MDR-A - Texas Department of State Health Services
advertisement
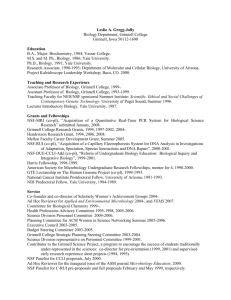
Note: Javascript is disabled or is not supported by your browser. All content is viewable but it will not display as intended. Skip to global menu 5 Skip to local menu 2 Skip to content 3 Skip to footer 6 Advanced Topics: A B C D E F G H I J K L M N O P Q R S T U V W X Y Z All Mobile | Inicio en español | Text Size: Font Larger Font Smaller Home About Us o Organization Chart o Visitor Information o Volunteer with DSHS o Site Map o o o o o o o o o o o Commissioner Legislative Information DSHS Council Advisory Committees Lists Library Resources Customer Service Contractor Resources Contracts and Budgets Data and Reports More... News o o o o Press Office News Releases News Updates I am a... o Health Professional o Public Citizen o Parent o Licensee o DSHS Contractor o eGrants User o Student o DSHS Job Applicant o News Media Representative o Government Official o More... I want to... o Prepare for an Emergency o Obtain/Renew a Professional License o Find Information About EMS o Get a Birth or Death Certificate o Get information about immunizations o Learn about WIC o Find a Mental Health Facility o Learn about funding opportunities o Learn about doing business with DSHS o Access eGrants o Search jobs o Contact Customer Service o More... Resources o Calendar of Events o o o o o o o o o Open Meetings Disease Reporting Forms and Literature Catalog Library Resources Funding Information Center Research Articles by DSHS Staff Find Services o Mental Health Services Search o Substance Abuse Services Search o DSHS Laboratory o Health Service Regions o Texas Local Public Health Organizations o Other Health Sites o Skip to content 3 IDCU HomeInfectious Diseases A-C Amebiasis Amebic Central Nervous System (CNS) Infections Anthrax Arboviral Encephalitides Avian Flu Botulism Brucella (Brucellosis) Campylobacteriosis Carbapenem-Resistant Enterobacteriaceae (CRE) Chagas Disease Chickenpox (Varicella) Chikungunya Virus Cholera Chronic Wasting Disease Clostridium difficile (C. diff) Coccidioidomycosis Congenital Rubella Syndrome Coronavirus, novel Creutzfeldt-Jakob Disease (CJD) Cryptosporidiosis Cyclospora D-G Dengue Fever & DHF Diphtheria Ebola Echinococcosis Ehrlichiosis Encephalitides, Arboviral Encephalitis,Bacterial or Viral E.coli O157:H7 Flu Gastroenteritis (Foodborne Illness) H-L Haemophilus influenzae Type b (Hib) Hansen's Disease (Leprosy) Hantaviruses Hepatitis A,B,C & E Hepatitis A Hepatitis B Hepatitis C Hepatitis E HIV Impetigo Influenza Influenza-associated pediatric mortality Legionellosis Leishmaniasis Leptospirosis Listeriosis Lyme Disease M-Q Malaria MDR-A (Multi-drug resistant Acinetobacter) Measles Meningitis Meningococcal Invasive MERS (Coronavirus, novel) MRSA Mumps Murine Typhus Pertussis Plague Polio Primary Amebic Meningoencephalitis Psittacosis Q Fever R-S Rabies Respiratory Syncytial Virus Rocky Mountain Spotted Fever Rubella Salmonellosis SARS (Coronavirus, novel) Shigellosis Smallpox Staphylococci Streptococci (Strep - Group A & B, S.Pneumo) T-Z Taeniasis Tetanus Tick Borne Diseases Toxoplasmosis Trichinosis Tuberculosis (TB) Tularemia Typhoid Fever Typhus Vibrio Infections West Nile Yellow Fever VISA/VRSA Zika IDCU Health Topics Animal Control Officer Training Animal Control & Shelters Animal in Disasters Animals in Public Places Annual Report Antibiotic Resistance (CRE, MDRO, MRSA, VRE & VRSA) Bloodborne Pathogens Contaminated Sharps Injury Education, Professional Envenomization Foodborne Illness Health Care Associated Infections (HAI) Health Care Safety Historical Data Infection Prevention Infectious Disease International Travel Investigation Guidance Lab Tests/Specimen Submission Instructions Laboratory Tests for Diseases and Agents Management of Occupational Exposure to Blood/Body Fluids Oral Rabies Vaccine Programs Outdoor Health and Safety Pet Ownership Preventable Adverse Events Rabies Schools & Child-Care Centers Tick Borne Diseases Vaccine Preventable Diseases Veterinarian Information Waterborne Diseases Zoonotic Diseases Zoonotic Health Topics Disease Reporting Disease Reporting Contacts Notifiable Conditions Investigation and Surveillance Forms Reporting Forms Lab Test/Specimen Submission Laboratory Tests for Diseases and Agents Laboratory Reporting Veterinary Reporting Epi Case Criteria (PDF) Blood Lead Level Reporting Cancer Reporting Contaminated Sharps Injury Electronic Reporting (NEDSS) HIV/STD Reporting TB Forms Related Rules & Regulations Notifiable Conditions Communicable Disease Control Measures Texas Administrative Code Impoundment Facilities Veterinary Responsibilities in Disease Reporting Animal Import and Export Requirements Statewide Wild Animal Transport Restrictions Pet Vaccine Requirements and Protocol Animal Shelters Rabies Quarantine and Impoundment Facilities Local Animal Control Regulations Pet Stores and Salmonellosis Acquired from Reptiles Dangerous Wild Animals (bears, lions, tigers, chimpanzees) Immunization BranchAbout IDCU Unit Mission Statement Unit Overview & Branch Information Related Branches, Sections, and Units Texas Health Service Regions Related DSHS Sites Community Preparedness Section Regional Epidemiological Response Teams Immunization Branch Laboratory Services Section Public Health Preparedness Staff Contact List Call List of Diseases Contact Us Infectious Disease Control Unit Mail Code: 1960 PO BOX 149347 - Austin, TX 78714-9347 1100 West 49th Street, Suite T801 Austin, TX 78714 Phone: 512 776 7676 Fax: (512) 776-7616 E-mail Home > Infectious Disease Control > MDR-A MDR-A Last updated December 08, 2015 Contact Us | Visitor Information | Site Map | Search | Topics A-Z | Compact with Texans | File Viewing Information Internet Policy | HHS Agencies | Homeland Security | Statewide Search | Texas.gov | Privacy Practices Health Care Safety Home AR/MDROs Home Investigation Reporting Organisms, Causative Agent, or Etiologic Agent Multi-drug Resistant Acinetobacter (MDR-A) The term MDR-A stands for multi-drug resistant Acinetobacter. Acinetobacter species are gram negative bacteria and have more than 25 types or species under its genus name, such as Acinetobacter baumannii. These bacteria c have a built-in resistance factor enabling them to be resistant to the antibiotics called carbapenems and penicillins. There are several ways Acinetobacter can be nonsusceptible to antibiotics, but no matter the mechanisms when an Acinetobacter species carries this resistance we refer to the bacteria as multi-drug resistant Acinetobacter or MDR-A. Transmission Acinetobacter species have been found in soil, water, animals and humans. In humans, it has been isolated from t skin, throat and rectum, and has been reported to be a colonizer of the respiratory tract in health care settings. Be a carrier of a bacterium without any symptoms or infection is known as being “colonized”. The germ is spread through contact. This contact can be either direct person-to-person contact or secondary contact with contaminate environmental surfaces, medical devices, or equipment. For example, a healthcare worker may touch an infected person or soiled equipment and not clean their hands before touching the next patient or patient equipment. Symptoms Acinetobacter can cause many types of infections, such as pneumonia, urinary tract infections, and bloodstream infections. When the same infection is caused by MDR-A the infections are harder to treat because the bacteria a very resistant to antibiotics. An individual can also be a colonized with Acinetobacter and have no symptoms. Prevention Generally, MDR-A affects people with underlying medical problems such as diabetes or a weakened immune sys and rarely occurs outside of health care facilities. There are many prevention measures you can put in place early to help lessen your chance of getting MDR-A. Maintain your health now so that you lessen your chance of having to be in healthcare facilities when you older, this includes limiting high risk behaviors. A few examples of high risk behaviors are substance abu riding without a helmet, violence, and unprotected sex. When you are prescribed antibiotics take all that come in the package, take them as listed on the instructio If you do not understand the instructions, ask your pharmacist. Do not share or save antibiotics. Do not st taking the antibiotics even if you feel better;, finish all the antibiotics you are prescribed. Ensure cleanliness and appropriate disinfection. o When you visit health care facilities wash or sanitize your hands frequently and ask others to do th same before having contact with you or your belongings. o If you are hospitalized, ask if your room has been disinfected each day and ask for equipment to b disinfected before it used on you. o For the two items mentioned above, don’t be afraid to ask the hospital staff each time to have clea hands or to make sure equipment is disinfected. It can be scary to ask them but you want to make they are doing their best job. You can also visit a patient safety foundation or patient advocacy gro for tips on things to look out for during your hospital stay. One example of a patient advocacy gro is Louise H. Batz Foundation, you can visit their website at www.louisebatz.org If you or someone you know is hospitalized, stay involved in the health care process. If you have an indwelling device, ask daily about when it can be removed. Examples of indwelling devices: surgical drai central venous catheter, dialysis lines, PICCs, urinary catheter, tracheostomy tube and ventilator. School Exclusion MDR-A infections are rare in children. Unless directed by a physician, students with any type of MDR-A wound infection need to be excluded from attending school until drainage from wound or skin and soft tissue infection i contained and maintained in a clean, dry bandage. Restrict a child from activity that could result in the infected a being touched by others or becoming exposed, wet, soiled, or otherwise compromised. Texas Trends Multi-drug resistant Acinetobacter has been found in Texas. The prevalence of MDR-A is currently unknown. B on the 2012 Texas Annual Report on Health care-associated Infections Overall Antibiogram, antibiotic sensitivit for Acinetobacter baumannii ranged from 36% susceptible (Imipenem) to 70% Tetracycline.