ACINETOBACTER Chelsey Schaplow, Kristen Slodysko, Kelsey Cardner, Megan Stewart
advertisement
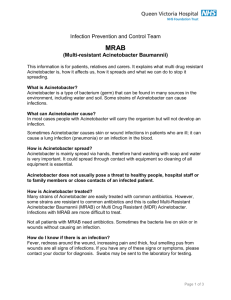
ACINETOBACTER Chelsey Schaplow, Kristen Slodysko, Kelsey Cardner, Megan Stewart Acinetobacter Acinetobacter [asz−in−ée−toe–back−ter] is a group of bacteria commonly found in soil and water. Outbreaks of Acinetobacter infections typically occur in intensive care units and healthcare settings housing very ill patients. While there are many types or “species” of Acinetobacter and all can cause human disease, Acinetobacter baumannii [asz−in−ée−toe–back−ter bō–maa–nee–ie] accounts for about 80% of reported infections. Acinetobacter infections rarely occur outside of healthcare settings. Common in military settings? Reservoir: soil and water. Acinetobacter can live on the skin and may survive in the environment for several days. Careful attention to infection control procedures, such as hand hygiene and environmental cleaning, can reduce the risk of transmission. Portals of entry and exit: Acinetobacter can be spread to susceptible persons by person-to-person contact or contact with contaminated surfaces. (Direct and indirect via fomites) Diseases: Acinetobacter causes a variety of diseases, ranging from pneumonia to serious blood or wound infections, and the symptoms vary depending on the disease. Acinetobacter may also “colonize” or live in a patient without causing infection or symptoms, especially in tracheostomy sites or open wounds. Symptoms: dependent of diseases caused How transmitted in healthcare setting: Outbreaks of Acinetobacter infections typically occur in intensive care units and healthcare settings housing very ill patients. Acinetobacter infections rarely occur outside of healthcare settings Acinetobacter poses very little risk to healthy people. However, people who have weakened immune systems, chronic lung disease, or diabetes may be more susceptible to infections with Acinetobacter. Hospitalized patients, especially very ill patients on a ventilator, those with a prolonged hospital stay, those who have open wounds, or any person with invasive devices like urinary catheters are also at greater risk for Acinetobacter infection. Acinetobacter can be spread to susceptible persons by person-toperson contact or contact with contaminated surfaces. Morbidity/ Mortality: Although Acinetobacter is primarily a colonizer in the hospital environment, it occasionally causes infection. Mortality and morbidity resulting from A baumannii infection relate to the underlying cardiopulmonary immune status of the host rather than the inherent virulence of the organism. Mortality and morbidity rates in patients who are very ill with multisystem disease are increased because of their underlying illness rather than the superimposed infection with Acinetobacter. Additional information: Acinetobacter is often resistant to many commonly prescribed antibiotics. http://www.cdc.gov/HAI/organisms/acinetobacter.html http://www.cdc.gov/hai/organisms/organisms.html#a http://emedicine.medscape.com/article/236891-overview#a0199 Acinetobacter Alicia Brannan, Chris Gunnink, Fary Mirzaee, Terri Dakin-Dodge Acinetobacter [asz−in−ée−toe–back−ter] is a group of bacteria commonly found in soil and water. While there are many types or “species” of Acinetobacter and all can cause human disease, Acinetobacter baumannii accounts for about 80% of reported infections. Outbreaks of Acinetobacter infections typically occur in intensive care units and healthcare settings housing very ill patients. Acinetobacter infections rarely occur outside of healthcare settings. Bacteria or Virus? Acinetobacter is a group of bacteria commonly found in soil and water. Reservoir of infection for this microbe? Acinetobacter often live in a patient without causing infection or symptoms, especially in tracheostomy sites or open wounds. Acinetobacter can also be found in soil and water. Portal of entry/exit? However, people who have weakened immune systems, chronic lung disease, or diabetes may be more susceptible to infections with Acinetobacter. Hospitalized patients, especially very ill patients on a ventilator, those with a prolonged hospital stay, those who have open wounds, or any person with invasive devices like urinary catheters are also at greater risk for Acinetobacter infection. Acinetobacter can be spread to susceptible persons by person-to-person contact or contact with contaminated surfaces. What diseases does it cause? Acinetobacter causes a variety of diseases, ranging from pneumonia to serious blood or wound infections, and the symptoms vary depending on the disease. This bacteria can also cause urinary tract infections but these infections are indistinguishable from other bacteria causing UTIs. What are the symptoms of the disease? Symptoms may vary depending on the disease. For pneumonia symptoms may include coughing, fever, fatigue, nausea, vomiting, rapid breathing or shortness of breath, chills, or chest pain. http://www.cdc.gov/Features/Pneumonia/ How is your microbe transmitted in a healthcare setting? However, people who have weakened immune systems, chronic lung disease, or diabetes may be more susceptible to infections with Acinetobacter. Hospitalized patients, especially very ill patients on a ventilator, those with a prolonged hospital stay, those who have open wounds, or any person with invasive devices like urinary catheters are also at greater risk for Acinetobacter infection. Acinetobacter can be spread to susceptible persons by person-to-person contact or contact with contaminated surfaces. All the above information taken from http://www.cdc.gov/HAI/organisms/acinetobacter.html Nick Collins-Feay & Kelli Moseley & Lyndsay Dicus & Melissa Bennett BIO 260 – HAI In class research Burkohlderia Cepacia Burkholderia cepacia [burk-hōld–er–ee-uh si−pay−shee−uh] is the name for a group or "complex" of bacteria that can be found in soil and water. Burkholderia cepacia bacteria are often resistant to common antibiotics. Burkholderia cepacia poses little medical risk to healthy people; however, it is a known cause of infections in hospitalized patients. People with certain health conditions, like weakened immune systems or chronic lung diseases (particularly cystic fibrosis), may be more susceptible to infections with Burkholderia cepacia. [Burkholderia cepacia is also called B. cepacia Taken from: http://www.cdc.gov/hai/organisms/organisms.html#b 1. Bacteria 2. Soil and water 3. Transmission of B. cepacia from contaminated medicines and devices has been reported.. B. cepacia can also be spread to susceptible persons by: Person-to-person contact, contact with contaminated surfaces, exposure to B. cepacia in the environment. Also: oral, injection site. (from: http://www.cdc.gov/HAI/organisms/bCepacia.html) 4. Once B. cepacia enters the body, there are three possible effects and it is not possible to predict which will happen. Sometimes B. cepacia colonizes in the lungs, causes no symptoms, and has no long term effect. Other times B. cepacia colonizes in the lungs and causes damaging lung infections and inflammation that lead to a slow deterioration of lung function. In the worst case scenario, B. cepacia can spread throughout the body causing “cepacia syndrome”, which leads to a rapid deterioration of lung function. Cepacia syndrome is a serious condition that does not always respond well to treatment. Unfortunately, even with proper treatment, cepacia syndrome can lead to death within a few weeks.The effects of B. cepacia on people vary widely, ranging from no symptoms at all to serious respiratory infections, especially in patients with cystic fibrosis. (from: http://cysticfibrosis.about.com/od/relateddiseases/tp/bcepacia.htm 5. (from: http://www.cdc.gov/HAI/organisms/bCepacia.html) 6. Transmitted in a healthcare setting by person to person (direct) contact, as well as fomites (contaminated surfaces or equipment) 7. Morbidity & Mortality: at risk populations include patients with cystic fibrosis, pre-existing lung infections, and immune compromised individuals. “The overall 28-day mortality rate was 41% (11/27). In univariate analysis, underlying diabetes mellitus (p = 0.033), inappropriate initial empirical antimicrobial therapy (p = 0.033), and an elevated Sequential Organ Failure Assessment (SOFA) score (p = 0.002) were significantly associated with mortality. In multivariate analysis, inappropriate initial empirical antimicrobial therapy and an elevated SOFA score were independent risk factors for increased mortality (p = 0.032 and p = 0.028, respectively).” (from: http://www.ncbi.nlm.nih.gov/pubmed/21888567 Burkhaolderia Cepacia - - - Maria Peletskaya Margaret Huisinga Lucy Kinsey Salome Abaata Water and soil and infected plants & people (hosts) are reservoirs of this antibiotic-resistant bacteria. Persons with weakened immunity or respiratory conditions are particularly susceptible to respiratory infection from B. cepacia. http://www.cdc.gov/HAI/organisms/bCepacia.html Portal of entry o Skin, mouth, injection site Portal of exit o Contaminated medical devices, sublingual probes, area of dermal contact Symptoms o The effects of B. cepacia on people vary widely, ranging from no symptoms at all to serious respiratory infections like pneumonia, especially in patients with cystic fibrosis. How is the microbe transmitted in a healthcare setting? o Person-to-person contact o Contact with contaminated surfaces o Exposure to B. cepacia in the environment o contaminated medicines and devices, including mouthwash and nasal spray. Mortality: There is a high mortality rate in patients infected with Burkholderia cepacia. Many develop what is known as cepacia syndrome. This is a fatal necrotizing pneumonia that is currently untreatable. (http://microbewiki.kenyon.edu/index.php/Burkholderia_cepacia)\ Interesting Facts: “An organism that reduces an onion to a macerated pulp, protects other crops from bacterial and fungal disease, devastates the health and social life of cystic fibrosis patients, and not only is resistant to the most famous of antibiotics, penicillin, but can use it as a nutrient!" (J. R. W. Govan, 1998) C DIFF Jennifer Honda and Brian Iversen Clostridium difficile is a spore-forming, Gram-positive anaerobic bacillus that produces two exotoxins: toxin A and toxin B. It is a common cause of antibiotic-associated diarrhea (AAD). It accounts for 15-25% of all episodes of AAD. http://www.cdc.gov/HAI/organisms/cdiff/Cdiff_faqs_HCP.html#a1 What diseases result from Clostridium difficile infection? pseudomembranous colitis (PMC) toxic megacolon perforations of the colon sepsis death (rarely) What are the main clinical symptoms of Clostridium difficile infection? Clinical symptoms include: watery diarrhea fever loss of appetite nausea abdominal pain/tendernes How is Clostridium difficile transmitted? Clostridium difficile is shed in feces. Any surface, device, or material (e.g., commodes, bathing tubs, and electronic rectal thermometers) that becomes contaminated with feces may serve as a reservoir for the Clostridium difficile spores. Clostridium difficile spores are transferred to patients mainly via the hands of healthcare personnel who have touched a contaminated surface or item. Clostridium difficile can live for long periods on surfaces. Clostridium difficile infection (CDI) often occurs in patients in health-care settings, where antibiotics are prescribed and symptomatic patients, an important source for transmission, are concentrated. From 2000 to 2009, the number of hospitalized patients with any CDI discharge diagnoses more than doubled, from approximately 139,000 to 336,600, and the number with a primary CDI diagnosis more than tripled, from 33,000 to 111,000. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6109a3.htm The incidence, mortality, and medical care costs of CDIs have reached historic highs (1,3,9,10). The estimated number of deaths attributed to CDI, based on multiple cause-of-death mortality data, increased from 3,000 deaths per year during 1999–2000 to 14,000 during 2006–2007, with more than 90% of deaths in persons aged ≥65 years (10). http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6109a3.htm?s_cid=mm6109a3_w Clostridium Dificile Diana, Adrian, Karina, Suzie http://www.cdc.gov/HAI/organisms/cdiff/Cdiff_infect.html http://www.phac-aspc.gc.ca/id-mi/cdiff-eng.php When antibiotics destroy a person's good bowel bacteria, C. difficile bacteria can grow. When this occurs, the C. difficile bacteria produce toxins, which can damage the bowel and cause diarrhea. However, some people can have C. difficile bacteria present in their bowel and not show symptoms. 1. http://www.mayoclinic.com/health/c-difficile/DS00736 Clostridium difficile (klos-TRID-e-um dif-uh-SEEL), often called C. difficile or C. diff, is a bacterium that can cause symptoms ranging from diarrhea to life-threatening inflammation of the colon. 2. http://www.azdhs.gov/phs/oids/epi/disease/cdif/documents/CDADforLTCFs.pdf Reservoir: The two major reservoirs of C. difficile are colonized or infected persons and contaminated environments. C. difficile spores can survive for weeks to months on environmental surfaces. Any surface, device or material (e.g. commodes, bathing tubs, and electronic rectal thermometers) that becomes contaminated with infectious feces may serve as a reservoir for the C. difficile spores. 3. The bacteria are found in the feces. People can become infected if they touch items or surfaces that are contaminated with feces and then touch their mouth or mucous membranes 4. http://www.medicinenet.com/clostridium_difficile_colitis/article.htm the bacterium that causes an inflammation of the colon; this condition is called colitis 5. http://www.cdc.gov/HAI/organisms/cdiff/Cdiff_excerpt.html The degree to which the environment becomes contaminated with C. difficile spores is proportional to the number of patients with C. difficile-associated diarrhea, although asymptomatic, colonized patients may also serve as a source of contamination. 6. Transmitted in healthcare setting: Healthcare workers can spread the bacteria to patients or contaminate surfaces through hand contact 7. Mortality: C. difficile causes diarrhea linked to 14,000 American deaths each year. Student Names: Lucas Metzger Kevin Holte Amanda Rimmer Leanna Hawkins Verena Aziz Researching HIAs Microbiology, Biology 260 September 24, 2013 Clostridium sordellii A rare bacterium that causes pneumonia, endocarditis, arthritis, peritonitis, and myonecrosis Bacteria Reservoirs of Infection--It is not known how C. sordellii is spread between persons or from the environment to persons but originates from people. Portal of Entry/Exit—Direct, Sexual, Fecal-Oral, Possible Droplet Diseases it Causes-- pneumonia, endocarditis, arthritis, peritonitis, and myonecrosis. Symptoms--nausea, vomiting, diarrhea, and sometimes abdominal pain without fever. How transmitted-- spread from person to person and sometimes contaminated surfaces are involved in this transmission. Tests performed by the Food and Drug Administration (FDA) have not detected contamination with C. sordellii of either of the medications used in medical abortions. Mortality:100% Mortality Rate with pregnant women and their newborns Websites Used: http://www.cdc.gov/HAI/organisms/cSordellii.html www.ncbi.nlm.nih.gov/pmc/articles/PMC2805323/ Hazel Utevsky, Allison Griffing, wosenyelsh abebe, Dersane sahlu Hepatitis B It is a virus called HBV. There is no cure but there is a vaccination. The reservoirs are humans. It is transmitted by blood and body fluids. Usually transmitted by direct exposure to blood or body fluids, via sexual intercourse or needle stick in a healthcare setting. It is considered a sexually transmitted disease. Symptoms include abdominal pain, dark urine, fever, joint pain, loss of appetite, nausea, vomit, weakness, fatigue, jaundice. Causes liver disease, liver failure, cirrhosis (scarring) of liver, lifelong infection, and death. Resources from: http:/www.cdc.gov/HAI/organisms/organisms.html Lauren Ewing Elliot Novak Evi Riveria Jennifer Yee Researching HAIs 10am Klebsiella Gram negative Bacteria Reservoir- Human body Portal- respiratory system and bloodstream, intestines (fecal-oral) Disease- pneumonia, blood infections, and meningitis. Liver abscess (UW Medicine) Symptoms- Pneumonia -high fever, chills, and cough with bloody sputum Meningitis- nausea, vomiting, altered mental status Liver abscess- weight loss, anorexia, shortness of breath This microbe is transmitted in a Healthcare setting the most by ventilators, catheters, and IV ports. If a healthcare worker visits patients without washing hands (direct contact) there is a much higher risk of spreading the disease. It is most common for a person with a lowered immune system to get infected with klebsiella. http://www.cdc.gov/HAI/organisms/klebsiella/klebsiella.html#a5 http://emedicine.medscape.com/article/219907-clinical http://ncbi.nlm.nih.gov/pmc/articles/pmc548117 Methicillin-resistant Staphylococcus aureus (MRSA) -Ky Cooper, Naeimeh Bagheri, Sitom Habte Methicillin-resistant Staphylococcus aureus (MRSA) is a type of staph bacteria that is resistant to certain antibiotics called beta-lactams. These antibiotics include methicillin and other more common antibiotics such as oxacillin, penicillin, and amoxicillin. In the community, most MRSA infections are skin infections. More severe or potentially life-threatening MRSA infections occur most frequently among patients in Healthcare Settings. [Methicillin-resistant Staphylococcus aureus is also called MRSA] http://www.cdc.gov/HAI/organisms/organisms.html#m 1. MRSA is a bacteria 2. Diseases and symptoms - MRSA can cause skin or wound infections, pneumonia and blood infections. Symptoms of these diseases can include chills fever, swollen rash, infected wounds emitting puss, and coughing shortness of breath. “This germ does not cause any problems for most people who have it on their skin. But someimes it can cause serious infections such as skin or wound infections, pneumonia, or infections of the blood.” http://www.cdc.gov/mrsa/pdf/SHEA-mrsa_tagged.pdf Often, people first think the area is a spider bite; however, unless a spider is actually seen, the irritation is likely not a spider bite. Most staph skin infections, including MRSA, appear as a bump or infected area on the skin that might be: Red, Swollen, Painful, Warm to the touch, Full of pus or other drainage, Accompanied by a fever http://www.cdc.gov/mrsa/community/index.html#q4 3. Portal of entery/exit and reservoirs of infection - MRSA can be passed by direct contact using the skin as a portal of exit and entry. MRSA can also be passed by indirect contact via numerous fomites usually equipment or furniture in hospitals and healthcare settings. The reservoirs of infection for MRSA include the infected person, skin of humans and numerous environmental reservoirs within healthcare settings. “People who have MRSA germs on their skin or who are infected with MRSA may be able to spread the germ to other people. MRSA can be passed on to bed linens, bed rails, bathroom ixtures, and medical equipment. It can spread to other people on contaminated equipment and on the hands of doctors, nurses, other healthcare providers and visitors.” http://www.cdc.gov/mrsa/pdf/SHEA-mrsa_tagged.pdf Bret Lucero Kristin Jue Abby deLa Cruz Rahel Mekonnen Nguyet Nguyen Micro 260 12-2:50 Enterobacteriaceae (carbapenem-resistance) E-coli • Briefly describe your microbe and the disease(s) that it cause. E-coli Escherichia coli (E. coli) bacteria normally live in the intestines of people and animals. Most E. coli are harmless and actually are an important part of a healthy human intestinal tract. However, some E. coli are pathogenic, meaning they can cause illness, either diarrhea or illness outside of the intestinal tract. o Bacteria or virus? Bacteria o What is/are the reservoir(s) of infection for this microbe?. live in the intestines of people and animals o What is the portal of entry and portal of exit for this microbe? The types of E. coli that can cause diarrhea can be transmitted through contaminated water or food, or through contact with animals or persons o What disease(s) does it cause? Shiga Toxin producing pathogenic E. coli, UTI, respiratory illness o What are some symptoms of the disease(s)? bloody diarrhea, nausea vomiting, fever, abdominal pain • How is your microbe transmitted in a healthcare setting? Bathroom, lack of hand washing, ignoring universal precautions, food handling • Optional: Can you find any information on the morbidity and/or mortality caused by this microbe in healthcare settings? Depends of what strain of E.coli is detected. O157 strain can cause liver and kidney failure, more deadly if children are exposed. http://www.cdc.gov/ecoli/general/index.html#soon_symptoms Enterobacteriaceae (carbapemem-resistance): E.coli (Escherichia coli) Mara Willaford, Sara Alzeer, Tiffany Short, Soledad Picon Bacteria or virus? There are both Bacterial strains, as well as viral strains. E-coli has What are the reservoirs of infection for this microbe? Animals and People. What is the portal of entry and portal of exit for this microbe? Fecal-oral. What disease(s) does it cause? We’re not sure! We know that it is linked to gastroenteritis, urinary tract infections, and neonatal meningitis. We believe that certain strains may cause disease but we’re not sure about bacterial vs. viral. What are some symptoms of the disease(s)? Stomach cramps, vomiting, diarrhea, and sometimes low fever. How is the microbe transmitted in a healthcare setting? If water was contaminated, improper food handling or prep, not properly washing hands. Optional: In healthcare settings, CRE infections most commonly occur among patients who are receiving treatment for other conditions. Patients whose care requires devices like ventilators (breathing machines), urinary (bladder) catheters, or intravenous (vein) catheters, and patients who are taking long courses of certain antibiotics are most at risk for CRE infections. Why are patients who are taking long courses of antibiotics more at risk? Recourses used : http://en.wikipedia.org/wiki/Escherichia_coli http://www.who.int/mediacentre/factsheets/fs125/en/ http://www.cdc.gov/ecoli/