WPA Position Statement on ECT
advertisement

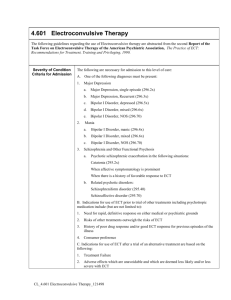
WORLD PSYCHIATRIC ASSOCIATION Position Statement on the Use and Safety of Electroconvulsive Therapy Prepared on behalf of the WPA Section on Biological Psychiatry by: Mohammed T Abou-Saleh, Chair of the WPA Section on Biological Psychiatry St George’s Hospital Medical School Cranmer Terrace London SW17 ORE , UK Tel 00442087252802 Fax 00442087252914 Email:mabousal@sghms.ac.uk Yiannis Papakostas yiargeke@hol.gr Ioannis Zervas Zervas@compulink.gr George Christodoulou gnchrist@compulink.gr Secretary for Sections, World Psychiatric Association President, International College of Psychosomatic Medicine Papadiamantopoulou 11 str., 115 28 Athens, GREECE Tel.: +30 210 72 91 389 Fax: +30 210 72 42 032 E-mail: gnchrist@compulink.gr This position statement on the use and safety of electroconvulsive therapy (ECT) has been prepared on behalf of the WPA Section on Biological Psychiatry at the request of the Executive Committee of the WPA. The statement is informed by available evidence and reference will be made to guidelines produced by a number of authoritative bodies, including the American Psychiatric Association, the Royal College of Psychiatrists, the UK National Institute of Clinical Excellence (NICE) and the World Federation of Societies of Biological Psychiatry. Moreover, for depressive disorders particular reference will be made to the recently published systematic review and meta-analysis by the UK ECT Review Group (2003) . Introduction Electroconvulsive therapy (ECT) is an important though controversial treatment for certain subgroups of individuals suffering from severe mental disorder. These subgroups consist primarily of patients with severe depressive disorder, catatonia, mania and occasionally certain patients with schizophrenia. In addition, depending on the comorbidity with medical and / or neurological disorders and on the risk analysis in relation to the necessity to treat, ECT can be administered either as a low risk or a high risk procedure. ECT should be administered following valid and informed consent by the patient when appropriate and in adherence to a set of guidelines of administration procedures. The scope of this statement is to consider the evidence for the efficacy of ECT in the treatment of depressive and other psychiatric disorders and its safety and determine its optimum use with continuation pharmacotherapy and provide recommendations for practice. Depressive Disorders The introduction of ECT for the treatment of severe depressive illness is one of the most dramatic developments in psychiatry. It is widely considered to be the most effective treatment for severe depressive illness compared with all other modalities including the range of pharmacological treatments. Since its introduction in the early 1930s it has undergone important development and improvement with the use of anaesthesia and muscle relaxation which rendered it more safe and acceptable. The recall of ECT in the US in the 1970s was “plagued by hostility to the treatment” (Fink, 2001) fuelled by images of barbaric, inhumane and coercive treatment. In contrast to such an approach, many national psychiatric associations and societies have promoted ECT and many countries have introduced guidelines for practice: Australia, Canada, New Zealand, UK and the US ( Bauer et al,2002). It is however of considerable concern that in many third world countries, ECT is still used without the benefit and safety of anaesthesia or modern ECT devices (Fink, 2001). Full review of the successful management of depressive disorders is beyond the scope of this Position Statement. It should however be based on comprehensive assessment, formulation and implementation of a treatment plan. Treatment is categorised into an acute phase to induce a remission in the disorder over a period of 6 to 8 weeks, a continuation phase to maintain remission and to achieve recovery over a period of 16 to 20 weeks to prevent a relapse in the disorder and a prophylatic/maintenance phase to prevent a recurrence in the disorder (occurrence of a new episode of illness) the duration of which is dependent upon the previous frequency and severity of the disorder. Assessment Comprehensive assessment of the patient includes the following components: Diagnostic evaluation to determine the diagnosis of the episode of illness and whether the patient is suffering from bipolar depression or non bipolar depression with or without melancholia or psychotic features including delusional depression. Evaluation of the safety of the patient and others based on assessment of risk of self harm or harm to others. Evaluation of risk is based on presence of suicidal or homicidal ideas intent and plans; access to means for self harm or harm to others and history of suicidal behaviour. Evaluation of functional impairment in ability to work and in family and social relationships. Determination of the optimal treatment setting to attain assessment and treatment objectives and importantly to maintain patient safety and minimise risk to self neglect, risk to self harm and harm to others. Treatment setting ranges from the least restrictive community and outpatient clinic to inpatient treatment under voluntary or involuntary conditions. (APA Treatment Recommendations, 2000). Consent to ECT Valid consent to ECT is required unless common law or statue provides authority to treat without consent when treatment is in the patient’s best interest i.e. necessary to save life or prevent deterioration or ensure an improvement in physical and mental health .Consent may be withdrawn by the patient at any time. If the patient refuses or is incapable of giving or withholding consent to ECT, a second opinion of a specialist colleague should be obtained and the patient’s relatives are consulted before a decision is made to give ECT. A patient who is ill enough to require ECT, is almost certainly unable to give fully informed consent. Acute Treatment ECT is particularly indicated for patients with severe depressive disorder associated with greater severity ( in terms of intensity , frequency, and duration ) of symptoms including the presence of psychotic feature (delusional depression) or catatonic symptoms, and the urgent need for improvement in those with high suicide risk or those who are at risk of serious physical deterioration. Under these circumstances, ECT is the treatment of first choice with or without pharmacotherapy with antidepressants and anti-psychotics when 2 indicated. Prior history of improvement with ECT and patient preference for the treatment are also important considerations. The evidence base A recent systematic review and metanalyasis of randomised controlled trials and observational studies of the efficacy and safety of ECT in depressive disorders (UK ECT Review Group, 2003) reported the following findings: ECT versus simulated ECT – ECT was significantly more effective than simulated ECT in the reduction of depressive symptoms and no difference in premature discontinuation from treatment for patients receiving ECT and simulated ECT. Patients treated with ECT were better able to retrieve remote memories than those treated with simulated ECT and had more recognition errors immediately after treatment. ECT versus pharmacotherapy – treatment with ECT was significantly more effective than pharmacotherapy and discontinuation was significantly lower in the ECT group than in the pharmacotherapy group. Bilateral versus unilateral electrode placement – Bilateral ECT was more effective than unilateral ECT in the reduction of depressive symptoms High-dose unilateral ECT might be as effective as bilateral ECT and causes fewer adverse cognitive effects. Bilateral ECT was associated with impairment in anterograde memory impairment within seven days of the end of the randomised phase of treatment but no long term cognitive impairment. Frequency of ECT – ECT administered once a week, twice and three times a week had similar effects on depressive symptoms and no difference in discontinuation of treatment but more frequent ECT lead to more cognitive impairment. Dose of electrical stimulus – high dose ECT lead to greater reduction in depressive symptoms, but was associated with more impairment in anterograde memory but not in terms of personal memory. Stimulus wave form – brief pulse and sign wave ECT were equally effective with some indication that patients receiving brief pulse ECT recovered more quickly and had better recall of word associates learned shortly before the treatment than did those receiving sign wave ECT. A meta-analysis of the efficacy of ECT in depression deriving from 15 randomised controlled trials (RCTs) showed ECT to be superior to pharmacotherapy and simulated ECT, with the presence of psychotic symptoms predicting better response to ECT (Kho et al, 2003). The report found no evidence for a superior speed of action of ECT or for a difference between sine wave and brief pulse stimulation. ECT has been shown to be more effective in delusional than in non-delusional depression (Meyers et al, 2001, Birkenhager et al, 2003).A recent Cochrane Review assessed the efficacy and safety of ECT compared to simulated ECT or antidepressants in the depressed elderly (Van der Wurff et al, 2003). Only 3 trials could be included and all had methodological shortcomings. The results indicated the efficacy of ECT compared to simulated ECT, but the efficacy of unilateral over bilateral ECT and safety could not be assessed adequately. Older age confers a greater likelihood of achieving a remission with bilateral, dose-titerated, continuation ECT in comparison with continuation pharmacotherapy (O’Connor et al, 2001). The NICE Review (2003) of data from 90 RCTs of ECT in depressive disorders concluded that real ECT (where electric current was applied) is more effective than simulated ECT (no electric current was applied) in the short term 3 bilateral ECT is more effective than unilateral ECT. raising the electrical stimulus above the individual’s threshold supported the efficacy of unilateral ECT at the expense of increased cognitive impairment. ECT was more effective than antidepressants notwithstanding the variable quality of RCTs and the inadequate doses and duration of antidepressants that were used in many of the trials ECT is associated with cognitive impairment, particularly in those who had bilateral ECT or unilateral ECT applied to the dominant hemisphere cognitive function does not last more than six months from the administration of ECT there is no evidence that ECT is associated with greater mortality than that associated with the administration of general anaesthetics. Studies that use brain/scanning techniques showed no evidence that ECT causes brain damage. there is no evidence to suggest that the benefits and safety of ECT are agedependent. there are no complications of ECT in pregnancy but the risks should be balanced against refusing antidepressant. Continuation pharmacotherapy after ECT High relapse rates of depression have been consistently reported after remission with ECT. Five controlled trials have demonstrated the efficacy of continuation treatment with antidepressants and lithium in reducing relapse after remission with ECT (AbouSaleh and Coppen, 1988). Further RCTs have demonstrated the efficacy of continuation treatment with imipramine and paroxetine in relapse prevention in such patients (Lauritzen et al, 1996). Nortriptyline monotherapy and its combination with lithium has also been shown to be superior to placebo over 6 months in preventing relapses in unipolar depression following remission with ECT (Sackeim et al, 2001) . Schizophrenia A Cochrane Review assessed the evidence for the efficacy of ECT in clinically meaningful benefits in patients with schizophrenia and whether variations in the practical administration of ECT influences outcome (Tharyan and Adams, 2002). The Review included 24 trials and 46 reports and showed the following: Fewer patients remain unimproved with ECT, with less relapses and earlier discharge than patients treated with placebo or simulated ECT limited data indicated visual memory impairment with ECT compared with simulated ECT ECT is less beneficial than antipsychotic medication continuation ECT added to antipsychotics is superior to antipsychotics alone but is associated with more memory impairment. ECT has been shown to have good short-term effects and be safe in middle aged and elderly patients with intractable catatonic schizophrenia (Suzuki, et al, 2003) and in treatment-resistant schizophrenia (Tang and Ungvari, 2003). In schizophrenia, the NICE Review (2003) of the data from 25 RCTs indicated that ECT may be effective in acute episodes of certain types of schizophrenia and reduces the occurrence of relapses. However, the results were not conclusive and the design of many of the studies did not reflect current practice. Moreover, there are no RCTs of ECT compared with antipsychotics. Furthermore, studies that include patients with treatmentresistant schizophrenia had not reported the use of clozapine. The review concluded that ECT alone is not more effective than antipsychotic medication but that the combination of ECT and pharmacotherapy may be more effective than pharmacotherapy alone although the evidence is not conclusive. 4 Mania The NICE Review (2003) of 4 RCTs indicated that ECT may be of benefit in rapid control of mania and catatonia, a suggestion that is supported by the results of observational studies. Overall however, it concluded that the evidence for the effectiveness of ECT and for the determination of the most appropriate therapeutic strategy is inconclusive. In contrast, a recent literature review of continuation and maintenance ECT in treatment-resistant bipolar disorder reported good evidence for efficacy (Vaidya et al, 2003).ECT is indicated in severe and prolonged mania (excitement, delirium, psychosis, or rapid –cycling manic states), especially when the anti-manic medications (lithium, neuroleptics) have been relatively inefficient (Mukherjee et al. 1994). It seems that the NICE review has been restrictive in the studies it considered and the conclusions drawn from them. Other indications In certain rare conditions ECT is widely considered to be a first-line treatment choice. Catatonia, i.e. marked abnormalities in the overall level of motor activity, either on the stuporous, or the excited form, can be manifested in the context of mood disorders and schizophrenia. Since this condition constitutes a state of psychiatric emergency and although some pharmacological interventions (such as benzodiazepines, barbiturates) may have some effectiveness, ECT should be considered early in the treatment plan (McCall, 1992). ECT should also be considered as a life-saving treatment for certain cases of neuroleptic malignant syndrome- a condition sharing some similarities with catatonic stupor- particularly if conservative treatments (direct dopamine agonists, dantrolene sodium, etc.) have failed to control the condition within a few days (Trollor & Sachdev 1999). ECT has been occasionally employed in several non-mood disorder diagnosesincluding alcoholism, anorexia nervosa, OCD, dementia, personality disorders and Parkinson’s disease (McCall, 2001) but the current state of the evidence does not allow the general use of ECT in these conditions. It must be noted that when ECT is used in special population groups, such as during pregnancy, in older people, and in children and young people, and in view of its possible risks, clinicians should exercise particular caution (National Institute for Clinical Excellence,UK, 2003) Risks The mortality associated with ECT is similar to that associated with minor procedures involving general anaesthesia (1/100,000 per treated patients), with death almost exclusively due to cardiac complications. However, with adherence to administration guidelines, serious cardiac complications such as myocardial infarction, ventricular fibrillation, and ruptured aneurysms- are rare even in patients with pre-existing cardiac disease (Zielinsky et al 1993). Cognitive disturbances in the acute use of ECT retrograde and anterograde amnesia and confusion are in general transient and reversible and in most cases do not pose a major or persistent clinical problem. Further, controlled brain imaging studies failed to provide any evidence that ECT causes brain damage (National Institute for Clinical Excellence, 2003). However, the issue of cognitive dysfunction in the case of continuation and maintenance ECT is still open to inquiry. In addition cognitive dysfunction associated with ECT, even though difficult to differentiate at times from the effects of psychopathology itself, is extremely distressing to certain patients and should always be followed closely. A recent systematic review of studies of patients’ perspectives on its benefits and its effects on memory, showed that the perceived benefits were less in patient led studies than clinician led ones .Moreover at least one third of patients reported significant memory loss after treatment with no difference between patient and clinician based studies (Rose et al, 2003). Contra-indications 5 There are no known absolute contra-indications to ECT but certain relative contraindications do exist: Brain tumour or cerebral infarction, history of myocardial infarction or cardiac arrhythmias, cardiac pacemakers, aneurysms, retinal detachment, pheochromocytoma, and pulmonary diseases are among the potentially dangerous conditions where the use of ECT is considered high risk and requires additional precautions (Stevens et al 1996). Practical considerations There are no grounds for administering unmodified (no anaesthesia) ECT .Anaesthesia for ECT involves pre-ECT assessment and investigations to consider contraindications, preparation, premedication, anaesthetic induction agents, muscle relaxants, ventilation and recovery from anaethesia. The routine medications administered are atropine (not universally employed by the clinicians) to prevent vagotonic bradycardia, succinylcholine as muscle relaxant, and pentothal, methohexital or etomidate as hypnotics. Six to 8 sessions is the average number of treatments for depression (up to 12 or more, on occasion, if there is no clinical improvement), while for mania the number is 8-12 (usually up to 16). Patients who are reported to respond fast (after 6-8 treatments) and relapse fast, may suggest a necessity to switch early to continuation therapy (Abrams and Swartz, 1992). Three times a week ECT (as used in the USA) as opposed to twice a week schedule (as used in Europe) are similar in effectiveness. Patients progress should be monitored after each treatment to assess efficacy and side effects. ECT should be continued until clinical improvement is observed. Regarding the electrical stimulus the best results are expected, as a general rule, with brief-pulse square wave, electrical doses about 2.0 to 2.5 times higher to the seizure threshold (rather than doses around the seizure threshold) and with bilateral ECT as opposed to unilateral ECT electrode placement. However, optimal electrical dosing and electrode placement should be individualized for each patient. Monitoring seizure activity is achieved by simply timing the convulsion and the use of the cuff technique .The cuff technique unlike the timing of the convulsion is not affected by muscle relaxants. EEG monitoring is the most direct assessment of cerebral seizure activity and is useful when total paralysis is desired. There are indications that continuation of ECT treatments at biweekly or monthly intervals over 4 to 6 months following acute ECT administration, could be beneficial sustain the treatment benefits. The systematic studies to evaluate these forms of treatment are currently underway and no conclusive data are available as yet. Clinical judgement and prudence are recommended in the use of these outpatient forms of ECT. Important components of good practice in ECT are the education of patients, their carers and the general public. Fact sheets for patients and carers would facilitate their cooperation and allay understandable concerns. Public education on ECT is an important component of professional bodies antistigma campaigns. Administration of psychotropics during ECT There is controversy regarding the co-administration of antidepressants and ECT. On one hand the discontinuation of a failed antidepressant seems reasonable. Yet, a synergistic effect cannot be ruled out as no data are available, neither the possibility of withdrawal symptoms upon the abrupt antidepressant discontinuation (McCall, 2001). Reviews of the interactions of ECT and other psychotropic drugs find some interactions to be synergistic (neuroleptics in psychoses but not in depression), some antagonistic (benzodiazepines and anticonvulsants), and some eliciting adverse reactions, such as confusion (lithium) or cardiovascular complications (MAOI). The co-administration of compounds such as thyroid hormones, pindolol, or caffeine, as augmentation strategies during ECT, has not reached a general consensus. Perspectives After seventy years from its introduction, convulsive (and electroconvulsive) therapy represents an effective intervention for several disorders. Regarding its future 6 perspectives, optimization of the treatment procedure as well as the estimation of its value for continuation and maintenance treatment remains of high priority. On a theoretical level, the elucidation of its mechanism of action is expected to advance our knowledge not only in treating depression but in elucidating the nature of the illness itself. Guidance and Recommendations - - - - - ECT should only be considered after a comprehensive assessment and careful diagnosis of the illness with the assessment of the balance of potential benefits and risks including: risks of anaesthesia, physical condition, anticipated adverse events, particularly cognitive impairment; and the risk of not having treatment. ECT should only be administered after informed consent is obtained from patients with capacity. Appropriate guidelines for patients with impaired capacity should be adhered to. With these provisos, ECT is strongly recommended as a first line acute treatment for severe depressive disorder particularly depressive disorder with psychotic symptoms (delusional depression), depression with high risk of suicide, harm to others, self neglect and physical deterioration. ECT is effective in the treatment of antidepressant-resistant depression and the rapid control of symptoms of catatonia and prolonged or severe manic disorder. ECT is associated with high rates of relapse following remission of depressive disorder and it is strongly advocated to use continuation pharmacotherapy with antidepressants or lithium for a period of 16-20 weeks following remission of the illness. ECT is not recommended for the general treatment of schizophrenia. There is insufficient evidence for the long term benefits and risks of maintenance ECT for depressive illness. Careful consideration of risks is advocated in pregnant patients, older people and children. ECT is a safe treatment but has adverse effects on the short term memory and long term recovery of memory impairment is the rule. Bilateral ECT is associated with more cognitive impairment compared with unilateral ECT applied to the non-dominant hemisphere of the brain. The frequency of ECT and other parameters have little impact on its efficacy. Acknowledgement We are grateful for the endorsement and comments of members of the Section on the first draft and this statement, particularly those from C L Katona and C P Freeman. References Abou-Saleh MT, Coppen AJ. Continuation Therapy with Antidepressants After Electroconvulsive Therapy; 4 (4) : 263-268, 1988. Abrams R and Swartz CM. Stimulus Dosing Strategies and Unilateral ECT. Convulsive Therapy; 8 (1) : 52-53, 1992. American Psychiatric Association : Treatment recommendations for patients with major depressive disorder. Am J Psychiatry 2000 ;157:1-44 7 Bauer M, Whybrow PC, Angst J, Versiani M and Moller HJ. World Federation of Societies of Biological Psychiatry (WFSBF) Task Force on Treatment Guidelines for Unipolar Depressive Disorders. World J Biol Psychiatry, Apr; 3 (2) : 69-86, 2002. Birkenhager TK, Pluijms EM and Lucius SA. ECT response in delusional versus nondelusional depressed inpatients. J Affective Disorders, April; 74 (2) : 191-5, 2003. Fink M ECT has much to offer our patients: it should not be ignored. World J Biol Psychiatry. 2001 ;2(1):1-8. Kho KH, Van Vreeswijk MF; Simpson S, Zwinderman AH. A meta-analysis of electroconvulsive therapy efficacy in depression. J ECT, Sep; 19 (3): 139-47, 2003. Lauritzen L, Odgaard K, Clemmesen L, Lunde M, Ohrstrom J, Black C, and Bech P. Relapse prevention by means of paroxetine in ECT-treated patients with major depression: a comparison with imipramine and placebo in medium-term continuation therapy. Acta Psychiatr Scand, Nov; 96 (5) : 405-6, 1997. McCall WV. The response to an amobarbital interview as a predictor of therapeutic outcome in patients with catatonic mutism. Convulsive Therapy 1992; 8:174-178) McCall WV. Electroconvulsive therapy in the era of modern psychopharmcology. International Journal of Neuropsychopharmacology 2001; 4:315-324 Meyers BS, Klimstra SA, Gabriele M, Hamilton M, Kakuma T, Tirumalasetti F and Alexopoulos GS. Continuation treatment of delusional depression in older adults. Am J Geriatric Psychiatry. Fall; 9 (4) : 415-22, 2001. Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episodes: a review of 50 years’ experience. Am J Psychiatry 1994; 151: 169-176 National Institute for Clinical Excellence. Guidance on the use of electroconvulsive therapy. 2003, 1-36 8 O'Connor MK, Knapp R, Husain M, Rummans TA, Petrides G, Smith G, Mueller M, Synder K, Bernstein H, Rush AJ, Fink M and Kellner C. The influence of age on the response of major depression to electroconvulsive therapy : a C. O. R. E. report. Am J Geriatric Psychiatry, Fall; 9 (4) : 382-90, 2001. Rose D, Fleischmann P, Wykes T, Leese M, Bindman J. Patients' perspectives on electroconvulsive therapy: systematic review. BMJ, Jun 21; 326 (7403) : 1363, 2003. Sackeim HA, Haskett RF, Mulsant BH, Thase ME, Mann JJ, Pettinati HM, Greenberg RM, Crowe RR, Cooper TB and Prudic J. Continuation pharmacotherapy in the prevention of relapse following electroconvulsive therapy: a randomised controlled trial. JAMA, Mar 14; 285 (10) : 1299-307, 2001. Sackeim HA. The anticonvulsant hypothesis of the mechanisms of action of ECT: Current status. J ECT 1999; 15: 5-26 Stevens A, Fisher A, Bartels M, Buchkremer G. Electroconvulsive therapy: a review on indications, methods, risks, and medication. Eur Psychiatry 1996; 11: 165-174 Suzuki K, Awata S and Matsuoka H. Short-term effect of ECT in middle-aged and elderly patients with intractable catatonic schizophrenia. J ECT. Jun; 19 (2) : 73-90, 2003. Tang WK and Ungvari GS. Efficacy of electroconvulsive therapy in treatment-resistant schizophrenia : a prospective open trial. Prog Neuropsychopharmacol Biol Psychiatry, May; 27 (3) : 373-9, 2003. Tharyan P and Adams CE. Electroconvulsive therapy for schizophrenia. Cochrane Database System Reviews, (2): CD000076, 2000. The UK Review Group: Efficacy and safety of electroconvulsive therapy in depressive disorder: a systematic review and meta-analysis. Lancet 2003; 361: 799-808 Trollor JN, Sachdev PS. Electroconvulsive therapy treatment of narcoleptic malignant syndrome: a review and report of cases. Australian and New Zealand Journal of Psychiatry 1999; 33: 650-659 9 Van der Wurff FB, Stek ML, Hoogendijk WL and Beekman ATF. Electroconvulsive therapy for the depressed elderly (Cochrane Review). The Cochrane Library, Issue 4, 2003. Chichester, UK: John Wiley & Sons Ltd. Vaidya NA, Mahableshwarkar AR, Shahid R. Continuation and maintenance ECT in treatment-resistant bipolar disorder. J ECT, Mar; 19 (1) : 10-6 Review, 2003. Zielinsky RJ, Rose SP, Devanand DP, Sackeim HA. Cardiovascular complications of ECT in depressed patients with cardiac disease. Am J Psychiatry 1993; 150: 904-909 10