health and safety of the patient or to other persons if the patient were not recalled to hospital for that purpose. Nearest Relative Unlike a persons next of kin, which is chosen by the patient, the Nearest Relative (NR) is defined by the MHA. Identifying a person’s NR can be a complex task and is generally carried out by an AMHP upon a patients admission to hospital. In s.26 of the MHA there is a hierarchy as follows; Husband, wife or civil partner Son or Daughter Father or Mother Brother or Sister Grandparent Grandchild Uncle or Aunt Nephew or Niece If there is no-one in the first category then you move to the next but if there is more than one person in a category then you would use the eldest. The NR must also be living in the United Kingdom. The first category includes people living with a patient as though they are a couple for over 6 months If anyone on the list is living with the patient or is a carer, they are the NR. If anyone is not on the list but they have lived with them for five years or more, they are the NR. If no one qualifies as a NR, the Court can appoint someone to act as NR. The MHA confers various rights and powers on a patient’s nearest relative in connection with detention, Supervised Community Treatment and Guardianship under the MHA. These include the right to: Apply for detention or Guardianship; Object to Approved Mental Health Professionals making applications for admission to hospital for treatment or for Guardianship; Page 9 Ask that their relative be assessed under the MHA, and receive written information if the decision is taken not to admit that person; and Discharge the patient (with various exceptions) or (in certain cases) to apply to the Mental Health Review Tribunal (MHRT) instead. Nearest relatives are also entitled to be given information in respect of patients in a variety of circumstances. They therefore provide a significant protection for people who experience mental distress – both in terms of helping them to get help when they need it and in being able to question and prevent the use of compulsion if it is not truly necessary. Due to the prescriptive nature of the hierarchy list there will be occasions where the NR identified is not suitable to act as such. In this event they can be displaced by a court. There are a number of people who can apply to court to displace a nearest relative: The patient Any relative of the patient Anyone who lives with the patient An AMHP If a patient or someone else wishes to make an application to the County Court for an order to displace their nearest relative, they may do so on a number of grounds: 1. That there is no nearest relative; 2. That the nearest relative is too ill to take on the role; 3. That the nearest relative has objected unreasonably to admission; 4. That the nearest relative has discharged the patient without regard to that person (or other people’s) safety; 5. That the nearest relative is ‘otherwise unsuitable’. The court will decide what constitutes ‘suitability’ but factors may include where the patient is known to have suffered abuse, is scared or is unknown to the person identified. Page 10 4 Hospital Managers Hearings 4.1 When to Hold a Review Section 132 of the MHA Chapter 2 of the Code Chapter 31 of the Code The reviews of a patient’s detention, carried out by a panel of three Hospital Managers can be described as a `review’, a `panel’ or a `hearing’. Hospital Managers have a duty to ensure that all patients are aware that they may seek discharge by the Hospital Managers and of the distinction between this and their right to a Mental Health Review Tribunal hearing (See 4.2). The delegated officers such as the Mental Health Act Administrators or nursing staff usually carry out this duty on behalf of the Hospital Manager’s. Hospital managers: May undertake a review of whether or not a patient should be discharged at any time at their discretion; Must undertake a review if the patient’s responsible clinician submits to them a report under section 20 of the Act renewing detention or under section 20A extending SCT; Should consider holding a review when they receive a request from (or on behalf of) a patient; and Should consider holding a review when the responsible clinician makes a report to them under section 25 barring an order by the nearest relative to discharge a patient. In the last two cases, when deciding whether to consider the case, managers’ panels are entitled to take into account whether the Tribunal has recently considered the patient’s case or is due to do so in the near future. In the Trust all contested renewals take place through the full hearings process. In the event of an uncontested renewal under section 20, patients should be interviewed by at least one member of the managers’ panel considering their case, if they request it, or if the panel thinks it desirable after reading the renewal or extension report. 4.2 Prior to the hearing: With the assistance of the Mental Health Act Office, the Hospital Managers should ensure that they have reports from the patient's Responsible Clinician and other relevant disciplines; Page 11 Para 2.31 of the Code Written reports should be accompanied by documentation compiled under the Care Programme Approach (or its equivalent). that, if the patient consents, his or her nearest relative (as defined by the Act) and/or most concerned relatives are informed of the review and asked to comment or to be in attendance. that, if the patient withholds consent to attendance of his/her nearest relative at the hearing, the appropriate professional concerned with the patient's care obtains the views of the patient's nearest relative and/or most concerned relatives and includes these in his or her report. This is also dependent upon the consent of the patient. The Mental Health Act Office will also: Para 31.26 of the Code identify panel members and select a chairperson from the approved list, paying due attention to the gender and ethnicity and other needs of the patient, and set a time for the hearing with the panel; organise legal representation on behalf of the patient, if so requested; Where the patient is on SCT consider the most appropriate location for the hearing, as the hospital may not be convenient or acceptable to the patient explain the procedure to the patient and his or her legal representative; ascertain whether the patient wishes a relative or friend to attend the hearing; inform the patient and (where appropriate) his or her friend/relative/legal representative of the date, time and venue of the hearing; inform relevant professional staff of the date, time and venue of the hearing; ensure that all reports are circulated to the patient and his or her friend/relative/legal adviser as appropriate (other than in exceptional circumstances where elements of the report may be withheld) In circumstances where reports are unavailable in the days prior to the hearing, ensure that reports are made available Page 12 to all parties at least one hour prior to the scheduled time of hearing. In most cases, the panel members attend 30 minutes prior to a hearing commencing and therefore the reports will be ready for their arrival. 4.3 The Hearing 4.3.1 The Review Panel Before the start of a meeting, each Manager should receive papers to be discussed. The review will be conducted by a Review Panel of three Hospital Managers, and where possible selected to provide a balance of experience, gender and ethnicity with regard to the patient concerned. The MHA Administrator will select the Chairperson (normally a NonExecutive Director) in advance of the hearing and will communicate the identity of the Chair to the other panel members. On the day of the hearing, another Panel member may be selected to be Chair if the Panel judges this to be in the best interest of the patient. 4.3.2 The Role of the Chair During the hearing, the Chair's role is to encourage comprehensive questioning and to ensure that each panel member has fully participated in discussion and the decision-making process. The Chair is also responsible for ensuring the decision is fully documented and given to the Mental Health Act Office. 4.3.3 Professional attendance and postponement of hearings It is desirable for the Responsible Clinician to be present but, if absence is unavoidable, a representative doctor will be asked to attend in place of the Responsible Clinician. Where appropriate staff are not present and/or up-to-date reports are missing, the Managers must consider whether or not they have sufficient available information in order to make an informed decision. In such circumstances, it may be necessary, in consultation with the patient and/or their legal representative and/or advocate, to postpone the hearing due to insufficient information being available. The Managers are able to receive verbal evidence in the absence of a written report or to provide an update if the report was written some time before the hearing. 4.3.4 Mental Health Act Administrator Attendance Page 13 It has been agreed that the Mental Health Act Administrator will not be present during the hearing unless requested by the panel or the patient. They will however be available during the hearing if required. Legal advice should be obtained in the first instance through the Mental Health Act Office who are able to escalate the issue to the Mental Health Law Coordinator 4.3.5 Opportunity for Private Consultation with the Panel The Chairperson should check whether the patient wishes to speak privately with the panel either at the beginning or at the end of the hearing. The patient and other parties to the review will normally be able to hear each other's statements to the Panel and to put questions to each other. However, the patient should always be offered the opportunity of speaking alone with the Panel. 4.3.6 Order of proceedings At the start of the hearing, the Chairperson should state clearly the order of proceedings, which should normally be as follows: introduce all those in attendance; state clearly the purpose of the hearing and the order of proceedings (to help focus the discussion and set the agenda); ask the Responsible Clinician and other professionals to give their views on whether the patient's continued detention or SCT is justified and the factors on which those views are based; give the patient the opportunity and any necessary help to comment on the views expressed, either personally, or through his/her advocate or solicitor if appointed; after each presentation, seek clarification or any further information. Provide the patient and/or his or her advocate or relative the opportunity to ask questions; if the patient agrees, the patient's representative or relative should be asked if they wish to make a statement and the Panel may seek clarification or any further information; the advocate or solicitor should be given the opportunity to ask the patient any questions and the patient the opportunity to respond; the patient and/or his or her advocate should have the opportunity of summarising the case for discharge in the light of the evidence presented. The Panel should bear in mind that: the hearing is likely to be stressful for the patient. The Panel should therefore balance the formality necessary to carry out their tasks with informality in the interest of supporting the patient; Page 14 they should assist, in so far as possible, the patient in making his or her case for discharge effectively where they do not have a representative; there is no set time for the length of a hearing. However, the Panel should consider the effect of a lengthy review on the patient's wellbeing; if the patient becomes distressed, a short break may be directed by the Chairperson; If the patient chooses to absent himself or herself from the hearing, the Panel should decide whether to continue with the hearing. The procedures for the hearing should be informal. For example, hearsay evidence may be accepted but should where possible be substantiated. Although all parties should be actively and positively questioned, formal cross-examination should be avoided. The questions should be asked of all parties in a manner which is thorough, fair and courteous. Care should be given not to undermine the patient's relationship with his or her family and with professional staff; Subject to the patient's right to object to the presence of relatives, all parties should normally be present throughout the hearing except: during any time when the patient wishes to speak to the Panel alone (usually at the beginning or end of the hearing); when the patient does not wish to be present. 4.4 Procedure for Reviewing Detention or SCT In exercising the powers of discharge, the Hospital Managers must act in a way that is fair, reasonable and lawful, giving due consideration to the various reports and recommendations made, but not being bound by such reports and recommendations. Managers' power to discharge a detained patient can be exercised only when all three members of the panel are in favour of discharge otherwise the decision will be unlawful. In cases where Managers uphold a patient's continued detention they must ensure that the patient and the patients’ nearest relative (where the patient consents to them being told) are fully informed of the reasons for this decision in line with guidance given in the Code and Article 5(2) of the Human Rights Act 1998. Managers have a responsibility to always ensure that full and comprehensive reasons for decisions are clearly recorded on the Managers’ Hearing Decision form. Page 15 Reasons for and decisions reached should not be irrational or appear that no other managers panel properly directing itself as to the law and on the available information, could have made. In the event that a legal challenge to a decision to continue detention arises, the information will facilitate a response. In this situation, the following actions should be taken: In collaboration with the Managers, the Administrator would write to the patient's solicitor (if appointed) giving a clear account of the reasons for the continued detention; Copies of relevant supporting documentation should accompany the letter in the event that the patient's solicitor continues to challenge the decision. Further advice must be obtained from the Trust's solicitors through the normal legal process of the Trust. 4.5 Criteria for the decision The MHA does not provide specific discharge criteria for the Hospital Managers to apply. Although the Code does offer guidance on this matter as follows; Hospital Managers should consider whether the grounds for continued detention or continued SCT under the Act are satisfied. To ensure that this is done in a systematic and consistent way, managers’ panels should consider the questions set out below, in the order stated. For patients detained for assessment under section 2 of the Act: Is the patient still suffering from mental disorder? If so, is the disorder of a nature or degree which warrants the continued detention of the patient in hospital? Ought the detention to continue in the interests of the patient’s health or safety or for the protection of other people? For other detained inpatients: Is the patient still suffering from mental disorder? If so, is the disorder of a nature or degree which makes treatment in a hospital appropriate? Is continued detention for medical treatment necessary for the patient’s health or safety or for the protection of other people? Is appropriate medical treatment available for the patient? For patients on SCT: Is the patient still suffering from mental disorder? Page 16 Dangerous is equal to the probability of dangerous acts, such as causing serious physical injury or lasting psychological harm, not merely on the patient’s general need for safety and others’ general need for protection If so, is the disorder of a nature or degree which makes it appropriate for the patient to receive medical treatment? If so, is it necessary in the interests of the patient’s health or safety or the protection of other people that the patient should receive such treatment? Is it still necessary for the responsible clinician to be able to exercise the power to recall the patient to hospital, if that is needed? Is appropriate medical treatment available for the patient? Where the answer to all the relevant questions above is “yes”, but the responsible clinician has made a report under section 25 barring a nearest relative’s attempt to discharge the patient, the managers should also consider the following question: Would the patient, if discharged, be likely to act in a manner that is dangerous to other people or to themselves? If the panel is satisfied from the evidence presented to them that the answer to any of these questions (except the Section 25 question) is "no", the patient should be discharged, providing there is evidence that adequate care would be in place. If it is not in place and its absence makes it likely that the patient's health or safety will be compromised, the panel have the powers to either adjourn the hearing or to defer discharge for a reasonable specified period to allow for care arrangements to be in place. The hospital managers do retain a residual discretion not to discharge in these cases, so panels should always consider whether there are exceptional reasons why the patient should not be discharged. Hospital Managers involved in these cases should ensure the reasons are well documented, guiding principles are applied and the MHA Office must be immediately informed. In all cases, hospital managers have discretion to discharge patients even if the criteria for continued detention or SCT are met. Managers’ panels must therefore always consider whether there are other reasons why the patient should be discharged despite the answers to the questions set out above. This must be well documented and the MHA Office must be immediately informed. 4.6 After the Hearing 4.6.1 Informing the patient of the Hospital Managers' Decision In communicating their decision, the Panel should ensure that: Their decision and the reasons for it are communicated immediately to the patient, to any relative who has been involved and to the relevant professionals; Page 17 Wherever possible, at least one member of the Panel explains to the patient in person the reason for the decision. But if the patient is unavailable or unwilling to meet with a panel member, the reason for the decision should be communicated by their advocate or a member of the professional staff; 5 Mental Health Review Tribunal The MHRT is the statutory, independent body responsible for hearing appeals against detention. It operates like a mobile court and sits in the hospital where the patient is detained. An MHRT will consist of a lawyer, a doctor and a lay member. The patient, their hospital doctor and social worker will also be at the hearing together with the patient's nearest relative, unless the patient objects. The legal member will chair the proceedings. Patients detained under section 2 of the MHA who wish to appeal to an MHRT must do so within 14 days of the start of their detention. If between making the appeal and the hearing the patient is transferred to a section 3, the MHRT will still hear the original appeal and it will not affect the patient's right to appeal under section 3. Patients detained under section 3 of the Mental Health Act may appeal to an MHRT once in a 6 month period. Patients under section 37 can only apply to an MHRT after the first 6 months. Thereafter, their rights of appeal are the same as for section 3 patients. Some patients have to have their cases referred by the Hospital Managers to an MHRT even though they have not asked for an appeal. These include patients detained under section 3 or SCT who have not been to an MHRT within the last 6 months and in the case of SCT did not appeal during their detention under section 3. Patients who have had their detention or SCT renewed and have not appealed to an MHRT in the last 3 years (if aged 18 years or over) or the last 1 year (if aged less than 18 years) will also be automatically referred. For patients detained under section 2 the hearing must take place within 7 days of the MHRT office receiving the application. For patients detained under section 3 the hearing will normally take place within 8 weeks. For restricted patients (sections with restrictions include s.37/41 or 48/49) the hearing will normally take place within 20 weeks. The MHRT's principal powers are: to discharge a detained patient from hospital immediately or after a short further period of detention. to recommend leave of absence to recommend SCT to recommend transfer to another hospital Page 18 Mental Health Act Team 1. Trust: Kim Shepherd Mental Health Law Manager Trust Headquarters St Petersfield 225 Old Street Ashton Under Lyne OL6 7SR Tel: 0161 604 3008 2. Bury: Lisa West / Carolyn Davis Roch House Fairfield General Hospital Rochdale Old Road Bury BL9 7TD Tel: 0161 778 3681 3. Oldham: Pam Smith / Gemma Scholes Parklands House Royal Oldham Hospital Rochdale Road Oldham OL1 2JH Tel: 0161 778 5753 4. Rochdale: Diane Birchall / Gemma Scholes Borough Mental Health Offices Birch Hill Hospital Littleborough Rochdale OL12 9QB Tel: 01706 754621 5. Stockport: Debbie Arrell Psychiatry Administration Department Stepping Hill Hospital Poplar Grove Stockport SK2 7JE Tel: 0161 419 5349 6. Tameside: Mia Majid / Jean Milhench Mental Health Unit Tameside General Hospital Fountain Street Ashton-under-Lyne OL6 9RW Tel: 0161 604 3777 6. Rehab: Luci Lewis / Jan Broomhead Mental Health Unit Tameside General Hospital Fountain Street Ashton-under-Lyne OL6 9RW Tel: 0161 604 3789 Page 19 Email addresses are firstname.surname@nhs.net Page 20 Glossary Key words and phrases Taken from the Code & MIND A Absent Without Leave (AWOL) When a detained patient leaves hospital without getting permission first or does not return to hospital when required to do so. Also applies to guardianship patients who leave the place their guardian says they should live and to SCT patients and conditionally discharged restricted patients who don’t return to hospital when recalled, or who leave the hospital without permission after they have been recalled. The Act Unless otherwise stated, the Mental Health Act 1983 (as amended by the Mental Health Act 2007). Advance Decision to Refuse Treatment A decision, under the Mental Capacity Act, to refuse specified treatment made in advance by a person who has capacity to do so. This decision will then apply at a future time when that person lacks capacity to consent to, or refuse the specified treatment. Advocacy Independent help and support with understanding issues and assistance in putting forward one’s own views, feelings and ideas. See also Independent mental health advocate. After-care Community care services following discharge from hospital; especially the duty of health and social services to provide after-care under section 117 of the Act, following the discharge of a patient from detention for treatment under the Act. The duty applies to SCT patients and conditionally discharged restricted patients, as well as those who have been fully discharged. Application An application made by an approved mental health professional, for detention or a nearest relative, under Part 2 of the Act for a patient to be detained in a hospital either for assessment or for medical treatment. Applications may be made under section 2 (application for admission for assessment), section 3 (application for admission for medical treatment) or section 4 (emergency application for admission for assessment). Appropriate Medical Treatment Medical treatment for mental disorder which is appropriate taking into account the nature and degree of the person’s mental disorder and all the other circumstances of their case. Appropriate Medical Treatment Test The requirement in some of the criteria for detention, and in the criteria for SCT, that appropriate medical treatment must be available for the patient. Approved Clinician A mental health professional approved by the Secretary of State (or the Welsh Ministers) to act as an approved clinician for the purposes of the Act. Some decisions under the Act can only be taken by people who are approved clinicians. All responsible clinicians must be approved clinicians. Approved Mental Health Practitioner A social worker or other professional approved by a local social services authority (LSSA) to carry out a variety of functions under the Act. Page 21 Assessment Examining a patient to establish whether the patient has a mental disorder and, if they do, what treatment and care they need. It is also used to be mean examining or interviewing a patient to decide whether an application for detention or a guardianship application should be made. Attorney Someone appointed under the Mental Capacity Act who has the legal right to make decisions (eg decisions about treatment) within the scope of their authority on behalf of the person (the donor) who made the power of attorney. Also known as a “donee of lasting power of attorney”. Acute Confusional state: A sudden & rapid onset of confusion, of an alarmingly high level, usually a symptom of an acute physical illness. The duration can be short & the cause treated. Affect: A subjective interpretation of the feelings accompanying an idea or image. Similar in meaning to ‘mood’, it can be defined as a state of emotional tone or feeling which can fluctuate through a range of depression & elation. Affective disorder: Disorder of mood including the commoner disturbances in emotional equilibrium that may form part of an overall clinical picture in mental disorder; depression, anxiety, incongruity and blunting of affect, la belle indifference, lability, hostility, depersonalisation. There may be difficulty in differentiating the symptoms of major affective disorder from an environmental causation or organic illness, therefore careful assessment & history taking is particularly important. Akathisia: A motor restlessness ranging from a feeling of inner disquiet, often localised in the muscles, to an inability to sit still or lie quietly; a side effect of some antipsychotic drugs. Antecedent: The stimulus or cue that occurs before behaviour that leads to occurrence. Antisocial personality disorder: A disorder occurring in adult patients with a history of conduct disorder; behaviour which is often characterised by poor work record, disregard for social norms, aggressiveness, financial irresponsibility, impulsiveness, lying, recklessness, inability to maintain close relationships or to meet responsibilities for significant others & a lack of remorse for harmful behaviour. Anxiety: A diffuse apprehension vague in nature & associated with feelings of uncertainty & helplessness. It is an emotion without a specific object, is subjectively experienced by the individual & is communicated interpersonally. It occurs as a result of a threat to the person’s being, self-esteem or identity. Apathy: Lack of feelings, emotions, interests or concern. Automatic thoughts: These are contained in a stream of thoughts which are usually going on in a individual’s head. They effect the person’s feelings and inform their behaviour, but often occur without the person being aware of them. It is only when individuals are asked to focus in on their unreported thoughts that they become aware of them Page 22 B Bipolar affective disorder: A sub-group of the affective disorders charcterised by at least an episode of manic behaviour, with or without a history of episodes of depression. Also known as manic depression Borderline personality disorder: A specific personality disorder with the essential features of unstable mood, interpersonal relationships & self image; characteristic behaviours may include unstable relationships, exploitation of others, impulsive behaviour, labile effect, problems expressing anger appropriately, self-destructive behaviour & identity disturbances. C Capacity The ability to take a decision about a particular matter at the time the decision needs to be made. Some people may lack capacity to take a particular decision (eg to consent to treatment) because they cannot understand, retain, use or weigh the information relevant to the decision. A legal definition of lack of capacity for people aged 16 or over is set out in section 2 of the Mental Capacity Act 2005. See also competence to consent. Care Programme Approach (CPA) A system of care and support for individuals with complex needs which includes an assessment, a care plan and a care coordinator. It is used mainly for adults in England who receive specialist mental healthcare and in some CAMHS services. There are similar systems for supporting other groups of individuals, including children and young people (Children’s Assessment Framework), older adults (Single Assessment Process) and people with learning disabilities (Person Centred Planning). Carer Someone who provides voluntary care by looking after and assisting a family member, friend or neighbour who requires support because of their mental health needs. Child (and children) A person under the age of 16. Child and adolescent mental health services (CAMHS) Specialist mental health services for children and adolescents. Over all types of provision and intervention – from mental health promotion and primary prevention and specialist community-based services through to very specialist care, as provided by in-patient units for children and young people with mental illness. They are mainly composed of a multi-disciplinary workforce with specialist training in child and adolescent mental health. Children Act 1989 A law relating to children and young people and those with parental responsibility for them. Commission The independent body which is responsible for monitoring the operation of the Act. At the time of publication, this is the Mental Health Act Commission (MHAC). However, legislation is currently before Parliament which will abolish the MHAC and transfer its functions to a new body, the Care Quality Commission, which is to establish a new integrated health and adult social care regulator, bringing together existing health and social care regulators into one regulatory body. Subject to Parliament, it is expected that the new Commission will be established in April 2009. Page 23 Community treatment order (CTO) Written authorisation on a statutory form for the discharge of a patient from detention in hospital onto supervised community treatment. Competence Similar to capacity to consent, but specifically about children. As well to consent as covering a child’s inability to make particular decisions because of their mental condition, it also covers children who do not have the maturity to take the particular decision in question. Compulsory Things that can be done to people under the Act without their measures agreement. This includes detention in hospital, supervised ommunity treatment and guardianship. Compulsory Medical Treatment: Treatment for mental disorder given under the Act against the wishes of the patient. Conditional discharge: from hospital by the Secretary of State for Justice or the Tribunal of a restricted patient subject to conditions. The patient remains subject to recall to hospital by the Secretary of State. Conditionally Discharged Restricted Patient: A restricted patient who has been given a conditional discharge. Consent Agreeing to allow someone else to do something to or for you. Particularly consent to treatment. Valid consent requires that the person has the capacity to make the decision (or the competence to consent, if a child), and they are given the information they need to make the decision, and that they are not under any duress or inappropriate pressure. Convey (and Conveyance) Transporting a patient under the Act to hospital (or anywhere else), compulsorily if necessary. Court of Protection The specialist court set up under the Mental Capacity Act to deal with all issues relating to people who lack capacity to take decisions for themselves. Criteria for detention: A set of criteria that must be met before a person can be detained, or remain detained, under the Act. The criteria are different in different sections of the Act. Criteria for SCT Patient A set of criteria that must be met before a person can become an SCT or remain an SCT patient. Criminal Records An Executive Agency of the Home Office, which provides access to criminal record information through its disclosure service. Capacity: In order to have ‘capacity’ a person must understand what the medical treatment is & why it is proposed in his/her instance. Catatonia: A syndrome of motor abnormalities occurring in schizophrenia and (less commonly) in organic cerebral disease, characterised by stupor and the adoption of strange postures or outbursts of excitement & hyperactivity. Rarely reported nowadays. Page 24 Chronic confusional state: A slow & insidious onset of confusion, which is likely to go unnoticed. It is a symptom of chronic physical illness such as thyroid gland underactivity. May occur over a period of years but can be reversed with treatment. Cognitive disorder: Disorder associated with the way in which the individual interprets the world. The underlying thought processes are seen as instrumental in determining how a person behaves & their emotional reactions. Cognitive disturbance: A self defeating attitude or responses which may become habitual particularly directed towards lowered self esteem. Compulsion: A recurring irresistible impulse to perform some act. Concreteness: Use of specific terminology rather than abstraction by the patient in describing feelings, experiences & behaviour. Confabulation: Asked what they had for breakfast that morning or for details of past psychiatric history, patients will tell amore or less plausible story that is completely invented. Congruent communication: A communication pattern in which the sender is communicating the same message on both verbal & non-verbal levels. D Deprivation of liberty A term used in Article 5 of the European Convention on Human Rights (ECHR) to mean the circumstances in which a person’s freedom is taken away. Its meaning in practice has been developed through case law. Deprivation of liberty Safeguards (DOLS) The framework of safeguards under the Mental Capacity Act (as amended by the Mental Health Act 2007) for people who need to be deprived of their liberty in their best interests for care or treatment to which they lack the capacity to consent themselves. Deputy (or Court appointed deputy) A person appointed by the Court of Protection under section 16 - of the Mental Capacity Act to take specified decisions on behalf of someone who lacks capacity to take those decisions themselves. This is not the same thing as the nominated deputy sometimes appointed by the doctor or approved clinician in charge of a patient’s treatment. Detained Patient: Unless otherwise stated, a patient who is detained in hospital under the Act, or who is liable to be detained in hospital but who is (for any reason) currently out of hospital. Detention (and detained) Unless otherwise stated, being held compulsorily in hospital under the Act for a period of assessment or medical treatment. Sometimes referred to colloquially as “sectioning”. Detention For Assessment The detention of a person in order to carry out an Can normally only last for a maximum of 28 days. Also known as “section 2 detention”. Detention for Medical Treatment The detention of a person in order to give them the medical treatment for mental disorder they need. There are various types of detention for medical treatment in the Act. It most often means detention as a (and Page 25 result of an application for detention under section 3 of the Act. But it also includes several types of detention under Part 3 of the Act, including hospital directions, hospital orders and interim hospital orders. Diagnostic Over-Shadowing A risk for everyone with a mental disorder, but a particular danger for people with learning disabilities, that behavioural problems may be misinterpreted as symptomatic of mental disorder when they are in fact a sign of an underlying physical health problem. Discharge Unless otherwise stated, a decision that a patient should no longer be subject to detention, supervised community treatment, guardianship or conditional discharge. Discharge from detention is not the same as being discharged from hospital. The patient might already have left hospital on leave of absence, or might agree to remain in hospital as an informal patient. Displacement (Of Nearest Relative) The provision under section 29 of the Act, under which the county court can order that the functions of the nearest relative be carried out by another person or by a local social services authority. Doctor A registered medical practitioner. Doctor Approved Under Section 12 A doctor who has been approved by the Secretary of State (or the Welsh Ministers) under the Act as having special experience in the diagnosis or treatment of mental disorder. In practice, strategic health authorities take these decisions on behalf of the Secretary of State in England. Some medical recommendations and medical evidence to courts under the Act can only be made by a doctor who is approved under section 12. (Doctors who are approved clinicians are automatically treated as though they have been approved under section 12.) Dangerousness: The probability that an individual will commit an act of violence on another person, in the near or distant future, if afforded the opportunity to do so. Delirium tremens: Associated with alcohol dependency & occurs about 24 hours after withdrawal. Characterised by tremor, restlessness, disorientation, visual hallucinations, autonomic arousal & occasionally fits. Delusions: A false belief that is firmly held even though it is not shared by others & is contradicted by social reality. Dementia: A progressive organic mental disorder resulting in a lowering of the usual level of mental ability. Alzheimer’s disease is most common (80% cases) but is also caused by Huntington’s disease, Pick’s disease, Creutzfeld-Jakob disease (CJD), long term alcohol/drug abuse, stroke, Parkinson’s disease, meningitis, syphilis, HIV/AIDS, hydrocephalus. Denial: Avoidance of disagreeable realities by ignoring or refusing to recognise them. Depersonalisation: A characteristic of depression when a person is aware of a change in self & may feel that they have become so different as to have become detached from their personality. The person may describe the feeling as ‘if in a dream’ or ‘like automatum’. Mild depersonalisation can occur in states of physical & mental fatigue. Depression: An abnormal extension or overelaboration of sadness or grief. Page 26 Disassocation: The separation of any group of mental or behavioural processes from the rest of a person’s consciousness or identity. Double bind: Simultaneous communication of conflicting messages in the context of a situation that does not allow escape. Dysphasia: A disturbance of either the comprehension or expression of speech. Dystonia: Acute tonic muscle spasms, often of the tongue, jaw, eye & neck but sometime the whole body. Usually occurs as a result of medication. E Electro-Convulsive Therapy (ECT) A form of medical treatment for mental disorder in which seizures are induced by passing electricity through the brain of an anaesthetised patient; generally used as treatment for severe depression. Emergency Application An application for detention for assessment made only one supporting medical recommendation in cases of urgent necessity. The patient can only be detained for a maximum of 72 hours unless a second medical recommendation is received. Also known as a “section 4 application”. European Convention on Human Rights (ECHR) The European Convention for the Protection of Human Rights and Fundamental Freedoms. The substantive rights it guarantees are largely incorporated into UK law by the Human Rights Act 1998. Echolia: Heard speech is repeated, usually only a word or phrase. Ertomania: Typical account is of a woman who falls in love with an unobtainable man of higher status. All acts by the man are interpreted to be consent with his love being returned to her, including blunt rejection. F Flight of ideas: Over productive speech characterised by rapid shifting from one topic to another & fragmented ideas. Free association: The verbalisation of thoughts as they occur, without any conscious screening or censorship G GP A patient’s general practitioner (or “family doctor”) Guardian See guardianship. Guardianship The appointment of a guardian to help and supervise patients in the community for their own welfare or to protect other people. The guardian may be either a local social services authority (LSSA) or someone else approved by an LSSA (a private guardian). Guardianship Application An application to a local social services authority by an approved mental health professional or a nearest relative for a patient to Page 27 become subject to guardianship. Guardianship Order An order by the court, under Part 3 of the Act that a mentally disordered offender should become subject to guardianship. Guiding Principles The principles set out in chapter 1 that have to be considered when decisions are made under the Act. Grandiose delusions: A belief that a person has a special skill, role or mission in the world; especially when there are elaborate beliefs about why the patient was chosen. H Habilitation Equipping someone with skills and abilities they have never had. As opposed to rehabilitation, which means helping them recover skills and abilities they have lost. Health Action Plan A plan which details the actions needed to maintain and improve the health of an individual with a learning disability and any help needed to achieve them. It links the individual with the range of services and supports they need in order to have better health. It is part of their broader person-centred plan. Holding Powers The powers in section 5 of the Act which allow hospital in-patients to be detained temporarily so that a decision can be made about whether an application for detention should be made. There are two holding powers: under section 5(2), doctors and approved clinicians can detain patients for up to 72 hours; and under section 5(4), certain nurses can detain patients for up to 6 hours. Hospital Direction An order by the court under Part 3 of the Act for the detention for medical treatment in hospital of a mentally disordered offender. It is given alongside a prison sentence. Hospital directions are given under section 45A of the Act. Hospital Managers The organisation (or individual) responsible for the operation of the Act in a particular hospital (eg an NHS trust, an NHS foundation trust or the owners of an independent hospital). Hospital managers have various functions under the Act, which include the power to discharge a patient. In practice, most of the hospital managers’ decisions are taken on their behalf by individuals (or groups of individuals) authorised by the hospital managers to do so. This can include clinical staff. Hospital managers’ decisions about discharge are normally delegated to a “managers’ panel” of three or more people. Hospital Order An order by a court under Part 3 of the Act for the detention for medical treatment in hospital of a mentally disordered offender, given instead of a prison sentence or other form of punishment. Hospital orders are normally made under section 37 of the Act. Human Rights Act 1998 A law largely incorporating into UK law the substantive rights set out in the European Convention on Human Rights. Hallucinations: Perceptual distortion arising from any of the five senses (ie seeing, hearing, feeling,tasting, smelling something that is not present). Hysteria: 1) When anxiety created by emotional conflict is converted into physical symptoms (eg paralysis, tics, mutism) ) A state of tension or excitement where there is a temporary loss of control over the emotions. Page 28 I Ideas of reference: Incorrect interpretation of casual incidents & external events as having direct personal references. Illusions: False perceptions or false responses to a sensory stimulus. Independent Hospital A hospital which is not managed by the NHS. Independent (IMHA) Advocate Mental Health An advocate available to offer help to patients under arrangements which are specifically required to be made under the Act.2 Independent Mental Health Advocate (IMHA) The services which make independent mental health advocates available to patients. The Act calls patients who are eligible for these services “qualifying patients”. Informal Patient Someone who is being treated for a mental disorder and who is not detained under the Act. Also sometimes known as a “voluntary patient”. Institutionalisation: The habituation of an individual to the patterns of behaviour & routines associated with, & expected in, an institution.This requirement to conform is associated with restriction in personal freesom & choice, creating loss of individuality. Interim Hospital Order An order by a court under Part 3 of the Act for the detention for medical treatment in hospital of a mentally disordered offender on an interim basis, to enable the court to decide whether to make a hospital order or deal with the offender’s case in some other way. Interim hospital orders are made under section 38 of the Act. Introjection: An intense type of identification in which one incorporates qualities or values of another person or group into one’s own ego structure. L Learning Disability In the Act, a learning disability means a state of arrested or incomplete development of the mind which includes significant impairment of intelligence and social functioning. It is a form of mental disorder. Learning Disability The rule which says that certain parts of the Act only apply to a learning disability if the learning disability is associated with qualification abnormally aggressive or seriously irresponsible behaviour on the part of the person concerned. Leave of Absence Permission for a patient who is detained in hospital to be absent from the hospital for short periods, eg to go to the shops or spend a weekend at home, or for much longer periods. Patients remain under the powers of the Act when they are on leave and can be recalled to hospital if necessary in the interest of the patient’s health or safety or for the protection of other people. Local Social Services Authority (LSSA) The local authority (or council) responsible for social services in a particular area of the country. Page 29 La belle indifference: A term sometimes applied to an apparent lack of concern commonly associated with symptoms of hysteria. Lability: A rapid change in mood, which can occur especially in elderly people with a mental disorder . Loose association: Lack of a logical relationship between thoughts & ideas that renders speech & thought inexact, vague, diffuse & unfocussed. Low stimulus environment: An area away from general ward areas where the patient is less aroused by the environment & where nursing is more intense. Related to Psychiatric intensive care unit (PICU). M Managers See hospital managers. Managers’ Panel A panel of three or more people appointed to take decisions on behalf of hospital managers about the discharge of patients from detention or supervised community treatment. Medical Recommendation Normally means a recommendation provided by a doctor in support of an application for detention or a guardianship application. Medical Treatment In the Act, this covers a wide range of services. As well as the kind of care and treatment given by doctors, it also includes nursing, psychological therapies, and specialist mental health habilitation, rehabilitation and care. Medical Treatment for Mental Disorder Medical treatment which is for the purpose of alleviating, or treatment preventing a worsening of, the mental disorder, or one or more of its for mental symptoms or manifestations. Mental Capacity Act The Mental Capacity Act 2005. An Act of Parliament that governs decision-making on behalf of people who lack capacity, both where they lose capacity at some point in their lives, eg as a result of dementia or brain injury, and where the incapacitating condition has been present since birth. Mental Disorder Any disorder or disability of the mind. As well as mental illnesses, it includes conditions like personality disorders, autistic spectrum disorders and learning disabilities. Mental Health Act Commission See Commission. Mental Illness An illness of the mind. It includes common conditions like depression and anxiety and less common conditions like schizophrenia, bipolar disorder, anorexia nervosa and dementia. Mentally Disordered Offender A person who has a mental disorder and who has committed a criminal offence. Mania: A condition characterised by a mood that is elated, expansive or irritable. Manic depression: Outdated term for bipolar affective disorder. Page 30 Mental disorder: means mental illness, arrested or incomplete development of mind, psychopathic disorder and any other disorder or disability of mind. Mental handicap: A dated term for learning difficulties and/or disabilities. Morbid jealousy: Conviction that a partner is having an affair, checks partner’s clothes and movements. Denial is interpreted as proof. Patients are potentially dangerous as they may resort to violence. Morbid jealousy is often associated with alcoholism and is more common in men. It can arise in organic states. Mood: A general overview of predominant feelings: includes past & current affective experiences. N Nearest Relative A person defined by section 26 of the Act who has certain rights and powers under the Act in respect of a patient for whom they are the nearest relative. NHS The National Health Service. NHS Commissioners Primary care trusts (PCTs) and other bodies responsible for commissioning NHS services. NHS Trust and NHS Foundation Trust Types of NHS body responsible for providing NHS services in a local area. Nominated Deputy A doctor or approved clinician who may make a report detaining a patient under the holding powers in section 5 in the absence of the doctor or approved clinician who is in charge of the patient’s treatment. Neurosis: disorder, which does not affect the whole personality; characterised by anxiety & tension. P Part 2 The part of the Act which deals with detention, guardianship and supervised community treatment for civil (ie non-offender) patients. Some aspects of Part 2 also apply to some patients who have been detained or made subject to guardianship by the courts or who have been transferred from prison to detenton in hospital by the Secretary of State for Justice under Part 3 of the Act. Part 2 Patient A civil patient – ie a patient who became subject to compulsory measures under the Act as a result of an application for detention or a guardianship application by a nearest relative or an approved mental health professional under Part 2 of the Act. Part 3 The part of the Act which deals with mentally disordered offenders and defendants in criminal proceedings. Among other things, it allows courts to detain people in hospital for treatment instead of punishing them, where particular criteria are met. It also allows the Secretary of State for Justice to transfer people from prison to detention in hospital for treatment. Page 31 Part 3 Patient A patient made subject to compulsory measures under the Act by the courts or by being transferred to detention in hospital from prison under Part 3 of the Act. Part 3 patients can be either “restricted” (ie subject to special restrictions on when they can be discharged, given leave of absence, and various other matters) or “unrestricted” (ie treated for the most part like a Part 2 patient). Part 4 The part of the Act which deals mainly with the medical treatment for mental disorder of detained patients (including SCT patients who have been recalled to hospital). In particular, it sets out when they can and cannot be treated for their mental disorder without their consent. Part 4A The Part of the Act which deals with the medical treatment for mental disorder of SCT patients when they have not been recalled to hospital. Part 4A Certificate A SOAD certificate approving particular forms of medical treatment for mental disorder for an SCT patient. Part 4A Patient means an SCT patient who has not been patient recalled to hospital. Patient People who are, or appear to be, suffering from a mental disorder. This use of the term is not a recommendation that the term “patient” should be used in practice in preference to other terms such as “service users”, “clients” or similar terms. It is simply a reflection of the terminology used in the Act itself. Person Centred Plan An individual plan for each person with a learning disability, tailored to their needs and aspirations, which aims to help them to be a part of their community and to help the community to welcome them. Place of Safety A place in which people may be temporarily detained under the Act. In particular, a place to which the police may remove a person for the purpose of assessment under section 135 or 136 of the Act. (A place of safety may be a hospital, a residential care home, a police station, or any other suitable place.) Primary Care Trust (PCT) The NHS body responsible, in particular, for commissioning (arranging) NHS services for a particular part of England. PCTs may also provide NHS services themselves. Private Guardian An individual person (rather than a local social services authority) who is a patient’s guardian under the Act. Perception: The organisation & interpretation of stimuli into meaningful knowledge. Polypharmacy: Use of combinations of psychoactive drugs in a patient at the same time; more than one drug may not be more effective than a single agent, can cause drug interactions & may increase the incidence of adverse reactions. Projection: Attributing one’s own thoughts or impulses to another person. Through this process the person can attribute intolerable wishes, emotional feelings or motivations to another person. Psychopath: A person with an antisocial personality (also known as sociopath). Not connected to pyschosis. Page 32 Psychosis: A category of health problems that are distinguished by regressive behaviour, personality disintegration, reduced level of awareness, great difficulty in functioning adequately & gross impairment in reality testing. Q Qualifying Patients Patients who are eligible for support from independent mental health advocacy services. R Recall (and Recalled) A requirement that a patient who is subject to the Act return to hospital. It can apply to patients who are on leave of absence, who are on supervised community treatment, or who have been given a conditional discharge from hospital. Regulations Secondary legislation made under the Act. In most cases, it means the Mental Health (Hospital, Guardianship and Treatment) (England) Regulations 2008. Rehabilitation See habilitation. Remand to Hospital (and Remanded to Hospital) An order by a court under Part 3 of the Act for the detention in hospital of a defendant in criminal proceedings. Remand under section 35 is for a report on the person’s mental condition. Remand under section 36 is for medical treatment for mental disorder. Responsible Clinician The approved clinician with overall responsibility for a patient’s case. Certain decisions (such as renewing a patient’s detention or placing a patient on supervised community treatment) can only be taken by the responsible clinician. Responsible Hospital The hospital whose managers are responsible for an SCT patient. To begin with, at least, this is the hospital in which the patient was detained before being discharged onto supervised community treatment. Responsible Local Social Services Authority (LSSA) The local social services authority (LSSA) responsible for a patient who is subject to guardianship under the Act. The responsible LSSA is normally the LSSA for the area where the patient lives. But if the patient has a private guardian, it is the LSSA for the area where the guardian lives. Restricted Patient A Part 3 patient who, following criminal proceedings, is made subject to a restriction order under section 41 of the Act, to a limitation direction under section 45A or to a restriction direction under section 49. The order or direction will be imposed on an offender where it appears that it is necessary to protect the public from serious harm. One of the effects of the restrictions imposed by these sections is that restricted patients cannot be given leave of absence or be transferred to another hospital without the consent of the Secretary of State for Justice, and only the Tribunal can discharge them without the Secretary of State’s agreement. See also Unrestricted Part 3 patient. Revocation (and Revoke) Term used in the Act to describe the rescinding of a community treatment order (CTO) when an SCT patient needs further treatment in hospital under the Act. If a patient’s CTO is revoked, the patient is detained under the powers of the Act in the same way as before the CTO was made. Page 33 Reality orientation: Formal process of keeping a person alert to events in the here & now. Relapse: Return of symptoms. S SCT patient A patient who is on supervised community treatment. Second Opinion Appointed Doctor (SOAD) An independent doctor appointed by the Commission who gives a second opinion on whether certain types of medical treatment for mental disorder should be given without the patient’s consent. Secretary of State Cabinet ministers in the Government. In the Act, either the Secretary of State for Health or the Secretary of State for Justice, depending on the context. Secretary of State for Health Secretary of State for Justice The Secretary of State who is responsible, among other things, for the NHS and social services for adults. The Secretary of State for Health is supported by the Department of Health. The Secretary of State who is responsible, among other things, for courts, prisons, probation, criminal law and sentencing. The Secretary of State for Justice is supported by the Ministry of Justice. Section 4 Application See emergency application. Section 57 Treatment A form of medical treatment for mental disorder to which the special treatment rules in section 57 of the Act apply, especially neurosurgery for mental disorder (sometimes called “psychosurgery”). It is possible that other forms of treatment may be added to section 57, section 58 or section 58A by regulations. Section 58 Treatment A form of medical treatment for mental disorder to which the special rules in section 58 of the Act apply, which means medication for mental disorder for detained patients after an initial three-month period. Section 58A Treatment A form of medical treatment for mental disorder to which the special rules in section 58 of the Act apply, especially electro-convulsive therapy. Section 117 See after-care. SOAD Certificate A certificate issued by a second opinion appointed doctor (SOAD) approving particular forms of medical treatment for a patient. Strategic Health Authority (SHA) NHS body responsible for overseeing all NHS services in a particular region of England. Supervised Community Treatment Arrangements under which patients can be discharged from detention in hospital under the Act, but remain subject to the Act in the community rather than in hospital. Patients on SCT are expected to comply with conditions set out in the community treatment order and can be recalled to hospital if treatment in hospital is necessary again. Schizoaffective disorder: Diagnosis given to patients who meets the diagnostic criteria Page 34 for schizophrenia as well as one or both of the major mood disorders of bipolar disorder & major depression. Schizophrenia: Umbrella term for a range of symptoms. A person can’t distinguish their own intense thoughts, ideas, perceptions and imaginings from reality (the shared perceptions, sets of ideas and values that other people in that culture hold to be real). Among other symptoms, a person might be hearing voices, or may believe that other people can read their mind and control their thoughts. Schizophrenia does not mean ‘a split personality’. Seclusion: Separating the patient from others in a safe, contained environment. Self-esteem: The person’s judgement of personal worth obtained by analysing how well his or her behaviour conforms to self ideal. Splitting: Viewing people & situations as either all good or bad. Failure to integrate the positive & negative qualities of oneself & of objects. T Tribunal A judicial body which has the power to discharge patients from detention, supervised community treatment, guardianship and conditional discharge. At the time of publication, this means the Mental Health Review Tribunal (MHRT). However, subject to Parliament, the MHRT is intended to be replaced in England by a new First Tier Tribunal established under the Tribunals, Courts and Enforcement Act 2007. Tardive dyskinesia: Literally ‘late appearing abnormal movements’, a variable complex of choreiform or athetoid movements developing in patients exposed to antipsychotic drugs. Typical movements include tongue withering or protrusion, chewing, lip puckering, chorieform finger movements, toe & ankle movements, leg jiggling & movements of neck, trunk & pelvis. Thought blocking: Sudden stopping in the train of thoughts or in the midst of a sentence. Thought broadcasting: A person believes that everybody can hear their thoughts. Thought withdrawal: A belief that thoughts are being taken away from an individual. Thought insertion: A belief that thoughts are being inserted into an individual’s head. U Unrestricted Part 3 Patient A patient subject to a hospital order or guardianship order under Part 3 of the Act, or who has been transferred from prison to detention in hospital under that Part, who is not also subject to a restriction order or direction. For the most part, unrestricted patients are treated in the same way as Part 2 patients, although they cannot be discharged by their nearest relative. See also Restricted patient. Page 35 V Voluntary Patient See informal patient. W Word salad: Series of words that seem totally unrelated. Welsh Ministers Ministers in the Welsh Assembly Government. Y Young Person A person aged 16 or 17. Page 36 Common Sections SECTION 5(2) IN PATIENT EMERGENCY 2 ASSESSMENT 3 TREATMENT 4 EMERGENCY ADMISSION 17A SUPERVISED COMMUNITY TREATMENT DURATION IMPLEMENTATION PROCESS APPEAL DISCHARGE PROCESS FOLLOWED BY SPECIAL INSTRUCTIONS NO EXPIRES/S23 BY RC/ ASSESSED & NOT DETAINABLE EXPIRES BECOMES INFORMAL OR CONVERTED TO A 2 OR 3 72 HOURS BEGINS WHEN RECEIVED BY MANAGERS (FORM 14) 28 DAYS 2 MEDICAL RECOMMENDATIONS 1 ASW OR NEAREST RELATIVE APPLICATION WITHIN FIRST 14 DAYS TO MHRT OR ANY TIME TO MANAGERS EXPIRES OR RC S23 OR MHRT/MANAGERS EXPIRES BECOMES INFORMAL OR SEC 3 ASSESSMENT ONLY MUST BE CONVERTED TO S3 IF DIAGNOSIS MADE 6 MONTHS 2 MEDICAL RECOMMENDATIONS 1 ASW OR NEAREST RELATIVE APPLICATION ONCE IN 1ST 6-MTH THEN EVERY PERIOD OF DETENTION OR ANY TIME TO MANAGERS EXPIRES OR RC S23 OR MHRT/MANAGERS RENEWABLE AFTER 6 MTH THEN YEARLY 72 HOURS 1 MEDICAL RECOMMENDATION 1 ASW APPLICATION NO EXPIRES/S23 OR ASSESSED & NOT DETAINABLE CONVERT TO 2 OR APPLICATION FOR 3 6 MONTHS RESPONSIBLE CLINICIAN WITH AGREEMENT OF AMHP ONCE IN 1ST 6-MTH THEN EVERY PERIOD OF DETENTION OR ANY TIME TO MANAGERS EXPIRES OR RC S23 OR REVOCATION OR MHRT/MANAGERS RENEWABLE AFTER 6 MTH THEN YEARLY 72 HOURS RC/SHO IN PSYCHIATRY NO RC/12(2) AFTER FULL ASSESSMENT ASW MUST ASSESS SHO CANNOT DISCHARGE INFORMAL ADMISSION S2 / S3 OR DISCHARGE RC/COVERING RC NOT SPR NO NOT APPLICABLE FURTHER SEC 17 NOT APPLICABLE NOT APPLICABLE RC OR MHRT/MANAGERS 117 FOR SEC 3 136 POLICE – PLACE OF SAFETY 72 HOURS POLICE 17 LEAVE AS SPECIFIED 23 DISCHARGE NOT APPLICABLE THE THREE MONTH RULE FOR TREATMENT APPLIES SUBJECT TO S117 ON DISCHARGE BEGINS WHEN PATIENT ARRIVES IN HOSPITAL 2 MED REC CONVERTS S4 TO S2 (WITHIN 72 HOURS) PART 4A FOR TREATMENT APPLIES. SUBJECT TO S117. MAY BE RECALLED FOR UPTO 72 HOURS PLACE OF SAFETY MAY ALSO BE POLICE STATION IF INTOXICATED/VIOLENT. A&E EN ROUTE IF REQ’S MEDICAL ATTENTION POLICE TO STAY UNTIL MANAGERS ACCEPT RESPONSIBILITY TIMES, ESCORTS AND DESTINATION TO BE SPECIFIED S23 TO BE SIGNED BY RC Page 37 FLOWCHART OF DETENTION MHA Assessment by AMHP Emergency – s.4 or s.135 Non-Emergency – s.2, 3 Patient in Community Police Officer - S.136 Court Before Sentencing Assessment – s.35 Treatment – s.36 Interim – s.38 After Sentencing Hospital Order – s37 Guardianship Order – s37 (return to community) Hospital Order with Restrictions – 37/41 Hospital Recall / Revocation Community Supervised Community Treatment – s.17A Conditionally Discharged – s.41 Community Informal Aftercare – s.117 Guardianship – s.7 Conditionally Discharged – s.41 38 Remand Centre Transfer – s48 Transfer with Restrictions – s.48/49 Prison Transfer – s47 Transfer with Restrictions – s.47/49