Locality Planning Q and A - Shetland Islands Council
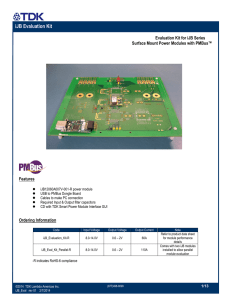
advertisement
Question and Answer Session from Localities Seminar Strategic commissioning and Locality Planning Q&A Q) Is the strategic Planning Group made up of IJB members ie a sub-group? A) It is up to IJB to decide, the membership is prescribed but could be same individuals as on IJB. Eg user / carer representatives or different folk. We have done preparatory work to set out what the options are and what we think might work, so that the IJB can hit the ground running, but it will be the IJB's job to establish the Strategic Planning Group, approve the plan for this year, and develop the plan for next year so that we take account of locality needs and strategic needs assessment. Q) What is meant by 'providers' for strategic planning group? A) We don't have a private health or care sector in Shetland, although we have an active Voluntary sector. 'Providers' are all those delivering services, including LA / NHS / Jointly managed services, and third sector provided services, and private sector. Q) If this is about change to improve things, what difference will IJB have made in a year's time? A) The difference should be related to health & well being outcomes, eg. preventing unnecessary hospital admissions by changing the care we can provide in the community to prevent an admission. Q) If this is to happen, will it require more funding eg in to community, and where will that money come from? A) The answer may be about more funding, which will require decisions about priorities and savings elsewhere. It may be also be about using current resources differently. This will be part of the role of the IJB. It will also be to challenge and inform policy decisions of SIC or NHS. Example given by a member of staff was of a cancer patient, at end of life, at home who could have been cared for in a care home, but admission was controlled by specific Social Worker and duty out of hours service couldn't give this permission, might have led to an unnecessary hospital admission if not resolved, so solution can be more about working together differently to solve problems rather than new investment. Q) Localities (communities) may be interested in very different issues than health & social care, how wide will this go? A) The context is community planning, but focus is health & social care, so other issues need to be signposted to the appropriate service. Plan is to do this jointly with colleagues in community planning and development team, so that hopefully it can develop into continuing conversations with communities on their own priorities. Q) What will you do if no-one comes to a locality meeting? A) Will start with core staff - GP, care home / care at home manager, community nursing, health improvement, plus local Councillors, invite Community council reps, and then see where the local group wants to take things. Can then offer support to take forward specific local issues, to feed other issues into relevant service, develop so that the relevant people come together to deal with the relevant issue, involving wider community / other individuals / groups as and when appropriate. 1 Q) What will you do where there are more than one GP practice / community council in one locality? A) Start by inviting them all in (not all community council members, but a rep from each one), and then see where we can find common interest, or opportunities for joint working. Localities Service Delivery and IRISS Feedback Q's & A’s Q) 2 pilot areas - did people in localities know about the work? A) Deliberate decision to start with staff and then be able to take issues into locality – we see Locality planning as the route for this. At one of the Unst sessions there were some local people there. Q) Emphasis on starting where staff already are is very important. What will some of the intended hard outputs - what will be seen to be different? A) Multidisciplinary discussion and response rather than seeing separate professionals at different times. Q) Will it test accountabilities and more delegated responsibilities. The comment raised earlier by a member of staff regarding Social Work. Linking to the trust and permission element? A) Yes, and reinforcing / strengthening things already in places but not well delivered eg A care centre manager already has the responsibility for admitting a palliative care patient, but perhaps staff need to be reminded of that and build on existing processes that are already in place. Q) How are we going to create a sense of newness, feeling of autonomy to make decisions? A) Start as we mean to go on, accountability, visibility of IJB, give people the confidence, regular attention and prompting - why do we do things this a particular way, why do you need permission? What for? What will it take to change? Q) Have we measured the cost of the baseline of where we are now? A) Doing things with people in the right way and people using services feeling the benefit A) Do need good enough financial information, but it would be a mistake to simply focus on financial baseline to measure success. Should be measuring outcomes and be able to show where we're achieving improvement in outcomes - quantifiable and narrative. Need to be clear about what we are aiming to achieve and whether we have been successful - holding to account and IJB showing measures of success. I.e more freeing up staff time to work in preventative areas of work could be a seen as success. We must move from crisis to prevention. The outcome would be that we have fewer crisis. Should spend more time on what we are trying to achieve rather than the minutia of financial information because you can do that forever and not make a difference. Q) yes but surely we must supply the narrative for evidence whether that be outcome based or financial. A) Agreed 2 Comment that named person mustn't be at the expense of shared responsibility - if the named person is on holiday, can't use that as an excuse for everyone else to disown the problem. A) Agreed there needs to be a culture of shared responsibility. Q) Within localities where does dementia care fit? A) The ideal would be that people with dementia would be cared for within localities, as many are now, staff with additional expertise need to relate to localities through named responsible person linking into each Locality. Need to develop and extend current skills amongst staff to make sure that appropriate care can be delivered as close to home as possible, supported by more specialist skills in some staff in the specialist team. Management in localities Q&A Q) Comment about barriers of different patient and client records so information held in lots of different places (in example of who to contact to organise services around an individual patient). How will this work in practice, How do we break down the barriers. Challenge about leadership within localities to drive change as well as coordinate care. A) You face barriers in the best systems. We won’t solve all the IT issues immediately, so will have to work with what we have got in the first instance but make that work better. We need clear leadership in localities and clear pathways. Do we make accountability work across professional and service boundaries, how do we design this so that people make decisions across organisational boundaries? Q) How much is your thinking shaped by the thoughts of the people on the ground as local communities can be really useful at helping to challenge the ‘status quo’. Also wondered whether there are existing national models so that people can be clear about the options on management and shared responsibilities? A) There are different models elsewhere, aware of Orkney experience, which has had successes and challenges, need more engagement locally to come up with local arrangements. Q) Why are we not using better IT methods, this may solve some of the problems? Rather than multiple phone calls to fix a problem, send one e-mail which arrives at multiple destinations or one message which arrives at multiple destinations? A) Yes, investment in IT may support staff in real time. Though often it's about staff involvement and building or tweaking systems and how they are used. The need is to understand what IT systems are needed for and how to make best use of them. Often it is about information governance. Comment – One of the many points IRISS raised was around our shared Vision and lack of clarity for practitioners. If the only reason we are doing this is because it's statutory then that isn't going to improve outcomes. Where we have joined up eg on training we have identified outcomes and identified the 'tree of responsibility', identifying actions and allocating work (decomposition of outcomes) - could fairly quickly do work to get on with the localities work. 3 Comments on medicines reconciliation as an example of something that is more complex than you first think, but if we could get that sorted it would make a real difference. For example 20% of hospital admissions are due to medicine problems. If we could get that one problem sorted collectively, that would be a huge success. A) Lots of ideas about practical things that could be sorted that would make things easier for staff working on the ground. Themes from post-its: - community engagement - risks that one organisation will take over another, balance of power between organisations - more info about IJB role and responsibilities - how to engage and support staff - staff as the biggest asset - Q about how to get staff rep into strategic Planning Group - what about equity across localities and equity of outcomes - resources - recognition of pressures on resources and avoiding duplication 4