article - Rhizome Community Herbal Clinic
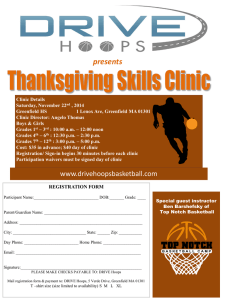
advertisement

Finding Common Ground My year working at Common Ground Health Clinic, New Orleans Becs Griffiths I spent 2010 working as a medical herbalist at a free primary healthcare clinic in New Orleans. The clinic offers integrated healthcare to the residents of Algiers, a predominantly African American neighborhood, located on the opposite bank of the Mississippi River from the city. The clinic was formed 5 days after Hurricane Katrina hit the city, which is where this story should begin. The Background At 8 am on the 29th of August 2005, Hurricane Katrina made landfall on the Gulf Coast. It hit New Orleans that evening and was gone by the next morning. Even though it was the third largest hurricane on record to make landfall in the U.S., New Orleans survived. It was not until two days later that the city started to flood. The devastation that resulted was due to the failure of the levee system. Approximately 85 % of the city eventually flooded up to 20 feet in some places and at least 1,800 people died. The levees and flood walls were built to withstand the storm surge from hurricanes but years of mismanagement and lack of funding had left the city vulnerable. New Orleans inhabits a unique place surrounded by vast amounts of water: it is tucked in from the south by the Mississippi river; the north of the city touches Lake Pontchartrain, a gigantic lake covering 630 square miles; and a system of industrial canals is mapped out across the city. The neglect and failure of the levees is indicative of how New Orleans has always been treated by the rest of the country. I have attended many community meetings in an attempt to comprehend the complicated historical and sociopolitical situation of this city. New Orleans was founded in 1718 by the French. It became the largest slave trading centre in the country and has always had a majority African American population. Segregation was only outlawed here in 1964 and institutional racism has played a part in keeping over 50% of the city living around or below the poverty line. Another huge impact on New Orleans is the oil industry, which has had a devastating effect on the environment and people's health. The Louisiana wetlands, formed over 7,500 years by the Mississippi river flooding and annually depositing silt, have been almost completely destroyed in the last 75 years. The oil industry has cut canals through the wetlands, to transport drilling equipment and oil from the city to the Gulf, which has gradually eroded them. These wetlands act as a natural defence against hurricane storm surges. As the wetlands decrease, the coastal towns all the way up to New Orleans become more vulnerable. Pollution is also a big problem. The ten oil refineries dotted around the city churn out so many toxins that the industrial corridor north of New Orleans is known as cancer alley. As the city flooded the federal response to Katrina was one of shocking neglect. People were left without food or water for four days. Those rescued were stranded on the interstate under scorching sun and high humidity. The scenes that were broadcast around the world of people 'looting' criminalised those left in the city. This 'looting' has been recounted to me as predominantly one of collective action where food and water were taken from shops and distributed amongst the survivors. The city was put under lockdown with a shoot to kill order and a dusk to dawn curfew issued by the governor. During this time there were many incidents of racist police violence. Armed white vigilantes prevented people escaping across the bridge from New Orleans to Algiers, which had not been flooded. Seventeen young black men were later found shot dead in this area. This is the context in which people managed to set up Common Ground Health Clinic. The Clinic Three days after the storm two community organizers living in Algiers, one of them a former Black Panther, put a call out for concerned individuals to come and stand in support of the black community. Within days volunteers started arriving, some of these were medical workers who established a free community health clinic in the neighborhood mosque, this eventually developed into Common Ground Health Clinic. No other aid or relief agencies came to this area. There have been a number of damning reports on the Red Cross's inadequate response to this disaster even though it received roughly 60% of the $3.6 billion that Americans donated for hurricane relief. The clinic started as a first aid station but by October 2005 it was seeing over a hundred dropins a day. The first medics to arrive discovered that the community had never had adequate healthcare and that people's poor health was exacerbated by Katrina - not caused by it. It was obvious that a permanent clinic was needed to provide healthcare for this community, particularly the uninsured. The amount of uninsured in the city dramatically increased after Katrina as so many livelihoods were lost. The main public hospital, Charity, was permanently closed down. By March 2006 the clinic had provided 10,000 free patient visits. It continued for the next 2 years to be a volunteer led clinic with nurses, physicians, herbalists, acupuncturists, EMTs, social workers and community activists coming from around the world. The main health conditions were chronic but were exacerbated by stress and post-traumatic stress disorder. There was, and still is, a crisis in mental health services in the city which has contributed to an increase in suicides. I first visited New Orleans in February 2007 for 3 months, 18 months after Katrina. The destruction was still widespread. Piles of debris lay by the roadsides. There were masses of empty houses and empty land where the houses had been destroyed. Some areas still had no electricity or water and the trauma was still felt deeply by all those that lived there. The clinic by that time had started to transition from a volunteer run clinic to employing full time staff, although all operational decisions were still made by consensus. Herbal medicine was part of treatment from very early on, partly because a nurse who was also a herbalist introduced it. There were four herbalists working as volunteers when I arrived and three are still involved today: Amy Seifert, Rachael Reeves and Wendy Hounsel. Two things made the clinic special: they provided free healthcare for people who had no other access to it and herbal medicine was offered as a choice for treatment – which is unique at a primary care level. The other incredible aspect of the clinic was its role in community organising. There was a continuous discussion about the societal factors that contributed to the ill health in that community such as systemic racism, poverty, poor housing and slum landlords and the role the clinic had in trying to challenge these. One of the first points of action was in collaboration with the People's Institute of Survival and Beyond, a 28-year-old New Orleans based anti-racist training organisation whose workshops focus on how racism was constructed and how it can be 'undone' through effective anti-racist organizing with, and in accountability to, the communities most impacted. Every person in the clinic has to go to at least one of these trainings, and the clinic also organises for members of the community to attend. The clinic has tried to remain accountable to the community in two ways. Firstly, it endeavors to have half of the board of directors formed by clinic patients who live in the community. Secondly, there are regular community meetings where patients are invited to input their opinion on the running of the clinic. The clinic is now a registered 501c3 nonprofit and has a dramatically changed structure with an executive director spearheading the organisation. It has bought a larger building and hopes to raise enough money to renovate it. The clinic is open three days a week and is currently staffed by: the nurse practitioner as the clinic manager, a volunteer doctor, two volunteer nurses, a medical office assistant, a social worker, three Spanish/Portuguese translators who also work the front desk, two community organizers, an acupuncturist, the herbalists and about six long-term volunteers who are mainly from the community. It sees around a hundred patients a week – eighty-five of whom are uninsured. The other project that runs out of the clinic is LHOP – Latino Health Outreach Programme. This is a mobile clinic that provides outreach care to the growing Latino community. Herbalism in the clinic It has been an incredible opportunity to work in this clinic and meet patients who would normally not have access to a herbalist in a primary healthcare setting. Each patient that I have seen has inspired me with their strength and resilience. Strong relationships have been built over the years with the patients and there is considerable support for herbal medicine here. We have seen positive health outcomes with many patients being able to turn their health prognosis around. Herbal consultations take an hour and there is also a nutrition class each week that every patient is invited to. As herbalists we see patients if they self refer or are referred by the physicians. Every patient has to visit the physician before any herbal consultation takes place. This can be extremely frustrating at times, but understandable in the specific situation of the clinic and Louisiana legislation. In late 2007, as the clinic became more official, the herbalists were asked to take time out and develop protocols on certain conditions that the physicians had agreed on. These protocols were basically a list of herbs that would be used to treat ten conditions. The parameters of treatment were limited and we have spent this year trying to develop more comprehensive protocols that encompass a wider scope of practice for us. Many of our patients have diabetes, hypertension and high total cholesterol but we have been unable to treat the insulin resistance - the underlying pathophysiology. Our most detailed new protocol has been for metabolic syndrome and insulin resistance. All the herbs were initially donated by herbalists from all over the States and there are still donations today. Most of the tinctures are made by the herbalists from bought dried stock or wildcrafted local plants, although this is limited as there isn't an abundance of accessible swamp herbs! Phyllis Light has been the herbalist's mentor for the last few years. I have been extremely fortunate to be able to study with her each month over the last year. Phyllis is a fourth generation herbalist from north Alabama who apprenticed with her Cherokee Grandma and the Appalachian folk herbalist Tommie Bass. The injustices suffered by the people of New Orleans continue to affect their lives and health on a daily basis. This article has only been able to introduce these issues. If you would like to read more I can recommend the following books: 'What lies beneath: Katrina, Race and the State of the Nation' by The South End Press Collective and 'Floodlines' by Jordan Flaherty. Rhizome Community Herbal Clinic takes it's inspiration from Common Ground and all the other amazing community herbal projects around the world.