Title page
advertisement

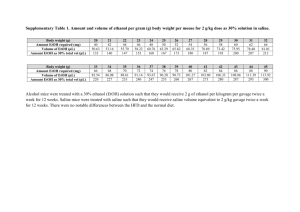
Title page Title Influence of small doses of various vehicles on acetaminophen induced liver injury Running title: Vehicles in acetaminophen hepatotoxicity Authors Tomislav Kelava1, Ivan Ćavar1,2, and Filip Čulo1,2 Affiliations: 1 Department of Physiology, School of Medicine, University of Zagreb, Croatia 2 Department of Physiology, School of Medicine, University of Mostar, Bosnia and Herzegovina Corresponding author: Tomislav Kelava, Department of Physiology, School of Medicine, University of Zagreb, Croatia, Šalata 3b, 10000 Zagreb, Croatia. Phone number: 00 385 91 34 70 585 Fax Number: 00 385 1 4590-207 E-mails: tkelava@yahoo.co.uk, ivancavarsb@yahoo.com, fculo@mef.hr All investigations were conducted at Department of Physiology, School of Medicine, University of Zagreb, Croatia Source of support: Supported by Research project No. 0108-0000000-0328 by Croatian Ministry of Science, Higher Education and Sports Summary: Background: Organic solvents or detergents are used in biological studies to facilitate solution of drugs with low solubility. Although they are generally thought of as being relatively inert, they can induce effects that are often overlooked. Inadequate usage of vehicles is the leading cause of artifacts in acetaminophen induced liver injury (AILI) investigations. Therefore, we decided to investigate the effect of dimethylsulfoxide (DMSO), dimethylformamide (DMF), propylene glycol (PG), ethanol (ETOH) and Tween20 on AILI. Material and methods: C57BL/6 male mice received intraperitoneally (i.p.) 30 minutes before acetaminophen (300 mg/kg, i.p., in warm saline) injection of saline, DMSO, DMF, PG or Tween 20, at 0,6 mL/kg or 0,2 mL/kg. Control groups received only vehicle. After seven hours blood and livers were taken for analysis. Alanine aminotransferase levels (ALT) in plasma and reduced glutathione (GSH) levels in liver were determined and histopatological slides were evaluated. Results: DMSO and DMF (both doses) almost completely abolished AILI. PG (0,6 mL/kg) was also protective, but the dose of 0.2 mL/kg was only partially effective. These three solvent blocked acetaminophen induced GSH depletion. ETOH (0,6 mL/kg) was partially effective, while the dose of 0,2 mL/kg and TWEEN 20 (both doses) had no influence. In control groups DMF (0,6 mL/kg) slightly decreased GSH levels, while the dose of 0,2 mL/kg and any other vehicle had no significant influence on GSH or ALT levels. None of the vehicles was protective in model of liver injury caused by D-galactosamine and lipopolysaccharide. Conclusion: Extreme caution is needed when organic solvents are used in AILI investigations. Key words: acetaminophen, dimethylsulfoxide, dimethylformamide, propylene glycol, ethanol, liver injury Influence of small doses of various vehicles on acetaminophen induced liver injury Background Acetaminophen (APAP) is a widely used analgesic and antipyretic drug that is considered safe at therapeutic doses. Overdose of APAP causes liver damage and for the last two decades this is the leading cause of acute hepatic failure in the western world [1, 2]. The toxicity is initiated by formation of a reactive metabolite, N-acetyl-p-benzoquinone imine (NAPQI), by liver microsomal enzymes, -which first depletes glutathione and then covalently binds to cellular proteins [3, 4]. APAP induced liver injury (AILI) in mice is the most extensively used model for studying mechanisms of drug induced liver injury [5, 6]. Some of the major biases in AILI investigations have occurred because drug solvents, which have biological effect per se, were used, particularly DMSO. For example El-Hassan et al reported a protective effect of the pancaspase inhibitor Z-VAD-fmk against APAP toxicity in mice. As a control, they used cathepsin inhibitor benzyloxycarbonyl-Phe-Alafluoromethylketone (Z-FA-fmk) and found no protection with this compound. However, they did not add small amount of DMSO to Z-FA-fmk which was used to help Z-VAD-fmk dilution [7]. Later it was shown that small amount of DMSO and not Z-VAD-fmk protected mice from APAP [8]. Similarly, it was reported that natural killer cells (NK) have a pathogenic role in AILI [9], but recently it was shown that this is true only when DMSO is used to help dissolve APAP (as it was in above mentioned experiments), but not when APAP was given without DMSO [6]. Vehicles commonly used in AILI experiments include DMSO [7], ethanol (ETOH), corn oil [10], olive oil [11], Tween 20 [12], Tween 80 [13], propylene glycol (PG) [14] and methylcellulose [15]. They are used for two purposes; to facilitate solution of some other substance - investigated for its effect on AILI or to help dissolve APAP itself; in the later case PG is frequently used. Despite its obvious importance, influence of vehicles on AILI is rarely investigated; it is usually done when bias already happened. So far, it was shown, more or less convincible, that DMSO, PG and ETOH, if injected 15-30 minutes before APAP or 1-2 hours after APAP abolish its toxicity, most probably by preventing APAP conversion to NAPQI by CYP2e1 inhibition. However, most of these investigations were done for doses of vehicles larger than 1 mL/kg [16-18] and in AILI experiments smaller doses are usually used. Notable exception is DMSO, for which good dose dependant study was conducted, which showed a strong protective effect even when DMSO was administered at dose of 0.2 mL/kg [19]. The effects of various solvent, to our knowledge, were never compared. Therefore, we decided to compare effect of three most often used solvent (DMSO, PG and ETOH) on AILI as well to investigate the effect of Tween 20 and DMF which has not been investigated. Main object of our study was to show which vehicle at doses of 0,2 and 0,6 mL/kg change the intensity of AILI and which is indifferent. Beside common parameter of APAP toxicity (serum aminotransferase level) and pathohistology, the influence on GSH content in liver and microsomal enzyme activity was also investigated. Materials and Methods Animals C57BL/6 mice were raised in an animal colony unit at the Department of Physiology, School of Medicine, Zagreb. Male mice aged 12-16 weeks and weighing 20-25 g were used in all experiments. The cages were stored in rooms with a 12 h light period from 6 a.m. to 6 p.m., and the temperature and relative humidity in the animal room were 21±2°C and 50±5%, respectively. The cages were sanitized twice weekly. All mice were given free access to tap water and standard mouse chow diet (Diete Standard 4 RF21 Mucedola S.r.i., Milan, Italy). All animal protocols were approved by the Ethics Committee of the University of Zagreb, School of Medicine (Zagreb, Croatia). Chemicals Pure APAP substance was a kind gift from the Belupo Pharmaceutical Company (Koprivnica, Croatia). Trichloroacetic acid (TCA), Ethanol (96%), DMSO, PG and DMF were purchased from Kemika, Zagreb, Croatia. Thiopental sodium was from Rotex Medica , Trittau, Germany). L-Glutathione reduced, D-galactosamine, Bovine serum albumine (BSA) and 5,5dithiobis 2-nitro-benzoic acid (DTNB) were from Sigma-Aldrich, St. Louis, U.S.A. Acetaminophen induced liver injury A total of five experiments were conducted. In all experiments mice were fasted overnight (16 hours). Next morning they were randomly divided into groups (n = 6-8) and received i.p. 30 minutes before APAP either saline, DMSO, DMF, PG or Tween 20 (all diluted in saline), at 0,6 mL/kg in first and 0,2 mL/kg in second experiment in a volume of approximately 0,2 mL per animal. APAP, dissolved in warm saline under mild magnetic stirring, was administered also i.p. at 300 mg/kg, in a volume of approximately 0,5 mL per animal. Control groups of animals received only vehicle (i.e. without APAP). In majority of published experiments APAP and investigated substance were both injected i.p. To exclude the effect of administration route, and possible interferences of chemicals, we conducted third experiment which………….. lavage. In fourth experiment saline or DMF (0,6 mL/kg, i.p) were injected 2 hours before or 1, 2.5 and 4 hours after APAP administration. In fifth experiment mice received sodium phenobarbitone (300 mg/L) in drinking water for 7 days prior to APAP administration in order to induce liver microsomal enzymes. DMSO (0.2 mL/kg, i.p.) or saline (i.p.) were injected 30 minutes before APAP. In all experiments food was returned 4 hours after APAP and after additional 3 hours mice were anesthetized with Avertine; blood was collected by puncture of the medial eye angle with heparinized glass capillary tubes and the livers were removed for analyses. Hepatic injury induced by D-galactosamine (GalN) and lipopolysaccharide (LPS) Mice were injected i.p. simultaneously with GalN (300 mg/kg) and LPS (15 g/kg). Saline, DMSO, DMF, ETOH, PG or Tween 20 were injected i.p. (0,6 mL/kg) 30 minutes before intoxication with GalN + LPS. Evaluation of liver injury Blood was centrifuged and plasma was collected and stored at -80°C. Alanine aminotransferase (ALT) levels were determined by standard laboratory techniques in clinical diagnostic laboratory. A portion of the liver was fixed in 10% neutral formalin, processed by histologic techniques, stained with hematoxylin-eosin, and examined for morphologic evidence of liver injury. Hepatic GSH Determination Reduced glutathione (GSH) in liver tissues was determined according to the Ellman method [20]. A portion (approximately 100 mg) of liver was homogenized in Tris-HCl buffer (25mmol/l, pH 7.4) and 0.1 mL of homogenate was mixed with 0.2 mL 5% TCA, followed by centrifugation at 860 g for 10 minutes. Supernatant was mixed with DTNB. The absorbance was determined at 412 nm. The GSH level was compared with a standard curve prepared with six different GSH concentrations. From the rest of homogenate protein concentrations were determined using the Bradford method with bovine serum albumin as the standard [21] and GSH content was calculated in nmoles/mg proteins. Measurement of thiopental sleeping time Mice (n=4 per group) were injected with saline, DMSO, DMF, PG, ETOH or Tween 20 (0,6 mL/kg, 1l/g, i.p.), and after 30 minutes thiopental sodium (50 mg/kg, i.p.) was injected. The sleeping time was defined as the sleep-time period from the loss of the righting reflex to its complete recovery [22, 23]. Statistical analysis Data are presented as means ± SEM. Statistical significance was evaluated by ANOVA followed by Dunnetts’ multiple comparison test, and accepted when P < 0.05. Results At dose of 0.6 mL/kg DMSO, DMF, and PG almost completely abolished AILI; ALT levels were 37, 45 and 15 times, respectively, smaller then in control group (which received saline before APAP) (Table1). The difference was clearly visible histopathologically and also macroscopically (Figure 1). ETOH only slightly reduced ALT levels (not statistically significant - NS) and Tween 20 had no influence at all. APAP depleted GSH from liver and DMF, DMSO and PG inhibited this depletion. When given alone (i.e. without APAP treatment) DMF reduced slightly but significantly GSH level in comparison to mice given saline, while other vehicles had no such effect. DMF alone reduced slightly but significantly GSH level, while other vehicles had no such effect. None of the vehicles alone increased ALT levels in blood significantly (Table 1). The different protective effect of these substances was clearly visible histopathologically (Figure 1); centrilobular necrosis seen in mice given saline (or Tween 20) before APAP Fig. 1A,C), was almost absent in mice given DMF (Fig. 1B,D) or DMSO before APAP. At dose of 0.2 mL/kg DMF and DMSO were similarly effective; ALT levels were 15 and 18 times smaller (lower) then in the control group, they also inhibited GSH depletion. At this dose PG also reduced ALT concentration and blocked GSH depletion, but not significantly. ETOH and Tween 20 had no influence. DMF alone had no influence on GSH levels (Table 2) DMF at dose 0.6 mL/kg completely blocked APAP toxicity if given 2 hours before APAP; it was also effective if given 1 hour after APAP administration, but ineffective not if given 2.5 or 4 hours after APAP (Figure 2). DMSO at dose 0.2 mL/kg was highly protective even in mice which were given sodium phenobarbitone in drinking water for 7 days before APAP administration. ALT levels were 30 fold smaller in DMSO group then in control group (Figure 3). DMSO and DMF increased thiopental sleeping time significantly. PG also prolonged it, but not significantly, while TWEEN20 or ETOH had no influence (Table 3). None of the vehicles was able to protect mice from liver injury caused by LPS/GalN administration (Figure 4). Discussion Although solvents are generally thought of as being relatively inert, they can induce biological effects that are often overlooked. AILI is shown to be very sensitive to bias caused by solvents [6, 8]. Our results show that DMSO and DMF greatly suppress AILI even at small doses (0,2 mL/kg), PG is somewhat less protective and it seems that doses of ETOH (0,2 mL/kg) and Tween 20 (0,2 and 0,6 mL/kg) are indifferent. None of them appears to be hepatotoxic itself at above mentioned doses. The most probable way of protection is interference with liver microsomal metabolism of APAP. This is supported with our findings that PG, DMSO and DMF block APAP induced GSH depletion and prolong thiopental sleeping time. None of them change GSH content if given alone, except DMF at dose of 0,6 mL/kg which caused a small but significant GSH depletion. Yoon ET all proposed that DMSO inhibits microsomal formation of NAPQI in competitive manner [19]. Therefore, we hypothesized that experimental model in which microsomal enzymes are induced prior to APAP administration will be less sensitive to DMSO. However, our results show that model, in which microsomal enzymes are induced with phenobarbitone for 7 days in drinking water [24, 25], is equally sensitive to DMSO. Beside its effect on APAP metabolism each of these vehicles can change several others parameters that play role in AILI. For example, DMSO posses antioxidative activity [26, 27], and adjuvant-like actions on the immune system [28, 29], the later effect was the cause of bias in already mentioned NK cell investigation and several antioxidants protect from AILI [30, 31], Since DMSO is so frequently shown to invalidate investigations, we thought that DMF might be an useful alternative (some of the substances that we intend to investigate in the future can be dissolved in both DMSO and DMF). However, DMF showed similar protective effect as DMSO. There are no reports about its effect on oxidative stress or immunological system. On the other hand, DMF possess anticoagulant like effect [32] and some anticoagulants are able to protect from AILI [33]. Since this is the first report about the protective effect of DMF we further investigated the effect of time of its application. It showed typical pattern for substances that interfere with APAP metabolism - a very strong protection if given before APAP, but no protection if given 2.5 hours after APAP (although it was protective if given 1 hour after APAP). DMF inhibits CYP2e1 most probably by suicidal enzyme inactivation [34]. Protective effect of PG is well known; however all experiment were conducted with high doses (between 2 and 4 mL/kg) [17, 18] and our results demonstrate that even small doses (0.2 and particularly 0.6 mL/kg) can suppress AILI. For ETOH it is generally accepted that its chronic consumption increase AILI, but acute administration together with or shortly before APAP suppresses AILI [35]. With dose of 0,2 mL/kg there was no protection, and dose of 0,6 mL/kg only slightly decreased ALT levels. PG and ETOH can reduce inflammatory response and oppositely to DMSO, inhibit NK activity [36-39]. Detergents, TWEEN 20 and TWEEN 80, are also sometimes added to help solubility of lipophilic drugs in AILI experiments. It appears that doses of TWEEN 20 of 0.2 and 0.6 mL/kg do not change magnitude of AILI and GSH liver content. There are no reports about its influence neither on immunological response, oxidative stress, and Cyp2e1 activity nor coagulation system. In another common model of liver injury (GalN/LPS) none of the vehicles was protective or harmful. Interestingly, there are reports that show that DMSO is protective against D-galactosamine alone in rats. However, in those experiments the dose of DMSO was much larger (2.5 mL/kg) [40] To avoid artifacts in AILI investigations it would be good to use, when it is possible, pure saline as a vehicle without adding any organic solvent or detergent. This is possible in more occasions then is actually done. For example, 300 mg/kg of APAP, dissolved in warm saline under mild magnetic stirring, can be safely administered in a volume of approximately 0.5 mL per mice and this is more then enough to induce AILI. Since PG and DMSO suppress AILI when they are used as vehicles for APAP, the dose of APAP must be increased to 500 or even 750 mg/kg [14] in order to cause similar rate of AILI. The result is unnecessary increase of APAP dose and application of more biologically different organic solvent. Liu et al reported that 300 mg/kg of APAP is not enough to induce AILI to C57Bl/6 mice and concluded that this strain is more resistant to APAP [9]. Apparently this was because DMSO was added to APAP vehicle. In our experience the dose 300 mg/kg of APAP induces severe hepatitis in CBA or BALB/c mice and similar was shown for some other mice strains [15]. When substances with low solubility in water are investigated for its effect on AILI the control groups should be planned more carefully. Typical investigations include group which gets substance of interest dissolved in organic vehicle and the control group which gets only vehicle. It would be good to include at least in first experiment one more control group which would be treated with pure saline or distilled water, in order to better understand effect of vehicle. The dose of solvent or detergent added to vehicle should be as small as possible and explicitly quoted. It is probably better to use vehicles that interfere less with APAP toxicity. This means that Tween 20 and ETOH should be considered first, and then PG. DMSO and DMF should be used if there is no other option. Alternatively, some water insoluble substances become soluble if pH of saline is changed or if Tris buffer (pH 7.4) instead DMSO is used [41], although Tris buffer also possess some biological effects. If some general hepatoprotective mechanism is investigated it would be helpful to see if it works on GalN/LPS model of hepatotoxicity also. Since this model appears to be more robust to vehicle usage. Conclusion To avoid possible experimental artifacts with water insoluble drugs, it necessary to reduce the amount of injected of biologically active organic solvent (or reduces its concentration in vitro experiments) to possible minimum, use organic solvent with smaller biological effect, try to dissolve the substance in aqueous solvent with changed pH or different buffer. Finally, most important is to include control groups in which the effect of vehicle (solvent) alone will be tested. Table 1 Effect of DMSO, DMF, ETOH, PG and Tween 20 treatment (0.6 mL/kg) on AILI Vehicle (0.6 mL/kg) Saline DMSO DMF ETOH PG Tween 20 Saline DMSO DMF ETOH PG Tween 20 Normal mice APAP (mg/kg) 300 300 300 300 300 300 - ALT (U/L) 6747.5 ± 2290.4 178.6 ± 96.9* 135 ± 47.7* 4633.8 ± 2066.4 441.4 ± 317.8* 5268.6 ± 2512.6 20 ± 1.5 30.7 ± 5.7 27 ± 1.5 32.7 ± 5.2 28.3 ± 4.4 37.3 ± 7.1 22 ± 1.1 GSH (nmol/mg of proteins) 9.8 ± 1.26 53.2 ± 1.7* 56.1 ± 1.0* 19.6 ± 5.1 46.2 ± 5.7* 9.4 ± 2.5 64.9 ± 0.5 65.8 ± 0.9 57.1 ± 0.28** 63.8 ± 1.3 65.1 ± 0.7 64.5 ± 2.4 64.4 ±0.8 Mice were treated with DMSO, DMF, ETOH, PG, Tween20 or saline intraperitoneally 30 minutes prior to APAP or only with DMSO, DMF, ETOH, PG, Tween20. Each value represents the mean ± S.E of six to eight mice. * Significantly different from mice treated with saline before APAP ** Significantly different from mice given only saline (ANOVA followed by Dunnetts’ multiple comparison test, p<0.05). Table 2 Effect of DMSO, DMF, ETOH, PG and Tween20 treatment (0.2 mL/kg) on AILI Vehicle (0.2 mL/kg) Saline DMSO DMF ETOH PG Tween 20 Saline DMSO DMF ETOH PG Tween 20 APAP (mg/kg) 300 300 300 300 300 300 - ALT (U/L) 8767 ± 1663 585 ± 397* 470 ± 188* 8991 ± 2048 5830 ± 1242 8774 ± 1762 25.6 ± 1.6 29 ± 1.3 34.6 ± 3.5 24.6 ± 1.9 20.3 ± 0.2 29.6 ± 3.3 GSH (nmol/mg of proteins) 9.7 ± 0.9 44.9 ± 1.7* 44 ± 2.9* 12.1 ± 4.5 17.2 ± 5.5 11 ± 2.2 67.5 ± 1.8 65.6 ± 0.5 65.7 ± 0.7 65.8 ± 1.9 65.3 ± 1.8 64.1 ± 2.1 Mice were treated with DMSO, DMF, ETOH, PG, Tween20 or saline intraperitoneally 30 minutes prior to APAP or only with DMSO, DMF, ETOH, PG, Tween20 and saline. Each value represents the mean ± S.E. of six mice. * Significantly different from mice treated with saline before APAP (ANOVA followed by Dunnetts’ multiple comparison test, p<0.05). Table 3 Effect of DMSO, DMF, ETOH, PG, Tween20 treatment (0.6 mL/kg) on thiopental sleeping time Vehicle (0.6 mL/kg) Saline DMSO DMF ETOH PG Tween 20 Sleeping time (min) 1.1 ± 0.3 26.2 ± 2.3** 26 ± 2.2** 1 ± 0.3 3.8 ± 0.7 0.9 ± 0.1 Mice were treated with DMSO, DMF, ETOH, PG, Tween 20 or saline intraperitoneally 30 minutes prior to thiopental sodium. Each value represents the mean ± S.E. of four mice. ** Significantly different from mice treated with saline (ANOVA followed by Dunnetts’ multiple comparison test, p<0.01). A B C D Figure 1 histopathology In the typical microphotograph of the liver in the rat treated with acetaminophen, extensive zonal necrosis of centrilobular hepatocytes was observed (Fig. 5A). In contrast, neither hepatic necrosis nor abnormality was observed in the hepatic section from the rat treated with ONO-1714 at 100 Ag/ kg in addition to acetaminophen (Fig. 5B). 16000 14000 ALT (U/L) 12000 10000 8000 6000 4000 ** 2000 * 0 Saline DMF (-2h) DMF(+1h) DMF (+2.5h) DMF (+4h) Figure 2. Time effect of DMF on ALT plasma levels. Mice were treated with saline or DMF (0.6 mL/kg) at indicated times prior or after the APAP. Each value represents the mean ± S.E of six or seven mice. *, ** Significantly different from mice treated with saline and APAP (ANOVA followed by Dunnetts’ multiple comparison test, p<0.05, 0.001 respectively). ALT (U/L) 15000 10000 5000 ** 0 Saline DMSO Figure 3. Effect of DMSO on ALT levels in mice treated with phenobarbitone before APAP. Mice were pretreated with phenobarbitone in drinking water (300 mg/l) and then treated with DMSO (0.2 mL/kg) or saline prior to APAP. Each value represents the mean ± S.E of eight mice. ** significantly different from mice treated with saline before APAP (Student’s t-test, p<0.001). 6000 ALT (U/L) 5000 4000 3000 2000 1000 0 Saline DMSO DMF ETOH PG Tween 20 + GalN/LPS Figure 4. Effect of DMSO, DMF, ETOH, PG and Tween20 on ALT levels in GalN/LPS model. Mice were treated with DMSO, DMF, ETOH, PG, Tween20 or saline intraperitoneally 30 minutes prior to D-galactosamine and lipopolysaccharide administration. Each value represents the mean ± S.E of six mice. 1. Lee WM: Acetaminophen and the U.S. Acute Liver Failure Study Group: lowering the risks of hepatic failure. Hepatology 2004; 40(1): 6-9. 2. Norris W, Paredes AH, Lewis JH: Drug-induced liver injury in 2007. Curr Opin Gastroenterol 2008; 24(3): 287-97. 3. Nelson SD: Metabolic activation and drug toxicity. J Med Chem 1982; 25(7): 753-65. 4. Mitchell JR, Jollow DJ, Potter WZ, Davis DC, Gillette JR, Brodie BB: Acetaminopheninduced hepatic necrosis. I. Role of drug metabolism. J Pharmacol Exp Ther 1973; 187(1): 185-94. 5. Gunawan BK, Kaplowitz N: Mechanisms of drug-induced liver disease. Clin Liver Dis 2007; 11(3): 459-75, v. 6. Masson MJ, Carpenter LD, Graf ML, Pohl LR: Pathogenic role of natural killer T and natural killer cells in acetaminophen-induced liver injury in mice is dependent on the presence of dimethyl sulfoxide. Hepatology 2008; 48(3): 889-97. 7. El-Hassan H, Anwar K, Macanas-Pirard P, et al.: Involvement of mitochondria in acetaminophen-induced apoptosis and hepatic injury: roles of cytochrome c, Bax, Bid, and caspases. Toxicol Appl Pharmacol 2003; 191(2): 118-29. 8. Jaeschke H, Cover C, Bajt ML: Role of caspases in acetaminophen-induced liver injury. Life Sci 2006; 78(15): 1670-6. 9. Liu ZX, Govindarajan S, Kaplowitz N: Innate immune system plays a critical role in determining the progression and severity of acetaminophen hepatotoxicity. Gastroenterology 2004; 127(6): 1760-74. 10. Donthamsetty S, Bhave VS, Mitra MS, Latendresse JR, Mehendale HM: Nonalcoholic steatohepatitic (NASH) mice are protected from higher hepatotoxicity of acetaminophen upon induction of PPARalpha with clofibrate. Toxicol Appl Pharmacol 2008; 230(3): 327-37. 11. Jodynis-Liebert J, Matlawska I, Bylka W, Murias M: Protective effect of Aquilegia vulgaris (L.) on APAP-induced oxidative stress in rats. J Ethnopharmacol 2005; 97(2): 351-8. 12. Renic M, Culo F, Bilic A, Bukovec Z, Sabolovic D, Zupanovic Z: The effect of interleukin 1 alpha on acetaminophen-induced hepatotoxicity. Cytokine 1993; 5(3): 192-7. 13. Kamanaka Y, Kawabata A, Matsuya H, Taga C, Sekiguchi F, Kawao N: Effect of a potent iNOS inhibitor (ONO-1714) on acetaminophen-induced hepatotoxicity in the rat. Life Sci 2003; 74(6): 793-802. 14. Oz HS, Chen TS: Green-tea polyphenols downregulate cyclooxygenase and Bcl-2 activity in acetaminophen-induced hepatotoxicity. Dig Dis Sci 2008; 53(11): 2980-8. 15. Harrill AH, Ross PK, Gatti DM, Threadgill DW, Rusyn I: Population-based discovery of toxicogenomics biomarkers for hepatotoxicity using a laboratory strain diversity panel. Toxicol Sci 2009; 110(1): 235-43. 16. Lee SM, Cho TS, Kim DJ, Cha YN: Protective effect of ethanol against acetaminopheninduced hepatotoxicity in mice: role of NADH:quinone reductase. Biochem Pharmacol 1999; 58(10): 1547-55. 17. Hughes RD, Gove CD, Williams R: Protective effects of propylene glycol, a solvent used pharmaceutically, against paracetamol-induced liver injury in mice. Biochem Pharmacol 1991; 42(3): 710-3. 18. Thomsen MS, Loft S, Roberts DW, Poulsen HE: Cytochrome P4502E1 inhibition by propylene glycol prevents acetaminophen (paracetamol) hepatotoxicity in mice without cytochrome P4501A2 inhibition. Pharmacol Toxicol 1995; 76(6): 395-9. 19. Yoon MY, Kim SJ, Lee BH, Chung JH, Kim YC: Effects of dimethylsulfoxide on metabolism and toxicity of acetaminophen in mice. Biol Pharm Bull 2006; 29(8): 1618-24. 20. Ellman GL: Tissue sulfhydryl groups. Arch Biochem Biophys 1959; 82(1): 70-7. 21. Bradford MM: A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 1976; 72: 248-54. 22. Henderson CJ, Otto DM, Carrie D, et al.: Inactivation of the hepatic cytochrome P450 system by conditional deletion of hepatic cytochrome P450 reductase. J Biol Chem 2003; 278(15): 13480-6. 23. Piel MT, Aldrete JA, Jones G: Influence of enzyme induction on the sleeping time of rats. Can Anaesth Soc J 1969; 16(6): 538-46. 24. Guarner F, Boughton-Smith NK, Blackwell GJ, Moncada S: Reduction by prostacyclin of acetaminophen-induced liver toxicity in the mouse. Hepatology 1988; 8(2): 248-53. 25. Belardinelli MC, Pereira F, Baldo G, et al.: Adult derived mononuclear bone marrow cells improve survival in a model of acetaminophen-induced acute liver failure in rats. Toxicology 2008; 247(1): 1-5. 26. Jeffery EH, Arndt K, Haschek WM: Mechanism of inhibition of hepatic bioactivation of paracetamol by dimethyl sulfoxide. Drug Metabol Drug Interact 1988; 6(3-4): 413-24. 27. Dunphy GB, Chen G, Webster JM: The antioxidants dimethylsulfoxide and dimethylthiourea affect the immediate adhesion responses of larval haemocytes from 3 lepidopteran insect species. Can J Microbiol 2007; 53(12): 1330-47. 28. Kunze M: Production of interferon in the white mouse by dimethyl sulfoxide. Ann N Y Acad Sci 1975; 243: 308-10. 29. Yamasaki T, Klein G, Ljunggren HG, et al.: Effects of dimethyl sulfoxide treatment on H2 expression and susceptibility to NK- or cytotoxic T-lymphocyte-mediated lysis of the YAC1 lymphoma and its beta 2-microglobulin-deficient variant. J Natl Cancer Inst 1988; 80(4): 263-9. 30. Marotta F, Yadav H, Gumaste U, Helmy A, Jain S, Minelli E: Protective effect of a phytocompound on oxidative stress and DNA fragmentation against paracetamol-induced liver damage. Ann Hepatol 2009; 8(1): 50-6. 31. Reisman SA, Aleksunes LM, Klaassen CD: Oleanolic acid activates Nrf2 and protects from acetaminophen hepatotoxicity via Nrf2-dependent and Nrf2-independent processes. Biochem Pharmacol 2009; 77(7): 1273-82. 32. Imbriani M, Ghittori S, Prestinoni A, Longoni P, Cascone G, Gamba G: Effects of dimethylformamide (DMF) on coagulation and platelet activity. Arch Environ Health 1986; 41(2): 90-3. 33. Ganey PE, Luyendyk JP, Newport SW, et al.: Role of the coagulation system in acetaminophen-induced hepatotoxicity in mice. Hepatology 2007; 46(4): 1177-86. 34. Tolando R, Zanovello A, Ferrara R, Iley JN, Manno M: Inactivation of rat liver cytochrome P450 (P450) by N,N-dimethylformamide and N,N-dimethylacetamide. Toxicol Lett 2001; 124(1-3): 101-11. 35. Prescott LF: Paracetamol, alcohol and the liver. Br J Clin Pharmacol 2000; 49(4): 291301. 36. Denning DW, Webster AD: Detrimental effect of propylene glycol on natural killer cell and neutrophil function. J Pharm Pharmacol 1987; 39(3): 236-8. 37. Oshiro TT, Teixeira CF, Oga S: Propylene glycol enhances anti-inflammatory effects of phenylbutazone. Gen Pharmacol 1990; 21(1): 131-4. 38. Chen CP, Boyadjieva NI, Advis JP, Sarkar DK: Ethanol suppression of the hypothalamic proopiomelanocortin level and the splenic NK cell cytolytic activity is associated with a reduction in the expression of proinflammatory cytokines but not anti-inflammatory cytokines in neuroendocrine and immune cells. Alcohol Clin Exp Res 2006; 30(11): 1925-32. 39. Pan HN, Sun R, Jaruga B, Hong F, Kim WH, Gao B: Chronic ethanol consumption inhibits hepatic natural killer cell activity and accelerates murine cytomegalovirus-induced hepatitis. Alcohol Clin Exp Res 2006; 30(9): 1615-23. 40. Iida C, Fujii K, Koga E, Washino Y, Ichi I, Kojo S: Inhibitory effect of dimethyl sulfoxide (DMSO) on necrosis and oxidative stress caused by D-galactosamine in the rat liver. J Nutr Sci Vitaminol (Tokyo) 2007; 53(2): 160-5. 41. Baber SR, Champion HC, Bivalacqua TJ, Hyman AL, Kadowitz PJ: Role of cyclooxygenase-2 in the generation of vasoactive prostanoids in the rat pulmonary and systemic vascular beds. Circulation 2003; 108(7): 896-901.