PRECONCEPTION HEALTH CARE
advertisement

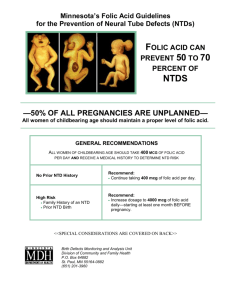
PRECONCEPTION HEALTH CARE Preconception health care is defined as the identification of conditions that could affect a future pregnancy but may be altered by early intervention with maternal lifestyle modification and improved health prior to conception. Promoting healthy lifestyles for women may be the most important factor during the preconception health planning visit in the prevention of birth defects. (Refer also to the Family Planning Section.) Components of preconception health care include the following four areas: Identification of risk factors Individualized education to meet the woman’s needs Woman’s decision to alter behavior to modify the identified risks Inclusion of the folic acid protocols Preconception assessment of risk factors and subsequent counseling is based on the medical and social history. Preconception counseling is RARELY a stand-alone service. It is usually an additional service that takes place as part of a family planning, preventive health visit, or pregnancy test visit. The following health department visits require that preconception health care be routinely provided: Initial family planning examination visit Annual family planning examination visit Initial women’s preventive health examination if of childbearing age without a permanent method of contraception (hysterectomy or tubal ligation) Pregnancy test visit (only if negative test results) All reproductive-age women, who have not had a hysterectomy, should be considered at risk for pregnancy and be advised about anticipatory activities that are important during preconception care. A detailed Hx should include information on rubella, varicella, and hepatits B immunizations. Counseling on folic acid supplementation, ATOD, appropriate nutrition and weight, genetic carrier screening (depending on the patient’s ethnicity) should also be provided. Include appropriate referrals to other health care sources as indicated by risk assessment. Women with an obstetric Hx that includes such conditions as preeclampsia, intrauterine fetal demise, intrauterine growth retardation (IUGR), recurrent elective termination of pregnancies, preterm deliveries, stillbirths, thrombophlebitis, diabetes mellitus, hypertension, or congenital malformations, should be evaluated and counseled prior to another pregnancy. Encourage women to formulate a reproductive health plan considering individual risk factors. Such a plan requires an ongoing conscientious assessment of the desirability of a future pregnancy, determination of steps that need to be taken either to prevent or to plan for a pregnancy, and evaluation of current health status and other issues relevant to the health of the pregnancy. Page 1 of 4 Kentucky Public Health Practice Reference Section: Preconception/Folic Acid July 1, 2006 PRECONCEPTION HEALTH CARE (continued) Preconception interventions may include the following: A dialogue regarding the patient’s readiness for pregnancy An evaluation of her overall health and opportunities to improve her health Education about the significant impact that social, environmental, occupational, behavioral, and genetic factors have on pregnancy Identification of women at high risk for an adverse pregnancy outcome with appropriate referrals to a health care professional Assessment and counseling should be provided only by a qualified provider who has training in medical, psychosocial, nutritional, and genetic risk identification with the ability to provide appropriate counseling and referrals. Assessment/counseling/referrals of pregnancy related risk factors include: Advanced maternal age––poses a higher risk of chromosomal abnormalities in the fetus and medical problems to the mother during pregnancy Ethnic backgrounds––a family Hx that is positive for certain diseases may indicate the need for additional screening Sexually transmitted diseases––early treatment decreases the risk of transmission to the fetus and preterm delivery Vaccination Hx (Refer to Immunizations Section) Chronic disease (hypertension, diabetes, obesity, epilepsy, DVT, depression) ATOD Domestic violence Exercise Nutrition Optimizing the health care of every woman is the ultimate goal of preconception counseling. Documentation of preconception risk assessment and counseling may be made in the CH3A notes or if provided at the time of the health examination, on the CH-13 or CH-14 by the provider who performs the counseling. Page 2 of 4 Kentucky Public Health Practice Reference Section: Preconception/Folic Acid July 1, 2006 PRECONCEPTION HEALTH CARE FOLIC ACID SUPPLEMENTATION AND COUNSELING GUIDELINES Definition: Folic acid supplementation has been shown to reduce the incidence of neural tube defects (NTD) such as spina bifida and anecephaly. Many pregnancies are unplanned and once discovered it may be too late to prevent these defects. Therefore, it is essential that all women of childbearing age consume 0.4 mg (400 mcg) of folic acid on a daily basis. This meets the RDA requirement and is recommended by the National Institute of Medicine, the Centers for Disease Control and Prevention, and the US Public Health Service. (The average woman receives about 100 mcg of folic acid per day from fortified breads and grains.) A. Determine Risk Status ASSESSMENT HIGH RISK LOW RISK RISK FACTORS Previous pregnancy with NTD Self or partner with NTD Close relative with NTD Women taking anti-seizure medication Valproic Acid (Depakote, Depacon) or Carbamazepine (Epitol, Tegretol). Women with insulin dependent diabetes mellitus (IDDM) Obese women* (exception: follow the same plan of action as low risk) None of the above identifiable risk factors are present B. Action Based On Risk Status RISK STATUS APPROPRIATE PLAN OF ACTION HIGH RISK LOW RISK Describe NTD and prevention strategies Individualized counseling/education with documentation in the medical record Discuss dietary sources of folic acid Provide education handouts If not planning a pregnancy, provide a one year supply of a multivitamin containg 0.4 mg. folic acid without iron. Discuss need for genetic counseling, medical nutrition therapy (MNT) and consultation for possible prescription levels of folic acid if a pregnancy is planned in the future. If planning a pregnancy but without a previous NTD, provide a supply of multivitamins containing 0.4 mg. folic acid without iron and promptly refer the client for genetic counseling, MNT, and consultation with a health care provider to discuss additional folic acid supplementation. If planning a pregnancy with a history of a previous NTD, provide a prescription for 4 mg (4000mcg) of folic acid to be taken daily 3 months prior to pregnancy and during the first trimester. (If patient is taking a multivitamin containing folic acid, the 4 mg. folic acid prescription level supplement should be adjusted to attain the proper dosage as prescribed per health care provider.) Also promptly refer the patient for genetic counseling and MNT. If a patient has a positive pregnancy test with a history of NTD, provide a prescription for 4 mg (4000mcg) of folic acid to be taken daily during the first trimester. If patient is taking a multivitamin containing folic acid, the folic acid prescription level supplement should be adjusted to attain the proper dosage as prescribed per health care provider. Refer promptly to a prenatal care provider, genetic counselor, and MNT. If a patient has a positive pregnancy test without a history of NTD, provide a 3 month supply of a prenatal vitamin or a multivitamin containing a minimum of 0.4 mg. folic acid approved by the Prenatal Program. (Refer to Prenatal Section.) (Note: This offering makes it possible to assure continuity of folic acid intake during the first 3 months of pregnancy; however, should only be provided with folic acid funding when a patient is unable to access the prenatal vitamins immediately through another payment source.) Assess and document consumption at each visit to the LHD. Describe NTD and prevention strategies Individualized counseling/education with documentation in the medical record Discuss dietary sources of folic acid Provide a three month supply of a multivitamin containing 0.4 mg. folic acid without iron Provide educational handouts Assess and document consumption at each visit to the LHD *Note: “Although there is now strong evidence that maternal obesity is associated with an increased risk of having offspring with neural tube defects, there is no intervention specifically aimed at obese women.” (Contemporary OB/GYN––October 1997) Page 3 of 4 Kentucky Public Health Practice Reference Section: Preconception/Folic Acid July 1, 2006 PRECONCEPTION HEALTH CARE FOLIC ACID SUPPLEMENTATION AND COUNSELING GUIDELINES (continued) C. Best Practice Facts 1. 2. 3. 4. 5. 6. 7. 8. D. Nurses (ARNP, RN, or LPN), nutritionist, dieticians, health educators and physicians may provide folic acid counseling. Assess the client’s attitude to determine if the client is a contemplator vs. a non-contemplator. Counseling should include NTD facts: Description of neural tube defects The incidence in Kentucky is 1 out of every 500 births 50% of all pregnancies are not planned NTD occurs before a pregnancy test is positive Dietary sources of folic acid and how to incorporate supplement into a daily routine Counseling sessions should be an opportunity for the client to ask questions and for the provider to assess the client’s knowledge about the health benefits of folic acid. Encourage clients to spread the word about folic acid. Provide appropriate folic acid brochure at each visit. Provide supplementation to women having tubal ligation but not hysterectomy. Provide folic acid supplements to all protocol appropriate women regardless of income eligibility and payor source. Notify the Genetic Counselor with the Kentucky Birth Surveillance Registry at 502-564-3756, extension 3768 for any woman identified as having a previous NTD delivery. Be prepared to give the name of the mother (name at time of birth) and name of affected child, stillbirth/livebirth, date of birth of affected child and delivery facility. Resources Centers for Disease Folic Acid Research Information Control and Prevention “Before You Know You’re Pregnant” Brochure in Spanish and English Atlanta, Georgia “Ready Not” Brochure in Spanish and English (770) 488-7190 CDC Folic Acid Publications Order Form Web site: http://www2.cdc.gov/ncbddd/faorder/orderform.htm Email: flo@cdc.gov Responses to questions about folic acid Frankfort Habilitation 3755 Lawrenceburg Road Frankfort, KY 40601 (502) 227-9529 FAX (502) 227-7191 “Folic Acid” – PAM-ACH 29 March of Dimes Greater Kentucky Chapter 4802 Sherburn Lane Louisville, KY 40202 (502) 895-3734 Folic Acid Research Information “Before You Know It” Promotional Material Folic Acid Resource Kit for Health Care Providers State Department for Public Health Frankfort, KY 40621-001 Folic Acid Program Coordinator (502) 564-2154, ext. 3784 Folic Acid Training Modules: http://chfs.ky.gov/dph/ Page 4 of 4 Kentucky Public Health Practice Reference Section: Preconception/Folic Acid July 1, 2006