Supplementary information (doc 150K)
advertisement

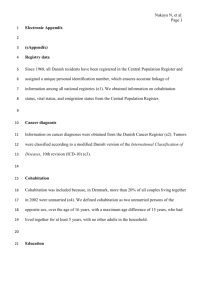
ONLINE SUPPLEMENTARY Statin use and risk of non-melanoma skin cancer: a nationwide study in Denmark Data sources Drug exposure classification Supplementary analyses Supplementary references Code list Supplementary Tables Sidsel Arnspang1, Anton Pottegård1,2, Søren Friis3, Ole Clemmensen4, Klaus Ejner Andersen5, Jesper Hallas1,2, David Gaist6 1 Clinical Pharmacology, Institute of Public Health, University of Southern Denmark, J.B. Winsløws Vej 19, 2.sal , 5000 Odense C, Denmark 2 Department of Clinical Chemistry & Pharmacology, Odense University Hospital, J.B. Winsløws Vej 19, 2.sal , 5000 Odense C, Denmark 3 Danish Cancer Society Research Centre, Strandboulevarden 49, 2100 Copenhagen Ø, Denmark; Faculty of Health, Institute of Clinical Medicine, Aarhus University, Aarhus, Denmark; and Department of Public Health, University of Copenhagen, Copenhagen, Denmark. 4 Department of Clinical Pathology, Odense University Hospital, J.B. Winsløws Vej 15, 5000 Odense C, Denmark 5 Department of Dermatology and Allergy Centre, Odense University Hospital, Institute of Clinical Research, Faculty of Health Sciences, University of Southern Denmark, Sdr. Boulevard 29, 5000 Odense C, Denmark 6 Department of Neurology, Odense University Hospital, Institute of Clinical Research, Faculty of Health Sciences, University of Southern Denmark, Sdr. Boulevard 29, 5000 Odense C, Denmark 22nd June 2014 1 DATASOURCES Our study was based on information from the following nationwide Danish registries: the Danish Cancer Registry (DCR) (Gjerstorff 2011), the Danish Civil Registration System (Pedersen 2011), the Danish National Prescription Registry (Kildemoes 2011), the Danish National Patient Register (DNPR) (Lynge 2011), and registries in Statistics Denmark (Thygesen 2011, Thygesen 2014). Cancer diagnoses in the DCR are recorded according to the International Classification of Diseases, version 10 (ICD-10), and the ICD for Oncology (ICD-O-3) for topography and morphology codes. Linkage to the Danish Pathology Registry has ensured a virtually complete registration of BCC in the DCR since 2004 (Bjerregaard 2011). Diagnoses of BCC and SCC were ascertained on the basis of the ICD-10 diagnosis for NMSC and the specific ICD-O-3 codes for SCC and BCC (Code list). Controls were selected from the entire Danish population using the Civil Registration System (Pedersen 2011) and risk-set sampling (Rothman 2008), i.e., the controls had to be alive and at risk for a first diagnosis of BCC/SCC at the time the corresponding case was diagnosed (index date). The Civil Registration System is continuously updated and includes data on vital status and migration. Information on highest educational level achieved by study subjects according to annually updated information was retrieved from registries at Statistics Denmark (Jensen 2011). Information on use of statins and other drugs was obtained from the National Prescription Registry, which contains information on all prescriptions dispensed at community pharmacies in Denmark since 1995 (Kildemoes 2011). For each prescription, the Prescription Registry records date and a full description of the dispensed product, including the anatomical therapeutic code (ATC) (WHO 2012) and the number of defined daily doses (DDD) in each package. One DDD represents the typical daily dose required by an adult when the drug is used for its main indication (WHO 2012). Drugs used for the same indication are thus in principle equipotent when measured in DDD. DRUG EXPOSURE CLASSIFICATION We retrieved prescription data from 1995 to the index date for both cases and controls. In the main analyses, we evaluated statin use in a 10-year time-window prior to the index date. We disregarded statin prescriptions redeemed within the last year before the index date, in order to avoid 2 potential selective prescribing of statins among cases close to the NMSC diagnosis (Rothman 2008). Based on the number of statin prescriptions dispensed during the 10-year period (i.e., 1-10 years) prior to index date, statin use was classified as ever use (≥2 statin prescriptions; ATC group C10AA) or non-use (0 or 1 prescription for statins). We further defined duration of statin use based on the dates of prescription and number of days covered by the individual prescriptions. The coverage of each prescription was calculated as the sum of tablets for the prescription plus a grace period of 25% of the dispensed tablets. We used the sum of tablets as this measure has been shown to concord highly with the prescribed daily dose for statins (Kanstrup 2004). The grace period was introduced to allow some degree of non-compliance. The arbitrarily chosen length of the grace period corresponds to an approximate adherence of 80%. A continuous treatment period lasted for as long as consecutive prescriptions were presented within the time-window defined by the coverage of the preceding prescription. For study subjects with more than one treatment period, the durations of separate treatment periods were added. The cumulative duration of use was categorised into four mutually exclusive strata: <1, 1 to <3, 3 to <5, and ≥5 years. We also classified statin use by the total number of DDDs presented during the 10-year period prior to the index date: 1-199, 200-499, 500-999, 1000-1999, ≥2000 DDD. We defined intensity of statin use as the cumulative number of DDDs of statins prescribed to a study subject divided by the number of days between the first and last eligible statin prescription plus 60 days. Furthermore, we classified statins as lipophilic (simvastatin, lovastatin, fluvastatin, atorvastatin, and cerivastatin) and hydrophilic (pravastatin and rosuvastatin). Exposure to the potential confounder drugs was defined as ≥2 prescriptions during the 10-year time period prior to the index date, with the exception of non-aspirin NSAID use, which was classified in three categories, i.e., non-use (0-1 prescriptions), low use (2-9 prescriptions), or high use (≥10 prescriptions). SUPPLEMENTARY ANALYSES We performed a number of supplementary analyses in which we: (i) stratified by gender, age, and NSAID use to explore possible effect measure modification, (ii) restricted the sample to subjects with index dates during 2008-2009, thus expanding the exposure period to 12 years prior to index date and examining effects of long-term statin exposure defined as 5+ years and 10+ years, 3 (iii) evaluated the influence of i) including exposure within one year prior to index date and ii) expanding the lag-period to 2 years prior to index date. All analyses were performed using Stata Release 13.0 (StataCorp, College Station, TX, USA). The study was approved by the Danish Data Protection Agency and Statens Serum Institut. Ethical approval is not required for purely registry based studies according to Danish law (Thygesen 2011). SUPPLEMENTARY REFERENCES Bjerregaard B, Larsen OB (2011) The Danish Pathology Register. Scand J Public Health 39(Suppl): 72-4 Jensen VM, Rasmussen AW (2011) Danish education registers. Scand J Public Health 39(7 Suppl): 91-94 Kanstrup H, Lassen JF, Heickendorff L, Lauritzen T, Larsen ML (2004) Quality of lipid-lowering therapy in patients with ischaemic heart disease: a register-based study in 3477 patients. J Intern Med 255: 367-372 Kildemoes HW, Toft Sørensen H, Hallas J (2011) The Danish National Prescription registry. Scand J Public Health 39(7 Suppl): 38–41 Lynge E, Sandegaard JL, Rebolj M (2011) The Danish National Patient Register. Scand J Public Health 39(7 Suppl): 30–33 Thygesen LC, Daasnes C, Thaulow I, Brønnum-Hansen H (2011) Introduction to Danish (nationwide) Registers on Health and Social Issues: Structure, Access, Legislation, and Archiving. Scandinavian Journal of Public Health 39(7 Suppl): 12–16 Thygesen LC, Ersbøll AK (2014) When the entire population is the sample: strengths and limitations in register-based epidemiology. Eur J Epidemiol DOI: 10.1007/s10654-013-9873-0 [Epub ahead of print] WHO Collaborating Centre for Drug Statistics Methodology, Guidelines for ATC classification and DDD assignment, 2013. Oslo, 2012 4 CODE LIST Cancer codes ICD-10 C44 – Non-melanoma skin cancer ICD-0-3 morphology Basal cell carcinoma 80903, 80913, 80923, 80933, 80943, 80953, 80973, 80983 Squamous cell carcinoma 80513, 80703, 80713, 80723, 80733, 80743, 80753, 80763, 80783, 80833, 80843 ATC codes Statins C10AA01 - Simvastatin C10AA02 – Lovastatin C10AA03 – Pravastatina C10AA04 - Fluvastatin C10AA05 – Atorvastatin C10AA06 – Cerivastatin C10AA07 – Rosuvastatina Other drugs (covariates) Aspirin – low-dose B01AC06 – acetylsalicylic acid (75 mg, 100 mg, or 150 mg per tablet) B01AC30 – acetylsalicylic acid (50 mg per tablet) in combination with dipyridamole Non-aspirin nonsteroidal anti-inflammatory drugs M01A (including Cox2 inhibitors), excluding M01AX Antidiabetics A10 Diuretics C03A, C03EA01, C03EA13, C07B, C07D, C09BA, C09DA, C09XA52, C09XA54 – thiazides C03CA01 C03EB01 C03CA02 C03EB02 C03EA01 C03DA01 – other diuretics Immunosuppressants H02AB06 H02AB07 – glucocorticoids L04AX01 – azathioprine L01AA01, L04AA06, L04AD01, L04AD02, L04AX03 – other immunosuppressants Hormone replacement therapy G03CA03 G03CA04 G03CA53 G03CA57 G03CB01 G03CX01 G03FA01 G03FA12 G03FA10 G03FA11 G03FA15 G03FA17 G03FB11 G03FB05 G03FB06 G03FB01 G03FB09 G03DC02 G03DA02 G03DA04 G03DB08 G03DB01 G03DC03 Amiodarone C01BD01 Antipsoriatics for topical use D05AX Hospital discharge codes Diabetes ICD-8: 249, 250 ICD-10: E10-E14 COPD ICD-8: 49000 49100 49101 49103 5 ICD-10: J42 J43 J44 Atopic dermatitis ICD-8: 691 ICD-10: L20 Psoriasis ICD-8: 69609 69610 69619 ICD-10: L40 M070 M071 M072 M073 Connective tissue disease (rheumatoid arthritis and other inflammatory polyarthropathies, polymyalgia rheumatica, diffuse connective disease, sarcoidosis) ICD-8: 135.99, 446, 712, 716, 734 ICD-10: D86, M05, M06, M08, M09, M30-M36 Moderate to severe renal disease (glomurelonephritis, nephropathies, and end-stage renal disease) ICD-8: 403, 404, 580-583, 590.09, 593.19, 753.10-753.19, 792 ICD-10: I12, I13, N00-N05, N07, N11, N14, N17-N19, Q61 Organ transplant recipients ICD-8 or NCSPb: Y9509, or NCSP procedure: 32209, 32219, 32229, 32240, 32250, 35609, 47270, 47279, 48840, 48849, 57480, 57490 ICD-10 or NCSPb: DZ940- DZ944, DZ948, DZ949 or NCSP procedure: KGDG, KFQA, KFQB, KJJC, KJLE, KKAS a Classified as hydrophilic; other statins classified as lipophilic. b Nordic Classification of Surgical Procedures (NCSP) code. 6 SUPPLEMENTARY TABLES eTable 1. Characteristics of non-melanoma skin cancer cases and their matched controls Gender Male Female Age, median (interquartile range) Schooling, number of years 7-10 11-12 ≥13 Missing History of a Diabetesb Psoriasisb Atopic dermatitis COPD Connective tissue disease Kidney disease Charlson Comorbidity Index (CCI) score 0 1 2 ≥3 Drug usec Statin Glucocorticoid Azathioprine Other immunosuppressant Amiodarone Thiazides Other diuretics Hormone replacement therapy Aspirin, low-dose Non-aspirin NSAID, number of prescriptions 0-1 2-9 10+ Basal cell carcinoma Cases Controls (n=38,484) (n=384,756) Squamous cell carcinoma Cases Controls (n=3,724) (n=37,188) 18,136 (47.1) 20,348 (52.9) 66 (57 - 76) 181,320 (47.1) 203,436 (52.9) 66 (57 - 76) 2,144 (57.6) 1,580 (42.4) 77 (67 - 84) 21,411 (57.6) 15,777 (42.4) 77 (67 - 84) 11,553 (30.0) 14,574 (37.9) 9,807 (25.5) 2,549 (6.6) 146,154 (38.0) 135,136 (35.1) 76,543 (19.9) 26,913 (7.0) 1,449 (38.9) 1,022 (27.4) 573 (15.4) 680 (18.3) 14,533 (39.1) 10,464 (28.1) 5,289 (14.2) 6,902 (18.6) 2,279 (5.9) 363 (0.9) 63 (0.2) 1,553 (4.0) 1,497 (3.9) 665 (1.7) 28,173 (7.3) 2,589 (0.7) 605 (0.2) 17,504 (4.5) 12,969 (3.4) 6,075 (1.6) 404 (10.8) 42 (1.1) 12 (0.3) 275 (7.4) 207 (5.6) 123 (3.3) 3,364 (9.0) 231 (0.6) 35 (0.1) 2,379 (6.4) 1,573 (4.2) 887 (2.4) 28,247 (73.4) 6,578 (17.1) 2,046 (5.3) 1,613 (4.2) 277,142 (72.0) 67,362 (17.5) 21,987 (5.7) 18,265 (4.7) 2,134 (57.3) 920 (24.7) 351 (9.4) 319 (8.6) 23,110 (62.1) 8,231 (22.1) 3,222 (8.7) 2,625 (7.1) 6,744 (17.5) 2,457 (6.4) 214 (0.6) 536 (1.4) 197 (0.5) 10,060 (26.1) 4,475 (11.6) 7,396 (19.2) 8,021 (20.8) 66,148 (17.2) 23,151 (6.0) 1,179 (0.3) 3,652 (0.9) 1,844 (0.5) 98,590 (25.6) 46,848 (12.2) 59,873 (15.6) 81,116 (21.1) 778 (20.9) 367 (9.8) 41 (1.1) 71 (1.9) 25 (0.7) 1,454 (39.0) 1,024 (27.5) 537 (14.4) 1,286 (34.5) 7,176 (19.3) 3,036 (8.2) 94 (0.3) 363 (1.0) 261 (0.7) 12,600 (33.9) 7,109 (19.1) 4,728 (12.7) 12,233 (32.9) 20,957 (54.5) 13,118 (34.1) 4,409 (11.5) 213,723 (55.5) 127,221 (33.1) 43,812 (11.4) 1,951 (52.4) 1,276 (34.3) 497 (13.3) 20,310 (54.6) 11,760 (31.6) 5,118 (13.8) a Based on Patient Registry data. Based on Patient and Prescription Registry data. c Based on Prescription Registry data. b 7 eTable 2. Long-term exposure to statins (≥5 years) and risk of NMSC stratified by age and gender. Cases Controls Exposed/Unexposed Exposed/Unexposed Adj ORa (95% CI) – model 1 Adj ORb (95% CI) – model 2 Basocellular carcinoma All 1,418 / 31,740 13,806 / 318,608 1.04 (0.98-1.10) 1.10 (1.03-1.17) Gender Male 824 / 14,427 8,107 / 145,612 1.03 (0.96-1.12) 1.07 (0.98-1.16) Female 594 / 17,313 5,699 / 172,996 1.04 (0.95-1.14) 1.14 (1.04-1.25) Age group, years <60 88 / 11,368 1,040 / 112,722 0.84 (0.68-1.05) 0.96 (0.76-1.21) 60-75 741 / 12,303 7,437 / 122,799 1.01 (0.93-1.09) 1.10 (1.00-1.20) ≥75 589 / 8,069 5,329 / 83,087 1.13 (1.03-1.24) 1.16 (1.06-1.28) Squamous cell carcinoma All 171 / 2,946 1,573 / 30,012 1.14 (0.96-1.35) 1.02 (0.85-1.22) Gender Male 108 / 1,648 1,080 / 16,792 1.05 (0.85-1.30) 0.95 (0.75-1.19) Female 63 / 1,298 493 / 13,220 1.32 (1.00-1.75) 1.08 (0.88-1.58) Age group, years <60 7 / 321 44 / 3,357 1.69 (0.75-3.84) 0.99 (0.37-2.64) 60-75 65 / 966 632 / 9,731 1.08 (0.83-1.42) 0.93 (0.69-1.26) ≥75 99 / 1,659 897 / 16,924 1.15 (0.92-1.44) 1.07 (0.84-1.35) a Adjusted for age and gender b Adjusted for age, gender, years of schooling, history of atopic dermatitis, psoriasis, COPD, diabetes, CCIscore, and use of systemic glucocorticoids, azathioprine, other immunosuppressants, thiazides, other diuretics, hormone replacement therapy, amiodarone, low-dose aspirin, or non-aspirin NSAID drugs 8