BCCA clinical governance guidelines for congenital heart disease
advertisement

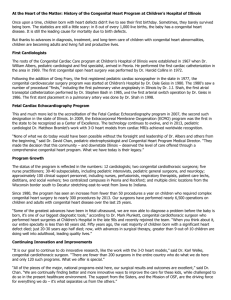
QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. BCCA clinical governance guidelines for congenital heart disease outpatient consultation duration April 2007 Background The Bristol Inquiry Report emphasised that National standards of clinical care should be patient centred. The Paediatric and Congenital Cardiac Services Review (PCCSR)1, published by the Department of Health in response to the Bristol Inquiry was endorsed almost in its entirety by Ministers. The PCCSR set numerous specific standards of care for patients with congenital heart disease, including endorsement of the British Cardiac Society (BCS) workforce committee’s recommendation at that time for a minimum of 2 consultant paediatric cardiologists per million population to provide an adequate level of care.2 In 2005 the BCS revised this recommendation to 3 per million, based upon the increased demand for specialist consultation and the EU working time directive.3 These recommendations have not been implemented; there are currently 76 NHS consultant paediatric cardiologists in the UK (population approximately 62million) - a huge shortfall from the recommendations of the PCCSR and the BCS. The British Cardiac Society’s recommendations for adult congenital cardiologists in 2005, based upon workload data,3 was 1.3 to 1.5 full time consultants per million population, increasing to double this figure by 2014. These recommendations have also been ignored; there are currently 14 UK full time consultants (with some part time support from paediatric cardiologists). This shortage of manpower is most strongly reflected in the quality of provision of outpatient care. Neither the PCCSR nor the Department of Health Commissioning Guide for Adult Congenital Cardiac Services4 made specific recommendations on standards for duration of outpatient consultations. The BCCA feel that this is a fundamentally important aspect of quality of care. Current outpatient practice Outpatient consultations for children and adults with congenital heart disease are highly variable, ranging from straightforward and very focussed (for instance an innocent murmur or mild valvar stenosis) to extremely complex multidisciplinary episodes (for instance an adolescent or young adult with complex heart disease and extensive past history who requires advice on lifestyle, prognosis, treatment, pregnancy and contraception as well as the heart disease itself). Whilst duration of outpatient consultation does not necessarily equate to quality, adequate time is clearly a prerequisite for safety. It is apparent that allocation of time for a consultation varies widely across the UK. The majority of new and follow up consultations involve the consultant reading relevant correspondence, taking a history from the patient or parents, getting the patient undressed, carrying out a clinical examination, in children carrying out an echocardiogram there and then, getting the patient dressed, sometimes also interpreting an ECG and/or chest Xray, counselling the patient and/or family, dictating a letter and often writing an echocardiogram report with diagnostic coding. It is apparent that in some centres the time allocated at present for all this to be done is 7.5 minutes. The BCCA view this as potentially unsafe. Cardiologists have traditionally found it difficult to refuse to see patients (particularly children) because of lack of time. Whilst such an attitude is commendable, it has led to very large clinics with very short consultation times, has proved counterproductive in terms of improving patient care and has removed incentive for funding of badly needed new consultant posts. The British Cardiac Society’s 5th Report on Cardiovascular Services recommended in 2005 that an average consultation for a child or an adult with congenital heart disease required between 20 and 30 minutes.2 Hard data on time requirement for a “safe” consultation is not available, so the following recommendations are based upon a consensus view from the Council of the BCCA, the Children’s Heart Federation (CHF) and the Grown up Congenital Heart Patients Association (GUCH). Overall duration of outpatient clinics (and therefore the overall number of patients seen) will inevitably vary and will depend upon many factors including availability of local resources, funding, and consultant travelling time for outreach clinics; what is most important to optimise quality is the time allocated to each consultation. In addition to the recommendations set out below, all patients and/or their parents should have access to a specialist cardiac liaison nurse as recommended by the PCCSR. Recommendations for children Accepting that some straightforward cases will prove less demanding on time and some complex cases will be more demanding, we recommend that an average of 20 minutes should be allocated to each new patient and an average of 15 minutes for each follow up consultation. Adolescents in transition from paediatric to adult congenital services for follow up require will require multidisciplinary input and should be allocated a minimum of 20 minutes. Recommendations for adults Most new patients referred to adult congenital cardiology have many years’ records from paediatric cardiology which can be very time consuming to digest, even when the referral has been accompanied by a summary of past history. It is particularly time consuming to ensure that a young adult has an appropriate understanding of what is wrong and what treatment has been carried out during childhood as a prerequisite to making treatment plans and patient counselling. Generally, counselling and investigations such as echocardiography take more time than a similar consultation for a child. We recommend that an average of 40 minutes should be allocated for each new patient and 20 minutes for each follow up consultation, excluding time for echocardiography. Trainees in outpatients Trainees are usually present in specialist clinics held within a tertiary cardiac centre. It is the view of the BCCA, the CHF and the GUCH association that trainees attend clinics to be supervised and trained, not to provide a “subconsultant” consultation. This will be of particular importance with the introduction of shorter training programmes in August 2007. We recommend that trainees should be regarded as supernumerary in outpatients, that clinic sizes should not be increased by allocation of patients to trainees, and that consultations in a trainee’s presence should be recognised as being more rather than less demanding on time. New training programmes introduced under Modernising Medical Careers (MMC) and the Postgraduate Medical Education and Training Board (PMETB) dictate that trainees’ competence should be assessed in a wide variety of skill areas, including outpatient consultations. These assessments (mini clinical evaluation exercises, or MiniCex) require direct observation of trainee performance by a consultant, with feedback to the trainee on various aspects of their performance as well as written documentation of the assessment. Competence assessment is clearly beneficial to trainees and patients and should be appropriately provided for in outpatient clinic planning. When a consultation includes a MiniCex we recommend that 15 minutes should be added to the consultation times suggested above. References 1. Paediatric and Congenital Cardiac Services Review. November 2002. www.dh.gov.uk/Consultations 2. Fifth report on the provision of services for patients with heart disease. Heart 2002;88(Suppl III):1–59. 3. Cardiac workforce requirements in the UK. British Cardiac Society, June 2005. www.bcs.com/documents/guidelines 4. Adult Congenital Heart Disease. A commissioning guide for services for young people and grown ups with congenital heart disease (GUCH). www.dh.gov.uk/en/Policyandguidance bcca@bcs.com April 2007