RESIDENT MANUAL - School of Medicine
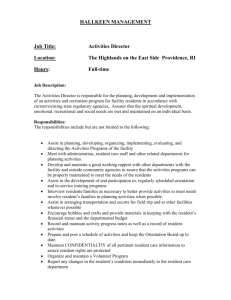
advertisement

RESIDENT MANUAL 2015-2016 MASON EYE INSTITUTE UNIVERSITY OF MISSOURI – COLUMBIA SCHOOL OF MEDICINE TABLE OF CONTENTS STATEMENT OF PURPOSE/EDUCATIONAL GOALS ROLES, DUTIES AND RESPONSIBILITIES OF RESIDENTS INSTITUTIONAL POLICIES, SCHOOL OF MEDICINE. ............................................................TAB DIVIDER Commitment to Graduate Medical Education ................................................................................................ 4 Primary Verification of Credentials For Applicants to Residency and Fellowship .....................................5-6 Graduate Medical Education Committee – Composition & Responsibilities ...............................................7-9 Internal Review Protocol, GMC Oversight Committee, University of Missouri Hospitals & Clinics .....10-14 Policy on Resident Recruitment, Eligibility & Selection .........................................................................15-16 Supervision of Residents and Fellows .....................................................................................................17-20 Policy Teamwork .......................................................................................................................................... 21 Transitions of Care ...................................................................................................................................22-23 Ophthalmology Monitoring of Patients hand-off(On-Call and In-Patient) ................................................... 25 House Staff Compliance with Timely Completion of Medical Records ..................................................26-27 Resident/Fellow Stipends .............................................................................................................................. 28 Policy: Required ACLS/BLS/PALS Certification ........................................................................................ 29 USMLE Step 3 – defining requirements for passing prior to completion of program .................................. 30 Reporting of Other Learners in a Program .................................................................................................... 31 Moonlighting Professional Activities Outside the Education Program ...................................................32-34 Moonlighting – J1 or H1B Visa Holders ...................................................................................................... 35 Policy for Payment of Fees Associated with an H1B Visa ........................................................................... 36 Professionalism, Personal Responsibility, and Patient Safety ....................................................................... 37 Duty Hour Policy for the University of Missouri ....................................................................................38-39 Alertness Management and Fatigue Mitigation ........................................................................................40-41 Institutional Vacation and Leave Policy ....................................................................................................... 42 Resident Leave Restriction Policy................................................................................................................. 43 Policy for Processing Anonymous Evaluations ............................................................................................ 44 Policy for Educational/Career Counseling ................................................................................................... 45 Professional Assistance Policy ................................................................................................................46-48 Attachment A: Substance Abuse and Impaired Physician Policy .............................................49-51 Attachment B: Financial Advice/Counseling Resources ..........................................................52-54 Policy to Address Resident Concerns ........................................................................................................... 55 Grievance Policy for Residents/Fellows ..................................................................................................56-57 Grievance Procedure ................................................................................................................................58-61 Sexual Harassment ........................................................................................................................................ 62 Drug Testing Policy For Training Physicians ..........................................................................................63-65 Policy to Monitor Residents and Fellows with Prior Issues of Concern/ University of Missouri Health Care .............................................................................................................. 66 Disciplinary Action Policy For Residents/Fellows ....................................................................................... 67 Non-Renewal Of A Resident/Fellow Contract at University of Missouri Health Sciences Center .............. 68 Administrative Support for Programs and Residents in the Event of a Disaster or Interruption of Patient Care ............................................................................................................................................................... 69 Process for Requesting a Change in Resident/Fellow Complement or Starting a New Program .................. 70 Reduction In Size Or Closure Of A Residency Program/Fellowship Program ............................................ 71 Consensual Amorous Relationships ............................................................................................................. 72 ACGME REQUIREMENT FOR RESIDENCY TRAINING IN OPHTHALMOLOGY. TAB DIVIDER AAO CODE OF ETHICS ....................................................................................................................TAB DIVIDER MILESTONES .....................................................................................................................................TAB DIVIDER GOALS & OBJECTIVE GME………………………………………………………………………TAB DIVIDER SUB-SPECIALTY SECTION. ............................................................................................................TAB DIVIDER Cornea/External Disease and Refractive Surgery Service ........................................................................74-75 Contact Lens Service ..................................................................................................................................... 76 General Clinic and Emergency Clinic Service .............................................................................................. 77 Glaucoma Service ......................................................................................................................................... 78 Intraocular Service ........................................................................................................................................ 79 Low Vision Service ....................................................................................................................................... 80 Neuro-Ophthalmology and Consultation Service .....................................................................................81-82 Inpatient Consults and Emergency Patients Policy at Women’s & Children’s Hospital ............................... 83 Ocular Pathology. .......................................................................................................................................... 84 Ophthalmic Plastic/Orbital Surgery. ........................................................................................................85-86 Pediatric and Strabismus Service. ................................................................................................................. 87 Vitreoretinal Service.................................................................................................................................88-89 CLINIC ROTATION DESCRIPTIONS. ...........................................................................................TAB DIVIDER First Year Resident (PGY-2) .................................................................................................................90-91 Emergency Service Cornea/External Disease Service Oculoplastics Service Neuro-Ophthalmology/Consults VA Hospital/General Ophthalmology Second Year Resident (PGY-3) . ...........................................................................................................91-93 Retina/Vitreous Service Pediatric/Strabismus Service Third Year Resident (PGY-4) . .............................................................................................................93-95 Cornea/External Disease Service Oculoplastics Service Glaucoma VA Hospital/General Ophthalmology PGY-2 & PGY-4 Resident General Clinics. .........................................................................................96-97 Resident Instruction/Supervision Instruction in Ethical Issues, Socioeconomics of Health Care, Cost-effective Medical Practice (Narrative Description). .............................................................................................................98-99 Harry S. Truman Memorial Veterans’ Hospital VA Hospital Statement of Purpose ................................................................................. 100 Narrative Description for Resident Supervision ......................................................101-103 Resident Supervision-Department of Veterans Affairs ................................................ insert Goals and Responsibilities for VA Ophthalmology Rotation ..................................105-108 Second Year Resident (PGY-3) Responsibilities ......................................105-106 Third Year Resident (PGY-4) Responsibilities .........................................107-108 VA Hospital Policy Memorandum. ............................................................................ Insert Program Letter of Agreement between the Harry S. Truman Memorial Veterans Administration Hospital Eye Clinic and the Department of Ophthalmology. ............. Insert EVALUATIONS ...................................................................................................................................TAB DIVIDER Evaluation Description. ........................................................................................................................111-112 Clinical Skills and Procedures ..................................................................................................................... 113 360-Degree Evaluations .............................................................................................................................. 114 Ophthalmology Resident Global Evaluation Form. ................................................................................. Insert Sub-Specialty Evaluations Forms............................................................................................................. Insert Resident Evaluation of Institution (MEI rotation) .................................................................................... Insert Resident Evaluation of VA Hospital/Eye Clinic (rotation) ...................................................................... Insert Resident Evaluation of Clinical & Courtesy Faculty ............................................................................... Insert Ophthalmic Clinical Evaluation Exercise (OCEX) Form......................................................................... Insert Ophthalmology Resident Surgical Skills Assessment Form ....................................................................... 117 CLINIC POLICIES AND PROCEDURES ........................................................................................TAB DIVIDER Attendance. .................................................................................................................................................. 118 Schedules..................................................................................................................................................... 118 Clinic Support Staff. .............................................................................................................................118-119 Technical Staff. ........................................................................................................................................... 119 Paperwork. .................................................................................................................................................. 120 Documentation Billing Forms Return Patient Forms Phone Messages. ......................................................................................................................................... 121 Guest Relations Patient Injuries/Falls Difficulties Triage Inmates ........................................................................................................................................................ 122 Emergency Patients Surgical Boarding Procedures. .............................................................................................................122-123 Surgery Log 123-124 Definition of Classes Lasers Ultrasound/A & B Scans IOL Master Equipment BILLING AND INSURANCE .............................................................................................................TAB DIVIDER Diagnosis Coding. ....................................................................................................................................... 125 Encounter Form Contact Lenses Surgery Funding. ......................................................................................................................................... 126 Insurance Requirements. ............................................................................................................................. 127 Medicare. ..................................................................................................................................................... 127 Glasses Secondary Cataract (PCO) Blepharoplasty/Blepharoptosis. ................................................................................................................... 127 Photography. ............................................................................................................................................... 128 Insurances. ................................................................................................................................................... 128 Cigna, Coventry, Missouri Care, Mercy Health Plan, Healthcare USA, Mercy Care Partners, Rehabilitation Services for the Blind, Prevention of Blindness Program (POB), Humana HMO/PPO GENERAL PROGRAM INFORMATION. .......................................................................................TAB DIVIDER General Organization of Patient Care at the Mason Eye Institute. ...............................................130-133 Call Curriculum (didactic instruction) Research Conference Attendance Documentation Participation in Medical Student Teaching Annual Contract Description. .................................................................................................................. 133 Absences. .............................................................................................................................................134-137 Vacation, Meetings, Sick Leave, Maternity Leave, Paternity Leave, Holidays, Death In Family, Cancellation of Sub-Specialty Clinics, Unscheduled Time, Unanticipated Absences Moonlighting Policy for Ophthalmology Residents................................................................................ 138 Resident Call & Call Schedule Policy. ..............................................................................................139-140 Educational Allowances & Benefits. .................................................................................................141-142 Days Away Research Cash Professional Allowances Basic Science Course and Books Annual Residents & Alumni Day Ophthalmology Library Computer and Internet Office Assistance Conferences, Exams, and Related Policies. ......................................................................................143-144 Conference Attendance Policy, Attendance Roster, Intra-Department Meetings, Resident Orientation OKAP Examination. ..................................................................................................................... 144 CHIEF RESIDENT RESPONSIBILITIES. .......................................................................................TAB DIVIDER Chief Resident ....................................................................................................................................................145-147 Organize and Conduct Grand Rounds; Coordination and Supervision of Photo Conferences; Review Resident’s daily schedules; Care of Emergency Patients; Coordination of Consult Service (absence of consult resident); Call Schedule; Resident Dictation; Resident Recruitment; Clinic Flow; Co-supervision clinic operations; surgical schedule problems. PROFESSIONAL RESPONSIBILITIES .............................................................................................................. 148 STATEMENT OF PURPOSE/EDUCATIONAL GOALS The purpose of residency training in the Mason Eye Institute, University of Missouri, School of Medicine is to provide an optimal clinical education to physicians in the science and art of ophthalmology; all functions of the department are structured to maximize this educational mission. The program is designed to provide a broad foundation in all of the subspecialties of ophthalmology in a 36month curriculum which combines a structured clinical science course in didactic presentations, clinical conferences and independent study. The department adheres to the ethical standards and practice guidelines as set forth by the American Academy of Ophthalmology, and by example, we wish to instill in the residents this code of ethics. Resident physicians are expected to achieve the 7 ophthalmology competencies of: Patient Care – PC Medical Knowledge – MK Interpersonal and Communication Skills – ICS Professionalism – P Practice-based Learning and Improvement – PBLI Systems-based Practice – SBP Technical/Surgical Skill – TS During the tenure of the residency, residents should accomplish the following: develop a personal program of self-study and professional growth with guidance from the teaching faculty (MK) participate in safe, effective and compassionate medical and surgical patient care under supervision, commensurate with their level of advancement and responsibility (PC,TS,MK,P,SBP) participate fully in the educational activities of their program and, as required, assume responsibility for teaching and supervising other residents and students (PBLI,MK,ICS) participate in institutional programs and activities involving the medical staff and adhere to established practices, procedures and policies of the institutions (ICS,PBLI,P) participate in institutional committees and councils, especially those that relate to patient care review activities (P,ICS,SBP) apply cost containment measures in the provision of patient care (SBP) 2 Roles, Duties, and Responsibilities of Residents Ophthalmology Residents First Year Ophthalmology Resident (PGY-2) Comprehensive Eye Examination (including Indirect Ophthalmoscopy, Manifest and Cycloplegic Refraction) Writes inpatient and outpatient orders Instrumentation: o Lensometry, Automated Keratometry, Automated Refraction o Tonometry, Gonioscopy, Ultrasonic Pachymetry o Static & Kinetic Perimetry (Humphrey, Goldmann) o A&B scan Ultrasonography, Specular Microscopy o IOL Master and Immersion A-scan o Corneal Topography, Slit-Lamp & Fundus Photography o Rust ring remover, Electro-epilator Injections: o Intraocular, Periocular/Retrobulbar, Dermal, Intravenous (including Fluorescein Angiogram) for diagnosis and therapy Run codes (ACLS) Supervised by 2nd or 3rd year resident (until deemed competent) Laser surgery (direct supervision by faculty until deemed competent): o YAG capsulotomy, Peripheral Iridotomy o Argon Panretinal Photocoagulation (PRP), Argon Laser Trabeculectomy (ALT), Peripheral Iridotomy (PI), other Surgery (direct supervision by faculty): o Cataract surgery, Glaucoma surgery, Strabismus surgery o Eyelid surgery, Retina surgery, Cornea surgery, Temporal Artery Biopsy Second and Third Year Ophthalmology Resident (PGY-3 & PGY-4) Above independent after deemed competent, plus: Surgery (direct supervision by faculty of key components): o Cataract surgery, Glaucoma surgery, Strabismus surgery o Eyelid surgery, Retina surgery, Cornea surgery, Temporal Artery Biopsy 3 Insert PDF Dean’s letter of commitment 4 UNIVERSITY OF MISSOURI - HEALTH SCIENCES CENTER PRIMARY VERIFICATION OF CREDENTIALS FOR APPLICANTS TO RESIDENCY AND FELLOWSHIP TRAINING PROGRAMS Programs must select applicants on the basis of preparedness, ability, credentials, communication skills and personal qualities like motivation and integrity. Discrimination by gender, race, color, national origin and disability is prohibited. Restrictive covenants are not permitted. Each program director must be certain each resident/fellow candidate meets all ACGME, general Missouri State Licensing Board criteria and immigration requirements before accepting the individual into the program. The acceptance of unqualified candidates can lead to withdrawal of certification by the ACGME. The primary verification process consists of the following activities: Programs will participate in an organized matching program, such as the National Resident Matching Program (NRMP), if available. A. New US Graduates I. Application for residency/fellowship through the Electronic Residency Application Service (ERAS) serves as primary verification. (Minimum documents required: graduate of MD or DO medical school in the US or Canada which is accredited by LCMF or AOA respectively; medical school transcript, Dean’s letter; United States Medical Licensing Examination (USMLE) Step 1 and 2 scores; reference letters) or: II. Completion of the Universal Residency Application with the above stated documents attached. Transcripts must be verified with the school. B. Foreign-Born and International Medical Graduates (IMG: a physician whose basic medical degree is conferred by a medical school located outside the US, Canada or Puerto Rico) must: 1. Hold J-1 visa (exchange visitor) H-1B visa (temporary worker), immigrant visa or “green card” or an Immigration and Naturalization Service (INS) issued or approved work permit if not a US citizen. 2. Have a full unrestricted license to practice medicine in a US licensing jurisdiction or hold an Educational Commission for Foreign Medical Graduates (ECFMG) Standard Certificate, which is a prerequisite to practice medicine in the US and is an eligibility requirement to take Step 3 of the USMLE. A Standard ECFMG Certificate is issued to an applicant who meets the examination requirements, fulfills the medical education credentialing requirement and clears their financial account with ECFMG. This Certificate is considered valid if the “valid through” dates of the English test and CSA is not later than the program start date. In order for an applicant to obtain permanent validation of the Certificate, ECFMG must receive documentation from an official of the program confirming the applicant’s entry to the program, at which time, ECFMG will provide a “valid indefinitely” sticker to the holder of the Certificate. C. Residents Entering a Program After Completing Preliminary Year at Another Institution - In addition to the requirements of A or B of this policy, requires a: 1. Letter from the program director of the resident’s preliminary year program indicating he/she has successfully completed the preliminary year of training. 5 D. Physicians Entering a Fellowship - In addition to the requirements of A or B of this policy, requires a: Letter from the program director of the resident’s previous program indicating he/she successfully completed the residency program. 6 1. 2. Verification that the completed residency program is accredited and meets the ACGME requirements for entry into that particular fellowship. 3. Reference letter from the Hospital where the physician previously practiced and a National Practitioners Data Bank (NPDB) query, if the fellowship start date is not immediately after residency completion. E. Restrictive Covenants 1. ACGME accredited residencies must not require residents to sign a non-competition guarantee. Revisions approved by the GMEOC: 12/4/07 7 POLICY Graduate Medical Education Committee – Composition & Responsibilities PURPOSE: To define the composition and responsibilities of the Graduate Medical Education Committee (hereafter referred to as GMEC) at UMHC, in accordance with the standards established by the Accreditation Council for Graduate Medical Education (hereafter referred to as ACGME) in the Institutional Requirements GMEC Composition and Meetings The ACGME requires that the sponsoring institution have a GMEC. Voting members on the committee include: The DIO Program Directors (of programs that have 11 or more residents) The House Staff Organization President, President-elect, and Counselors (3) Representatives from Hospital Administration: Chief Quality Officer and Manager UMHC Chief of Staff VA Chief/Associate Chief of Staff Other (non-voting) members include: UMHC Associate Chief Financial Officer and Reimbursement Manager UMC School of Medicine Senior Associate Dean for Education and Faculty Development UMC School of Medicine Associate Dean for Education and Improvement/Research Assistant GME Instructional Design Specialist GME Coordinator Meetings are open to any other program directors who wish to attend, as non-voting members The GMEC is required to meet at least quarterly; the GMEC at UMHC endeavors to meet monthly. The GMEC is required to maintain written minutes of their meetings. GMEC Responsibilities The GMEC establishes and implements policies and procedures regarding the quality of education and the work environment for residents in all programs. These policies and procedures include: Stipends and Position Allocation 8 In collaboration with the GME Resources Committee, the GMEC annually reviews and makes recommendations to UMHC administration regarding resident stipends, benefits, and funding for resident positions. Communication with Program Directors The GMEC ensures that communication mechanisms exist between the GMEC and all program directors within the institution. The GMEC ensures that program directors maintain effective communication mechanisms with the site directors at each participating site for their respective programs to maintain proper oversight at all clinical sites. Resident Duty Hours The GMEC must develop and implement written policies and procedures regarding resident duty hours to ensure compliance with the Institutional, Common, and Specialty/Subspecialty-specific Program Requirements. The GMEC will consider for approval requests from program directors prior to submission to an RRC for exceptions in the weekly limit on duty hours up to 10% or up to a maximum of 88 hours in compliance with ACGME Policies and Procedures for duty hour exceptions. Resident Supervision The GMEC monitors programs’ supervision of residents and ensure that supervision is consistent with Provision of safe and effective patient care Educational needs of residents Progressive responsibility appropriate to residents’ level of education, competence, and experience Other applicable Common and Specialty/Subspecialty-specific Program Requirements Communication with Medical Staff The GMEC facilitates communication between leadership of the medical staff regarding the safety and quality of patient care that includes: The annual report to the OMS Description of resident participation in patient safety and quality of care education The accreditation status of programs and any citations regarding patient care issues Curriculum and Evaluation The GME monitors curriculum and evaluation procedures to assure that each program provides a curriculum and an evaluation system that enables residents to demonstrate achievement of the ACGME general competencies as defined in the Common and Specialty/Subspecialty-specific Program Requirements. Resident Status The GMEC monitors selection, evaluation, promotion, transfer, discipline and/or dismissal of residents in compliance with the Institutional and Common Program Requirements. Oversight of Program Accreditation 9 The GMEC reviews all of the ACGME program accreditation letters of notification and monitors action plans for correction of citations and areas of noncompliance. Management of Institutional Accreditation The GMEC reviews the Sponsoring Institution’s ACGME letter of notification from the IRC and monitors action plans for correction of citations and areas of noncompliance Oversight of Program Changes The GMEC reviews the following for approval, prior to submission to the ACGME by program directors: All applications for ACGME accreditation of new programs Changes in resident complement Major changes in program structure of length of training Additions and deletions of participating sites Appointments of new program directors Progress reports requested by any Review Committee Responses to all proposed adverse actions Requests for exceptions of resident duty hours Voluntary withdrawal of program accreditation Requests for an appeal of an adverse action Appeal presentations to a Board of Appeal or the ACGME Experimentation and Innovation The GMEC provides oversight of all phases of educational experiments and innovations that may deviate from Institutional, Common, and Specialty/Subspecialty-specific Program Requirements, including: Approval prior to submission to the ACGME and/or respective Review Committee Adherence to procedures for “Approving Proposals for Experimentation or Innovative Projects” in ACGME Policies and Procedures Monitoring quality of education provided to residents for the duration of such a project. Oversight of Reductions and Closures The GMEC provides oversight of all processes related to reductions and/or closures of: Individual programs Major participating sites The Sponsoring Institution Vendor Interactions The GMEC supports the UMHC policy that addresses interactions between vendor representatives/corporations and residents/GME programs. Internal Review Process The GMEC develops, implements, and oversees an internal review process. The process is described in the Internal Review Procedure and Protocol Policy. Original Effective date: 7/01/07, approved by GMEC 8/28/07 Amended policy approved 1/6/09, 7/2010 Revisions Approved by GMEC 6/7/11 10 Internal Review Protocol Graduate Medical Education Committee University of Missouri Hospitals and Clinics All accredited graduate medical education programs (residency and fellowship) sponsored by the University of Missouri Hospitals and Clinics (UMHC) undergo a periodic internal review as described in the Institutional Requirements of the Accreditation Council for Graduate Medical Education (ACGME). The review is conducted under the guidance of the Graduate Medical Education Committee (GMEC), which reviews the final report of each internal review and makes recommendations as indicated. The internal review is conducted at approximately the mid-point of the accreditation cycle. (The accreditation cycle is calculated from the date of the meeting at which the final accreditation action was taken to the time of the next site visit.) When a program has no residents enrolled at the mid-point of the review cycle, the following circumstances will apply: The GMEC will demonstrate continued oversight of those programs through a modified internal review that ensures the program has maintained adequate faculty and staff resources, clinical volume, and other necessary curricular elements required to be in substantial compliance with the Institutional, Common and specialty-specific Program Requirements prior to the program enrolling a resident. After enrolling a resident, an internal review must be completed within the second six-month period of the resident’s first year in the program. Internal Review Subcommittee Membership and Responsibilities The GMEC Chair and DIO select the Internal Review Subcommittee for each program being reviewed. Each Subcommittee is chaired by the Internal Review Director. In addition to the chair, the Subcommittee will consist of a faculty member (a program director chosen from outside the program being reviewed), a Resident (chosen by this program director), the GMEC Chair and designated GME Staff (GME Coordinator and GME Instructional Design Specialist). Other members may be appointed at the discretion of the Internal Review Chair. No member of the committee may have a direct relationship to the program under review. The responsibilities of the subcommittee are to review the Internal Review Packet (described below) to conduct interviews with the Program Director, the residents, the program coordinator, faculty and other staff members of the department to provide a final report to the GMEC. 11 Required Questionnaires/Interviews The Program Director Self-Study Questionnaire Includes questions about the educational program, general competencies, evaluation, supervision, scholarship and research and policies. This self-study is sent to the Program Director approximately four months prior to the internal review along with guidelines for the upcoming internal review. The self-study, completed by the Program Director and key teaching faculty, is due one month prior to the internal review so that it can be distributed to the Internal Review Subcommittee. The Resident Questionnaire Includes questions about ACGME Program, Common and Institutional requirements. The Resident Questionnaire is sent to the residents approximately four months prior to the internal review. This questionnaire is due two months prior to the internal review. The resident member of the Internal Review subcommittee, the Chair of the GMEC or the DIO and the GME staff meet with a group of residents in the program (all residents are asked to attend and assure there is at least one from each PGY year) to review the Resident Questionnaire. This meeting occurs approximately one month prior to the internal review meeting so that all materials may be assembled for the Internal Review Subcommittee. A summary of this meeting is placed in the internal review packet. Required Submissions from Program Director to Internal Review Committee One month prior to the Internal Review Subcommittee meeting, the program is required to submit Goals and Objectives for each rotation Evaluation forms – used by residents to evaluate faculty, by faculty to evaluate residents by residents to evaluate the program, final summative evaluation of a recently finishing resident (name blacked out) any other evaluation forms used such as 360, procedure check list, etc. List of educational tools and resources currently being used (i.e. education modules, simulation, etc.) List of conferences during the past year ( if required topics are not covered each year, program should confirm these are part of the didactic curriculum) Most recent completed resident case logs, as applicable; national data on averages, if available Most recent Program Annual Review (with most recent ACGME Resident Survey) Completed PIF from last site visit Program manual Duty hour monitoring data Program Manual Outcome measures (board scores, in-service scores, etc) Program Letters of Agreement A representative resident’s file 12 This material is reviewed by the Chair of the Internal Review Subcommittee, the DIO and GME Staff. A report is prepared and the materials are available for review by the full subcommittee. Internal Review Preliminary Meetings Approximately one month prior to the Internal Review Subcommittee meeting, the Internal Review Director meets with key teaching faculty and staff of the program under review to discuss goals and objectives of the program, research opportunities, clinical and didactic teaching, evaluation and feedback, duty hour issues and recommendations for improving the program. A summary of this meeting is placed in the internal review packet. Internal Review Packet Materials The Internal Review Packet Materials are distributed to all internal reviewers approximately two weeks prior to the internal review preliminary meeting. It includes: The Summary from the last Internal Review; all correspondence/progress reports to the GMEC The most current ACGME Requirements, including Institutional and Common Program Requirements Any correspondence with the ACGME including questions, citations, or progress reports The Program Director Self-Study Questionnaire The Resident Questionnaire – Summary of responses Summary of Faculty Interview Summary of Resident Interview The most recent Annual Program Report (including AGME Resident Survey) Summary of review by the Internal Review Subcommittee Chair, DIO and GME staff of data submitted by the program The Internal Review Subcommittee reviews the packet and formulates a list of issues/questions to be addressed. In addition, a list of additional documents that the committee would like to examine at the time of the internal review is prepared and sent to the department. The Subcommittee then meets with the program director, key teaching faculty and staff to discuss its findings based on the surveys, interviews and review of the submitted materials. They review changes that have been made based on the RRC recommendations, problems with meeting the Program, Common and Institutional Requirements, plans for improvement, and any innovations that have been implemented. . Internal Review Final Meeting The Internal Review Subcommittee assesses the program’s Compliance with the program and institutional requirements Educational objectives and effectiveness in meeting those objectives Educational and financial resources to meet those objectives Effectiveness in addressing areas of non-compliance and concern in previous ACGME letters of notification and internal reviews 13 Effectiveness of educational outcomes in the ACGME core competencies Effectiveness of using evaluation tools and outcome measures to assess the resident’s competence in each of the ACGME core competencies Annual program improvement efforts in resident performance using aggregated resident data, faculty development, graduate performance on certification exams and program quality Internal Review Report and Follow-up Following the meeting, the Chair of the Internal Review Subcommittee prepares an Internal Review Report, which follows a standard template, which includes The name of the program reviewed The date of the assigned midpoint and the status of the GMEC’s oversight of the internal review at that midpoint The names and titles of the Internal Review Subcommittee members A brief description of how the internal review process was conducted, including the list of the groups/individuals interviewed and the documents reviewed Sufficient documentation to demonstrate that a comprehensive review followed the GMEC’s internal review protocol A list of the citations and areas of non-compliance or any concerns or comments from the previous ACGME accreditation letter of notification with a summary of how the program and/or institution subsequently addressed each item Commendations and recommendations for improvement. The summary (report) of the Internal Review is sent to the members of the Internal Review Subcommittee for review. Following their review, the report is then sent to the Program Director for clerical corrections. A final report, with Program Director responses, is then reviewed at the next GMEC meeting. The Program Director is asked to attend this meeting to respond to any questions by the GMEC, which becomes part of the record. Action plans recommended by the GMEC to correct identified deficiencies and recommended monitoring are included in the final report. The approved report is then sent to the Program Director and their Department Chair. The DIO and the GMEC must monitor the response by the program to actions recommended by the GMEC in the internal review process. The Sponsoring Institution must submit the most recent internal review report for each training program as a part of the Institutional Review Document (IRD). If the institutional site visitor simultaneously conducts individual program reviews at the same time as the institutional review, the internal review reports for those programs must not be shared with the site visitor. Revisions Approved by GMEC 6/7/11 14 Cycle of Program Review by GMEC GMEC monitors corrective action plans and reviews and approves any required response or progress report for the ACGME Internal Review process begins 4 months before ACGME identified time for IR. Program self-study, resident questionnaire, faculty and resident interviews PD attends GMEC meeting to review notification letter and present corrective action plans for any citations. GMEC determines schedule for follow up of action plans IR subcommittee reviews materials and develops list of questions for the program director and list of documents to be reviewed at IR. This is sent to the program. ACGME notification letter received by PD and DIO. Date for Internal Review and approximate date for next site visit entered into GME calendar Post ACGME Site Visit Survey from program reviewed by GME staff and periodically reviewed by GMEC for process improvement Internal Review – IR committee meets with PD and coordinator to review the questions and the requested materials IR report written and reviewed by committee and PD, including action plans proposed by the program to address concerns identified by the committee. Site Visit IR report presented to GMEC by IR subcommittee chair with PD present to answer questions. GMEC approves report and determines monitoring schedule for follow up of action plans. GME staff helps prepare PIF. DIO reviews and signs before submission to ACGME Program notified of ACGME site visit and prepares PIF 15 POLICY ON RESIDENT RECRUITMENT, ELIGIBILITY & SELECTION Programs must select applicants on the basis of preparedness, ability, aptitude, academic credentials, communication skills and personal qualities such as motivation and integrity. Discrimination by gender, race, age, religion, color, national origin, disability or any other applicable legally protected status is prohibited. Restrictive covenants are not permitted. Each program director must be certain each resident/fellow candidate meets all ACGME, general Missouri State Licensing Board criteria and immigration requirements before accepting the individual into the program. The acceptance of unqualified candidates can lead to withdrawal of certification by the ACGME. The primary verification process consists of the following activities: Programs will participate in an organized matching program, such as the National Resident Matching Program (NRMP), if available. B. New US Graduates III. Application for residency/fellowship through the Electronic Residency Application Service (ERAS) serves as primary verification. (Minimum documents required: graduate of MD or DO medical school in the US or Canada which is accredited by LCME or AOA respectively; medical school transcript; Dean’s letter; United States Medical Licensing Examination (USMLE) Step 1 and 2 scores or COMLEX score; reference letters) or: IV. Completion of the Universal Residency Application with the above stated documents attached. Transcripts must be verified with the school. C. Foreign-Born and International Medical Graduates (IMG: a physician whose basic medical degree is conferred by a medical school located outside the US, Canada or Puerto Rico) must: 3. Hold J-1 visa (exchange visitor) H-1B visa (temporary worker), immigrant visa or “green card” or an Immigration and Naturalization Service (INS) issued or approved work permit if not a US citizen. 4. Have a full unrestricted license to practice medicine in the State of Missouri or hold an Educational Commission for Foreign Medical Graduates (ECFMG) Standard Certificate, which is a prerequisite to practice medicine in the US and is an eligibility requirement to take Step 3 of the USMLE. A Standard ECFMG Certificate is issued to an applicant who meets the examination requirements, fulfills the medical education credentialing requirement and clears their financial account with ECFMG. This Certificate is considered valid if the “valid through” dates of the English test and CSA is not later than the program start date. In order for an applicant to obtain permanent validation of the Certificate, ECFMG must receive documentation from an official of the program confirming the applicant’s entry to the program, at which time, ECFMG will provide a “valid indefinitely” sticker to the holder of the Certificate. 16 C. Residents Entering a Program After Completing Preliminary Year at Another Institution - In addition to the requirements of A or B of this policy, requires a: 2. Letter from the program director of the resident’s preliminary year program indicating he/she has successfully completed the preliminary year of training and must obtain written or electronic verification of previous educational experiences and a summative competency-based performance evaluation of the transferring resident. D. Graduates of medical schools outside the United States who have completed a Fifth Pathway program provided by an LCME-accredited medical school. A Fifth Pathway program is an academic year of supervised clinical education provided by an LCME-accredited medical school to students who meet the following conditions: (1) have completed, in an accredited college or university in the United States, undergraduate premedical education of the quality acceptable for matriculation in an accredited United States medical school; (2) have studied at a medical school outside the United States and Canada but listed in the World Health Organization Directory of Medical Schools; (3) have completed all of the formal requirements of the foreign medical school except internship and/or social service; (4) have attained a score satisfactory to the sponsoring medical school on a screening examination; and (5) have passed either the Foreign Medical Graduate Examination in the Medical Sciences, Parts I and II of the examination of the National Board of Medical Examiners, or Steps 1 and 2 of the United States Medical Licensing Examination (USMLE). E. Physicians Entering a Fellowship - In addition to the requirements of A or B of this policy, requires a: Letter from the program director of the resident’s previous program indicating he/she successfully completed the residency program. 17 4. 5. Verification that the completed residency program is accredited and meets the ACGME requirements for entry into that particular fellowship. 6. Reference letter from the Hospital where the physician previously practiced and a National Practitioners Data Bank (NPDB) query, if the fellowship start date is not immediately after residency completion. F. 2. Restrictive Covenants ACGME accredited residencies must not require residents to sign a non-competition guarantee. Revisions approved by the GMEOC: 12/4/07; 10/6/09 18 POLICY SUPERVISION and PROGRESSIVE AUTHORITY and RESPONSIBILITY OF RESIDENTS AND FELLOWS (HEREAFTER REFERRED TO AS RESIDENTS) AT UNIVERSITY OF MISSOURI-COLUMBIA HEALTH SCIENCES CENTER Purpose: To set institutional standards for faculty supervision of residents that assures their education and our compliance with ACGME institutional standards. [Note: These standards are not meant to comply with standards required for billing purposes.] Assuring adequate supervision of residents and fellows is the responsibility of the program director, faculty physicians, departments, and the institution. The following are standards for all MU resident and fellow positions, irrespective of where they are training. These are minimum rules. No program can fall below these standards, but they will be expanded if: 1. Medical Staff rules at a given institution exceed these. 2. Additional standards are required by JCAHO, CMS, PATH or other regulatory body. 3. An individual program has more stringent RRC requirements for supervision. 4. The clinical setting where the resident physician is training has additional rules. For example, the Harry S. Truman Memorial Veterans Hospital Policy is described in: Resident Supervision, VAH Handbook 1400.1, March 21, 2000, available in the Resident Coordinators Office or at the VA. Standards All patient care performed by residents during training will be under the supervision of a physician faculty member qualified to provide the appropriate level of care. The specifics of this supervision must be documented in the medical record by the supervising physician or resident. Residents, fellows, and faculty members should inform their patients of their respective roles in each patient’s care. 19 Levels of Supervision: Appropriate supervision of residents must be available at all times. Levels of supervision may vary depending on circumstances or skill and experience of the resident. Definitions relative to levels of supervision are: Direct Supervision: The supervising physician is physically present with both the resident and the patient Indirect Supervision Direct supervision immediately available: The supervising physician is physically within the confines of the site of the patient care and immediately available to provide DIRECT supervision. Direct supervision available. The supervising physician is not physically present within the confines of the site of patient care, but is immediately available by phone, and is available to come in and provide DIRECT supervision. Oversight: The supervising physician is available to provide review of procedures/encounters with feedback provided after the care has been delivered. Supervising Physician: The supervising physician can be a faculty member or a more senior resident than the one needing supervision. Each resident must know the level of supervision required for them in all circumstances. PGY-1 residents must have, at all times, either direct supervision or indirect supervision with direct supervision immediately available. PGY-1’s may not be alone on a hospital service. PGY-1 residents cannot take at-home call. Senior residents or fellows may serve as a supervisor for a junior resident, based on the needs of the patient and the skills of the individual. The supervising physician must be immediately available to the resident or fellow in person or by telephone 24 hours a day during clinical duty. Programs must assure this occurs: Residents must know which supervising physician is on call and how to reach this individual. Contact information and schedules for residents, attending physicians, and other designated patient care individuals should be readily available to all parties involved with patient care The attending physician must clearly communicate to the residents when and under which circumstances they expect to be contacted by the resident concerning patients. At a minimum, the resident must notify the attending of any significant changes in the patient’s condition, including but not limited to: Patient admission to hospital Transfer of patient to intensive care unit Need for intubation or ventilator support Cardiac arrest or significant changes in hemodynamic status Development of significant neurological changes Development of major wound complications Medication errors requiring clinical intervention 20 Any significant clinical problem that will require an invasive procedure or surgery Any condition which requires the response of a special team End-of-life decisions Any patient request to do so Inpatient supervision: The supervising physician must obtain a comprehensive presentation for each admission. This must be done within a reasonable time, but always within 24 hours of admission. The supervising physician must also require the resident to present the progress of each inpatient daily, including discharge planning. All required supervision must be documented in the medical record by the resident and/or the supervising faculty member Outpatient supervision: The supervising physician must require residents to present each outpatient’s history, physical exam and proposed decisions. All required supervision must be documented in the medical record by the resident and/or the supervising faculty member. Transitions of Patient Care: Covered in Transitions of Care Policy. Supervision of consultations: The supervising attending must communicate with the resident and obtain a presentation of the history, physical exam and proposed decisions for each referral. This must be done within an appropriate time but no longer than 24 hours after notification of the consultation request. All required supervision must be documented in the medical record by the resident and/or the supervising faculty member. Supervision of procedures: The supervising faculty physician must be certain that procedures performed by the resident are warranted, that adequate informed consent has been obtained and that the resident has appropriate supervision during the procedure to include sedation. Whenever there is more than minor risk to the patient, the supervising physician must be present during the key part of the procedure. All required supervision must be documented in the medical record by the resident and/or the supervising faculty member. Supervision of emergencies: During emergencies, the resident should provide care for the patient and notify the supervising physician as soon as possible to present the history, physical exam and planned decisions. All required supervision must be documented in the medical record by the resident and/or the supervising faculty member. Progressive authority and responsibility for Residents: Increasing responsibility for patient care is an integral part of the medical education process. Specific roles and tasks for patient care must be assigned by program directors and faculty members. 21 Roles and responsibilities for residents are determined by the program director. Decisions for individual residents must be based on specific criteria and evaluation based on specific national standards-based competencies. Faculty members in the role of attending/supervising physicians should delegate portions of patient care to residents based on the needs of the patient and the skills and experience of the resident. Each resident must know the limits of his/her scope of authority and responsibility and the circumstances under which varying levels of supervision apply. Faculty supervision assignments to individual residents should be of duration adequate to assess the knowledge, level, and scope of residents and to delegate and observe the resident in circumstances of increasing patient care responsibility V. Common questions: VI. When does the supervising physician have to come in to see a patient? This would be typical of expected practice, or whenever the resident asks the supervising physician to be present or whenever CMS or Medical Staff rules require this. VII. To whom are faculty responsible for resident supervision? The program director, the chair of the department, the GME Oversight Committee and the Dean of the School of Medicine for educational supervision. The supervising physician is also responsible for CMS documentation requirements and Medical Staff rules. Approved by the GMEC: 5/2/00 Revised/Approved by the GMEC: 9/2/03 Revised/Approved by the GMEC: 3/12/04 Revised/Approved by the GMEC: 6/7/11 22 Policy Teamwork University of Missouri-Columbia Residents must care for patients in an environment that maximizes effective communication. This must include the opportunity to work as a member of effective interprofessional teams that are appropriate to the delivery of care in the specialty. Adopted May 2011 GMEC Approved 6/7/11 23 POLICY Transitions of Care PURPOSE: To establish protocol and standards within the Graduate Medical Education Committee at the University of Missouri to ensure the quality and safety of patient care when transfer of responsibility occurs during duty hour shift changes and other scheduled or unexpected circumstances. STANDARDS: Individual programs must design schedules and clinical assignments to maximize the learning experience for residents as well as ensure quality care and patient safety, and adhere to general institutional policies concerning transitions of patient care. Transitions of care are necessary in the hospital setting for various reasons. The transition/hand-off process is an interactive communication process of passing specific, essential patient information from one caregiver to another. Transition of care occurs regularly under the following conditions: Change in level of patient care, including inpatient admission from an outpatient procedure or diagnostic area or ER and transfer to or from a critical care unit. Temporary transfer of care to other healthcare professionals within procedure or diagnostic areas Discharge, including discharge to home or another facility such as skilled nursing care Change in provider or service change, including change of shift for nurses, resident signout, and rotation changes for residents. The transition/hand-off process must involve face-to-face interaction with both verbal and written communication. The transition process should include, at a minimum, the following information in a standardized format that is universal across all services: Identification of patient, including name, medical record number, and date of birth Identification of admitting/primary physician Diagnosis and current status/condition of patient Recent events, including changes in condition or treatment, current medication status, recent lab tests, allergies, anticipated procedures and actions to be taken. Changes in patient condition that may occur requiring interventions or contingency plans Each program must develop components ancillary to the institutional transition of care policy and that integrate specifics from their specialty field. Programs are required to develop scheduling and transition/hand-off procedures to ensure that: 24 Residents do not exceed the 80-hour per week duty limit averaged over 4 weeks. Faculty are scheduled and available for appropriate supervision levels according to the requirements for the scheduled residents. All parties involved in a particular program and/or transition process have access to one another’s schedules and contact information. All call schedules are available on the MUHC MyApps website and with the hospital operator. Patients are not inconvenienced or endangered in any way by frequent transitions in their care. All parties directly involved in the patient’s care before, during, and after the transition have opportunity for communication, consultation, and clarification of information. Safeguards exist for coverage when unexpected changes in patient care may occur due to circumstances such as resident illness, fatigue, or emergency. Each program must include the transition of care process in its curriculum. Residents must demonstrate competency in performance of this task. Programs must develop and utilize a method of monitoring the transition of care process and update as necessary. GMEC Approved 6/7/11 25 26 Ophthalmology Monitoring of Patient Hand-off (On-Call and In-Patients) The accreditation Committee for Graduate Medical Education (ACGME) requires the following: a) An effective, structured transition of patient care that facilitates continuity of care and patient safety; b) Residents are competent in communicating with team members in the hand-over process; and c) The availability of schedules that inform all members of the health care team of attending physicians and residents who are currently responsible for each patient’s care. In accordance with the ACGME requirements regarding Transition of Care, the Ophthalmology Department publishes monthly (with updates as needed) a schedule of residents and attending faculty members who are on-call for emergency outpatients or in-hospital patients. The following policy is also undertaken: For patients who are currently in the hospital and whose eye care is being supervised by the Ophthalmology Department, the resident caring for the patient on a daily basis will discuss the patient care with the on-call resident, prior to the end of the working day and the following morning to ensure effective communication and transfer of care; For patients who are currently in the hospital and who previously had not been evaluated by the Ophthalmology Department (i.e., new inpatient consult), the on-call resident will discuss the patient care with the attending faculty on-call at that time or by the following morning, to ensure effective communication and transfer of care; For patients who are evaluated through the Emergency Room and who have on-going issues (e.g., acute glaucoma, corneal ulcer, etc.), the on-call resident will discuss the patient care with the attending faculty on-call at that time or by the following morning, to ensure effective communication and transfer of care. 27 HOUSE STAFF COMPLIANCE WITH TIMELY COMPLETION OF MEDICAL RECORDS Objective: To outline a process that will be used to assure the timely completion of patient medical records (MR) by House Staff at University Hospitals and Clinics (UHC), in compliance with the Medical Staff policy MS-01: Suspension of Privileges – Delinquent Inpatient Medical Records. To provide a process that holds residents accountable for their role in the timely completion of patient records and therefore facilitates appropriate continuity of patient care and contributes directly to UHC’s ability to meet regulatory expectations on MAR completion. Policy: House Staff must complete all elements of the MR for which they are responsible within fifteen (15) business days of patient discharge. As directed by UHC’s Medical Staff Rules and Regulations, such items for completion include signing of the history and physical, discharge summary, operative notes and verbal orders. Failure to do so may result in negative evaluations citing failure to meet proficiency in the core competency professionalism. All requests for verification of affiliation or education during search for employment will include a response that evaluations during residency training indicate issues identified with regard to timely MR completion. Department-specific methods may be used to ensure compliance with this policy. For programs choosing to develop a different process from that prescribed within this policy, approval of the plan shall be sought through the Graduate Medical Education Oversight Committee before implementation. Proposed Process: 1. All practitioners will have immediate notification of, and access to, all MR items requiring signature via their electronic MR Inbox. 2. In addition, the Medical Records Department will assure multiple notifications of items requiring signature by using the following steps: A. Effective November 7, 2006, all unsigned documents will remain visible in a user's Inbox until they are either signed or appropriately refused and forwarded back to medical records. B. Every Tuesday, Medical Records staff will hand-deliver lists of deficiencies that are older then 7 days to each department for notification to physicians. C. Every Tuesday, via e-mail, the Medical Records Document Completion supervisor will also notify Department Chairs, Department Administrators and Residency Program Directors (PDs) of all MR items that are delinquent at 15 days or older requiring dictation. 3. Once a week, Medical Records staff will send a listing of all delinquent record items to the Residency PDs for final notification to the responsible residents. This will include all 28 unsigned items that are 21 days post-discharge. At this point, following notification by the PDs, the resident will be expected to complete the records within 10 business days. 4. As these weekly reports continue to be provided, the PDs are encouraged follow the following steps with residents who have delinquent items reported: A. Verbal counseling – For the first occurrence, the PD will meet with the resident to detail the concern, including the date of the event. The resident’s explanation will be heard and documented. B. Letter of formal counseling – For the second occurrence, the PD will inform the resident of the delinquency incident, document the details of the concern in a formal letter of counseling and then meet with the resident to discuss the event and expectations for resolution. C. Formal counseling reevaluation – The PD will meet with the resident for reevaluation three months following the second occurrence, or sooner if another delinquent record incident occurs. If the meeting is a result of a third incident, the information will be documented in a letter that both the PD and the resident will sign. It will then be forward to the Department Chairman for signature and additional recommendations for action. At the third incident, formal documentation of failure to meet professionalism expectations will be included in the resident’s formal evaluation file. 5. If the resident has additional incidents, or shows persistent deficiency in ability to meet this professional proficiency or other core competencies, the PD may determine the need to engage disciplinary steps as determined by the program and may result in actions such as program-level remediation and subsequent formal probation. Approved by the Graduate Medical Education Oversight Committee - 12/5/06 29 Policy: Resident/Fellow Stipends Effective: July 1, 2007 Approved by the GMEOC: 8-28-07 The GMEOC, in collaboration with the GME Resources Committee, reviews the Association of American Medical Colleges (AAMC) Council of Teaching Hospitals (COTH) annual resident stipend report, which is received by the GME Office in November/December each year. This report is used as a guide in determining salaries for the upcoming academic year, July 1 – June 30. Proposed salaries are based on data reported for the Midwest during the previous year and are presented to Hospital Administration for final approval. 30 BLS/ACLS/PALS Certification (Basic Life Support / Advanced Cardiac Life Support / Pediatric Advanced Life Support) 31 All residents/fellows who have direct contact with patients must maintain active certification in BLS and ACLS which has been endorsed by the American Heart Association. Exceptions to certification include: - - Pathology residents will not be mandated to take BLS or ACLS. General Surgery residents will be required to take BLS and ACLS as new residents and will only be required to maintain current certification in ATLS for the duration of training. Pediatrics residents will be required to maintain BLS, PALS and NRP certification for the duration of training and will not be required to be ACLS certified. PALS (certification must be endorsed by the American Heart Association): - Family Medicine residents must maintain PALS certification (in addition to BLS, ACLS) Med/Peds residents must maintain PALS certification (in addition to BLS, ACLS) GMEOC approved 2/5/02 GMEOC approved amended policy 4/3/07 GMEOC approved amended policy 7/1/98 32 Step 3 / COMLEX Exam Requirements Policy: To define requirements for passing USMLE Step 3(for MDs) and COMLEX (for DOs) prior to completing the training program Effective: For All New Training Physicians starting July 1, 2009, and after All residents are required to pass Step 3 of USMLE (for MDs) or COMLEX (for DOs) prior to starting their final year of residency, and all fellows are required to pass the respective exam during their first year of training. Evidence of successful completion of this exam must be given to the program director and kept in the resident’s file. Residents are encouraged to take the exam by early in the PGY 2 year, in order to allow remediation if necessary. Failure to provide evidence of successful completion of Step 3 of USMLE for MD physicians or COMLEX for DO physicians prior to beginning the final year may result in non renewal of the contract and dismissal from the program. Individual training programs may have requirements for successful completion of the exam prior to the timeline outlined above. Approved by the GMEOC: August 5, 2008 Revision Approved: February 3, 2009 33 POLICY: Reporting of Other Learners in a Program Effective: 7-1-07 Approved by the GMEOC: 8-28-07 The presence of other learners (including, but not limited to, residents from other specialties, subspecialty fellows, PhD students and advance practice nursing students) in the training program must not interfere with the appointed resident/fellow’s education. The presence of other learners during the current academic year must be reported in the program’s Annual Report to the GMEOC. 34 Moonlighting Professional Activities Outside the Educational Program Policy: The ACGME requires that the institution assure that each training program maintains a policy that specifies moonlighting conditions, including both internal and external moonlighting, and setting forth specific requirements for such activity. The moonlighting policy, whether it is allowed by individual programs or not, is to be referenced in each trainee contract. Purpose: This policy has been created to: Provide an institutional policy that guides and provides a basis upon which programs will develop their own specific policies. Inform and protect Housestaff who choose to moonlight while training at University of Missouri Healthcare, Columbia (hereafter referred to as UMHC). Residents who consider moonlighting and/or other professional activities outside of the UMHC educational program must adhere to the requirements, standards, and definitions listed below: Requirements, Standards, and Definitions: Housestaff: Residents and fellows who are physicians in training for Board certification Required to have a temporary or permanent Missouri medical license Are provided UMHC malpractice insurance during official training activities. Billing, directly or indirectly, for services during such training hours is not permitted Internal Moonlighting Internal Supervised Resident Activity (ISRA) Elective resident/fellow participation in patient care within their specialty program and license that exceeds ACGME and program requirements. ISRA includes an additional stipend, but must be voluntary Must be on the UMHC clinics and campuses or at a UMHC site where training normally occurs Must be rendered under GME Oversight Committee approval with the same faculty supervision, attending billing, and documentation rules Must be at a level of clinical responsibility that is appropriate for the resident’s level of training An individual resident or fellow may voluntarily choose to participate in this elective responsibility, if offered the opportunity by their program, upon successful completion of the PGY-1 year. 35 This activity is counted as part of the resident’s regular duties in the 80-hour per week duty requirement. A resident or fellow wishing to participate in internal moonlighting must have written permission to do so and this documentation must be maintained in the resident/fellow file. A PGY-1 resident is not eligible for internal moonlighting at any time or under any circumstance. External Moonlighting: 36 External moonlighting is voluntary medical practice/work done by residents or fellows outside of his or her training program and outside the scope of training. Standards applicable to external moonlighting: Any resident or fellow wishing to moonlight must receive written approval to do so from their program director Written permission from the program director must be stored and maintained in the resident/fellow file. Moonlighting must be approved by the Department Chairman and the Program Director of the training program of the individual, with determination and assurances that moonlighting is not detrimental to the resident’s training in any significant way. The program director must monitor the moonlighting activity to ensure that the resident/fellow does not become excessively fatigued. The program director may limit or suspend moonlighting activity, either individually or unilaterally, if excessive fatigue or interference with the required training activities is found. External moonlighters, since they are functioning as attending physicians, must: Hold permanent licenses (Missouri medical, Federal narcotics (DEA) and State Narcotics (BNDD) before beginning any moonlighting work. Have medical staff privileges and malpractice coverage for the patient care they will provide. External moonlighting can be a medical practice outside of the training program, but within a UMHC location or under a UMHC. In this situation, UMHC provides for malpractice coverage and any related legal representation. A permanent State of Missouri license and Medical Staff privileging and credentialing are still necessary. CMS requires that for in-house moonlighting, the training institution must have a contract with each resident/fellow that specifies the moonlighting is separate from ACGME training and is done under a regular state license and for CMS approved medical services. A resident/fellow moonlighting at any health care entity which is not a part of UMHC requires that arrangements be made between the moonlighter and the health care entity for malpractice coverage and related legal representation. The moonlighter is operating independently of UMHC and must assume no such coverage exists unless these arrangements have been completed. External moonlighters are subject to all local, state, and federal laws that apply to attendings when and where they moonlight. All moonlighting must comply with Visa guidelines. Certain Visas do not allow work outside the normal activity of the training program. Each program must create a policy that complies with this UMHC Policy and place this and the institutional policy in the program manual. Programs may choose to permit, nor permit or limit moonlighting. Program policy should require that moonlighting will not interfere with Housestaff training responsibilities/schedules or contribute to excessive fatigue, as well as stipulate consequences for Housestaff who do not comply with the training program policy. Moonlighting must not interfere with the ability of the resident to achieve the goals, objectives, and responsibility of their training program. Time spent moonlighting, both internal and external, must be counted in the 80-hour per week duty hour maximum. PGY-1 residents are not permitted to moonlight under any circumstances. GMEOC Approval 6/15/9 Dean Approval 6/24/99 Revisions Approved GMEC 5/2/00 Revisions Approved GMEC 10/05/05 Revisions Approved GMEC 02/02/10 Revisions Approved GMEC 6/7/11 37 Health Sciences Center Moonlighting Policy J-1 or H-1B Visa Holders In the June 30, 1999, Federal Register the USIA (United States Information Agency) outlined policies regarding moonlighting of non-resident aliens with visas. J-1* visa holders are prohibited to obtain employment that is not a part of their training program. H-1B** visa holders are also prohibited from moonlighting unless specifically allowed, as specified, in their visa. Any resident or fellow in a training program at the University of Missouri who fails to comply with this regulation is at risk for deportation. To ensure compliance with this regulation, the following process will be followed: 1. Any resident/fellow wishing to moonlight must receive approval to do so from their program director. Moonlighting must be approved by the Department Chairman and Resident Program Director of the training program and these individuals should assure that moonlighting is not detrimental to training in any significant way. (Please refer to the “Professional Activities Outside the Educational Program” policy of the Health Sciences Center for moonlighting requirements.) 2. The Department Chairman and/or Resident Program Director must verify visa status. If it is determined that the resident/fellow wishing to moonlight is a J-1visa holder, the Chairman and/or Resident Program Director will not allow the resident/fellow to moonlight. 3. If it is determined that the resident/fellow wishing to moonlight is an H-1B visa holder, the Chairman and/or Resident Program Director must request that the resident/fellow submit his H1B visa documents for review by the University of Missouri Legal Counsel to determine whether the stipulation for outside employment is written in the visa. If moonlighting is not specifically allowed in the visa, the Chairman and/or Resident Program Director will not allow the resident/fellow to moonlight. 4. Each program must create a policy that complies with this Health Sciences Center Institutional Policy and place this and the institutional policy in their program manual. 38 Policy for Payment of Fees Associated with an H1B Visa As part of the H1B petition, the employer, serving as the petitioner of the H1B visa, is responsible for the INS filing fees, costs and legal fees incurred for the petition of the H1B visa. (All programs must contact Nancie Hawke, UMC Legal Counsel, to be referred to a list of legal representatives who are approved to file petitions on behalf of the training physician.) The following fees will be equally shared between University Hospitals & Clinics and the department accepting a training physician requesting an H1B visa. These costs will apply to new petitions in addition to yearly renewals. 1. Application/Filing Fee 2. All legal fees associated with processing the H1B petition The department will pay all costs initially. Documentation of payments made should be sent to the GME Office with a request for reimbursement of half the total costs incurred. The following fees will be the sole responsibility of the training physician. This must be disclosed to the training physician at the time of inquiry or in discussion about application for H1B visas. 1. Fees to expedite the H1B visa 2. A one-time anti-fraud/homeland security fee of $500* * If a department chooses, they may pay this fee, in hardship cases. In this circumstance, the cost is the full responsibility of the department. Approved by the Graduate Medical Education Oversight Committee 1/3/06 39 Policy Professionalism, Personal Responsibility, and Patient Safety Purpose: Standards: University of Missouri To set institutional standards for education of residents and faculty concerning their professional and personal responsibilities for the safety of their patients. Programs must work to assure the health and well-being of residents, the safety of patients and an excellent educational experience for the residents. The programs must develop scheduling that adheres to the 80-hour per week duty hour requirements as set forth in the GMEC Duty Hours Policy as well as develop procedures for transitions of care and education on alertness, fatigue, and sleep deprivation, in accordance with GMEC policies. Programs must educate residents and faculty concerning the professional duty of physicians to appear for duty rested, alert, and ready to provide services to patients. Programs must develop education and scheduling policies to maximize patient safety and resident well-being. Programs must require residents to actively participate in interdisciplinary clinical quality improvement and patient safety programs. Programs must provide to residents an appropriate blend of supervised patient care responsibilities, clinical teaching, and didactic education. Programs must ensure that there is not an excessive reliance on residents to fulfill nonphysician service obligations. Programs must include in the curriculum the importance of a culture of professionalism that promotes patient safety and responsibility and the resident’s personal responsibility in: Assuring the safety and welfare of patients entrusted to their care Providing patient- and family-centered care Assuring their fitness for duty Management of their time before, during, and after clinical assignments Recognition of impairment, including illness and fatigue, in themselves and in their peers Attention to life-long learning Monitoring of their patient care performance improvement indicators Honest, accurate, and timely reporting of duty hours, patient records and outcomes, and clinical experience data. Programs must ensure that residents understand their personal responsibility to put the patient’s needs ahead of their own and that there will be situations when transitioning the patients care to another physician may be in the best interest of the patient. GMEC Approved 6/7/11 40 Duty Hour Policy For the University of Missouri Purpose: To set institutional standards for resident duty hours and in-house on-call frequency that ensure resident duty hours are not excessive. Standards: Resident duty hours should both foster resident education and facilitate the care of patients. The educational goals of each residency program and the learning objectives of the residents must not be compromised by excessive reliance on residents to fulfill institutional service obligations. However, duty hours must reflect the fact that responsibilities for continuing patient care are not automatically discharged at specific times. Programs must ensure that residents are provided appropriate back-up support when patient care responsibilities are especially prolonged or difficult. Each residency program must adhere to the duty hour limitations set by their individual RRC (Residency Review Committees) and the ACGME institutional requirements. The structuring of duty hours and oncall schedules must focus on the needs of the patient, continuity of care and the educational needs of the resident. Duty hours must be limited to 80 hours per week, averaged over a four-week period, inclusive of all in-house call activities and all moonlighting hours. Internal and external moonlighting hours must be counted as part of the resident’s total work hours. Some specialties do not allow averaging. Residents must be provided with 1 (one) day (24 hours) in 7 (seven) free from all educational and clinical responsibilities, averaged over a four-week period, including conferences. No at-home call can be assigned during any of these 24-hour periods. Mandated time off between assigned “shifts” (duty periods) must be provided to allow adequate time for rest and personal activities. 41 PGY-1 residents must have 8 hours, but should have 10 hours, off between scheduled shifts. Intermediate-level residents (defined by program-specific RRC) must have 8 hours, but should have 10 hours, off between scheduled shifts. Also, they must have 14 hours free after a 24-hour period of in-house duty. Senior-level/chief residents (as defined by program-specific RRC) must be prepared to enter the unsupervised practice of medicine and care of patients over irregular and extended periods. This preparation must occur within the context of the 80-hour maximum duty period length and 1-day free in 7 standards. While it is desirable to have 8 hours off between shifts, there may be circumstances when these residents must stay on duty to care for their patients or return to the hospital less than 8 hours after their prior shift. These instances must be monitored by the program director. On-call Activities No resident may have more than 6 nights of consecutive night-float duty. Continuous On-Site Duty PGY-1 residents may not exceed 16 hours of continuous duty. These 16 hours include educational conferences, hand-offs, etc. No new patients may be accepted after 16 hours of continuous duty. PGY-2 and higher residents may not exceed 24 hours of assigned continuous duty, but an additional 4 hours (totaling 28 hours) may be used for hand-offs and educational activities. However, there should be no additional clinical activities during these additional 4 hours (clinics, consultations, etc.). In unusual circumstances a senior-level resident may choose voluntarily to stay beyond his/her assigned duty period to provide care to a single patient. These instances must be documented as to the educational validity by the program director. The care of other patients on the service must be turned over to another physician. No new patients may be accepted after 24 hours of continuous duty. Maximum In-House Call Frequency PGY-1 residents are not eligible for in-house call immediately following daytime duty hours. PGY-2 and higher residents can have in-house call no more frequently than every third night averaged over 4 weeks. At-home call (or pager call) The frequency of at-home call is not subject to the every-third-night, or 24+6 limitation. However at-home call must not be so frequent as to preclude rest and reasonable personal and study time for each resident. Residents taking at-home call must be provided with one day (24 hours) in seven completely free from all educational and clinical responsibilities, averaged over a four-week period. When residents are called into the hospital from home, the hours residents spend in-house are counted toward the 80-hour limit. Internal and external moonlighting must be considered part of the 80-hour weekly limit on duty hours. PGY-2 or higher residents may come in at night to see established or new patients and this will not violate the 8-10 hour rule, but they must count the time in-house as part of their work hours PGY-1 residents are not eligible for at-home call. Sleep Facilities and Safe Transportation Home Options. Refer to Alertness Management/Fatigue Mitigation Policy. Continuity of Care. Refer to Transitions of Care policy GMEC Approved 6/7/11 42 POLICY Alertness Management and Fatigue Mitigation It is essential to the education, health and well-being of residents/fellows and the safety of patients that faculty and residents alike develop awareness of the symptoms and dangers of physician fatigue. It is a requirement of the ACGME for all residency programs to educate faculty and residents concerning alertness and fatigue, require that faculty and residents participate in such educational experiences, and to document and monitor such participation. Evidence based literature indicates that fatigue impacts resident/fellow learning and well-being. Duty hour requirements are part of the solution, but such requirements do not address all issues relevant to alertness and fatigue. Research indicates that most people do not realize they are sleepy until they are extremely fatigued. Psychomotor function after 24 hours without sleep is equivalent to a blood alcohol content level of 0.08%, a level recognized legally as inebriation. As with alcohol impairment, individuals may not be able to evaluate their own degree of fatigue. Causes of fatigue include: Too little sleep. Most adults require an average of 8.2 hours of sleep per night. Fragmented sleep. When sleep is interrupted, a person may not have sufficient time spent in the deeper, restorative stages of sleep. Circadian Rhythm disruption. Circadian rhythms are the body’s internal biological clock, managing system functions throughout a 24-hour period. Frequent disruption of sleep schedules, as in extended duty hours or shift changes can result in fatigue and sleep deprivation. Other conditions, including anxiety, depression, medication, and physical illness. Sleep debt can occur with as little as 2 hours less sleep than usual. Incidents of less than optimal sleep time over several nights will increase the deficit. Sleep debt requires several consecutive nights of optimal sleep for recovery. Symptoms of sleepiness/fatigue include: Repeated yawning and “nodding off” at inappropriate times Microsleep—a few seconds of sleep that an individual may not even recognize Increased tolerance for risk Inattention to details Decreased cognitive functions Increased errors Accidents, especially automobile accidents In the interest of the health and well-being of residents and patient safety, the GMEC requires: Educational experiences must be developed in each program to educate both faculty and residents to recognize the causes, symptoms, and remedies for sleep deprivation, including recognition of impairment in others and their personal responsibility to be well-rested and alert when on duty. 43 Participation in sleep deprivation educational experiences must be documented and monitored by each program In accordance with duty hours and transition of care requirements, each program must have a process in place to ensure continuity of care in the event that a resident may be unable to perform patient care duties due to fatigue, illness, or other impairments. Faculty, residents, and other health care personnel must be trained in the process of recognizing fatigue, illness, or other impairments in their colleagues and encouraged to intervene when necessary to maintain the health and well-being of their colleagues and the safety of patients. Residents must be educated concerning possible short-term strategies for counter-acting sleep deprivation symptoms, including napping and occasional moderate use of caffeine Residents must be educated as to their personal responsibility to appear for duty on-time, appropriately rested, and otherwise fit for duty. Residents must demonstrate compliance with their responsibility for their own health and wellbeing by careful management of their time before, during and after duty hours. Accurate and timely reporting of duty hours is mandatory. Each program must make sure that adequate sleep facilities/on-call rooms are available for their residents. Such facilities are provided by UMHC. Each program must ensure that residents know the location and scheduling of the sleep facilities/on-call rooms. These facilities are available before, during, and after a resident’s duty hours. To enable residents with the opportunity for safe transportation home in the event of fatigue, illness, or other impairment, each resident will be given a voucher to use for a taxicab ride home. The resident is responsible for returning the receipt for the service in a timely manner, including documentation of the reason for the transportation. (This process is in development at this time and updates will be provided to GMEC as soon as details are determined.) Resources Duke University, Prevention, Identification, & Management of Fatigue in Graduate Medical Education, November 11, 2010. http://www.gme.duke.edu/newsletters/2010December/Fatigue_11-16-2010.pdf University of Tennessee College of Medicine, Alertness and Fatigue Management Policy, April, 2011. http://www.uthsc.edu/GME/policies/fatigue2011.pdf University of Colorado Denver School of Medicine Duty Hours Policy, June 2011. http://www.ucdenver.edu/academics/colleges/medicalschool/education/graduatemedicaleducation/GMEDocuments/ Documents/4.Policies%20and%20Procedures/GME%20Duty%20Hours%20Policy.pdf GMEC Approved 6/7/11 44 INSTITUTIONAL VACATION AND LEAVE POLICY Purpose: The ACGME requires an Institutional Leave Policy that is known to all Residents. Each program must have its own vacation and professional leave policy that it makes available to its residents/fellows before they sign their contracts and that: • Follows ACGME program requirements. • Complies with MU’s Family Leave Policy. To review this policy in context, please visit our website at: http://www.umsystem.edu/ums/departments/hr/manual/ If you have questions or comments about the revisions, please contact your campus human resource office. The institution will fund up to one month each year of any combination of vacation and leave for each resident. To hold a GME position for their return, residents/fellows must obtain written approval from their department for leave/vacation that exceeds one month per year. Adverse decisions, as always, may be appealed through the Policy to Address Resident Concerns, and then as a grievance. 45 Resident Leave Restriction Policy A program director (PD) may specify the rotations on which their residents may take leave (as defined by your program). Residents rotating outside their department may take up to one week (5 week days and one weekend) of leave on rotations of 4 weeks (or one month) unless a restriction has been mutually agreed upon by both PDs. If a resident rotates to another department for longer than 4 weeks (one month), the proportion of their leave allowed on those rotations should be proportional to the time on those rotations. (e.g. if a neurosurgery resident rotates for 3 months on general surgery, they should be allowed to take ¼ (3/12) of their leave while on those rotations. Leave should be scheduled and agreed upon between the two program directors. If no agreement is reached, the GMEOC will arbitrate. The decision will be determined by a majority vote of the members present. Approved by the GMEOC 7/7/09 46 POLICY FOR PROCESSING ANONYMOUS EVALUATIONS The ACGME requires that faculty members sign evaluations they complete of training physicians. Programs may elect to have additional health care staff evaluate the training physician, including peers or other co-workers (i.e., nursing staff, techs). These evaluations should be kept anonymous from the training physician being evaluated, to the extent possible under the law. Anonymity may be maintained by having a summary of these evaluations prepared by the program director or coordinator, which is then placed in the training physician file. The evaluation instrument itself may be destroyed or, if kept, assurance should be made that the anonymity of the evaluator will be maintained. Approved by the Graduate Medical Education Oversight Committee1/3/06 47 POLICY FOR EDUCATIONAL/ CAREER COUNSELING Occasionally, a residency program director will request that a resident receive evaluation and counseling for a problem they are having. This is usually done by members of the UMC Psychiatry Department, although a program director may request evaluation by someone outside the department or outside the University. The following guidelines should be followed. 1. The request for evaluation must be in writing from the program director with a general statement of the reason for the request. 2. The evaluator will keep a record of the encounter(s) but not as part of the resident’s medical record. Appropriate confidentiality will be maintained. 3. The evaluator will update the program director regarding the resident’s progress. At the outset, the resident will be informed that the program director will receive updates from the evaluator. The resident will discuss with the evaluator what information will be shared to maintain confidentiality. 4. If a mental health disorder or substance abuse is found during the course of evaluation or counseling, appropriate referral to the health care system will be made. All University and State of Missouri requirements for reporting must be followed. 5. The requesting department is responsible for the cost of the evaluation and counseling. If referral is made to the health care system, the resident’s insurance will be billed, and the resident will be responsible for any other expenses (just as with any other medical condition). 48 PROFESSIONAL ASSISTANCE POLICY Policy: The policy of providing assistance to residents and fellows is delineated for the following conditions: 1) Mental Health; 2) Physical (Medical) Health; 3) Impaired Physicians; and 4) Financial. All requests for resource information will be treated confidentially. The Associate Dean for Medical Education will be the safety net to help trainees who feel they cannot get what they need through their Program Director. The Associate Dean will also be a resource to Program Directors in solving trainee issues. This individual or designee may be contacted at any time for emergencies. Purpose: Graduate Medical Education can be a stressful time for residents and fellows. It is our job to nurture and support our trainees so each is the best person and physician that he or she can be. The program directors are charged by their Residency Review Committees (RRCs) to monitor stress, depression, mental and/or physical illness of their trainees, and to assist in obtaining treatment and/or identifying methods of counseling. The institution is required by the ACGME to facilitate resident/fellow access to appropriate and confidential counseling, medical, and psychological support services. This includes the stipulation of written policies describing how physician impairment, including substance abuse, will be handled. Definitions: Substance Abuse: Use of alcohol or drugs with resulting diminution of ability to carry out responsibilities in the workplace. Resident Physicians: Resident or fellow trainees Impaired Physician: Physician is unable to perform trainee duties, in best judgement of the Health Sciences Center Physician Health Committee. General Information: All trainees are enrolled in the University of Missouri group plans for life insurance, long term disability, and medical benefits. This coverage includes medical treatment as well as psychiatric counseling and treatment. In addition, the Housestaff Organization has arranged for additional disability coverage at the individual trainee’s expense. Medical/Physical Health Time off for treatment of medical or physical conditions will be granted in accordance with the program’s specifics for medical leave of absence. The trainee may refer to their training manual for this information or contact their program director. Emotional/Psychological Psychological illness such as short term psychological problems of situational distress, anxiety, or stress, may result in impairing the ability to perform assigned job responsibilities. Please refer to number 3 above and Attachment A, for information on actions required by the Medical School. Treatment for such illness is generally covered by existing health benefits. Impaired Physicians Residents or Fellows with substance abuse problems should be aware that the Health Sciences Center’s policy is nonpunitive if the treatment plan is adhered to, except as identified in Attachment A, item B,5 of the “Substance Abuse Policy for Clinical Faculty and Resident 49 Physicians, ” which states that probable cause of impairment due to substance abuse will result in a report to the Missouri Physician’s Health Committee (MPHC) for further investigation and action. In accordance with laws regarding reporting, the MPHC will be required to report substantiated substance abuse to the National Practitioner Data Bank. Also, please reference the University of Missouri policy on drug/alcohol abuse – HR508 “Drug/Alcohol Abuse in the Workplace,” University of Missouri, Human Resources Benefits Manual. Financial Consultation Trainees in need of financial advice/counseling are encouraged to make early contact with the University of Missouri - Columbia Medical School Financial Aid Coordinator. Other private counseling organizations may be utilized and a list of local organizations is provided in Attachment B. Procedure Trainee: 1. Graduate Medical Education trainees should seek professional help on their own when they feel this is necessary. If this is a medical/physical or emotional/psychological condition, the trainees primary physician should be contacted, or the campus Employee Assistance Program may be contacted at 8826701 to provide free, confidential evaluation and referral for any problem - financial, medical, psychological, etc. 2. Trainees are strongly encouraged, but not required, to inform their Chief Resident and Program Director of medical illness, emotional or psychiatric illness when any of these may interfere with professional performance. Confidentiality will be maintained unless this is not consistent with good patient care. Program Director: 1. The Program Director, upon becoming aware of a problem, either through trainee performance, reports from others, or through communication with the trainee, should be the first line to help the resident physician resolve any issues. The Program Director should discuss alternative sources of counseling and/or other care with the resident physician and assist in initiating the process for counseling. 2. Program Directors may, at their discretion, seek information about alternatives for handling medical/physical or emotional/psychological problems from other sources, such as other Program Directors or the Graduate Medical Education Office, while maintaining confidentiality. 3. If the determination has been made that the trainee is not able to carry out assigned responsibilities due to substance abuse and, after discussing the identified issues with the trainee, the trainee is not willing or able to correct the problem, the Program Director may temporarily remove the trainee from the rotation or change the schedule pending expedient implementation of Attachment A: “Substance Abuse Policy for 50 Clinical Faculty and Resident Physicians,”. The trainee will continue to receive pay, fringe benefits, and due process during the impaired physician process of Attachment A. Attachment A - Impaired Physician Policy, Clinical Faculty and Resident Physicians Attachment B - List of Local Counseling Resources. References: 1. HR508 “Drug/Alcohol Abuse in the Workplace,” University of Missouri, Human Resources Benefits Manual. 2. Housestaff Bylaws, Rules and Regulations Approved by GMEOC 2/2/99 51 Attachment A SUBSTANCE ABUSE AND IMPAIRED PHYSICIAN POLICY UNIVERSITY OF MISSOURI-COLUMBIA SCHOOL OF MEDICINE HOUSESTAFF PROGRAM The Dean, University of Missouri-Columbia School of Medicine, has established the following program to address the issue of substance abuse and impairment by residents /fellows operating under the auspices of the University of Missouri-Columbia Health Sciences Center. This policy is similar to that in place for our clinical faculty. Physicians hold a unique place in society. Professional standards require that persons seeking care can be assured that their physicians are not impaired by reason of substance abuse or mental illness. The purpose of this policy is: 1. To assure that patients receiving care from physicians, operating under the auspices of the University of Missouri-Columbia Health Sciences Center, receive the highest quality health care from individuals not only well trained and highly motivated, but unimpaired by reason of substance abuse or mental illness. 2. To assure that individual residents/fellows have access to appropriate health care and assurance of continued access to employment so long as they comply with institutional requirements and standards. A. HEALTH SCIENCES CENTER PHYSICIAN HEALTH COMMITTEE 1. The Health Sciences Center Physician Health Committee will, as needed, be appointed by the Dean, School of Medicine, to assume responsibility for oversight of the Health Sciences Center Physician Health Program to address issues of physician impairment or substance abuse. 2. Membership of the Health Sciences Center Physician Health Committee will consist of: a. Two members of the clinical faculty appointed by the Dean, School of Medicine. Individuals may be reappointed at the discretion of the Dean. One of these individuals will be designated by the Dean to chair the committee. b. One resident physician or clinical fellow appointed by THE DEAN FROM RECOMMENDATIONS BY the House Staff Organization. 3. The Health Sciences Center Physician Health Committee will meet as often as necessary to fulfill its obligation. 4. All information presented at meetings of the Health Sciences Center Physician Health Committee, and all actions of the committee will be considered to be confidential except as provided herein and except that such information will be available to the Dean, School of Medicine and otherwise as required by law. 52 B. RESPONSIBILITIES OF THE HEALTH SCIENCES CENTER PHYSICIAN HEALTH COMMITTEE. 1. The Health Sciences Center Physician Health Committee will initially establish a definition of impairment. This definition will be utilized by future committees. Following its establishment, it must be approved by the Dean, School of Medicine. 2. It is the responsibility of the Health Sciences Center Physician Health Committee to receive any admission of substance abuse or mental health problems by a physician, or allegations of impairment of physicians due to substance abuse or mental illness. 3. The Health Sciences Center Physicians Health Committee will be responsible for investigating those allegations. The Committee shall inform the individual in writing of the allegations and provide him/her an opportunity to respond to the allegations. 4. The Health Sciences Center Physician Health Committee shall inform the Dean if the Committee suspects the individual is impaired by substance abuse or mental illness, and presents potential risk to patients. 5. If probable cause to believe that impairment due to substance abuse is present, allegations related to possible substance abuse must be reported to the Missouri Physicians Health Committee for further investigation and action. 6. If there is probable cause to believe that impairment due to mental illness is present, the Health Sciences Center Physician Health Committee shall require psychiatric evaluation by a psychiatrist approved by the Health Sciences Center Physician Health Committee. 7. Upon determination that a resident/fellow is impaired due to substance abuse or mental illness, the Health Sciences Center Physician Health Committee will notify the Dean, School of Medicine. C. PERMISSION TO CONTINUE CLINICAL RESPONSIBILITIES 1. If the resident/fellow has been removed from clinical responsibilities by the Dean, permission to resume clinical responsibilities will be granted only with the agreement of the Health Sciences Center Physician Health Committee and the Dean. D. CONTINUATION OF FACULTY APPOINTMENT 1. Residents/fellows found to be impaired by reason of substance abuse or mental illness may not be dismissed from employment prior to full evaluation of their impairment. They may, however, be removed from clinical responsibility. Full evaluation of impairment due to substance abuse will be made by the Missouri Physicians Health Committee. Full evaluation of mental illness will be made by a licensed psychiatrist approved by the Health Sciences Center Physicians Health Committee. The allegedly impaired physician may participate in determining the identity of that physician. 2. Residents/fellows found to be impaired by reason of substance abuse or mental illness may not be terminated based upon such substance abuse or mental illness during the term of their 53 contract if they are compliant with the requirements of the Health Sciences Center Physician Health Committee, and the Missouri Physician Health Committee. E. TERMINATION OF APPOINTMENT 1. A resident/fellow who has been found to be non-compliant with the Health Sciences Center Physician Health Committee or the Missouri Physician Health Committee will be reported to the Dean, School of Medicine. 2. Noncompliance may be grounds for termination of appointment. 3. Any dismissal shall conform to applicable University procedures. 6/18/91 REVISIONS 2/99/REVISIONS 5//00 54 Attachment B FINANCIAL ADVICE/COUNSELING RESOURCES Conway Jones University of Missouri - Columbia Medical School Financial Aid Coordinator MA202 Medical Science Building .................................................................................................. 882-2923 FINANCIAL/COUNSELING ORGANIZATIONS - LOCAL A. G. Edwards & Sons, Inc. 2100 Forum Blvd., Columbia ............................................................................................ 445-7088 American Express Financial 1316 Old Hwy .63 S, Columbia ......................................................................................... 499-4945 American Express Financial Advisors 601 Nifong, Columbia ....................................................................................................... 499-4880 American Express Financial Advisors, Inc. 2710 Forum Blvd., Columbia ............................................................................................ 446-2744 American Tax Service 311A Bernadette Dr., Columbia ........................................................................................ 445-8364 David Banks, CFP 2611 Luan Ct., Columbia ................................................................................................... 445-4308 Boone County National Bank Columbia ............................................................................................................................ 874-8490 Boone County National Bank Investor Services Columbia ............................................................................................................................ 874-8446 Alan Bunch, LUTCF Principal Financial Group 401 Vandiver Dr., Columbia .............................................................................................. 443-3535 Cambria Financial Management, Inc. Columbia ............................................................................................................................ 817-3180 Casey and Company, LLC, CPAs 1 E. Broadway, Columbia .................................................................................................. 442-8427 Consumer Credit Counseling Services of Mid-America (Staffed, in part, by MU Department of Consumer and Family Economics Students) 205 E. Ash, Columbia ........................................................................................................ 443-0303 Dollar-Kuretich Doris Financial Advisor 55 116 S. Jefferson, Jefferson City ......................................................................................... 581-5994 Finance World 601 Business Loop 70 W, Columbia ................................................................................. 815-9700 Financial Architects, Inc. 1000 W. Nifong Blvd., Columbia ...................................................................................... 443-3183 Fundbuilder 4818 Santana Cir., Columbia ............................................................................................. 815-1055 Kammerich Financial Services 1951 Boone Village Plaza, Ste. D, Boonville .............................................................660-882-7620 Thomas Lightfoot 1414 Rangeline, Columbia ................................................................................................. 874-3888 Lincoln Financial Advisors 601 E. Broadway, Ste. 304, Columbia ............................................................................... 443-1654 Merrill Lynch 2804 Forum Blvd., Ste. 2, Columbia……….…………………………..446-7023 or 800-937-0948 Mita Financial Services 1961 Hirst Dr. .............................................................................................................660-263-8096 Money Concepts Financial Planning Center 217 E. Jackson, Mexico ..................................................................................................... 581-4313 Northwestern Mutual Life The Peter W. Graff District Agency 1900 N. Providence Rd., Ste. 307, Columbia .................................................................... 449-2488 Nova Financial 811 Cherry St., Columbia .................................................................................................. 874-0434 Principal Financial Group Betty Schuster, CFP 401 Vandiver Dr., Columbia .............................................................................................. 443-0389 Professional Planning Group Christine Marks, CLU, ChFC 108 E. Green Meadows Rd., Ste. 7, Columbia……..................…………………………………...443-8628 Sims & Associates Insurance & Financial Services 4818 Santana Cir., Ste. B, Columbia ................................................................................. 874-4494 Waddell & Reed, Inc. 1900 N. Providence Rd., Columbia ................................................................................... 875-4494 56 OTHER COUNSELING SERVICES Employee Assistance Program...................................................................................................... 882-6701 University Physicians Psychiatry Clinic ...................................................................................... 882-2511 57 POLICY TO ADDRESS RESIDENT CONCERNS Purpose: The ACGME requires that the Housestaff have assurance of an educational environment in which to raise and resolve issues without fear of intimidation or retaliation. This policy outlines a process by which residents can address concerns in a confidential and protected manner. The Housestaff representatives to the GME Oversight Committee will give a monthly report of resident issues identified during their monthly meetings, or through communication among resident(s). This report should include, but not be limited to concerns of residents about fairness of schedules, treatment, workloads, etc. Concerns will be addressed as needed in a way that excludes and prohibits retaliation toward any fellow or resident. Individual resident concerns should be addressed with the following process. Process: Resolution should be attempted at the most local level. If resolution is not obtained at this level, the resident or fellow may proceed to the next level as appropriate to the nature of the concern. 1. Contact the Chief Resident/Fellow of the Program 2. Contact the Program Director 3. Contact the Department Chair or Division Chief 4. Contact the Housestaff Organization 5. Contact the Associate Dean for Graduate Medical Education / Designated Institutional Official If the issue is not able to be resolved by this informal mechanism, then a formal grievance may be filed with the Program Director. See Grievance Policy. Revisions approved by the GMEOC 3-2-10 58 GRIEVANCE POLICY FOR RESIDENTS/FELLOWS Purpose To establish fair policies and procedures for the adjudication of resident grievances related to the actions which could result in dismissal, non-renewal of agreement of appointment, or any other action that could threaten a resident’s intended career development. A grievance procedure shall not be used to question a rule, procedure, or policy established by an authorized faculty or administrative body. Rather, it shall be used as due process by a resident who believes that a rule, procedure or policy has not been followed or has been applied in an inequitable manner. An action may not form the basis of a grievance if the resident merely challenges the judgment of the faculty as medical educators in evaluating the performance of the resident. For purposes of this policy, a grievance is defined as an allegation that: 1. There has been a violation, a misinterpretation, an arbitrary, or discriminatory application of University policy, regulation or procedure which applies personally to the resident physician, relating to the privileges, responsibilities, or terms and conditions of the residency training program including academic or other disciplinary actions or the employment of the resident physician; or 2. The resident physician has been discriminated against on the basis of race, color, religion, sex, national origin, age, disability, or status as a Vietnam era veteran. Filing a Grievance A resident physician who has a grievance shall initiate action by filing a signed, written account of the grievance with the program director within thirty (30) days after the occurrence of the event out of which the grievance has arisen. The program director shall respond to the grievance in writing within thirty (30) days after receipt of the written grievance. Grievance Appeals Should the resident physician be dissatisfied with the response of the program director, he/she may, within ten (10) days after receipt of such response, submit a written appeal to the Associate/Assistant Dean of the School of Medicine having responsibility over graduate medical education. Upon receipt of the written appeal, the Associate/Assistant Dean shall arrange a meeting with the resident physician and with the involved residency program director to discuss the allegations and the response. In an effort to reach a fair decision on the grievance, the Associate/Assistant Dean may elect to meet with others having knowledge of the circumstances giving rise to the grievance, including those identified by the resident physician or the residency program director. Upon completion of the Associate/Assistant Dean’s consideration of the appeal, the Associate/Assistant Dean shall provide a written decision to the resident physician and to the residency program director. Appeal to the Dean 59 If the resident physician is dissatisfied with the decision of the Associate/Assistant Dean, he/she may, within ten (10) days after receipt of such written decision, submit a written appeal to the Dean of the School of Medicine who shall decide whether the previous decision shall be affirmed, reversed or modified. In reaching that decision, the Dean may ask to meet with the resident physician, but is not required to do so; may utilize the services of an ad hoc advisory committee, appointed by the Dean, but is not required to do so; and may consult with the program director and faculty with whom the resident physician worked, but is not required to do so. The resident physician shall have no right of appeal from the Dean’s decision, but may request that the Chancellor exercise his or her discretion to review the Dean’s decision. (Also see the University of Missouri Employee Grievance Policy: 380.010 GRIEVANCE PROCEDURE FOR ADMINISTRATIVE, SERVICE & SUPPORT STAFF) 60 Grievance Procedure Summary The University recognizes the right of employees to express their grievances and to seek a solution concerning disagreements arising from working relationships, working conditions, employment practices or differences of interpretation of policy which might arise between the University and its employees. In addition, grievances may be filed alleging discrimination on the basis of race, color, religion, sex, sexual orientation, national origin, age, disability, and status as a Vietnam era veteran. This shall not be interpreted in such a manner as to violate the legal rights of religious organizations or military organizations associated with the Armed Forces of the United States of America. A regular employee may process a grievance regarding any of these matters upon completion of his/her probationary period. A probationary or nonregular employee may process a grievance concerning issues of prohibited discrimination or application/interpretation of University policies and procedures. Grievance Definition Any complaint by an employee concerning any aspect of the employment relationship other than merit increases, performance evaluations and job reclassifications, unless such exceptions include an allegation of prohibited discrimination or other illegality. Procedures Should an employee or the employee's representative feel, after oral discussion with the immediate supervisor, that employee's rights under University policy have been violated, the employee may originate a grievance within ten (10) days of the date the alleged grievable act occurred by presenting the facts in writing to the proper supervisor, department head, or designated representative of the University with a copy to the Campus Grievance Representative. The decision of such official shall be made in writing to the employee within ten (10) days after receipt of grievance. For an alleged act of prohibited discrimination, an employee has a 180-day filing period. Should the employee decide the reply is unsatisfactory, the employee or the employee's representative shall, within five (5) days, submit an appeal to the Campus Grievance Representative. The Campus Grievance Representative or designate shall respond in writing to the grievance within five (5) days from the date of the review. If the grievance is resolved, no further action will be necessary. If the grievance is not satisfactorily resolved, the employee or the employee's representative may appeal within five (5) days after receipt of response to the University Grievance Representative for the purpose of reviewing the grievance. The decision of the University Grievance Representative or designate shall be made in writing to the employee and/or employee's representative within five (5) days after the date of the review. 61 Should the employee decide that the reply of the University Grievance Representative or designate is unsatisfactory, the matter may be appealed within five (5) days of receipt of the response through the University Grievance Representative to a grievance committee which shall be established: the employee or employee's representative may designate one (1) member; the University through its Grievance Representative, with the approval of the Chancellor of the campus, shall appoint one (1) member; and the selection of the third member shall be made by these two (2) members. If mutually agreeable, the two (2) designated members may select the third member from a list recommended by either and approved by both. Otherwise, selection will be made from a list of committee members supplied by the Federal Mediation and Conciliation Service and maintained by UM Human Resources. The selection will be made by reducing the list in alternate turns. The toss of a coin shall determine the elimination sequence. A decision of the grievance committee may be reached upon the concurrence of any two (2) of the three (3) members. A hearing will be scheduled as soon as feasible after selection of the third committee member. The grievance committee shall keep a complete record of the hearing before it, including any exhibits or papers submitted to it in connection with the hearing and a complete record of any testimony taken. Upon the rendering of its decision, the complete record shall be filed in the Office of the President of the University and shall be available to the employee, employee's representative and the University Grievance Representative. Any cost of the third party on the committee and cost of transcript (if requested) shall be paid equally by the employee and the University. In the event the decision of the grievance committee is unsatisfactory to either the employee or the University Grievance Representative, either may, within five (5) days after receipt of the decision of the grievance committee, file a written notice of appeal to the Board of Curators by delivering such notice of appeal to the President of the University. Upon the receipt of the notice of appeal, the President of the University shall cause the record of the hearing before the grievance committee to be filed with the Board of Curators of the University, who shall review such record. The decision of the Board of Curators, upon such review, will be final. Time Limits The prescribed time limits may be extended by mutual agreement whenever necessary in order for these provisions to be implemented. The interpretation of "days" within this section is to be normal workdays (Monday through Friday) exclusive of official University holidays. University Grievance Representative Betsy Rodriguez Vice President, Human Resources Human Resources 104 University Hall Columbia, Missouri 65211 (573) 882-8270 62 Designated Campus Grievance Representatives University of Missouri System Betsy Rodriguez Vice President, Human Resources Human Resources 104 University Hall Columbia, Missouri 65211 (573) 882-8270 Columbia Karen Touzeau Assistant Vice Chancellor Human Resource Services (MU) 1095 Virginia Avenue, Room 101 Garage #7 Columbia, Missouri 65211 (573) 882-4256 Hospital and Clinics Phil Shearrer Staff Development Specialist Human Resources University of Missouri Healthcare 1 Hospital Drive, Room 4E55 Columbia, MO 65212 (573) 882-8444 Kansas City Jill Reyes Director Human Resources 226 Administration Center 5100 Rockhill Road Kansas City, Missouri 64110 (816) 235-1621 Rolla Randy Stoll Director, Business Services 210 Parker Hall Rolla, Missouri 65401 (573) 341-4122 63 St. Louis Peter Heithaus Director, Human Resources 222 General Services Building St. Louis, Missouri 63121 (314) 516-5809 Date Created: 9/26/97 Last Updated: 04/01/11 64 Sexual Harassment Executive Order No. 20, 3-17-81 (Rev. 7-1-81 and 9-20-83), Bd. Min. 3-18-93. This University of Missouri policy aims for an increased awareness regarding sexual harassment by making available information, education and guidance on the subject for the University community. A. Policy Statement -- It is the policy of the University of Missouri, in accord with providing a positive discrimination-free environment, that sexual harassment in the work place or the educational environment is unacceptable conduct. Sexual harassment is subject to discipline, up to and including separation from the institution. Definition -- Sexual harassment is defined for this policy as either: 1. Unwelcome sexual advances or requests for sexual activity by a University employee in a position of power or authority to a University employee or a member of the student body, or 2. Other unwelcome verbal or physical conduct of a sexual nature by a University employee or a member of the student body to a University employee or a member of the student body, when: a. Submission to or rejection of such conduct is used explicitly or implicitly as a condition for academic or employment decisions; or b. The purpose or effect of such conduct is to interfere unreasonably with the work or academic performance of the person being harassed; or c. The purpose or effect of such conduct to a reasonable person is, to create an intimidating, hostile, or offensive environment. B. C. Non-Retaliation -- This policy also prohibits retaliation against any person who brings an accusation of discrimination or sexual harassment or who assists with the investigation or resolution of sexual harassment. Notwithstanding this provision, the University may discipline an employee or student who has been determined to have brought an accusation of sexual harassment in bad faith. D. Redress Procedures -- Members of the University community who believe they have been sexually harassed may seek redress, using the following options: Pursue appropriate informal resolution procedures as defined by the individual campuses. These procedures are available from the campus Affirmative Action/Equal Opportunity Officer. Initiate a complaint or grievance within the period of time prescribed by the applicable grievance procedure. Faculty are referred to Section 370.010, "Academic Grievance Procedures"; staff to Section 380.010, "Grievance Procedure for Administrative, Service and Support Staff" and students to Section 390.010, "Discrimination Grievance Procedure for Students". Pursuing a complaint or informal resolution procedure does not compromise one's rights to initiate a grievance or seek redress under state or federal laws. E. Discipline -- Upon receiving an accusation of sexual harassment against a member of the faculty, staff, or student body, the University will investigate and, if substantiated, will initiate the appropriate disciplinary procedures. There is a five year limitation period from the date of occurrence for filing a charge that may lead to discipline. An individual who makes an accusation of sexual harassment will be informed: at the close of the investigation, whether or not disciplinary procedures will be initiated; and at the end of any disciplinary procedures, of the discipline imposed, if any. 65 Drug Testing Policy For Training Physicians Objective: In order to ensure safe patient care and protect the public, the University of Missouri Hospitals and Clinics will conduct pre-employment drug testing for all new residents and fellows. This policy provides guidelines for testing, notification of results and related employment decisions. Policy: Before commencing performance of duties, the selected resident or fellow (hereinafter referred to as “prospective resident”) must undergo drug testing as a condition of employment, and the drug test shall produce a negative result. No prospective resident shall begin working until results of the test have been reviewed in Human Resources. Any prospective resident who refuses to undergo such testing, may, at the discretion of their clinical department, not be considered qualified for employment, and previously extended offers of employment and contracts may be rescinded. A. Definitions 1. “Medical Review Officer” is an individual designated by the Chief Executive Officer of UM Health Care to review test results and review appeals of positive test results. 2. “Prohibited drug usage” is the illegal use of narcotics, drugs or controlled substances. B. Scope 1. All prospective residents shall submit to drug testing prior to employment as a condition of employment. C. Procedure 1. Testing services will be provided by a certified laboratory. The laboratory shall ensure: a. Proper maintenance of confidentiality. The name of the individual providing the sample will not be provided to the laboratory performing the test. Instead, testing numbers assigned to the specimen at the time of the test will be used for communication with the laboratory. The laboratory will only provide test results to the Chief Human Resources Officer of UMHC. b. Proper maintenance of chain of custody. c. Proper confirmation of a positive test by an approved confirmation test, such as gas chromatography/mass spectrometry. The laboratory will only report a positive test of a particular sample to the Medical Review Officer after both the screening and confirmation tests are positive. The Medical Review Officer will report confidential positive results to the Chief Human Resources Officer or designee. d. Proper specimen collection, labeling and protection from contamination. All specimen collection pursuant to this program shall be minimally intrusive as 66 follows: a) urine samples will be collected in a confidential environment; b) the collection will be performed by trained personnel; c) the procedures followed shall be similar to those required for physical examinations; and d) the personnel conducting the testing shall not directly observe the prospective resident produce a sample. e. Proper notification, at the time a specimen is produced, to all prospective residents or the necessity of declaring any prescription drugs or over-the-counter medication they are currently taking which may result in a positive drug test. D. Drugs 1. The certified laboratory will test all samples for the following drugs: a. Amphetamines: d-Amphetamines, Methamphetamines b. Cocaine c. Opiates: Codeine, Heroin, Hydromorphone, Morphine d. Phencyclidine (PCP) e. Cannabinoids (Marijuana metabolites) f. Methadone g. Propoxyphene E. Notification 1. Prior to finalizing a contract, the School of Medicine department where the residency program is housed and/or Human Resources shall inform all residents that UMHC conducts preemployment drug testing for safety-sensitive positions, including residents and fellows. 2. The School of Medicine department and/or Human Resources shall notify prospective residents that they need to go for a specimen collection. The prospective resident must report to the designated collection site on the date and time assigned. 3. It is a condition of employment at University of Missouri that residents be, and remain, free of illegal drugs, controlled substances and alcohol while at work and while performing job functions related to employment at the University of Missouri. If a confirmatory test reveals prohibited drug usage for prospective resident, the UMHC Human Resources department shall notify the Program Director of the School of Medicine department where the individual’s training program is housed, as well as the Associate Director at the University of Missouri Health Care who oversees coordination of all residency programs. The Program Director will be instructed to notify the prospective resident of the positive test results. 4. The Program Director, in consultation with the department chair, Chief of Staff and GME Dean, will determine if the prospective resident’s employment contract will be terminated. At the discretion of the department, the prospective resident may be given alternatives, such as delaying commencement of residency training for a period of time while completing a drug treatment program. Any costs associated with treatment will be borne by the resident and/or School of Medicine department. 5. The Program Director should provide a written agreement of a treatment plan and a plan for returning to the residency program, with copies to the individual resident and his/her personnel file. The agreement should outline all pertinent information, including, but not 67 limited to, leave status, salary, medical benefits, treatment costs, time period for the resident to be absent from the training program, and conditions for return to the training program. The plan will be reviewed and approved by a special committee convened by the GME chair. 6. Any required reporting to outside agencies will be done by the Associate Director at the University of Missouri Health Care who oversees the coordination of training programs. F. Compliance 1. Prospective residents will promptly comply with the UMHC’s request for testing. 2. If a prospective resident refuses to submit to testing or engages in any conduct jeopardizing the integrity of the specimen or the reliability of the drug test, the Program Director of the training program will be notified and the prospective resident’s contingent offer of employment may be rescinded. 3. If a prospective resident fails to schedule or to appear for a drug test specimen collection, or postpones or reschedules specimen collection without good cause, the Program Director will be notified and the resident’s employment may be terminated. G. Record Keeping 1. Drug testing records will be kept for a minimum of two years and will be kept confidential to the extent permitted by law. H. Appeals 1. A prospective resident who has tested positive for prohibited drugs will, upon request, be provided an opportunity for a meeting with the Medical Review Officer and Human Resources representative to explain mitigating circumstances. In order to evaluate said explanation, the prospective resident may be requested to provide a medical release. 2. If a prospective resident disputes the validity of a positive test result, the prospective resident may request a re-test of his or her original sample, after agreeing to pay any cost associated with the second test. If the second test is negative, UMHC will pay for or reimburse the prospective resident for the cost of the re-test. 3. A prospective resident appealing under provisions 1 and 2 of this section must provide a written appeal notice to the Human Resources Department within 72 hours of receiving notification of a positive test result. GMEOC Approved April 5, 2005 68 Policy to Monitor Residents and Fellows with Prior Issues of Concern University of Missouri Health Care Residents and fellows who have any issues of impairment identified by the various licensing agencies (Board of Healing Arts, DEA, BNDD) will have an appropriate monitoring and supervision plan developed by the program director. The plan may be proscribed by or in conjunction with the licensing agency. The plan will be approved by a subcommittee of the GMEOC authorized to act on the committee’s behalf in closed session. The medical executive committee or chief of staff at any hospital the resident/fellow is assigned will be notified of the issue and the monitoring plan prior to the resident/fellow working in that location. The chair of the GMEOC should be notified as soon as the issue is identified and preferably before a contract is offered. Approved by the GMEOC 9/7/04 Revisions approved by GMEOC 10/5/05 69 DISCIPLINARY ACTION POLICY FOR RESIDENTS/FELLOWS Resident physicians are subject to disciplinary actions including oral reprimands, written reprimands, suspensions and discharge for misconduct or for performance which does not meet acceptable standards. Suspension Without Pay or Termination Before a resident physician may be suspended without pay or terminated prior to the specified ending date of his or her appointment, the resident physician should be provided in writing with findings which the University believes support the proposed suspension without pay, or the termination. That written notice will be provided by the residency program director and will include details concerning the findings of misconduct or the performance deficiencies. In addition, the written notice will inform the resident physician that if he or she disagrees with such findings and desires to contest the proposed disciplinary suspension or termination, he or she must inform the residency program director in writing within ten (10) days of receipt of the written notice. After receiving notice that the resident physician disagrees with such allegations and desires to contest the proposed disciplinary suspension or termination, the residency program director will schedule a meeting with the resident physician so that he or she will have an opportunity to present information in support of his or her position regarding the findings. After discussing the issues with the resident, the residency program director shall decide whether (1) to impose the disciplinary suspension without pay or the termination which had been contemplated, (2) to impose some lesser degree of discipline or (3) that the resident physician should receive no discipline. That decision shall be communicated to the resident physician in writing as soon as possible. If the resident physician is dissatisfied with the decision of the residency program director, he or she may, within ten (10) days of receipt of such written decision, file a grievance in accordance procedures outlined in the Grievance Policy. References: 1. Collected Rules & Regulations, University of Missouri, Academic Grievances: Section 370.010. 2. Collected Rules & Regulations, University of Missouri, Grievance Procedure for Administrative, Service and Support Staff: Section 380.010. 3. Collected Rules & Regulations, University of Missouri, Discrimination Grievance Procedure for Students: Section 390.010 70 POLICY NON-RENEWAL OF A RESIDENT/FELLOW CONTRACT AT UNIVERSITY OF MISSOURI HEALTH SCIENCES CENTER Purpose: To provide a procedure in the event a resident or fellow’s contract will not be renewed for the following year. 1. The Program Director must provide a written notice to the resident/fellow indicating that their contract for the following year will not be renewed. Justification for non-renewal of the contract must be adequately outlined. This written intent must be given to the resident/fellow no later than four months prior to the end of the current appointment. 2. If the primary reason for non-renewal of the contract occurs within four months prior to the end of the current appointment, the Program Director must provide written notice as early as circumstances will allow, prior to the end of the appointment. 3. The resident/fellow must be allowed to implement the institution’s grievance procedures, including those outlined in the Health Sciences Center’s “Policy to Address Resident Concerns.” 71 POLICY: To Address Administrative Support for Programs and Residents in the Event of a Disaster or Interruption of Patient Care Effective: 7-1-07 Approved by the GMEOC: 8-28-07 In the event of a disaster or interruption of patient care, the Designated Institutional Official (DIO), or his/her designee, will call an emergency meeting of the Graduate Medical Education Oversight Committee (GMEOC) to assess the effect of the situation on residency/fellowship education, including the probable duration of the interruption. The DIO will work with Hospital Administration representatives and the Medical Staff Office to coordinate activities, including patient care issues. The GMEOC will develop a plan for residency/fellowship education that will be presented to the ACGME for review. If there is a need for residents/fellows to continue their training elsewhere, on a temporary basis, the GME Office will assist programs with arrangements for housing, salary and other issues involved in a temporary transfer to another program. If a permanent transfer is necessary, the GME Office will work with the accepting institution to arrange the transfer. All arrangements will be coordinated through the GME Office, working with the affected programs. The institution will continue to pay salary and benefits until other arrangements are in place. 72 POLICY: Process for Requesting a Change in Resident/Fellow Complement or Starting a New Program Effective: 7-1-09 Revisions Approved by the GMEOC: 3-2-10 All requests must first be approved by the School of Medicine Dean and UMHC CEO, regardless of the source of funding. In general, requests must be submitted one year prior to the expected start date of the resident/fellow. Process: 1. Submit a written request to the GME Office which includes the following: - brief business plan, including anticipated source of funding - educational rationale for the increase (or development of a new program) - brief description of the program including faculty numbers and clinical material - importance of the division/department to the UMHC, the State of Missouri and the specialty 2. The Associate Dean for GME/DIO will submit the written request, including the detailed information above, to the Dean and CEO. 3. If approved to move forward by the Dean and CEO, the request must then be presented to the GMEOC for approval. (The GME Office will coordinate this as an upcoming GMEOC agenda item.) 4. If approved by the GMEOC, the program may then submit the request to the ACGME (if applicable). New programs will need extensive paperwork submitted to the ACGME and this will need to be approved by the GMEOC before it is submitted. 73 Policy: Process for the: 1) Reduction in Size or Closure of a Program or 2) Closure of the Institution – Training Programs at University of Missouri-Health Care Effective: 7-1-07 Approved by the GMEOC: 8-28-07 Training Programs: 1. University of Missouri Health Care will inform the DIO, the GMEOC and residents/fellows as soon as possible when it intends to reduce the size of or close one or more programs. 2. Before any reductions or closures of programs occurs, the GMEOC will be asked for recommendations and input when there is a perceived need to reduce or close a program. The Dean will make final decisions. 3. For programs either reducing in size or closing, residents/fellows already in the program will either be allowed to complete their education or will be assisted in enrolling in an ACGMEaccredited program in which they can continue their education. 4. Notification will be sent to the ACGME, by the DIO, indicating intent to voluntarily reduce or close a program. 5. Residents will be given final notification of the action by the DIO and the Program Director. This will include the effective date of the reduction or closure as soon as known. Institution: University of Missouri Health Care will inform the DIO, GMEOC and residents/fellows as soon as possible if it intends to close. In the event that all training programs under the sponsorship of the University of Missouri-Columbia School of Medicine should be closed. All training physicians will receive notification of this action and the effective date of closure by the DIO and their Program Director as soon as possible. They will be assisted by their program director in finding new GME positions. In the event that an affiliated institution closes, all efforts will be made to arrange for similar educational experiences in another setting. Approved by the GMEOC 3/7/00 Revisions approved 8/27/07; 10/6/09 74 HR-519 Consensual Amorous Relationships Summary The University of Missouri promotes an atmosphere of professionalism based on mutual trust and respect. The integrity of interaction among faculty, staff and students must not be compromised. Consensual amorous relationships are prohibited in certain instances as outlined below. Conduct Consensual amorous relationships between members of the University community are prohibited when one participant has direct evaluative or supervisory authority over the other because such relationships create an inherent conflict of interest. Examples of such relationships that are prohibited include, but are not limited to, employee (faculty, staff or student)/student and supervisor (faculty, staff or student)/subordinate, when those relationships involve direct evaluative or supervisory authority. In such cases, the individual in the evaluative or supervisory position has an obligation to disclose the consensual amorous relationship to his or her administrative superior and to cooperate with the administrative superior in removing himself or herself from any such evaluative or supervisory activity in order to eliminate the existing or potential conflict of interest. Definition For purposes of this policy, consensual amorous relationships exist when two individuals mutually and consensually understand a relationship to be romantic and/or sexual in nature except when those two individuals are married to each other. Direct evaluative or supervisory authority exists when one participant is personally involved in evaluating, assessing, grading, or otherwise determining the other participant´s academic or employment performance, progress or potential. Violations Should a violation of this policy be claimed by a person involved in the consensual amorous relationship, the matter shall be investigated by the appropriate University official or, if that person elects to file a grievance, under the appropriate University grievance procedure. Should any employee or student not involved in the consensual amorous relationship claim to have been adversely affected personally by a violation of this policy, the situation will be investigated by the appropriate University official or, if that person elects to file a grievance, under the appropriate University grievance 75 procedure. A violation of this policy, regardless of the manner in which it is brought to the attention of the University, may lead to disciplinary action as appropriate, up to and including termination of employment in the most serious circumstances, following appropriate processes for such discipline. See Also HR 507 Conflict of Interest, HR 510 Sexual Harassment Date Created: 12/15/06 Last Updated: 12/15/06 Contact webmaster@umsystem.edu. Reviewed May 11, 2004 Human Resources Manual HomeIndexAbout the ManualEmployment Policies (HR-100)Compensation (HR-200)Benefits (HR-300)Leaves (HR-400)Workplace (HR-500)Employee Relations (HR-600)Service and AdvancingMissouri Maintenance EmployeesRecent Updates 76 SUB-SPECIALTY SECTION CORNEAL/EXTERNAL DISEASE AND REFREACTIVE SURGERY SERVICE Objectives: A. First year resident: 1. Complete patient examination, evaluation and proposed therapy. (PC, ICS, PBLI) 2. Diagnosis and management of corneal ulcers. (PC, MK, PBLI) 3. Knowledge and ability to do optical and ultrasonic pachymetry, computerize corneal topography (Pentacam), specular microscopy, and confocal microscopy. (MK, TS) 4. Microsurgery of animal and human globes in penetrating keratoplasty and refractive surgery techniques. (TS, PBLI) 5. Become familiar with the operating microscopes, and place sutures in corneal surgeries. (TS, PBLI) 6. Learn the diagnosis/management of: (MK, PC, ICS, PBLI) Bacterial corneal ulcers Chemical Corneal Burns Herpes Simplex/Herpes Zoster Ocular Surface Disease Ocular Adenoviral Infections Non-infected Corneal Ulceration Blepharoconjunctivitis Corneal graft rejection-reactions Superficial Punctate Keratitis Keratoconus Marginal Corneal Ulcers/Degenerations Corneal Dystrophies Recurrent Corneal Erosions Bullous Keratopathy Keratitis Sicca 7. Learn indications for: (MK, TS, PC, PBLI) Conjunctival Flap Superficial Keratectomy Penetrating Keratoplasty (PKP) Therapeutic Keratoplasty PKP with IOL exchange PKP with ECCE with IOL Lamellar Keratoplasty, DSAEK, DALK Refractive Surgery Astigmatic Keratotomy Kerato-limbal Allograft Amnionic Membrane Graft Excimer Laser PRK LASIK, LASEK Phototherapeutic Keratectomy (PTK) Keratoprosthesis (K-Pro) 8. Demonstrate Surgical Skills and knowledge of: (TS, PC) Corneal Suture Placement Instrument Tying Pterygium Removal Familiarity with Corneal/Trephines/Punches 77 B. Third year resident: 1. Assisting and performing part, or all, of a penetrating keratoplasty providing enough experience has been obtained. (TS, MK, P, PBLI, PC) 2. Assisting on refractive surgical procedures including the excimer laser. (TS, MK, PBLI, PC) 3. Assist or perform part of complex corneal procedures including keratoprosthesis, lamellar keratoplasty, DSAEK, kerato-limbal allografts, amniotic membrane grafts, combined PKP, ECCE with IOL, conjunctival flap construction. (TS, MK, P, PC, PBLI, ICS) 4. Understand or perform all of the first year objectives. (MK) 5. Learn Contact Lens Fitting in Keratoconus and post PKP patients. (PC, TS, MK, P) 6. Pre-operative Evaluations of Donor Tissue from the Eye Bank for Corneal Transplantation. (MK) 7. Post Keratoplasty Care (PC, ICS, MK, SBP) Immediate Long term Suture removal Visual Correction Recommended Reading & Resources: (MK, P) AAO Basic & Clinical Science Course, Section 8, External Disease and Cornea AAO Basic & Clinical Science Course, Section 14, Refractive Surgery External Infections of the Eye, Helena B. Fedukowicz Manual of Corneal Surgery, Bruner, Stark and Maumenee The Cornea, Smolin and Thoft Contact Lenses – Aquavella and Rao Corneal Surgery – Brightbill (newest edition) Grayson=s Disease of the Cornea, Fourth Edition, Robert C. Arffa Cornea Color Atlas – Krachmer, Palay Cornea Text, Vol. 2 – Krachmer, Holland, Morris (newest edition) Home Study Course: Infections of the Eye, Tabbara, Hyndink, and Brown LASIK – Pallikaris and Siganos The Cornea – Kaufman, Barron, McDonald, and Waltman DSAEK – Price, & Price 78 CONTACT LENS SERVICE Objectives: 1. Properly evaluate a patient's suitability for contact lenses, including appropriate pretesting and history. (PC, ICS) 2. Understand the advantages, disadvantages, proper fitting and uses of different types and brands of hard, soft, and specialty lenses. (MK, PC) 3. Insert and remove contact lenses on a patient. (PC, PBLI, TS) 4. Teach a patient to properly handle, clean, center, insert and remove a contact lens. (ICS, PC, P) 5. Properly evaluate an existing contact lens patient, including proper follow up testing and evaluation. (PC, MK, PBLI) 6. Recognize and remedy contact lens complications and proper intervention for improvement. (PC, PBLI) 7. Be knowledgeable about the different types, components and brands of disinfection systems, solutions, their use and potential problems. (MK, P) 8. Understand and be able to calculate the optics applicable to contact lenses including residual astigmatism, vertex distance, aniseikonia, power and base curve relationships, sagittal depth, etc. (MK) 9. Demonstrate proficiency in the technique of refraction. (PC, MK, P, ICS) Required Reading & Resources: (MK, PBLI, P) CLAO Residents Contact Lens Curriculum Manual, Steis, Preman – entire text Tyler's Quarterly Soft Contact Lens Parameter Guide Complications of Contact Lens Wear, T. Onlinson, Mosby, 1992 – Chapters 2, 6, 7, 9, and 10-12 AAO Basic & Clinical Science Course, Section 3, Optics, Refraction, Contact Lenses - Chapters 5 and 7 79 GENERAL CLINIC AND EMERGENCY CLINIC SERVICES Objectives: 1. The resident physicians will obtain a complete ophthalmological history and an applicable general medical history. (PC, ICS) 2. The resident will do a complete ophthalmological examination. (PC, ICS, MK) a. This to include visual acuity testing (and refraction of optical defects of the eye including retinoscopy as indicated). (TS, MK) b. Confrontation fields. c. Orbital and external exam. d. Ocular motility exam. e. Pupillary evaluation. f. Anterior segment exam with slit lamp biomicroscopy. g. Posterior segment evaluation using direct and indirect ophthalmoscopy (including biomicroscopy of the fundus as indicated). h. Intraocular pressure testing. i. Also, when applicable, learn to do color vision testing, Amsler Grid and Maddox rod testing, gonioscopy, conjunctival and corneal scrapings, Lacrimal evaluation. A and B scan techniques, and keratometry. j. Learn the appropriate indications for ordering automated or quantitative perimetry, fluorescein angiography, ocular photography, light or pattern evoked electrical potential tests (ERG, VEP), specular microscopy, corneal thickness measurements, and optical coherence tomography. k. Do A-scan for Intraocular lenses and B-scan for pathology. 3. The resident physician will complete a differential diagnosis and treatment regimen. He/she will discuss the diagnosis and treatment of each patient with an attending ophthalmologist for final disposition of the patient. (MK, PC, ICS) The resident will then review, as indicated with the patient, his diagnosis, prognosis and treatment regimen. (PC, ICS, P) The resident will review any special tests ordered in a timely manner and discuss these results with the attending staff. (P, PBLI, MK) 4. The resident will then treat the patients as medically or surgically indicated and see the patient for appropriate follow-up care. (MK, PC, TS) 5. The resident will complete the medical record, laboratory, x-ray and photographic requests to include all the above information as appropriate. (P, PBLI, ICS) 6. Understand and complete appropriate CPT and ICD-9 codes. (MK, P) 80 GLAUCOMA SERVICE Objectives: 1. Obtaining a careful and accurate history. (ICS, P, MK, PBLI) 2. To become comfortable with all aspects of a thorough glaucoma examination (including gonioscopy and optic nerve evaluation). (MK, P) 3. Master the technique perimetry with appropriate interpretation. (PC, PBLI, MK, P) 4. Perform glaucoma surgery under direct supervision. (TX, MK, PBLI, PC) 5. Perform Argon laser trabeculoplasty, laser peripheral iridectomies and laser suture lysis under direct supervision. (PC, TS, PBLI, P) Recommended Reading & Resources: (MK, P, PBLI) General Textbooks Weinreb RN, Mills RP. Glaucoma Surgery, Second Edition. AAO Monograph Number 4, 1998. Netland PA, Allen RC. Glaucoma Medical Therapy, AAO Monograph Number 13, 1999. AAO Home Study Course, Volume 10: Glaucoma. Visual Fields Heijl A, Patella VM. Essential Perimetry Third Edition. Carl Zeiss Meditec, Inc., 2002. Gonioscopy Wallace A. Color Atlas of Gonioscopy. AAO Monograph. 2001. 81 INTRAOCULAR SERVICE Objectives: 1. Become familiar and competent with a surgical microscope and instruments; perform anterior segment surgery in the animal lab or in eye bank globes. (MK, TS, PBLI, P) 2. Perform IOL Master and ultra sound A-scan with calculation of IOL power using various formulas for low, average and high myopic and hyperopic corrections. (TS, MK, PC) 3. Perform extracapsular cataract extraction or Phacoemulsification with intraocular lens, under direct supervision. (TS, PC) 4. Become proficient with phacoemulsification, clear corneal incisions, anterior segment reconstruction, and trabeculectomies. (TS, MK, PBLI) 5. Utilize the laser for YAG capsulotomies, peripheral iridectomies, Argon laser trabeculoplasties, and ciliary body ablation. (TS, MK, PBLI, PC) Recommended Readings: (MK, PBLI) Atlas of Ophthalmic Surgery: Techniques, Complications. Edited by Klaus Heilmann, David Paton, and G. Thieme Verlag. 3 volumes. 82 LOW VISION SERVICE Growing numbers of ophthalmologists and optometrists are offering low-vision care in their practices because of an increasing demand for such services from people with irreversible vision loss. At least 13 million Americans have low vision. With the demographics of the "graying of America," the number of people with low vision is expected to continue to increase dramatically well into the 21st century. As people increasingly seize their older years as an opportunity for renewed vitality and creativity, they are seeking vision care that enables them to continue to pursue a wide range of activities. At the same time, vision-care professionals are recognizing that something can be done for patients with low vision. The American Academy of Ophthalmology, American Academy of Optometry, American Optometric Association, and their related supporting and para-professional groups endorse low-vision care as an important step in comprehensive vision care. Patients with irreversible vision loss no longer need be told that nothing can be done for them. Objectives: 1. Evaluate a patients’ readiness for Low Vision (LV), rehabilitation, including psycho- social assessment and functional indicators. (PC, ICS, P) 2. Understand the use, advantages, or disadvantages for LV adaptive devices including high add spectacles, telescopes, binoculars, prisms, magnifiers, non-optical aids, CCTV’S, optical character recognition and adaptive computing component. (MK) 3. Recognize the impact of environmental factors on vision: glare, figure ground perception, lighting, and contrast sensitivity. (MK) 4. Describe eligibility requirements for agencies and services (Rehabilitation Services for the Blind, Social Security, Blind Pension, Tax Credit, Division of Motor Vehicles). (MK, P, ICS, SBP) 5. Identify local, state and national resources for Low Vision patients. (P) 6. Develop an understanding of the Special Education system and the ophthalmologists role on the education team. (P, SBP) Required Reading The Lighthouse Ophthalmology Resident Training Manual: A New Look at Low Vision Care. (A copy is available in our department library.)or through Sue Mussatt, RN, CLVT 83 NEURO-OPHTHALMOLOGY/CONSULTATIVE SERVICE This rotation is one of independent reading, aided by regular guidance and experience. The following instructions for rotating students and residents are to achieve each goal, complete each objective and follow all assignments. Goals 1. Recognize all common forms of neuro-ophthalmic disorders 2. Learn to obtain a thorough neuro-ophthalmic history and conduct a sound neuro-ophthalmic examination. 3. Institute appropriate diagnostic tests and treatment of all neuro-ophthalmologic disturbances. Objectives in: 1. The optic fundus a. Become thoroughly familiar with the normal optic fundus and understand the features of papilledema and optic atrophy. b. Know the causes of optic disc edema and pseudopapilledema and the major funduscopic disorders associated with specific neurological diagnoses. 2. The visual system a. Be able to diagnose dysfunction of the optic nerve and identify disorders of each segment of the optic nerve b. Localize the pattern of visual field defects to each component of the optic pathways 3. The infranuclear ocular motor system a. Recognize and distinguish disorders causing: six major syndromes of the pupils, third nerve palsies, unilateral ophthalmoplegias and bilateral ophthalmoplegias 4. The supranuclear ocular motor system a. Become familiar with the neuroanatomy of the supranuclear ocular motor systems b. Be able to identify the chief disorders of eye movement and determine their treatment c. Recognize the various types of nystagmus Assignments Tutorial assignments: 1. The Neuro-Ophthalmology Servival Guide, Anthony Pane, Michael Burdon, Neil R Miller 2. American Academy of Ophthalmology Manual: Neuro-Ophthalmology 3. Become regularly familiar with Miller and Newman et al.; Walsh and Hoyt’s Clinical NeuroOphthalmology, Sixth Edition, and Glaser’s Neuro-Ophthalmology, Third Edition 4. Visit NANOS (North America Neuro-Ophthalmology Society) web site for study materials 5. Divide study time into four segments: The ocular fundus, the optic nerve, chiasm and posterior visual system, the pupil and infranuclear ocular motor system and the supranuclear ocular motor system Experimental assignments: 1. Be familiar with all patients within MUHC who have neuroophthalmic disorders 2. Carry out selected inpatient consultations under supervision 3. Read and report on all papers that are pertinent to patient encounters Neuro-Ophthalmology/Consult Rotation Guide 84 General Conduct 1. Strive for excellence 2. Come prepared 3. Read books or papers which are relevant to patient care 4. Be profession and appear professional 5. Introduce yourself to the patient and each family member 6. Wash hands before starting the interview or when moving to a different room 7. Mind confidentiality: conversation about patients should be taken to a private area, even if that means suspending an encounter Interview 1. Use the neuro-Ophthalmology template (new), (follow-up) 2. Please fill the blanks and revise the template accourdingly 3. Please get detailed, thorough, pertinent histories from the patient and family Examination 1. Check visual acuity at far and at near 2. Check pupils with Dr. Jun for every new patient and any return patients who have new visual complaints or new findings 3. Dilate eyes as early as possible 4. Check color vision with H-R-R 5. Check stereopsis 6. For double vision, please do Worth Four dots, Three steps test, Double Maddox Rod test 7. For thyroid eye disease, check proptosis (exophthalmometer), lid retraction, lid lag, lateral flare, scleral show, lagophthalmos, corneal reflex, exposure keratitis 8. For Myasthenia Gravis, check eyelid ptosis, Cogan lid twitch, enhancement of ptosis with contralateral eyelid elevation 9. If you don’t know, please ask Documentation 1. Please try to complete your documentation when you finish the interview 2. Please summarize and think what condition you are dealing with 3. Please set up plans for further investigation, management and follow-up This is revised in 05/2015 by Dr. Jun 85 * Inpatient Consults and Emergency Patients Policy at Women & Children Hospital: 1. Ask if the patient has a private practice ophthalmologist. If affirmative, it should be suggested that the private ophthalmologist be called first, as a courtesy. 2. If the patient does not have a private practice ophthalmologist or if the ophthalmologist does not desire to make a hospital visit, then the following should be implemented: 3. Ask if the consult is Urgent or Not Urgent. 4. If not urgent: a. If the patient is not mobile, indicate to the caller that the ophthalmology resident and attending at Eye Institute East clinic will see the patient the next day. (Note: the on-call resident is responsible to inform the EIE Clinic resident/attending physician of the awaiting consult.) b. If the patient is mobile, have the patient come to the Mason Eye Institute the next day though the Emergency Clinic/Consult Services. 5. If the inpatient consult is urgent or the patient is in the Emergency Room at W&C Hospital: a. Ask if the patient could be transferred to Mason Eye Institute because we have all the equipment here that we will need. b. If unable to be transported and it is daytime, the resident and attending at Eye Institute East clinic should go. (Note: the on-call resident is responsible to inform the EIE Clinic resident/attending physician of the awaiting consult.) c. If unable to be transported and it is after hours, the resident physician on-call should go to Women & Children Hospital. d. If there is no attending at Eye Institute East clinic during the daytime, the resident physician on-call should go. 86 OCULAR PATHOLOGY Objectives: Understanding of the normal anatomy and histology of the eye (MK, PBLI, P) Basic understanding of pathologic processes How gross and microscopic findings correlate with clinical findings and treatment. How these findings are used to arrive at a diagnosis and treatment. Participation and understanding of how specimens are handled in the laboratory Importance of the clinical history What the path lab can and cannot do How to work with the pathologist to ensure optimal processing Resources: (MK, PBLI) Ophthalmic Pathology. D.J. Apple, M. Rabb: Ocular Pathology, 5th ed. Mosby, 1998. M. Yanoff, B.S. Fine. Ocular Pathology, 5th ed. Lippincott, 2002. Sassani JW (ed). Ophthalmic Pathology with Clinical Correlations. Philadelphia, LippincottRaven, 1997. [At this time, it is the best of the texts for residents.] Chapter: “Pathology” by Morton Smith, MD, The Requisites in Ophthalmology, ed. Krachmer, 2002. Eye Pathology: An Atlas and Basic Text. Eagle, 1999. American Academy of Ophthalmology BCSC, “Ophthalmic Pathology and Intraocular Tumors.” 87 OPHTHALMIC PLASTIC/ORBITAL DISEASE Objectives: 1. First year resident: a. Develop an understanding of the embryology and anatomy of the ocular adnexa, including the eyelid, lacrimal system, and orbit. (MK) b. Demonstrate an ability to perform a clinical evaluation of the ocular adnexa. (PC, MK, P) c. Demonstrate an understanding of the principals and techniques applied to the management of acute adnexa trauma. (PC, MK, P) 2. Third year resident: a. Develop a command of the embryology and anatomy of the ocular adnexa, including the eyelid, Lacrimal system, and orbit. (MK, P) b. Demonstrate complete capability to perform a clinical evaluation of the ocular adnexa. (MK, P) c. Demonstrate a command of the principals and techniques applied to the management of acute adnexal trauma. (MK, P) d. Demonstrate an understanding of the pathophysiology, diagnosis, and management of: dermatochalasis, brow ptosis, blepharoptosis, entropion, ectropion, trichiasis, eyelid retraction, facial dystonia, skin neoplasms, Lacrimal gland masses, lacrimal outflow dysfunction, anophthalmic socket, and orbital inflammatory diseases. (MK, P) e. Demonstrate an appropriate knowledge involving surgical anatomy and decision making. (MK, TS) Required write-ups: Provide Dr. Liu with a 2-5 page typewritten write-up detailing what you plan to do in each of the following situations. Write a detailed management plan beginning with your pre-operative evaluation. This includes some of the specific tests that you plan to do, what you look for or what to avoid, and so on. Explain how you prepare the patient and his/her family and how to properly word the consent. Tell me what specific instruments, equipments, sutures or special materials you need in each situation. Highlight some of the key steps of your proposed operation and in your pre-, intra- and post-operative orders, and other precautions you take. These are real life situations which all ophthalmologists face. The knowledge and skills are essential and of critical importance and should become your second nature. (PC, PBLI) This is essentially an open-book exam. Unless special provision is made before the start of the rotation, Dr. Liu must receive your write-up at the halfway point of your rotation, i.e. at the end of the first month on the service. This allows time to discuss and revise your work. 88 1. First year resident: (MK, TS, P) a. ruptured globe b. lacerated eyelids, involving lid margin and canaliculus c. orbital foreign body injury, metallic and non-metallic d. must be turned in before end of rotation 3. Third year resident: (MK, P, TS) a. dog bite to lids/face b. orbital blow out fracture c. chemical/burn injuries to the globe/lids/face d. must be turned in before end of rotation Resources: (MK, PBLI) Techniques in Ophthalmic Plastic Surgery with DVD: A Personal Tutorial Nerad Jeffrey A., Saunders Elsevier, Philadelphia, 2010 Disease of the Orbit: A Multidisciplinary Approach Rootman .J, Lippincott Williams & Wilkins, Co, Philadelphia, 2002 2nd Edition. Ophthalmic Pathology Yanoff M., Fine. B, Mosby –Wolfe, Philadelphia, 1996 4th Edition. Color Atlas of Oculoplastic Surgery Tse, David T. Lippincott Williams & Wilkins, Philadelphia, 2011. Required Reading: A suggested reading list will be available to the resident at the onset of the Oculoplastics rotation. It is the resident’s responsibility to acquire the list from Dr. Liu or his secretary during the first week of the rotation. Successful completion of the Oculoplastics rotation requires the reading and understanding of a minimum of thirty (30) articles from the suggested reading list. A completed readings citation form will be available from Ms. Stock. This form should be completed as each article is read. The completed form will be submitted to Ms. Stock or Dr. Liu at the rotation’s end. In-service Examination: An in-service examination will be given during the final week of the Oculoplastics rotation. The scope of examination will include all aspects of lacrimal, orbital, and ocular adnexal disease. Successful completion of the rotation requires a passing grade of 70% or greater on the examination. 89 PEDIATRIC AND STRABISMUS SERVICE Objectives: 1. Examine and evaluate infants in the intensive care nursery for retinopathy of prematurity. (PC, ICS) 2. Examine and evaluate children and adults with strabismus. (PC, ICS) 3. Perform strabismus surgery under direct supervision, usually recess-resect, transposition procedures as well as oblique procedures. (TS, PC) 4. Microscopic surgery for cataract and glaucoma. (PC, TS) 5. Nasolacrimal duct probing and intubation. (PC, TS) 6. Recognition of the genetic and metabolic eye diseases. (MK) 7. Systemic disease with ocular manifestations. (MK) 8. Develop a clinical research project for presentation at a national meeting. (P) Recommended Reading: (MK, PBLI) Ophthalmic Pathology. Yanoff M, Fine, B; Mosby-Wolfe 2002 Binocular Vision and Ocular Motility: Theory and Management of Strabismus. Gunter K. Von Noorden., CV Mosby. Atlas of Ophthalmic Surgery: Techniques, Complications. Edited by Klaus Heilmann, David, Paton and G. Thieme Verlag. Thieme-Stratton, 3 volumes. Journal of Pediatric Ophthalmology & Strabismus (in the department library – published 6 times per year.) 90 VITREORETINAL SERVICE Objectives: 1. Development of Basic Skills Including: (MK, PC, ICS, P) Understanding importance and techniques of history taking Retinal documentation, including formal fundus drawings and description of retinal findings Slit lamp examination Comprehensive retinal examination using indirect ophthalmoscopy, scleral depression, fundus and contact lens techniques Fluorescein angiography Basic electrophysiology and psychophysics Diagnostic Ultrasonography 2. Vitreoretinal Complications of Anterior Segment Surgery (MK,P, TS) Endophthalmitis Retained lens fragments Dislocated IOL Choroidal hemorrhage/effusion Cataract surgery and uveitis 3. Diagnosis/Management of Diabetic Retinopathy (MK, P, TS) Diabetic macular edema Proliferative diabetic retinopathy Surgical decision-making Rubeotic Glaucoma 4. Retinal Vascular Disorders (MK, P, TS) Hypertensive retinopathies Central retinal vein occlusion Branch retinal vein occlusion Central and Branch retinal artery occlusion Radiation Retinopathy Hemoglobinopathies Radiation Retinopathy 5. Diagnosis and Management of Macular Disease (MK, P, TS) Age-related macular degeneration Genetic maculopathies Macular holes Cystoid macular edema Central serous chorioretinopathy Epiretinal Membranes 6. High Myopia (MK) 7. Peripheral Retinal Disorders (MK) Lattice and other vitreoretinal degenerations Genetic abnormalities Retinal tears Subclinical retinal detachments 91 8. Retinal Detachments (MK, P, TS, PC) Rhegmatogenous retinal detachments Tractional retinal detachments Exudative retinal detachments Surgical decision-making 9. Uveitis/Endophthalmitis (MK, P) Anterior uveitis Intermediate uveitis Posterior uveitis Ocular complications of AIDS 10. Genetic Chorioretinal Diseases (MK, P) 11. Ocular Tumors (MK, P) 12. Surgical Skills (MK, TS, PC, ICS) Correlative anatomy Management of ocular trauma Laser techniques: Panretinal photocoagulation Focal and grid macular laser photocoagulation Ablative photoablation of choroidal neovascular membranes Retinal hole prophylactic laser Laser management of branch and central retinal vein occlusions Retinopathy of prematurity Retinal Detachment and Vitrectomy Surgeries Resources: (MK, PBLI) American Academy of Ophthalmology, Basic and Clinical Science Course, Section 11: Retina and Vitreous, Section 9: Intraocular Inflammation and Uveitits. Benson WE. Retinal Detachment: Diagnosis and Management, 2nd Edition. Lippincott. Peyman GA and Schulman JA. Intravitreal Surgery: Principles and Practice, 2nd edition. Appleton-Century-Crofts. Ryan SJ. Retina (2nd edition). Mosby. Jalkh A and Celerio W. Atlas of Fluorescein Angiography. WB Saunders. Freeman WR. Practical Atlas of Retinal Disease and Therapy. Raven. Nussenblatt RB, Whitcup SM, Palestine AG. Uveitis: Fundamentals and Clinical Practice. Mosby. Hampton GR, Nelsen PT. Age Related Macular Degeneration: Principles and Practice. Raven. Shields JA and Shields CL. Intraocular Tumors: A Text and Atlas. Saunders. Gass J. Stereoscopic Atlas of Macular Diseases: Diagnosis and Treatment, 4th edition. Mosby. Yannuzi, Guyer, Green. Retina Atlas. Mosby. 92 CLINIC ROTATION DESCRIPTIONS First Year Residents (PGY-II) Rotation: Emergency Service Months: Days: 2 rotations of 2 months each (not consecutive) All days covering Emergency Clinic. Duties and Responsibilities – Emergency Service: 1) 2) 3) 4) Rotation: Patient examination and evaluation. Obtain necessary tests. Determine and execute treatment plan, with faculty input. Read and know the “Uveitis” and “Lens” sections of the AAO Basic Science handbooks. (You will be the expert in uveitis.) Cornea/External Disease 2 Month Rotation (Please refer to the detailed rotation schedules for the year.) Duties and Responsibilities – Cornea/External Disease Service: 1) 2) 3) 4) Rotation: Superficial keratotomy Entire responsibility for keratoplasty for those interested and who have sufficient supervised micro surgery on animal eyes. Assisting experience in human keratoplasty. Observe and assist in refractive surgery. Oculoplastics 2 Month Rotation (Please refer to the detailed rotation schedules for the year.) Duties and Responsibilities – Oculoplastics Service: 1) 2) 3) 4) 93 Interview and evaluate patients with conditions pertaining to the ocular adnexa. Develop an understanding and expertise in the anatomy of the eyelid, orbit and lacrimal outflow system. Develop an understanding of the pathophysiology of conditions pertaining to the ocular adnexa. Develop treatment plans and assist in ocular adnexal surgeries. Rotation: Neuro-Ophthalmology/Consults and Low Vision/ Optometry Services 2 rotations of 2 months each (not consecutive) (Please refer to the detailed rotation schedules for the year.) Wednesday afternoon rotation will be in Low Vision / Optometry Services. (Residents may be eligible for early completion of Low Vision rotation based on meeting course objectives and required reading assignments, attendance and a score of 86% or better on rotation exam. Please discuss any request for early completion with Low Vision Coordinator.) Duties and Responsibilities – Neuro-Ophthalmology Service: The Neuro-Ophthalmology/Consults resident spends four half-days in the NeuroOphthalmology outpatient suite with Dr. Johnson, our neuro-ophthalmologist. The resident will obtain comprehensive histories and perform complete neuro-ophthalmologic examinations on all new neuro-ophthalmologic outpatient consults. The resident also will evaluate return (follow-up) neuro-ophthalmologic patients, but in a more directed/tailored manner. Evaluation and management plans will then be jointly formulated by Dr. Johnson and the Neuro-Ophthalmology/Consult resident. The resident will dictate for new patients only a detailed letter to the referring physician, including current journal references when appropriate. These letters are reviewed by Dr. Johnson with the residents thereby promoting increased knowledge of Neuro-Ophthalmology and community physician interactions. The Neuro-Ophthalmology/Consult resident, in general, will obtain comprehensive histories and perform complete ophthalmologic examinations on all inpatient consults. The resident will then formulate an assessment and management plan for each consult. Thereafter, the resident and Dr. Johnson, the faculty member chiefly responsible for supervising inpatient consults, will jointly evaluate the patients. The inpatient consults reflect a wide spectrum of diseases with primary emphasis on orbital/facial trauma, posttraumatic brain injury, strokes, and systemic diseases with ophthalmologic manifestations (e.g. diabetes mellitus). Although listed as four half-days per week, inpatient consults are evaluated daily during the work week and after regular clinic hours. Second Year Residents (PGY-3) Rotation: Retina/Vitreous 4 Month Rotation (Please refer to the detailed rotation schedules for the year.) Duties and Responsibilities – Retina/Vitreous Service: 1) 2) 3) 4) 5) 6) 94 Obtain relevant histories. Document ocular findings and progress notes. Slit lamp examination of the anterior segment. Gonioscopy. Direct ophthalmoscopy. Indirect ophthalmoscopy with scleral indentation and drawing of the retina. 7) 8) Slit lamp fundus biomicroscopy with contact lenses. Interpretation of fundus fluorescein angiography. All residents are expected to perform panretinal laser photocoagulation for various proliferative retinopathies. Depending on the volume of retinal detachment cases, occasionally residents will be able to perform scleral buckling procedures under direct staff supervision. Residents will also do many of the steps in a routine pars plana vitrectomy under the direct supervision of the attending. Rotation: Pediatrics (If no pediatrics please see General Ophthalmology below) 4 Month Rotation (Please refer to the detailed rotation schedules for the year.) Duties and Responsibilities – Pediatric/Strabismus Service: 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) Examine and evaluate infants in the intensive care nursery for retinopathy of prematurity. Accurately measure children and adults with strabismus. Perform strabismus surgery under direct supervision. Recognition of the genetic and metabolic eye diseases. Perform induced tropia test for preverbal visual acuity. Perform prism convergence test for motor fusion. Perform W4D, Bagolini, and stereo acuity to monitor sensory status. Retinoscopy Evoked saccades/confrontational VF. ICARE IOP testing. Retcam photography. Pediavision screening. Forced ductions. VEP interpretation. Counsel patching therapy. *****Note- No more than 2 weeks off Pediatric rotation(including vacation and meeting time).** Rotation: VA/General Ophthalmology 4 Month Rotation (Please refer to the detailed rotation schedules for the year.) Duties and Responsibilities – VA/General Ophthalmology: 1) 2) 95 The resident physician will obtain a complete ophthalmological history and an applicable general medical history. The resident will do a complete ophthalmological examination. a) This to include visual acuity testing (and refraction of optical defects of the eye including retinoscopy as indicated). b) Confrontation fields. c) Orbital and external exam. d) Ocular motility exam. e) f) g) 3) 4) 5) 6) 7) 8).. Pupillary evaluation. Anterior segment exam with slit lamp biomicroscopy. Posterior segment evaluation using direct and indirect ophthalmology (including biomicroscopy of the fundus as indicated). h) Intraocular pressure testing. i) Also, when applicable, learn to do color vision testing, Amsler Grid and Maddox rod testing, gonioscopy, conjunctival and corneal scrapings, lacrimal evaluation, A and B scan techniques, and keratometry. j) Learn the appropriate indications for ordering automated or quantitative perimetry, fluorescein angiography, ocular photography, light or pattern evoked electrical potential tests (ERG, VEP), and specular microscopy. k) Prescribe glasses or contact lenses as dictated by findings. The resident physician will complete a differential diagnosis and treatment regimen. The resident will review with the patient, his diagnosis, prognosis and treatment regimen. The resident will review any special tests ordered in a timely manner and discuss these results with the attending staff. The resident will treat the patient as medically or surgically indicated and see the patient for appropriate follow-up care. The resident will complete the medical record to include all the above information as appropriate. The resident will become familiar and competent with a surgical microscope and instruments; perform anterior segment surgery in the wet lab. The resident will perform extracapsular cataract extraction or phacoemulsification with or without intraocular lens, under direct supervision. The resident will become proficient with phacoemulsification anterior segment reconstruction, trabeculectomies, and glaucoma tube shunts. Third Year Resident (PGY-4) Rotation: Cornea/External Disease 2 Month Rotation (Please refer to the detailed rotation schedules for the year.) Duties and Responsibilities – Cornea/External Disease: 1) 2) 3) 4) Rotation: Superficial keratotomy. Entire responsibility for keratoplasty for those interested and who have sufficient supervised micro surgery on animal eyes. Assisting experience in human keratoplasty. Observe and assist in refractive surgery. Oculoplastics 2 Month Rotation (Please refer to the detailed rotation schedules for the year.) Duties and Responsibilities – Oculoplastics Service: 1) 2) 96 Interview and evaluate patients with conditions pertaining to the ocular adnexa. Develop an understanding and expertise in the anatomy of the eyelid, orbit and lacrimal outflow system. 3) 4) 97 Develop an understanding of the pathophysiology of conditions pertaining to the ocular adnexa. Develop treatment plans and assist in ocular adnexal surgeries. Rotation: Glaucoma 4 Month Rotation (Please refer to the detailed rotation schedules for the year.) Duties and Responsibilities – Glaucoma Service: 1) 2) 3) 4) 5) Rotation: Patient examination and evaluation. Visual fields. Gonioscopy. Laser therapy. Glaucoma surgery. VA Hospital/General Ophthalmology 4 Month Rotation Duties and Responsibilities: 1) The resident physician will obtain a complete ophthalmological history and an applicable general medical history. 2) The resident will do a complete ophthalmological examination. a) This to include visual acuity testing (and refraction of optical defects of the eye including retinoscopy as indicated). b) Confrontation fields. c) Orbital and external exam. d) Ocular motility exam. e) Pupillary evaluation. f) Anterior segment exam with slit lamp biomicroscopy. g) Posterior segment evaluation using direct and indirect ophthalmology (including biomicroscopy of the fundus as indicated). h) Intraocular pressure testing. i) Also, when applicable, perform vision testing, Amsler Grid and Maddox rod testing, gonioscopy, conjunctival and corneal scrapings, lacrimal evaluation, A and B scan techniques, keratometry and IOL Master. j) Learn the appropriate indications for ordering automated or quantitative perimetry, fluorescein angiography, ocular photography, light or pattern evoked electrical potential tests (ERG, VEP), and specular microscopy. k) Prescribe glasses or contact lenses as dictated by findings. 3) The resident physician will complete a differential diagnosis and treatment regimen. The resident will review with the patient, his diagnosis, prognosis and treatment regimen. The resident will review any special tests ordered in a timely manner and discuss these results with the attending staff. 4) The resident will treat the patient as medically or surgically indicated and see the patient for appropriate follow-up care. 5) The resident will complete the medical record to include all the above information as appropriate. 6) The resident will become familiar and competent with a surgical microscope and instruments; perform anterior segment surgery in the Wet lab. 7) The resident will perform extracapsular cataract extraction or phacoemulsification with or without intraocular lens, under direct supervision. 98 8) 9) The resident will become proficient with phacoemulsification anterior segment reconstruction, trabeculectomies, and Glaucoma tube shunts. The resident will be proficient in the use of the electronic health record at the VA including CPRS and MedFlow. First, Second and Third Year Residents (PGY2-PGY4) General Ophthalmology/Resident General Clinics Residents are assigned some general clinics at the university each year, as listed in the monthly rotation schedules. Duties and Responsibilities: 1) 2) 3) 4) 5) 6) 99 The resident physician will obtain a complete ophthalmological history and an applicable general medical history. The resident will do a complete ophthalmological examination. a) This to include visual acuity testing (and refraction of optical defects of the eye including retinoscopy as indicated). b) Confrontation fields. c) Orbital and external exam. d) Ocular motility exam. e) Pupillary evaluation. f) Anterior segment exam with slit lamp biomicroscopy. g) Posterior segment evaluation using direct and indirect ophthalmology (including biomicroscopy of the fundus as indicated). h) Intraocular pressure testing. i) Also, when applicable, learn to do color vision testing, Amsler Grid and Maddox rod testing, gonioscopy, conjunctival and corneal scrapings, lacrimal evaluation, A and B scan techniques, and keratometry. j) Learn the appropriate indications for ordering automated or quantitative perimetry, fluorescein angiography, ocular photography, light or pattern evoked electrical potential tests (ERG, VEP), and specular microscopy. k) Prescribe glasses or contact lenses, or low vision aid as dictated by findings. The resident physician will complete a differential diagnosis and treatment regimen. The resident will review with the patient, his diagnosis, prognosis and treatment regimen. The resident will review any special tests ordered in a timely manner and discuss these results with the attending staff. The resident will treat the patient as medically or surgically indicated and see the patient for appropriate follow-up care. The resident will complete the medical record to include all the above information as appropriate. The resident will become familiar and competent with a surgical microscope and instruments; perform anterior segment surgery in the animal lab. 7) 8) The resident will perform extracapsular cataract extraction or Phacoemulsification with or without intraocular lens, under direct supervision. The resident will become proficient with phacoemulsification anterior segment reconstruction, trabeculectomies, and Molteno valves. The rotations as listed above are standard. Naturally, due to vacation, Basic Science Course (San Antonio, Wills or other) and other external meetings (such as AAO or ARVO), some modifications occur during the year. Residents in each year are allowed three weeks’ for vacation or interviews and one additional week for meetings. Resident supervision in the General Clinic is the primary responsibility of Geetha Davis, MD, Theodore Wills, MD and Kathy Lentz, MD. In the absence of the primary supervising attending, other supervising faculty persons are assigned. See Ophthalmology Attending Coverage Calendar for Residents General Clinic for attending assigned to supervise the general clinics for each half day. Residents in sub-specialty clinics are supervised by the attending physician of the service. Patients are scheduled with the attending physician for all sub-specialty clinics. For sub-specialty clinics, the attending assigns the resident to initially see most of the patients on the schedule. When this occurs, the attending sees the patient after the evaluation. The resident progressively assumes greater responsibility during pre-evaluations. All patients who are admitted to the hospital are admitted to the service of a specific attending physician and the care is closely supervised by that physician. The resident is involved in the dayto-day care of the inpatients with daily discussions of the treatment plan with the attending physicians. Residents are responsible for daily rounding with progress notation for all inpatients receiving primary or consultatory care through the ophthalmology services. On patients admitted to ophthalmology services, the resident is responsible for the ophthalmic and general medical H/P, and discharge summary. 100 RESIDENT INSTRUCTION/SUPERVISION Instruction in Ethical Issues, Socioeconomics of Heath Care, Cost-Effective Medical Practice (Narrative Description for Resident Supervision) University of Missouri-Columbia The following is a list of programs that enable our residents to develop an understanding of ethical, socioeconomic and medical-legal issues. Each year a medical-legal conference is presented in the department by legal counsel member of the University of Missouri System. In July a “compliance” conference is moderated by the Office of Corporate Compliance regarding University Physicians Compliance and federal regulations covering medical billing. University Risk Management speaks with the new residents at the Hospital Orientation in July. The practice of medicine in an ethical manner is reflected in part in the quality of care that is perceived by our patients. The Chairman of the Department of Ophthalmology Quality Assurance Committee provides information to the residents about quality assessment and improvement in our Ophthalmology Program. Monthly Resident Practice Management Meetings are conducted by the Resident Program Director and Resident Program Coordinator. A formal agenda is prepared. Ethical, socioeconomic, and cost containment issues are included. Each new resident receives a Resident Orientation. This orientation provides formal training in cost containment issues by our billing and coding specialist, as well as a session in risk management. The ethical nature of performing surgery or prescribing medical management of patients is discussed on an individual basis and in case conferences. Ethical issues and socioeconomic issues are an ongoing issue with every patient. The first year residents receive, the American Academy of Ophthalmology Basic & Clinical Science Course books, which includes The Profession of Ophthalmology: Practice Management, Ethics and Advocacy and Basic Principles of Ophthalmic Surgery 1. Faculty assignments Faculty assignments are handled through the Chairman’s office. Dr. Theodore Wills has the primary responsibility for supervision of General Clinics and functions in this role. In his absence, other faculty (active or courtesy) are assigned. A monthly assignment schedule is distributed at the end of the preceding month. The name of the daily supervising attending is visibly displayed in the clinic. All residents are aware by both methods who the supervising attending is on any day. 2. Faculty Location and Activity Faculty assigned to direct supervision in the clinic are physically located in the clinic or adjoining faculty offices, while surgery supervisors are physically present in the operating room for, most or all of the procedures are expected to function in that role. At times faculty supervision may be diverted or delayed due to a patient call, etc. When emergencies occur necessitating the absence of the supervising physician, an alternate supervising attending physician is assigned. 101 3. Selection of visits for direct faculty supervision Direct faculty supervision is provided for nearly all patients examined by the residents. The extent of re-examination of patients by faculty depends on the level of experience of the resident. Patients assigned to the resident clinic are initially evaluated by the resident then presented to the attending. Sub-specialty patients are generally seen in conjunction with the faculty person. 4. Techniques of faculty supervision The faculty members: a.) Review of resident’s findings within patient exam room. b.) Review of resident’s findings within discussion with patient. c.) Patient examined with the resident. 5. Emergency care (faculty supervision) Monday-Friday, during regular hours: The assigned faculty supervisor provides supervision. (Please also refer to #1. Faculty Assignments.) Evenings and Weekends: The attending on call is available by telephone; the attending comes in to see the patient when direct faculty supervision is necessary, as deemed by the faculty or at the resident’s request. Whenever there is any question as to need for direct faculty supervision, the oncall faculty member will come in to evaluate the patient with the resident. Residents on-call have approval from the faculty to accept all referrals from referring physicians. 6. Documentation of faculty supervision *Faculty write notes and sign the medical records at the time of patient evaluation. Monthly, the residents are given a copy of the following: *Ophthalmology Resident Clinic Attending Calendar *Ophthalmology Call Schedule *Ophthalmology Lecture & Event Calendar *Ophthalmology VA Attending Calendar 102 OPHTHALMOLOGY: VA HOSPITAL STATEMENT OF PURPOSE The purpose of ophthalmology residency training at the Harry S. Truman Memorial Veterans Hospital, is to provide an optimal clinical education to physicians in the science and art of the specialty of ophthalmology; all functions of the department are structured to maximize this educational mission. Resident physicians are expected to: develop a personal program of self-study and professional growth with guidance from the teaching staff. Participate in safe, effective and compassionate patient care under supervision. Participate fully in the educational activities of their program and, as required, assume responsibility for teaching and supervising other residents and students; participate in institutional programs and activities involving the medical staff and adhere to established practices, procedures and policies of the institutions, participate in institutional committees and councils, especially those that relate to patient care review activities, and apply cost containment measures in the provision of patient care. The VA ophthalmology resident rotation is designed to foster independent patient evaluation and management commensurate with their level of advancement and responsibility. Resident physicians are expected to achieve the 7 ophthalmology competencies of: Patient Care – PC Medical Knowledge – MK Interpersonal and Communication Skills – ICS Professionalism – P Practice-based Learning and Improvement – PBLI Systems-based Practice – SBP Technical/Surgical Skill – TS During the tenure of the residency, residents should accomplish the following: develop a personal program of self-study and professional growth with guidance from the teaching faculty (MK) participate in safe, effective and compassionate medical and surgical patient care under supervision, commensurate with their level of advancement and responsibility (PC,TS,MK,P,SBP) participate fully in the educational activities of their program and, as required, assume responsibility for teaching and supervising other residents and students (PBLI,MK,ICS) participate in institutional programs and activities involving the medical staff and adhere to established practices, procedures and policies of the institutions (ICS,PBLI,P) participate in institutional committees and councils, especially those that relate to patient care review activities (P,ICS,SBP) apply cost containment measures in the provision of patient care (SBP) 103 Participating Institution - VA Hospital (Narrative Description for Resident Supervision) 1. Faculty assignments. How are supervising faculty assigned? For what time period? In what way are they identified to the residents concerned? Faculty assignments are handled through the Chairman’s office. Dr. Frank Rieger, the Local Director, has the primary responsibility for supervision of clinic and surgery. All residents are aware of his role. For sub-specialty cases, the resident contacts the appropriate attending for consultation and, as necessary, supervision. Dr. Rieger maintains general oversight, however, of all patient care. Other faculty (active or courtesy) are assigned to supervise clinic or surgery as well. A monthly assignment calendar is distributed for VA clinic and surgery days. 2. Faculty Location and Activity. Where are supervising faculty physically located during assigned supervision periods? Are such faculty involved in activities other than direct supervision during these period? Clinic Supervision: Dr. John Cowden (cornea) covers VA clinic (2, 4) and an as needed basis when a faculty member is scheduled out. Dr.Davis (general ophthalmology) covers VA surgery (1 & 5 Thursday AM) alternating with Dr. Reyes) covers VA clinic (1, Friday Morning) Dr. Dean Hainsworth (retina/vitreous) covers VA retina surgery (2, 4) Wednesday mornings and clinic (2, 3, 4, 5) Thursday mornings. Dr. Bokkwan Jun (neuro-ophthalmology) covers the VA Clinic (1,3) Tuesday mornings Dr. Don Liu (Oculoplastics) covers VA clinic every Monday morning, surgery (1, 3, 5) Wednesdays, clinic (2, 4) all day Wednesday; staff clinic Thursday morning and every Friday afternoon. Dr. Marcos Reyes (glaucoma) VA clinic (2, 4) Wednesday afternoons, and glaucoma surgery (2, 4) Thursday mornings. Dr. Frank Rieger Chief of Eye Service at the VA Hospital and is onsite and available 100% of the time. He sees his own patients (cornea & general) on Monday, Wednesday and Friday afternoons and all day Thursday. He is available to staff surgery and clinic all day Tuesdays. Dr. Scott McKnight, Courtesy Faculty staffs VA surgery the third Tuesday of most months all day. Dr. Jeff Wongskhaluang , Courtesy Faculty staffs VA surgery the third Thursday of most months all day. Please note: For any potential new faculty members joining the Department of Ophthalmology their schedules at the VA have not been finalized by the date of this manual printing. Surgery Supervision: All Ophthalmology surgeries in the OR are staffed by an attending physician. (See VA Week-day Attending Calendar) If a doctor is assigned to the VA (either OR or eye clinic), he/she should be physically at the VA. University subspecialists, not assigned to the VA Hospital Eye Clinic, are available for telephone consultation and sometimes on site consultations. 3. Selection of visits for direct faculty supervision. What is departmental policy as to which patient visits are to have direct faculty supervision? What instructions are given as to when to 104 initiate such direct supervision? Is the initiation of direct supervision primarily the responsibility of faculty or of residents? In the weekday operation of the outpatient clinic at the VA the attending must be personally present in the clinic. Direct faculty supervision, as mandated by the Department of Veterans (see attachement) Affairs, is provided for all patients examined by the residents. The patient is either seen by the attending or discussed with the resident. There is at least one attending physician assigned to the VA Eye Clinic every morning and afternoon Monday-Friday. Residents have ready access to any of the faculty members at the University for Telephone Consultation or direct consultation virtually any time during the day or evening hours. This can be done by having the faculty member see the patient at the VA Hospital or presenting a difficult or particularly challenging patient at grand rounds which are held once a month. Subspecialty patients are evaluated by the respective attending prior to scheduling surgical procedures. Cataract surgery patients are evaluated by the clinic attending preoperatively. Dr. Frank Rieger is onsite and available to see patients with the residents 100% of the time. 4. Techniques of supervision. In what way is direct faculty supervision provided? What provision is made to provide for consistent faculty supervision of post-operative care of Class 1 patients? a. b. c. 5. Direct faculty supervision at the VA Hospital is provided by having the faculty member physically present in the clinic at all times and providing resident supervision according to VA guidelines. The resident can also obtain a telephone consultation from a faculty member concerning a patient once the initial evaluation is done by the resident. This is typically a patient in need of subspecialty care and the needed subspecialist is not assigned to the VA clinic that day. Post-operative care for routine cases (cataract extractions) is administered by the residents with supervision by the attending physician assigned to the VA clinic. Subspecialty procedures are supervised postoperatively by the subspecialist involved in the surgical care of that patient. Emergency care. What special provision is made for direct faculty supervision of emergency visits? Monday-Friday, during regular hours: The assigned faculty supervisor is physically present at the VA Hospital Eye Clinic to provide supervision. Evenings and Weekends: The attending on call is available by telephone; the attending comes in to see the patient when direct faculty supervision is necessary. 6. Documentation. In what way is direct faculty supervision identifiable and documented? *Faculty note and electronic signature on chart in accordance with VA guidelines for resident supervision. Monthly the residents are given a copy of the following calendar/schedule: 105 *Ophthalmology Resident Clinic Attending Calendar *Ophthalmology Call Schedule *Ophthalmology Lecture & Event Calendar *Ophthalmology VA Attending Calendar 106 Insert “Resident Supervision Pocket Card – Office of Academic Affiliations” United States Department of Veterans Affairs http://www.va.gov/oaa/res-supervision-card-test.asp 107 VA Hospital Goals and Responsibilities for VA Ophthalmology Rotation Goals 1. To provide excellent medical and surgical ophthalmic care to the veterans using state of-theart knowledge and technology. To foster a teaching environment that allows the residents to progressively gain autonomy in their medical and surgical skills. To promote leadership skills that will become a part of the residents’ future practice patterns. To teach teamwork and respect for each member of the team. To ensure each resident is exposed to a vast array of ophthalmic problems and surgical cases. To promote an adequate hands-on surgical experience so that each resident is confident in their own surgical skills and cognizant of their own limitations. To provide continuity of care during the four month rotation and the one month post operative clinic. To teach the entire spectrum of patient care to include administrative duties, electronic medical record management as well as surgical and clinic scheduling. To be knowledgeable of advancements in information technology with an emphasis on medical practice. 2. 3. 4. 5. 6. 7. 8. 9. Duties These duties are progressively applied to the 2nd and 3rd year resident. A higher level expertise is expected in the 3rd year resident. Second Year Resident (PGY-3) - VA Hospital Duties and Responsibilities VA/General Ophthalmology Months: Days: 4 Mon AM – VA Clinic Tues AM – VA Surgery Wed AM – VA Clinic Thurs AM – VA Surgery Fri AM – VA Clinic PM – VA Clinic PM – VA Surgery PM – VA Clinic PM – VA Surgery PM – VA Clinic Duties and Responsibilities: 1) 2) 108 The resident physician will obtain a complete ophthalmological history and an applicable general medical history. The resident will do a complete ophthalmological examination. a) This to include visual acuity testing (and refraction of optical defects of the eye including retinoscopy as indicated). b) Confrontation fields. c) Orbital and external exam. d) Ocular motility exam. e) Pupillary evaluation. f) Anterior segment exam with slit lamp biomicroscopy. g) Posterior segment evaluation using direct and indirect ophthalmology (including biomicroscopy of the fundus as indicated). h) Intraocular pressure testing. i) j) k) l) m) n) o) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 109 Also, when applicable, learn to do color vision testing, Amsler Grid and Maddox rod testing, gonioscopy, conjunctival and corneal scrapings, lacrimal evaluation, A and B scan techniques, keratometry, and IOLMaster and Lenstar. Learn the appropriate indications for ordering automated or quantitative perimetry, fluorescein angiography, ocular photography, light or pattern evoked electrical potential tests (ERG, VEP), and specular microscopy. Prescribe glasses or consults for contact lenses as dictated by findings. Ocular Coherence Tomography (OCT). Wavefront analysis (OPD) Pentacam Confocal microscopy and specular microscopy The resident physician will complete a differential diagnosis and treatment regimen. The resident will review with the patient, his diagnosis, prognosis and treatment regimen. The resident will review any special tests ordered in a timely manner and discuss these results with the attending staff. The resident will treat the patient as medically or surgically indicated and see the patient for appropriate follow-up care. The resident will complete the medical record to include all the above information as appropriate. The resident will become familiar and competent with a surgical microscope and instruments; perform anterior segment surgery in the wet lab. The resident will perform extracapsular cataract extraction or phacoemulsification with or without intraocular lens, under direct supervision. They will also learn about pre-op evaluation and biometry and post-op care. The resident will become proficient with phacoemulsification anterior segment reconstruction, trabeculectomies, and glaucoma tube shunts. Oculoplastics procedures, Pterygium removal,Laser photocoagulation for CSME (clinically significant macular edema) and proliferative diabetic retinopathy YAG Laser Posterior capsulotomies Iridectomies Assist and perform some steps of penetrating kerotoplasties and DSAEK procedures. Minor in-office procedures Third Year Resident (PGY-4) - VA Hospital Duties and Responsibilities VA/General Ophthalmology Months: Days: 4 Mon AM – VA Clinic Tues AM – VA Surgery Wed AM – VA Clinic Thurs AM – VA Surgery Fri AM – VA Clinic PM – VA Clinic PM – VA Surgery PM – VA Clinic PM – VA Surgery PM – VA Clinic Duties and Responsibilities: 1) 2) 3) 4) 5) 6) 7) 110 The resident physician will obtain a complete ophthalmological history and an applicable general medical history. The resident will do a complete ophthalmological examination. a) This to include visual acuity testing (and refraction of optical defects of the eye including retinoscopy as indicated). b) Confrontation fields. c) Orbital and external exam. d) Ocular motility exam. e) Pupillary evaluation. f) Anterior segment exam with slit lamp biomicroscopy. g) Posterior segment evaluation using direct and indirect ophthalmology (including biomicroscopy of the fundus as indicated). h) Intraocular pressure testing. i) Also, when applicable, learn to do color vision testing, Amsler Grid and Maddox rod testing, gonioscopy, conjunctival and corneal scrapings, lacrimal evaluation, A and B scan techniques, keratometry, and IOL Master and Lenstar. j) Learn the appropriate indications for ordering automated or quantitative perimetry, fluorescein angiography, ocular photography, light or pattern evoked electrical potential tests (ERG, VEP), and specular microscopy. k) Prescribe glasses or contact lenses as dictated by findings. The resident physician will complete a differential diagnosis and treatment regimen. The resident will review with the patient, his or her diagnosis, prognosis and treatment regimen. The resident will review any special tests ordered in a timely manner and discuss these results with the attending staff. The resident will treat the patient as medically or surgically indicated and see the patient for appropriate follow-up care. The resident will complete the medical record to include all the above information as appropriate. The resident will become familiar and competent with a surgical microscope and instruments; perform anterior segment surgery in the wet lab. The resident will perform extracapsular cataract extraction or phacoemulsification with or without intraocular lens, under direct supervision. 8) 9) 10) 11) 12) 111 The resident will become proficient with phacoemulsification anterior segment reconstruction, trabeculectomies, and glaucoma tube shunts. Oculoplastics procedures,Pterygium removal,Laser photocoagulation for CSME (clinically significant macular edema) and proliferative diabetic retinopathy YAG Laser Posterior capsulotomies Iridectomies Assist and perform some steps of penetrating kerotoplasties and DSAEK procedures. Minor in-office procedures Insert (yellow) VA Hospital Policy Memorandum 112 Insert “Program Letter of Agreement Between Harry S. Truman Memorial Veterans Administration Hospital Eye Clinic and the Department of Ophthalmology” 113 RESIDENT EVALUATIONS Resident performance is an agenda item for discussion at the monthly faculty meeting. This gives a frequent forum to bring up issues of concern, without waiting for the more formal evaluation process which occurs at the end of each four-month rotation. Issues which surface at the monthly faculty meetings help the faculty to pay attention to and work with the resident to improve any deficit. Global Evaluation A resident evaluation meeting is held every four months (November, March, and June). Prior to the meeting, each clinical faculty member submits an electronic Global Evaluation evaluating the competencies of each resident. This is submitted through the hospital resident program software New-Innovations. The completed evaluations for each individual resident are printed and distributed to the clinical faculty as a beginning point for discussion at the meeting. Each resident receives a copy of their compiled evaluation, followed by a meeting with the program director to review his/her evaluation. The program director and the resident sign the evaluation form and this document becomes a part of the resident’s permanent evaluation record. Sub-specialty Evaluation Sub-specialty rotation evaluations at the end of each rotation period also occur. These evaluations are conducted by the attending of that sub-specialty rotation, signed by the resident and attending, and become part of the resident’s permanent evaluation file. The faculty member will submit an electronic Sub-specialty Evaluation. That evaluation will then be forwarded to the resident to review and sign. A copy of this evaluation will be signed by the attending and the resident on service. This sub-specialty evaluation becomes part of the resident’s permanent evaluation record. Please see the following examples of the Global Evaluation and the Sub-specialty Evaluation forms. The evaluation questionnaires are loaded into the hospital resident software program New Innovations. However, will not appear in this format but the questions and rating will be the same. Clinical Skills and Procedures A list of clinical procedures and skills in which the residents check whether they “have done” or “can interpret” the items on the list. The skills list is given to the residents in March of every year, after the first year residents have gone through several months of clinical experience and education. 360-degree Evaluation The Accreditation Council for Graduate Medical Education (ACGME) has mandated that residents are to be evaluated on clinical skills and medical knowledge by teaching faculty and others. The ACGME has identified that patients, nurses, resident peers, and other MD and nonMD professional associates interact with residents in different contexts and situations that are unique. These “perspectives add relevance, credibility, and scope to the assessment of residents.” 114 The 360-degree evaluation will be given once a year during February and presented at random to faculty, patients, technicians, support staff and resident peers. Ophthalmic Clinical Evaluation Exercise (OCEX) The OCEX is an observed encounter between a resident and a new patient. The attending is present in the exam room for the entire interactions. The intent is to rate the resident in interview skills, examination, interpersonal skills/professionalism, case presentation, and provide immediate feedback. Ophthalmology Resident Surgical Skills Assessment Form Residents are to give this form to the physician they are working with on their surgical specialties rotation. A minimum of 2 evaluations are expected during a 4-month rotation and one evaluation is expected during a 2-month rotation. Residents are evaluated on: Preparation for operative procedure Operative procedure Procedure specific skills Postoperative care Educational Purpose of Evaluations They are used for performance improvement opportunities. The resident should have a clear picture of what performance and knowledge are expected of him/her by review of their evaluation. As well, review of the evaluation form itself as a guide to expected performance and knowledge. It should enhance residency education through outcome assessment. 115 CLINICAL SKILLS and PROCEDURES □ 1st Year Resident □ 2nd Year Resident □ 3rd Year Resident Please check whether you have performed the procedure/technique or you can interpret the results. Have done Can interpret □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ Comprehensive eye examination Gonioscopy, tonometry - all types Indirect Ophthalmology with scleral depression Contact lens fitting, lensometry Automated keratometry - Humphries Automated refraction - Humphries Low Vision examination, use of aids Retinoscopy, manifest and cycloplegic refraction Humphrey visual fields Goldmann visual fields Tangent screen visual fields Ultrasonic pachymetry A&B scan ultrasonography Specular microscopy Computerized corneal topography - Pentacam Slit lamp photography Fundus photography Fluorescein angiography Electrophysiological Studies - ERG, EOG, VER Optical coherence tomography (OCT) Intraocular lens (IOL) master YAG laser - capsulotomies, P.I. Argon Laser - PRP, ALT, PI, etc. Minor Surgical Procedures and Operating of Equipment e.g. Cryotherapy Unit Microscopes All Types Rust ring remover Electro-epilation Print Name:_______________________ Signature: ____________________________ Date : ________ 116 360-Degree Evaluation: Thank you for taking the time to complete this important survey. Please circle the number that best reflects the qualities that Dr. _________________has displayed. Questions/Statements Much Improvement Outstanding Needed The physician demonstrates or displays Average Not Applicable N/A 1. 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 Caring and Respectful behavior to a. Patients b. Family N/A N/A 2. Compassion and sensitivity to the needs of the patient 1 2 3 4 5 N/A 1 1 2 2 3 3 4 4 5 5 N/A N/A 1 1 2 2 3 3 4 4 5 5 N/A N/A 1 1 2 2 3 3 4 4 5 5 N/A N/A 9. Professional appearance (dress, grooming, interpersonal relationship) 1 2 3 4 5 N/A 10. Good hygiene practice (hand-washing, cleanliness, wiping instruments) 1 2 3 4 5 N/A 11. Commitment to excellence 1 2 3 4 5 N/A 3. Attentive listening to patient’s concerns 4. Satisfactory medical explanation to patient’s problems/concerns 5. Excellence in clinical care/knowledge 6. Consideration of patient’s privacy 7. Commitment to ethical principles 8. Good working relationship with other care provider staff Additional comments: ______________________________________________________________________________ ______________________________________________________________________________ Please indicate your position: Patient_____ Staff_____ Technician_____ Physician____ Other____ Thank you for completing the survey. 117 Insert New-Innovations Global evaluation questionnaire, Subspecialties evaluation questionnaires, Resident evaluation of rotations (Mason Eye Institute & VA Hospital Eye Clinic, and Resident evaluation of faculty 118 Insert OCEX form 119 OPHTHALMOLOGY RESIDENT SURGICAL SKILLS ASSESSMENT FORM Resident Name: ___________________________________ G first-year G second-year G third-year Attending Physician Name: __________________________ Patient Medical Record Number: _____________________ Name of Procedure: __________________________ The following form is to be completed by an attending physician that has observed you perform one of the following procedures: cataract surgery, glaucoma surgery, eye muscle recession or resection, eyelid surgery (ptosis, entropion, ectropion), retina or glaucoma laser. Legend: 1 = below expectations 2 = meets expectations 3 = exceeds expectations I. 1 2 3 GGG GGG GGG GGG GGG GGG GGG Preparation for operative procedure: II. 1 2 3 GGG GGG GGG Operative procedure: III. Procedure-specific skills: Please list at least four different maneuvers performed during the surgery that the resident either performed well or had some difficulty with i.e. wound construction, lens insertion, eye muscle isolation, scleral sutures, placement of skin sutures, etc. Aware of indications for procedure Knows the order of steps to perform procedure Familiarity with alternative approaches to procedure Familiarity with instrumentation and machinery when applicable Prepares OR appropriately Adequately performs and understands the implications of informed consent Aware of indications and contraindications for procedure Interacts with non-physician staff appropriately Able to perform all critical steps of the procedure while mindful of personal limits Understands common complications and how to handle them 1 2 3 G G G _______________________________________________________________________________________ G G G _______________________________________________________________________________________ G G G _______________________________________________________________________________________ G G G _______________________________________________________________________________________ IV. Postoperative care: 1 2 3 GGG GGG GGG GGG Familiarity with appropriate coding for procedure Aware of appropriate times for postoperative care Aware of important symptoms and signs to be observed in the postoperative period Has appropriate interaction with patient and family postoperatively I, ______________________________ (attending physician), have observed the above resident perform the procedure described above, and we have discussed the procedure at length, as well as specific areas of mastery and any areas of concern. ___________________________________ Attending physician signature 120 ___________________________________ Resident signature _____________ Date CLINIC POLICIES AND PROCEDURES The goals of the clinic are to provide our patients with the best medical eye care possible and to provide you with a comprehensive educational experience. The structure of the clinic is designed to achieve these goals. Other factors that influence decisions regarding the structure of the clinic are room availability, staffing needs, operating room availability and requirements for accreditation. ATTENDANCE Attendance is mandatory during your scheduled clinic. Clinic begins at 9:00 a.m., Monday, Wednesday and Friday, and at 8:00 a.m. on Tuesday and Thursday. You are responsible for the preliminary work-up of your patients, and for this reason it is important that you arrive on time. Surgeries must be scheduled to be performed at times other than your scheduled clinic times. Plan your vacation/conference time well in advance so that your schedules can be cleared. Confer with Chief Resident to insure coverage if you are on the Emergency or Consult Rotation. IF YOU ARE ILL: Contact a live voice, if possible, first thing in the morning. Sheri Samp Office: 882-4688, Cell: 660-676-9390 E-mail: plasters@health.missouri.edu Laverne Fisher Office: 882-3179, Home: 474-0562, Cell: 529-0803 E-mail: FisherLK@health.missouri.edu Melissa Hines Office : 884-4366, Cell: 573-424-3923 E-mail: proctormd@health.missouri.edu Jen Tisone Office: 884-9140, Cell: 424-7453 E-mail: DavisLG@health.missouri.edu SCHEDULES Your schedules are structured to allow for new, return, post-op, contact lens and new to doctor patients. The basic schedule for first year residents allows for four patients per half day clinic. At times it may be necessary to schedule additional patients. A copy of your schedule is available for your review before each clinic session. Reviewing your schedule may help you to pace yourself through the day. Note: The number of patients on your schedule will increase as you progress through the program. If you anticipate difficulty with your schedule, please speak with the Laverne Fisher, Supervisor, or Dr. Fraunfelder, Medical Director/Chairman. CLINIC SUPPORT STAFF The clinic clerical staff consists of Laverne Fisher, Supervisor, Outpatient Services and Facilities Coordinator, Melissa Hines, Service Coordinator and Patient Service Representatives. The Outpatient Services Supervisor and Service Coordinator are responsible for programming your master schedule, "bumping" your schedule when you take vacations or attend conferences, and supervising the work of the Clerical Staff. 121 Patient Service Representatives are responsible for greeting your patients and processing the paperwork necessary for the clinic visit. They gather patient demographic and insurance information, and prepare the progress notes and billing forms university guidelines require. Ronnie Greenwell and Melissa Hines are Patient Service Representatives responsible for obtaining medical records. Incoming patient calls are answered here in clinic in the reception clerical area (front desk). All service representatives rotate through this duty. All patient visit appointments made at the end of a visit are scheduled through the Patient Service Representatives. TECHNICAL STAFF The technical staff consists of Ophthalmic Technician Certified, Ophthalmic Imagers, Ophthalmic Technician Non-Certified and Licensed Practical Nurses (LPN). The technical staff will provide as much support to the Residents as time allows. They will provide initial, limited work-up of patients when the resident gets backed up (if staffing levels permit). They will also conduct HVF analyses, prepare the minor surgery room for procedures, clean instruments, review your completed problems and procedure forms (these are your responsibility), and assists you with any patient who is difficult to examine. Many of our technical staff are exceptionally skilled at using the equipment and performing testing, and are readily available to assist in familiarizing and assisting in your training. Please note patient care assistants are often new and in training, and thus benefit greatly from any attention and medical instruction you can provide. The technicians and LPN staff provide technical support to the faculty physicians. They conduct the preliminary work-up on all patients and will perform any ancillary tests requested by the supervising physician. They will be assigned to assist residents when staffing levels permit. Chuck Hamm and Vonda Cross (Ophthalmic Imagers) are responsible for all patient photography including external, slit lamp, fundus and fluorescein angiography studies. The ophthalmic imager also provides endothelial cell counts, processes the fluorescein angiography studies and prepares for presentation material at the weekly photo conference. All patient photo files and records are maintained by the ophthalmic imager’s office. All technical staff is responsible for cleaning and stocking examination rooms each morning. If your room needs to be cleaned or restocked, please see the technical staff. Please remember, this is a resident training program. The Accreditation Council for Graduate Medical Education requires you, during your three years of residency, to personally complete an established number of examinations, refractions, etc. Technical support will be provided to Residents on a limited basis when staffing levels permit. Should you encounter delays of difficulty seeing your patients in a timely manner, please feel free to ask Laverne Fisher, Supervisor, if tech support is available. 122 PAPERWORK It is your responsibility to stay current with dictation, telephone messages, and insurance or disability forms. Please empty your mailbox and respond to messages daily. The clerical staff will take telephone messages and sort your mail and will help retrieve any medical records needing a response. In the evening, the chart completion crew may search the clinic and remove the medical records you need resulting in a lost form or message. Avoid the possibility of alienating a referring physician or patient because of neglect regarding referral letters. When you see patients "after hours" or on the weekend, please use an After Hour Patient Packet located on the wall holder of EC125. It can be identified by its bright blue color. Please record, legibly, the patient's first and last name, date of birth telephone number, and date of service. The clerical staff will contact the patient the next business day for any additional necessary information. All after hour or weekend patients are to be discussed with the attending ophthalmologist on call or the appropriate sub-specialist. DOCUMENTATION Document all patient complaints. Document all examination findings. Document all services rendered. Document all patient instructions. Document all risks and benefits explained. Document all prescriptions given for glasses or medications. Document all plans/dispositions. Document all telephone conversations. BILLING FORMS There are five billing forms used in the clinic. Encounter forms will be attached to each patient's medical record and should be used to record the professional services rendered. RETURN PATIENT FORMS Form 281 is a white form on which the physician can write any follow-up requests with comments for future testing. Form 281 can also be faxed to referring physicians as a means of communication. It is very important that any clinic attending changes be noted on Form 281 and sent to the front desk. THE MORE CLEAR, CONCISE INFORMATION THAT IS WRITTEN ON THIS FORM, THE BETTER ABLE STAFF ARE TO PROPERLY SCHEDULE FOLLOW-UP APPOINTMENTS AND TESTING. 123 PHONE MESSAGES Often, Patient Service Representatives will take a call from a patient that they cannot resolve. They will then generate an email through the Power Chart System. These messages can be found in the physician’s inbox for review and any other action needed. The patient’s hard chart may need to be ordered if the information that you need cannot be found in Power Chart. If the Hard chart is needed you would forward this request to Ronny Greenwell (MEI patients) or Melissa Hines (UEIE patients). GUEST RELATIONS Occasionally, a patient may be unhappy with the service we provide in the clinic. If a patient should express dissatisfaction with our clinic, for any reason, please contact Laverne Fisher, Supervisor, and Outpatient Services. Often patient dissatisfaction was a result of miscommunication which can be easily resolved. If you hear a patient complaining to staff, please contact Laverne. If a patient is creating a disturbance or becomes extremely agitated they may also be escorted to Guest Services across the hall for resolution of their issues. When in need of assistance by Laverne, please call her at 882-3179. PATIENT INJURIES/FALLS Please report all patient injuries or fall to Laverne Fisher for entry and resolution in the Patient Survey Net System. DIFFICULTIES Should you have any difficulties with clinic staff, please privately talk to Laverne Fisher, Clinic Supervisor, who will mediate and review the problem. Occasionally your patients will not be scheduled according to guidelines, should you have any problems please bring this to the attention of Laverne Fisher. TRIAGE All patients who walk in to the clinic must be triaged. Most times the technicians or PSR’s can make a decision to register an emergent walk-in patient when symptoms are obvious. Occasionally, a patient will arrive and wish to be seen for a non-emergent complaint (cataract, presbyopia, etc) and will need to be first triaged at the desk by a resident. We will always try to accommodate patient’s wishes, however, due to clinic congestion, non-emergent patients may at times need to be scheduled to a routine appointment if the screening residents feel this is appropriate. Each emergent patient who walks in our clinic is given a sheet describing our policy and informing them of a possible long wait. The resident on the Emergency Rotation is strongly encouraged to meet with the front office staff at the start of their rotation. This has been a successful way of ensuring everyone’s expectations are met throughout the rotation. 124 INMATES We often care for patients who are incarcerated and brought to our facility under guard. Clinic policy is they be transported in a wheelchair and legs covered with a blanket. They are not allowed to walk from room to room due to their leg shackles. When inmates arrive, the clinic policy is they not be left in a common waiting area. Ideally inmates are immediately moved by staff to room 118 if available. For security purposes, please, never indicate to an inmate patient the time frame of their follow-up appointments or surgeries. These are scheduled from the facility by them calling us secondary to your progress note given to the guard at the end of the visit. Inmates who are being seen at UEIE need to notify front desk by phone that they have arrived. The inmate is then let in through the side door only. Inmates are not to come through front lobby. EMERGENCY PATIENTS Residents seeing patients in the clinic after hours and on weekends should be especially attentive to the whereabouts of the patients and their families as there may be protected patient information in the reception clerical area (front desk) and in the department offices. There is also expensive equipment on the clinic counters and in the examination rooms. SURGICAL BOARDING PROCEDURES All surgical boarding and pre-certification is done by Chantell Monzingo. If the surgery boarding person is very busy or unavailable, their business card can be given to the patient. Chantell will call patients within 2 business days or scheduling. Surgical boarding includes these following locations: Missouri Center for Outpatient Surgery Surgery – Women’s and Children’s Hospital (WCH) Main OR Special Clinic Procedures should be scheduled through the attending's secretary to insure there is no conflict with the attending’s schedule. Each of the above surgery locations have different procedures which must be completed before surgery can take place. If you are uncertain about any procedures, please see Chantell. A. Missouri Center for Outpatient Surgery/Main OR Procedures 1. Complete Surgery Boarding Form/packet (which is in PowerChart). This must be done with all information provided. 2. Include your request for any special equipment needed. 3. Intraocular Lenses that MCOS does not stock must be special ordered. Please indicate the type, model number and dioptric power. A Lens Chart is located on the A-scan to assist you with your lens selection. 4. History, Physical, and Consent forms must be completed before surgery. Our History, Physical and Consent forms are good for 7 days. 5. For WCH the patient/guardian fills out a health questionnaire which is then faxed to pre-op clinic. The nurses then determine the patients’ needs. If we know that they will need a chest x-ray or cardiac clearance the attending physician has to order these. 125 6. HMO-POS patient must have a referral from their primary care physician with states surgery as an option for treatment. Complete the correspondence required by the primary care physician. Cataract surgery patients must complete a cataract surgery Medicare only questionnaire prior to surgery. These are in the surgery boarding packets. 7. Give the completed surgery packet to Chantell Monzingo to schedule the surgery. They will make all other arrangements for the case. If a special time or special instructions are needed, please note this on the Surgical Boarding Form. NOTE: Prisoners surgeries are performed at MCOS and must be scheduled with that facility’s nurse. For security reasons, never indicate to an inmate the dates they may be returning for surgery. B. Minor Surgery Room 1. Ensure attending coverage is available if booking procedure for a special time. This can be done by checking with the attending’s secretary. a. If pre-certification is needed, or you are not sure, contact Melissa Hines. SURGERY LOG The Resident Review Committee for Ophthalmology of the Accreditation Council for Graduate Medical Education requires documentation of the surgical experience of each resident. The surgical log covers the 36 month period of your residency and includes surgical experience at UMC and VA. The log, therefore, is in two sections (UMC and VA), and separated by year within each section. UMC A monthly computer-generated print out will be supplied. This includes all UMC activity – surgical and clinic. It contains all information required by the Accreditation Council except surgery class. Therefore, each month you will be given your log to add the appropriate class following the surgery description (1,2,3, or 4). Procedures will be highlighted prior to insertion to aid in location. VA The VA will print out a report for surgeries performed in the OR. It is the responsibility of the resident to keep a list of all procedures performed in the clinic minor room and lasers. DEFINITION OF CLASSES CLASS 1: This is for procedures that are done primarily by the resident (over 50%) with direct supervision by faculty present in the operating or minor surgery room. CLASS 2: This is for procedures that are done by the resident without faculty present. CLASS 3: This is for procedures that are done primarily by the faculty (over 50%) with the resident as first surgical assistant. Only classes 1 and 3 are counted by the ACGME relative to fulfilling your surgical experience requirements. Few Class 2 should occur. 126 LASERS When any laser is performed on a patient, the information must be filled out in the respective laser book. ULTRASOUND A & B-SCAN When an ultrasound is performed, fill out the Facility Fee Sheet (yellow). Place the thermal tape or printed calculations in the chart. This provides proof of service performed. Be sure to type the patient’s name into the machine, as well as specifying the correct eye so it will print. Also, please initial each scan to signify authenticity. IOL MASTER When an IOL Master is performed, fill out the Facility Fee Sheet (yellow). Be sure to type the patient’s name into the machine, as well as specifying the correct eye so it will print. Place copy in the patient’s chart. EQUIPMENT Should any clinic equipment fail or is missing, please contact Chuck Hamm , or Laverne Fisher immediately. 1. Removal of Equipment from Clinic We recognize that often equipment must be taken to an in-patient floor or to another facility for patient consultation or care. However, all residents should be especially mindful of returning all clinic equipment, including but not limited to Tonopens and indirect or portable slitlamps to the clinic immediately after use. 127 BILLING INFORMATION This section is provided to give you an overview of the billing procedures and forms that we use in our daily activities. CHARTS AND PROGRESS NOTES. Patient records, whether in charts or loose notes should NEVER be removed from the premises. Records must stay at the location where they were created. Please do not hold billing/notes. If you need a chart back to dictate or for some other reason, please put a note on the chart and it will be returned after billing is complete. Coders read and audit each note. If items are missing or incomplete, you will be paged to come to the billing room. If you haven’t come down after 3 pages, then the attending on the service you are rotating with will be notified and asked to send you down. DIAGNOSIS CODING Proper coding of patient services is extremely important. With the recent legislation regarding medical services, it has become increasingly important for us to code all diagnoses to the highest degree of certainty. What this means to you is that if becomes necessary for you to be very specific when you list a patient's condition. DO NOT USE diagnoses such as "probable", "suspect", "questionable", or "rule out". Use instead the principle reason for the encounter, such as symptoms, signs, patient or family history, abnormal test results or other reason for visit, such as headache, blurred vision, family history of glaucoma, etc. The only exception to this rule is "glaucoma suspect". It is acceptable to use this as a diagnosis. Another diagnosis to be avoided is "Refractive Disorder". Please list the patient's eye problem, such as myopia, presbyopia, astigmatism, etc. These codes should never be listed as the primary diagnosis unless there is no other diagnosis listed. Insurance companies do not pay for any type of refractive disorder under medical plans. Some plans are now providing one vision exam per year. Those should be so noted on the progress note so we can bill them appropriately. You will see many diagnoses in which a blanket term may seem appropriate without being more specific. Please remember to always be as specific as possible. One example of such a case is: melanoma of the eye. There are actually nine different types of melanoma of the eye. List which area is affected in those types of cases. As we approach the October 2014 deadline for implementation of ICD-10, specificity in documentation will become even more important. ENCOUNTER FORM The encounter form is used for billing outpatient visits to the clinic.. A sample Encounter Form will be provided to you during orientation. Proper procedure for choosing visit levels will be discussed at the orientation. Please do not quote patients charges. Never promise a reduced fee or free services to a patient. If patients are in financial difficulty, please refer them to Financial Counseling. Their offices are over at the Admissions area and their phone number is 573-884-9900. When you mark the diagnoses on the encounter form, please number them in the order of importance for this visit. Do not list diagnoses which are long resolved or are being managed by another physician (i.e. retina vs. glaucoma vs. cornea). Should you perform any procedures or diagnostic test during the visit, please be sure to mark the appropriate box or write the procedure in the spaces provided. All tests require and order and interpretation to be billable. 128 CONTACT LENSES When you see a patient who is interested in contact lenses, provide them with a Contact Lens brochure to read. Explain that any questions they have regarding Contact Lens prices will be answered by Norman when they meet with him (after you have fit the lenses). Be sure to explain to the patient that they will be charged an initial contact lens fitting fee and a minimum of one follow-up visit. Remember, children less than 18 years-of-age must have parents accompany them for contact lenses. SURGERY FUNDING Should a patient who has no insurance coverage require surgery, they must be screened for eligibility for funding prior to scheduling the surgery. Discounts are available from Hospital and UP for self pay patients. Funding for medically indigent patients usually takes ten day to two weeks. Do not schedule surgery until funding is secured. INSURANCE REQUIREMENTS The University deals with many different types of insurance, each of which has its own guidelines and requirements. The following are some of the more common requirements for the different insurances: MEDICAID Prior authorizations are required for the following procedures: Ocular surface reconstruction (CPT 65780 – 65782) Repair of blepharoptosis (CPT 67901-67908) Entropion repair by blepharoplasty (CPT 67916 & 67917) Ectropion repair by blepharoplasty (CPT 67923 & 67923) Blepharoplasty of upper or lower eyelid (CPT 15820 -15823) Any other procedure that may be considered cosmetic. The surgical boarder will initiate a prior authorization form and must be completed and submitted along with a copy of the visual fields to Medicaid. They will review and return an authorization form. Only then may we proceed with the surgery. MANAGED MEDICAID PLANS Missouri Care, Healthcare USA and Home State Health are all managed medicaid plans. Each of these plans has their own rules and list for pre-certifications and prior authorizations. For example, Missouri Care requires prior authorization on all muscle surgeries. MEDICARE Cataract Surgery - Cataract surgery may be performed without Medicare review as long as the following are documented: 1. Patient's desire to have the procedure due to decreased visual acuity is documented. 2. Ophthalmic examinations (slit lamp, dilated ophthalmoscopy, intraocular pressure) is performed by the operating surgeon within two months of the surgical procedure documenting a cataract and one of the following: 129 a. Etiology of visual loss felt to be the cataract, and best corrected Snellen distance vision of 20/50 or less. Glass testing visual acuity of 20/50 or less is also acceptable. b. Phacogenic glaucoma c. Phacoanaphylactic endophthalmitis d. Cataract and foreign body e. Cataract and ocular trauma f. Cataract extraction and corneal transplant g. Dislocated or subluxated lens causing glaucoma, monocular diplopia, aphakia, severe hyperopia (over +8 diopters), or astigmatism. 3. Documentation as to specific improvement in quality of life to be expected after cataract surgery. 4. Complete cataract surgery questionnaire. Forms are included in the surgery packets. Glasses - Medicare will partially pay for the patient's first frame and each lens following cataract surgery only. The Optical shop will submit a claim to Medicare. The patient will be responsible for their copay, deductible and any extra options which are non-covered. Medicare does not pay for glasses for any other reason. Secondary Cataract (PCO) - Discission of secondary membranous cataract ("after cataract") and/or anterior hyaloid laser surgery (one or more stages). Indications for surgical procedure 1. Decreased vision to 20/40 or less secondary to: a. b. 2. Cataract with pearls and/or fibrosis of posterior capsule. Membranous cataract. A time period of at least ninety days should have elapsed between the time of the initial cataract extraction and the performance of the discission of the secondary membranous cataract. Blepharoplasty/blepharoptosis - Blepharoplasty is a surgical procedure to remove excess upper or lower eyelid skin and fat. Reimbursement can be allowed if the procedure is considered reconstructive to improve impaired vision. This is usually manifested in the upper or peripheral field of vision or on forward gaze by skin resting on the upper eye lashes. Lower lid blepharoplasty is generally not reimbursable since it is usually performed for cosmetic reasons. Payment can be allowed, however if medical necessity for reconstructive reasons is demonstrated. 130 Blepharoptosis is a surgical procedure to repair levator muscle abnormality. Reimbursement can be allowed when it is evident that lid ptosis interferes with vision. Pre and post-operative photographs and/or visual field are required to support medical necessity and must be available upon request by insurance. Symptoms of lid heaviness, excessive tearing and visual impairment sufficient to impede daily living activities should be documented, if possible. Substantial visual loss exists when there is loss of the superior field to 20 degrees or less from the horizontal visual axis. Photography - Medicare has a list of diagnoses for which photos are allowed. If you request photos be taken and the diagnosis is not on the approved list, the patient will be required to sign a waiver indicating they will be responsible for the cost of the photos. Cigna – requires prior authorization on Botox injections. Missouri Care - A prior authorization must be obtained for all procedures performed in the clinic. This includes lasers as well as procedures performed in the minor surgery room. They require prior authorization on muscle surgery. Mercy Health Plan - Mercy requires prior authorization on Botox injections and all lasers performed in the clinic. Healthcare USA – Precertification must be received prior to surgery. Mercy Care Partners – We are NOT contracted providers. Rehabilitation Services for the Blind (RSB) - Rehabilitation Services authorizes all services provided prior to their being performed. If you have a patient in for an exam and feel additional diagnostic testing or a procedure is needed, you must call and obtain authorization prior to performing it. The phone number to call for authorization is: 573-751-2714 Prevention of Blindness Program (POB) - POB is a state agency which provides financial assistance to patients who meet financial and visual eligibility criteria. Once a patient has been approved, office visits and diagnostic tests are automatically covered. Procedures must be prior authorized. The phone number is: 573-751-3428 Humana Gold (HMO) Medicare & Coventry HMO Medicare- While these insurances do not require referrals to be seen in clinic, they do require a referral from the PCP to perform a procedure. 131 NOTE: IT IS THE RESPONSIBILITY OF THE ADMITTING PHYSICIAN AND THE HOSPITAL TO OBTAIN PRECERTIFICATION APPROVAL. IF PRECERTIFICATION IS NOT OBTAINED AND THE PATIENT ENTERS THE HOSPITAL, NO BENEFITS WILL BE PAID FOR HOSPITAL OR PHYSICIAN EXPENSES AND THE PATIENT CANNOT BE HELD FINANCIALLY RESPONSIBLE. 132 GENERAL PROGRAM INFORMATION General organization of the patient care services at the Mason Eye Institute The three-year residency program has a total of nine positions, with three residents in each postgraduate year. Residents in each year have clinic and surgical assignments. All rotations are two or four-month blocks. The Resident Rotation Schedule is by ½ day assignments Monday - Friday. Although the resident is assigned to a particular subspecialty rotation (i.e., pediatric ophthalmology), residents continue to have other primary patient care responsibilities as well. Most rotations include ½ day assignments among the sub-specialty clinic(s), general clinics (also referred to as resident clinics), and surgery. The inclusion of general clinics allows residents the opportunity to provide continuity of patient care throughout the three years. In some cases a patient sees the same resident (under the supervision of the attending physician) for the three-year residency duration. This establishment of a prolonged patient-physician relationship and observance of long-term disease course are considered valuable components of the training experience. Call All residents participate in evening and weekend on-call assignments. The call assignment schedule is developed among the residents. Normally, a second-year resident assigns call for first and second year residents; a senior resident assigns call for third-year residents. Each day the schedule includes three physicians on call (designated as firstcall, second-call, and third-call which is attending call). First call is handled by PGY-II and PGY-III residents. Therefore, first call is shared among 6 residents (the three first year residents and three second year residents). This means that during years one and two, each resident is assigned to first-call 1/6th of the time. PGY-IV residents take backup (or second) call. Therefore, senior residents are on call 1/3rd of the time. Attending call is normally assigned one week at a time (Monday-Sunday). The first-call resident handles the case as appropriate for his/her level of training; the senior resident is called to assist as necessary. The senior resident calls in the attending physician as necessary (or directs the resident on first-call to do so). In those situations where the attending’s services are not required, residents are required to discuss all such evening and weekend cases with either the attending on call or attending most appropriate for that particular case on the next work day. The University of Missouri-Columbia, Department of Ophthalmology does not recognize a separation of private and non-private patient populations. All patients, whenever possible, are evaluated by residents unless the patient specifically requests no resident involvement. Curriculum (didactic instruction in the basic and clinical sciences) The didactic sessions for the residents consist of Monday and Wednesday Conferences (days/times may vary and are subject to change) -- held between 7:30 and 9:00 am which are conducted by the clinical faculty. These are usually formal presentations. Topics as outlined by the American Academy of Ophthalmology Basic Science Course are used as a guide. Recent publications in peer reviewed journals are an important resource to help provide the most up-todate information. 133 Grand Rounds are held the first Friday at UMC and the third Friday at VA of each month from 7:30 to 9:00 am. Attending physicians, fellows, residents, and medical students, will examine selected patients whose clinical presentation pose interesting, heuristic, medical or surgical problems. This is followed by extended discussion. Photo Conference/M&M Conference is held on the fourth Friday of the month from 7:30 to 9:00 am. This conference includes the presentation and discussion of selected University of Missouri Eye Clinic and/or VA Eye Clinic patients (through 35mm slide/digital presentations). This conference covers a comprehensive array of ophthalmological disorders. Specific cases are discussed regarding findings and management. Fluorescein Conference is held on Thursdays from 7:00 to 8:00am at the VA eye clinic and is conducted by Dr. Hainsworth. Pathology Webinar Course: Webinar interactive sessions conducted on the second Friday of the month with Dr. Deepak Edward offers 36 hours in microscopic examination of pathological specimens. Deepak P. Edward, MD, FACS, is Professor of Ophthalmology and Director of Research at John Hopkins/Baltimore at King Khaled Eye Specialist Hospital in Riyadh, Saudi Arabia. Dr. Edward’s credentials: • Fellowship in Glaucoma, Washington University, St. Louis 1995-1996 • Residency in Ophthalmology, University of Illinois College of Medicine 1992-1995 • Internship in Pediatrics, University of Illinois Hospital, Chicago 1992 • Fellow in Ophthalmic Pathology, University of Illinois College of Medicine 1987-1989 • Master of Surgery (Ophthalmology) Post Graduate Institute of Medical Education and Research, Chandigarh, India 1984 • Bachelor of Medicine; Bachelor of Surgery, St. John’s Medical College, Bangalore, India 1980 Ocular Pathology Grossing and Specimen Review: Douglas Miller, MD, PhD, Professor of Pathology will conduct Ocular Pathology Grossing and Specimen Review Conferences 4 times annually. Journal Club meets monthly (ten per year) on Tuesday evenings from 5:15 to 8:30 pm. Residents are assigned articles for review and an active or courtesy faculty member moderates discussion of these articles. Invited Visiting Professor Conferences are held approximately two – three times per year on Saturdays -- usually 8:00 am to 12:00 Noon. These CME conferences usually include two hours of didactic lecture and one hour of case presentation and discussion by a visiting professor. Community ophthalmologists, optometrists, faculty, residents, fellows and medical students are present. 134 OKAP Study Lectures conducted by Dr. Geetha Davis, Clinical Instructor will be three – four sessions prior to the OKAP exam in April. The study lecture content is taken from the American Academy of Ophthalmology Basic & Clinic Science Course books. Resident and Alumni Day is held the weekend third weekend in May which is the weekend before the Memorial Day weekend. The usual schedule includes Friday afternoon and Saturday morning scientific conference. Each resident is required to present at this conference on a fifteen minute topic of their choice, generally pertaining to their research project for the year. Faculty and guest alumni speaker presentations are also given during these scientific sessions. The Resident and Alumni Day weekend ends with a banquet Saturday evening. Residents are required to attend all scientific sessions and the graduation/awards banquet. Research At the end of each year, our residents are required to present a research project during the Annual Resident & Alumni Day (“RADay”) Conference. The residents are encouraged to begin working with a faculty member on the research project by October/November of each year. The residents undertake a literature review using information technology provided by the Ophthalmology department and the University of Missouri’s Health Science Library (e.g., PubMed, Ovid, ONE Network). They conduct their research projects, analyze the data with members of the Biostatistics Department, and again review the scientific studies to support and improve their research findings and conclusions. The residents are encouraged to present their research findings at national meetings (e.g., Association of Research and Vision in Ophthalmology [ARVO], American Academy of Ophthalmology [AAO], etc.) and also to publish their research findings. As an incentive, the residents are provided up to 1 week of additional meeting time when presenting at a national meeting. Residents are reimbursed for travel expenses related to their presentations. However, residents are required to write a 1st draft of the manuscript and provide the faculty mentor a copy before an abstract is submitted for national presentation. The residents are informed that if the 1st draft of the manuscript is not completed before departing to the meeting, then travel expenses for this meeting will not be reimbursed, and vacation and/or meeting time may be deducted. 135 Conference Attendance Documentation An Attendance Roster is prepared for each conference. The typed roster has the name of each resident and attending with a section for their signature. The roster sheets are kept in a hanging file folder just to the side of the conference room TV monitor. The Chief Resident is responsible for ensuring these sheets are signed and given to the residency program coordinator (Sheri Samp). Resident Participation in Medical Student Teaching The residents participate in second year medical student education of ophthalmic physical diagnosis of the eye. We have third and fourth year medical students, both from the University of Missouri-Columbia and from other universities who choose to come to the University of Missouri-Columbia for their ophthalmology electives. The students are assigned to a resident and/or faculty member to observe in clinic and surgery. Annual Contract Each resident signs an annual contract for the July-June period. The contract specifically addresses the following: Medical licensure Responsibilities Performance appraisals and reappointment criteria Non-regular academic appointment Passing Step 3 of USMLE prior to starting final year of residency Comply by the Rules and Regulations of the University of Missouri, Medical Staff Bylaws and the Rules and Regulations of the Hospital and Clinics. Immunization documentation Drug screening Bylaws and Rules and Regulations of the House Staff Organization, including the procedures for discipline and redress of grievances Complying with departmental policies. Missouri Patient Care Review Foundations (Missouri’s PRO) Department policy regarding moonlighting Annual stipend and associated benefit programs University’s Medical, Professional and Patient General Liability Plan Annual vacation and meeting time Americans with Disabilities Act (ADA) Appointment jurisdiction 136 Absences 1. Submit requests to Sheri Samp (Linda Davis in Sheri’s absence) at least 30 days prior to your requested absence, however 60 days or more is preferred if clinic(s) will need to be closed (blue half sheet). The request will be returned to the resident noting approval or disapproval status. Days away from the office should be planned as far ahead as possible. It is never “too soon” to submit a request for time away. All requests for a change in your 8:00 a.m.-5:00 p.m. schedule must go through Sheri Samp or Linda Davis. Clinic staff, per direction by the Residency Program Director, does not have the authority to approve changes. 2. A “Cancellation Request” must be submitted no less than 30 days prior to the cancelled date(s). This will be returned to the resident noting approval or disapproval status. 3. It is preferable no more than 3 residents be allowed leave at any one time. 2 Residents at Mason Eye Institute 1 Resident at VA Hospital We may make exceptions during Holidays and other periods on a case by case basis. The assigned Emergency Clinic Resident and Consult Resident are not allowed to be absent at the same time. Residents are allowed to take time away during the VA rotation, but because of the greater amount of surgery available at the VA, this probably will be considered undesirable for most residents. VA residents must coordinate their time away with their VA colleague. 4. No leave one (1) week prior to the annual OKAP Exam. The annual OKAP Exam is taken on a Saturday (usually around the 3rd weekend in April). An attending or fellow will cover call during the exam, but residents resume call immediately following the exam. 5. All residents are to use vacation time between the last two weeks of July and the first two weeks of June each year. No vacations will be approved for the last two weeks of June or the first 2 weeks of July unless absolutely necessary, and approved by the program director. Vacation 1. Residents are entitled to three (3) weeks of vacation during each year of the program (15 weekdays). Vacation days are not interchangeable with meeting days. 2. No more than 2 weeks absence during a 4-month rotation and 1 week absence during a 2month rotation. 3. In the best interest of resident education taking two 5-day blocks and 5 days at optional times is encouraged. Each of the 2 vacation periods normally begin on Friday at 5:00 p.m. and ends at 8:00 a.m. on the 2nd Monday. The timing of the other five business days (M-F) is flexible. Time does not accrue and therefore must be used each year. 137 Meetings 1. There is one week of education/meeting time (5 weekdays). 2. Some residents elect to spend their meeting time attending a basic science course in their second year. 3. Residents who are first-authors and are invited presenters at a meeting are awarded additional meeting time – the meeting day(s) and, if applicable, travel days to/from the meeting. (See presentation grant for first authors page). Sick Leave 1. House officers accrue sick leave at the rate of eight (8) hours (one working day) per month which may be used for personal sick leave and/or family leave. This may be in conjunction with the Family and Medical Leave Act (FMLA). Time does not accrue from one contract year to the next. Additional sick leave may be granted at the discretion of the Program Director and Department Chairman, however an extension of your residency may be required to meet educational objectives. 2. Sick leave should be reported promptly to the Resident Program Coordinator (Sheri Samp) and Clinic Supervisor (Laverne Fisher). Some sick leave may be anticipated (such as scheduled surgery). In such cases, at least 31 days advance notice is preferred. The resident will submit the “Residency/Fellow Report of Sick Leave Absence” [pink] form prior to the absence in this case. In the case of an unanticipated absence, the resident will submit this form on the first day following the leave. Maternity Leave Maternity leave is provided to residents to the extent that such a leave is reasonably necessary. Available time includes accrued sick leave and vacation leave. Although this should provide sufficient leave in most cases, the provision exists for special situations where further time shall be provided without pay and the resident will be permitted to return to the program for the completion of training. This may require that the resident extend training by the amount of nonsalaried time off to satisfy the requirements of the American Board of Ophthalmology for Board Eligibility (36 months of formal residency training, which includes reasonable absences for vacation leave, etc.) Paternity Leave Paternity leave is provided to residents to the extent of available accrued sick leave and vacation time; additional time shall be permitted without pay in accordance with the terms of Maternity Leave policy described above. 138 Holidays 1. There are eight University holidays and these are the only days observed as holidays for the purposes of this residency program: New Year’s Day Martin Luther King Day Memorial Day Independence Day Labor Day Thanksgiving Day Day after Thanksgiving Christmas Day 2. There will be no scheduled clinic on these days, but residents will take call as usual. 3. When a holiday falls on Saturday, the preceding Friday is observed as the holiday. When a holiday falls on Sunday, the following Monday is observed as a holiday. 4. The VA observes three holidays the University does not: Presidents’ Day, Columbus Day and Veterans Day. Residents on the VA rotation for these days are reassigned to UMC. Residents are required to be available to help out if necessary and they must notify the clinic director and/or clinic supervisor of their whereabouts and always be available by pager. Residents must also attend all scheduled conferences, etc. If a resident prefers to take a vacation day for any of the above three holidays, this is certainly acceptable with submission of the appropriate form and approval. 5. The Friday following Thanksgiving is not a VA holiday; however, we annually request cancellation of the VA clinic on this date so all residents may observe the University Holiday. Absence Due to Death in the Immediate Family If a death occurs in your immediate family, you will be granted a maximum leave of three working days. Such leave may be taken at any time during the period beginning on the date of death and ending on the second calendar day after the funeral. No salary deduction or accrued vacation time will be taken for these days of leave. If schedule allows, additional days may be approved and will be charged to vacation or taken as excused leave without pay. “Immediate Family” as defined by the University guidelines is husband, wife, parent (including step-parent) grandparent, great-grandparent, grandchild, son, daughter, brother or sister, mother-in-law, fatherin-law and foster children who have become members of the family. Cancellation of Sub-Specialty Clinics When faculty clinics are canceled due to the absence of the faculty member, the resident is reassigned to their research project or OKAP studies, assist with emergency clinic, or cover emergency clinic in the absence of the emergency clinic resident, or help in another attending’s clinic. In all instances the resident is required to be available to help out as necessary, and must notify Sheri Samp, Coordinator, Resident Program, and the Chief Resident of their whereabouts and always be available by pager. In their absence, notify Laverne Fisher, Clinic Supervisor. 139 Unscheduled Time Occasionally, clinics will be canceled and/or a surgery will be canceled and residents will have unscheduled time. Residents are required to be available to help out if necessary and they must notify Sheri Samp, Coordinator, Resident Program, and the Chief Resident of their whereabouts and always be available by pager. In their absence, notify Laverne Fisher, Clinic Supervisor. For example: Residents should not leave for lunch until they have checked with the Emergency Service to help see the emergency patients as needed. Likewise, no resident should leave for the day until they have checked with the Emergency Service to help see the emergency patients as needed. This team work will provide better patient flow and management of our patients. Our motto is, “Perfect Patient Care.” Unanticipated Absences (sickness, death in family, etc.) Confusion often exists regarding what to do in emergency situations when the need for an unexpected leave occurs. Please do both of the following. Where you call may depend on whether it is a weekday or weekend. During the weekends, please call us at home. 1. Call: Sheri Samp Work: 882-4688 Cell: 660-676-9390 2. Call: Laverne Fisher Home: 474-0562 Work: 882-3179 Pager: 441-4311 If you get a voice mail at work, exercise the option that transfers you to the attendant. It is important that you reach someone and not just voice mail. If you get voice mail at our home(s), leave a message, but still attempt to call until you speak directly with at least one of us. If you cannot reach Sheri or Laverne, please try Linda Davis at home (268-6718) or work (882-1020). The sooner you let us know an emergency has occurred, the sooner we can begin doing what is necessary regarding clinic cancellations, etc. Residents should also contact the attending of their rotation. 140 MOONLIGHTING POLICY The Department of Ophthalmology, University of Missouri-Columbia, moonlighting policy is defined as specified in the ACGME Ophthalmology Program Requirements: Section VI-D (copied below), and in compliance with the sponsoring institution’s written policies and procedures regarding moonlighting (see Institutional Policies). 1. Because residency education is a full-time endeavor, the program director must ensure that moonlighting does not interfere with the ability of the resident to achieve the goals and objectives of the educational program. 2. The program director must comply with the sponsoring institution’s written policies and procedures regarding moonlighting, in compliance with the ACGME Institutional Requirements. 3. Any hours a resident works for compensation at the sponsoring institution or any of the sponsor’s primary clinical sites must be considered part of the 80-hour weekly limit on duty hours. This refers to the practice of internal moonlighting. 141 RESIDENT CALL & CALL SCHEDULE POLICY Resident Call Responsibilities 1. Residents should keep a telephone log of all calls while on evening or weekend call. 2. The resident on first call (first or second year resident) will contact the resident on second call (senior resident) to discuss all cases for disposition. If further input or consultation is necessary, the third year resident will contact the attending on call for disposition. 3. All recent post-operative cases will be discussed with the attending physician on call. 4. All cases requiring admission to the hospital or surgery will be discussed with the attending physician on call prior to admission. 5. All patients who were seen or who called during the night will be discussed with the attending on call or the appropriate faculty member the next morning. 6. Responsibility for the patient’s care rests with the attending faculty on call or the attending notified of the patient’s condition. 7. Exceptions to this policy must be specifically made by the attending physician on call or the department chairman. Call Schedule 1. All residents remain on the call schedule July 1- June 30 of each year, unless the resident has received approved leave. 2. Generally speaking, First or Second year residents takes first call. Senior Resident takes second call. Both residents on call (first and second call) must remain available by beeper. Call is athome call; residents are not required to remain within the hospital but must remain immediately accessible by beeper. 3. The call schedule is worked out among the residents themselves. 4. First and second year residents’ and the third year residents’ work out call among themselves. The schedule must be submitted to (Edna Green) by the 20th of each month. If not received by the 20th of the month, Edna will remind the responsible physician and the Chief Resident. If not received by then, Edna will complete the first and second year call schedule for the month and no changes will be accepted after the call being published. 5. The call schedule is required by various departments within the University and VA Hospitals. Delays and changes waste time, are costly, and cause frustrations for many individuals. Concerns regarding frequent delinquencies in residents submitting the call schedule on a timely basis will be brought to the attention of the Program Director. 142 6. Edna Green will type and distribute the call schedule once each month. Subsequent changes will be handled by Edna. Please anticipate changes before the new schedule has been distributed. If there are changes to the schedule do not call the hospital operator, give them to Edna Green. UMC (Call list sent via e-mail) Telecommunications- Hospital UMCHC Dan Crouch, Assistant Manager Zammone Lasker, Office Supervisor UMC Emergency Room Staci Walters, Assistant Manager UMC Registration Brenna Begemann UMC Nurses Mary Christine Engel Kathy A. Greenslate UMC Surgery Services Jeanne M. Campoli Jean R. Locke Amy Tinsley Dorothy M. Williams UMC Revenue Sandra L. Reynolds VA Hospital Jayna Hofstetter – SC/SURG (Jayna.Hofstetter@va.gov) Mary Ann Chandler (MaryAnn.Chandler2@va.gov ) Deana Griffin – VA Switchboard (deana.griffin@va.gov) Sarah Olson (sarah.olson2@va.gov ) Darlayna Scott (darlayna.scott@va.gov) 143 EDUCATIONAL ALLOWANCES & BENEFITS Days Away Meeting Days Away - One week Presentation Bonus Day(s): (See “Presentation Grant for First Authors” below.) Cash Professional Allowance – FY 15/16 (reviewed annually) A professional allowance is provided for the current fiscal year (7/1/15 – 6/30/16). The purpose of this allowance is to assist with continuing education costs, such as meetings/travel, books, journals, indirect lenses, etc. The department purchases indirect lenses for use in the clinic and in surgery. The department must place all orders on your behalf in keeping with university guidelines. NOTE: Residents must purchase their own indirect lenses for use in the clinic and in surgery. Upon arrival, see the clinic medical director (Dr. Reyes) for input on ordering (approximate cost $300 - $500). You must obtain these by November 1 of your first year. Research Please see attached Research form. This is the first step in requesting research time and funds. The Department of Ophthalmology pays all expenses associated with research projects–poster preparations, slides, literature searches, animals, etc., up to $1,000.00 per resident/per year. Costs must be pre-approved in conjunction with the attending that mentors the project. Guidelines to be met before a resident presents at a national meeting: Research Projects: Residents will have to present their research projects at Resident and Alumni Day. It generally takes at least 5 months to produce a good project. Therefore, the residents are encouraged to begin working on their projects by November-December of the academic year. Presentation of Research Projects at National Meetings: Residents are encouraged to present their projects at national meetings (e.g., ARVO, AAO, etc.). Residents are encouraged, to see the coordinator of Ophthalmology Resident Research, Dr. Rajiv R. Mohan, PhD. for guidance on a project accessing research institutional resources (animal labs, IRB approval, etc.). All clinical and basic science faculty are willing to serve as mentors with residents on their research endeavors. Presentation Grants for First Authors A presentation travel/meeting grant of up to $1,000 (actual expenses up to allowance) is available for first authors attending a meeting (approved by the Residency Program Director) at which they have been invited to present a paper or poster. Additional meeting time is also awarded – the meeting day(s) and, if applicable, travel days to/from the meeting. Books The department provides the following: *Thirteen Volume Set of Basic and Clinical Science Course Books for each new resident – $1025 144 Annual Residents and Alumni Day Research Award These awards are sponsored by John Aure Buesseler and Cathryn Anne Hansen Buesseler Foundation, Inc., in memory of John Aure Buesseler, M.D.,the founding Chief/Chairman of Ophthalmology(19591966). *Outstanding Resident Presentation Award (Annual Research Project) – $500 *First Runner Up Award (Annual Research Project) - $200 Ophthalmology Library The Department of Ophthalmology maintains an up-to-date library and electronic journals for the benefit of residents, medical students, and faculty. Suggestions for additions to the library should be discussed with a faculty member for their recommendation for purchase. It is advisable to make use of the valuable internal resource, as well as the J. Otto Lottes Health Science Library in the School of Medicine. Computer, Internet and Worldwide Web The Department of Ophthalmology provides four computers in the residents’ rooms which contain a variety of software. In addition, laptops are available for clinic patient care. Our web address is: http://medicine.missouri.edu/ophthalmology Office Assistance The Department of Ophthalmology provides secretarial assistance to the residents as follows: 1. 2. 3. 4. 5. 145 Transcription of patient dictation. Publications - - these should be submitted to the secretary of the attending physician included in the publication, in final form, preferably typed. Assistance in slide preparation for Residents and Alumni Day and external meetings such as ARVO, MoSEPS, etc. Crystal Peterson compiles the travel expense vouchers and vouchers for reimbursement. Please be sure to keep all receipts and other documentation of your expenses. Mandatory: All purchases from your professional allowance must be made on your behalf by the department office, in keeping with university guidelines. CONFERENCES, EXAMS, AND RELATED POLICIES Conference Attendance Policy The following policy was established by the Clinical Faculty at their regular meeting on June 11, 1996. Effective Date: 7/1/96: Residents are expected to attend all conferences. Un-excused absences greater than 25% in one month will result in the loss of OR privileges for one week. The Program Director will designate the week(s) OR privileges will be withdrawn. Attendance Roster Conference attendance must be attested to by the Program Director or Chairman at the conclusion of the training program. Attendance rosters are available in the conference room to indicate your presence or absence from meetings. The chief resident forwards the attendance roster to the Resident Program Coordinator (Sheri Samp) immediately following the conference for permanent record keeping. Attendance at all conferences, etc., must be PROMPT; chronic tardiness may be considered an absence. Second and third year residents may follow the attending to surgery, but are responsible for securing and studying the education material given at conference. A resident present in conference can only be called away from any teaching activity for the delivery of patient care in the case of an emergency which cannot await the conclusion of that activity. Excused absences will be noted through submission of the Absence Request form or Report of Absence form, which are submitted to the Resident Program Coordinator (Sheri Samp). Intra-department Meetings 1. Journal Club Excluding May or June (depending on Raday date) and December, the Journal Club meets on the third Tuesday of each month at 6:00 pm. A moderator is selected who assigns journal articles to the residents to review. 2. Photo Conference and M&M conferences Photo Conference and M&M conferences are held the fourth and fifth Friday. 3. Subspecialty Lectures Held every Monday and Wednesday (dates and times are subject to change) from 7:30 9:00 am. Each faculty member is designated to give a series of lectures on the topic of their choice. 4. Pathology Conference Dr. Deepak Edward’s pathology webinar is held the second Friday of each month 8:009:00 a.m. 146 5. Grand Rounds UM Grand Rounds is held the first Friday of each month. 6. Residents’ Meeting Held each month usually 8:00- 9:00am on Monday or Friday. The Program Director and Resident Program Coordinator also participate. If needed the Chairman, Clinic Supervisor will participate as well. 7. Visiting Lectureships A guest lecturer is invited for a half-day Saturday conference and sometimes part of the prior Friday afternoon, approximately once each quarter. 8. Residents and Alumni Weekend Held one of the last weekends (Friday afternoon and Saturday morning and evening) of May or June each year. Each resident is required to present a fifteen-minute presentation of their research project at the scientific session, held during the day. A dinner/dance honoring our senior residents is held on Saturday evening. The Outstanding Resident Presentation Award of $300 and 1st Runner Up award of $200 is presented that evening. 9. Fluorescein Conference Held on Thursdays from 7:00 to 8:00am at the VA eye clinic. Resident Orientation UMC resident orientation 1 – 2 weeks is conducted for new residents beginning the first business day in July. Residents also attend a VA orientation in July of their first year. OKAP Examination The Ophthalmic Knowledge Assessment Program (OKAP) was established in the late 1960s for the purpose of providing individual residents and training programs with a mechanism to measure academic performance, specific subject areas of success and any area needing improvement. This examination is taken by all ophthalmology residents each year. A median OKAP score of 70%ile or higher for the residents as a group is the goal established by the class year 2010. The results will be used by the Program Director as one of the many criteria in performing periodic resident evaluations. The results are used by the department in identifying programmatic strengths and weaknesses. The OKAP examination reports individual subject scores, overall scores and “core knowledge” scores as a percentile for all residents at the same level of training across the country. 147 CHIEF RESIDENT NOTE: Each 3rd year resident will serve as Chief Resident at Mason Eye Institute for an assigned period (usually 4 months). This resident will be expected to complete the following responsibilities: 1. Read “The Chief Resident As Manager” by Neal Whitman, Ed.D. and Elaine Weiss, Ed.D. 2. Organize and Conduct Grand Rounds - MEI: Coordinate with the attending ophthalmologist assigned for that day, prior to Grand Rounds, the particular patients to be discussed. Obtain three (3) patients with teaching potential. Assign a presenting resident for each patient’s evaluation and presentation. Note: If possible, use the resident who originally worked up the patient. It is the presenting resident’s responsibility to have the history and physical posted at the patients examining room. The presenting resident will review the patient’s record and discuss the patient with the attending assigned to Grand Rounds for that day. He/she will have available appropriate photographs, X-rays, fluorescein slides, and pathology slides. The presenting resident will review the literature pertinent to the particular disease process and then lead the discussion at Grand Rounds. Presentations will be with PowerPoint slides that will maximize learning. The presenting resident will question all the resident staff regarding pertinent history and physicals findings, a differential diagnosis, and an appropriate disposition of the patient regarding further diagnostic studies and treatment. Discussion: Maximum of 20 minutes per patient. It is the chief resident’s responsibility to ensure the presenting resident is prepared and available. If the presenting resident is unprepared or unavailable, it is the chief resident’s responsibility to conduct the discussion as indicated above. 3. Coordination and Supervision of Photo Conference: It is the Chief Residents responsibility to discuss each photo conference’s agenda with the assigned attending ophthalmologist. The attending ophthalmologist will direct each photo conference as he/she desires. However, it is the Chief Residents responsibility to ensure the correct photographs and patient charts are available. The photographer will pull the photos and obtain the patient charts as directed by the attending ophthalmologist and/or chief resident. 4. Review Resident’s daily schedules: If you feel the scheduling is inappropriate or not ensuring expeditious patient care, discuss with Laverne Fisher, Supervisor, Outpatient Services, or Sheri Samp. 5. Care of Emergency (Walk-in) Patients: You are responsible for ensuring these patients are seen appropriately and expeditiously. If the Emergency Resident is over 1 hour behind arrange for patients to be seen by another resident and/or coordinate with Sheri Samp. If the Emergency Resident is on 148 vacation or unavailable, it is your responsibility to organize the residents’ schedule (with the Clinic Supervisor) to ensure all Emergency patients are being seen expeditiously. 6. Coordinate Consult Service (when Consult resident is unavailable): A problem occurs primarily during the period when first year residents are attending the Basic Science Course or are on vacation. Coordinate with the Consult Attending regarding appropriate resident coverage of the Consult Service. 7. Resident Call Schedule: Ensure timely completion of the call schedule and submit to Edna Green by the 15th of the month. Any changes in the call schedule of resident’s times must be submitted to Edna in writing. 8. Responsible for: Resident’s Patient Charts, General Dictation and Letters to Primary Care Physicians Each week check to ensure all resident’s patient charts, general dictation regarding patient care, and letters to the Primary Care Physician are completed and submitted to the attending ophthalmologist in a timely manner. 9. Participate in Resident Selection Process: The Chief Resident, who is the designated member on the Residency Education Committee, will participate in the interview and selection procedure of potential resident applicants. 10. Monitor Clinic patient flow: The Chief Resident is responsible for ensuring all patients in all services of the Ophthalmology Clinic are seen in an expeditious manner. If he/she feels this is not occurring, discuss the problem with the attending ophthalmologist or Sheri Samp. 11. Co-supervision of the daily clinic operations: Co-supervise with Laverne Fisher, Supervisor, Outpatient Services the daily clinic operations involving all technical, photographic, and clerical staff. Ensure each technician is being utilized to their maximal potential. Each subspecialty clinic will have a lead technician and other technicians as determined by Laverne Fisher, Supervisor, Outpatient Services. However, if the Chief Resident feels a technician can be best utilized temporarily in another capacity for the most expeditious operation of the Ophthalmology clinic, the chief resident has the authority to direct a particular technician’s duties as he/she feels necessary. 12. Discuss problems regarding Resident Surgical Schedules: If a problem arises with the resident’s surgical schedules, resulting in conflicts of time, discuss with the appropriate attending ophthalmologists and then make changes as necessary. 149 13. Monthly Resident/Fellow Practice Management Meeting with the Resident Program Director, Resident Program Coordinator and Residents/Fellow. Attend a monthly meeting with the Resident Program Coordinator regarding the overall operations of the Ophthalmology Clinic. Be prepared (after prior discussion with fellow residents) to discuss any problems relating to clinic operation. 150 PROFESSIONAL RESPONSIBILITIES 1. Residents in Ophthalmology are fully trained physicians who have chosen to pursue advanced education beyond the minimum requirements for the practice of medicine. As such, they are expected to deport themselves at all times as colleagues of all other health professionals and relate to them in an appropriate fashion. Courtesy and respect are essential components of such relationships. In like manner, the faculty and staff are expected to relate to the residents in an appropriate professional manner. 2. A clean lab coat and your University of Missouri Health Care identification badge are to be worn when engaged in any clinic or patient care activities. 3. Residents must dress themselves in a manner which is appropriate to the profession of physicians at times when patient contact is anticipated. Appropriate dress for male residents is shirt and tie for weekday clinics or for weekend rounds. Appropriate attire for female residents is dress slacks with professional looking sweater or blouse, or professional looking dress. This attire is also required for visiting professor conferences. Blue jeans, shorts, tee-shirts, and athletic shoes are not appropriate attire for patient care or conferences. 4. For emergency visits, residents may wear scrub suits as appropriate attire if acceptable to the attending physician with whom you are working. 5. Attending physicians may set additional standards for their rotations. These standards should be adhered to by the resident on that service. 151