OUTLINE
I. Case Based
Introduction
Web Based Education Module 4: “Doc, I’m Tired and Have Little Energy”
FINAL DRAFT - CORE CONTENT
CONTENT
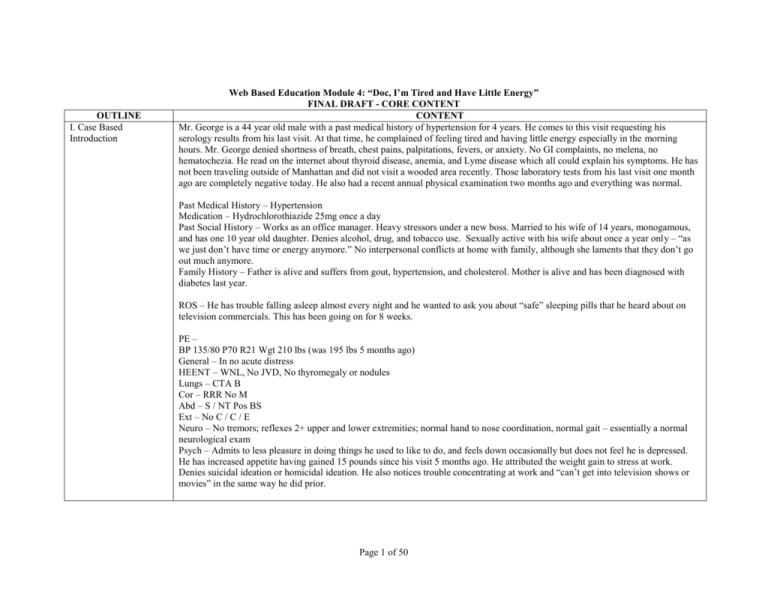
Mr. George is a 44 year old male with a past medical history of hypertension for 4 years. He comes to this visit requesting his
serology results from his last visit. At that time, he complained of feeling tired and having little energy especially in the morning
hours. Mr. George denied shortness of breath, chest pains, palpitations, fevers, or anxiety. No GI complaints, no melena, no
hematochezia. He read on the internet about thyroid disease, anemia, and Lyme disease which all could explain his symptoms. He has
not been traveling outside of Manhattan and did not visit a wooded area recently. Those laboratory tests from his last visit one month
ago are completely negative today. He also had a recent annual physical examination two months ago and everything was normal.
Past Medical History – Hypertension
Medication – Hydrochlorothiazide 25mg once a day
Past Social History – Works as an office manager. Heavy stressors under a new boss. Married to his wife of 14 years, monogamous,
and has one 10 year old daughter. Denies alcohol, drug, and tobacco use. Sexually active with his wife about once a year only – “as
we just don’t have time or energy anymore.” No interpersonal conflicts at home with family, although she laments that they don’t go
out much anymore.
Family History – Father is alive and suffers from gout, hypertension, and cholesterol. Mother is alive and has been diagnosed with
diabetes last year.
ROS – He has trouble falling asleep almost every night and he wanted to ask you about “safe” sleeping pills that he heard about on
television commercials. This has been going on for 8 weeks.
PE –
BP 135/80 P70 R21 Wgt 210 lbs (was 195 lbs 5 months ago)
General – In no acute distress
HEENT – WNL, No JVD, No thyromegaly or nodules
Lungs – CTA B
Cor – RRR No M
Abd – S / NT Pos BS
Ext – No C / C / E
Neuro – No tremors; reflexes 2+ upper and lower extremities; normal hand to nose coordination, normal gait – essentially a normal
neurological exam
Psych – Admits to less pleasure in doing things he used to like to do, and feels down occasionally but does not feel he is depressed.
He has increased appetite having gained 15 pounds since his visit 5 months ago. He attributed the weight gain to stress at work.
Denies suicidal ideation or homicidal ideation. He also notices trouble concentrating at work and “can’t get into television shows or
movies” in the same way he did prior.
Page 1 of 50
Labs:
Guaiacs Neg x 3
TSH 1.44 (WNL 0.34 – 4.25)
Chem 7 WNL
Hct 40
Lyme Titers Neg
Question 1) Mr. George feels tired and has little energy. His physical examination and lab work are negative. He completely denies
being depressed. Upon further questioning he does describe losing interest in activities he used to like to do, increased appetite and
weight gain, problems with concentration, and insomnia. At this point, Mr. George wants to know the next appropriate step in his
assessment and management. Of the following, which one is the most appropriate recommendation?
a)
b)
c)
d)
e)
f)
II. Facts About
Depression
Perform a whole body CT or MRI scan to look for an occult source
Recommend that Mr. George and his family go on a vacation
Consider testing for underlying neurological disease
Refer him to a gastroenterologist for a colonoscopy screen
Have Mr. George complete a standardized screening questionnaire for depression
Write him a prescription for sleeping medications
The correct answer is e. Mr. George has many classic signs and symptoms of depression (e.g., anhedonia, insomnia, weight
gain, etc.), and performing a standardized screening questionnaire for major depression is appropriate to assist in making the
diagnosis. Many people who suffer from depression do not report a depressed mood. Although some neurological diseases can
have depressive symptoms, major depression is much more common in the primary care setting and should be evaluated first. He
also has no neurological findings. A colonoscopy would not seem appropriate in a 44 year old man at this point without
gastrointestinal complaints, no findings of anemia, and weight gain. A whole body CT or MRI scan is not cost effective, and may
cause more physical and emotional harm than benefit. Insomnia may be a sentinel symptom of depression, and prescribing
sleeping medications without assessing the patient for depression would not be “best practice”. Although a vacation may be in
order for Mr. George and his family, it will not effectively treat an underlying depressive disorder.
Web Based Education Module 4: “The Diagnosis and Management of Depression in The Primary Care Setting”
Facts About Depression
Depression is one of the most common conditions seen by primary care physicians second only to hypertension. The point prevalence
in the outpatient primary care setting is between 4.8 – 8.6%, and the point prevalence in the inpatient setting is 14.6% Large scale
studies have suggested that 7 – 12% of men will suffer an episode of major depression at one point in their lives, while the percentage
for women is more on the order of 20 – 25%. Bipolar disorder is less common than depression (0.4% in men and 1.6% in women over
their lifetimes) but has no gender difference. Depression can begin in early adulthood, with a peak onset between ages 20 – 30. Over
Page 2 of 50
half the people who experience an episode of major depression are at risk for a relapse and recurrence (Cutler, J. Charon, R. 1999).
Depression costs the United States economy more than 43 million dollars every year in medical treatments and lost work productivity
(Kahn, 1999). Globally, depression accounts for 4.4% of the disease burden, which is similar to that of diarrheal diseases and ischemic
heart disease (Mann, 2003). 300 million people in the world suffer from depression with 18 million of them in the United States
(Harvard Press, 1996).
Depression has a high rate of morbidity and mortality when left untreated. Most patients do not necessarily complain of feeling
depressed, but rather that they have a lack of interest or pleasure in activities, may have somatic complaints, or vague unexplained
complaints. In one study, 69% of diagnosed depressed patients reported unexplained physical symptoms as their chief complaint
(NYCDOH, 2006). Unlike patients with depression in psychiatric inpatient or outpatient care settings, persons suffering from
depression in primary care settings often present as “undifferentiated” patients.
Depression is often undiagnosed and untreated, and even when it is diagnosed it is often under treated. Primary care physicians must
remain alert to effectively screen for depression in their patients. Barriers to effective screening include inadequate education and
training, limited coordination with mental health resources, time constraints, poor systematic follow up, and inadequate
reimbursement (NYCDOH, 2006). It is sometimes difficult for primary care providers to determine if a patient is depressed as
opposed to experiencing a normal response to the challenges of everyday life. Gender, age, culture, and language of the patient and
the physician may create further barriers. Furthermore, persons with mood disorders also may have enormous stigma associated with
being mentally ill – and may see it as a sign of weakness, fear the criticism of other people, or be concerned that they will be
institutionalized.
III. Goals and Objectives
Patients who suffer from diabetes, ischemic heart disease, stroke, or lung disorders that have concurrent depression have poorer
outcomes than those without depression. Depressed patients have a higher risk of death from heart disease, respiratory disorders,
stroke, accidents, and suicide (Mann, 2005). Fifteen percent of patients with severe mood disorders die from suicide. In one study
among older patients who committed suicide, 20% visited their primary care physician on the same day as their suicide (NYCDOH,
2006).
Educational Goal: Students will be able to demonstrate competencies in knowledge, skills, and attitudes of an effective clinician in
evaluating and caring for patients with depression and mood disorders in the primary care setting.
Medical Knowledge
The students will:
1. Apply the nationally recognized guidelines for screening and diagnosing depression and other mood disorders in patient care.
2. Apply the practice guidelines for the treatment of patients with major depressive disorders.
3. Identify appropriate elements of a suicide risk assessment and action plan.
Page 3 of 50
Patient Care
The students will:
1. Recognize the importance of effective detection and treatment of depression in adults.
2. Review the depressed mood algorithm and the DSM-IV to guide the differential diagnosis in the primary care setting.
3. Identify manic and hypomanic symptoms associated with bipolar disorder in depressed patients.
4. Formulate management plans for the longitudinal care of patients with depression.
5. Develop prevention plans, including health education and behavioral change strategies, for patients with depression.
Interpersonal and Communication Skills
The student will:
1. Explore relevant psychosocial and cultural issues that impact on care.
2. Provide effective education and counseling to patients with mood disorders and their families.
3. Demonstrate awareness of improved health care outcomes through effective communication and forming therapeutic
alliances with patients.
4. Discuss behaviors with patients, in an empathic, respectful and non judgmental manner.
Practice Based Learning
The student will:
1. Use information technology to access medical information and support self-education and clinical decision making.
2. Critically review the medical literature regarding new evidence based clinical trials and its implication on current treatment
guidelines of depression and mood disorders.
3. Use information technology to access patient and family education resources on depression.
Professionalism
The student will:
1. Demonstrate professionalism by completing this web module during the assigned period.
Systems Based Practice
The student will:
1. Identify which cases can be managed by the primary care physician and which should be referred for co-management with a
specialist.
2. Improve patient care outcomes through effective communication with other health care professionals, partnerships through
Page 4 of 50
IV. The Etiology of
Mood Disorders
community resources, and government agencies.
The Etiology of Mood Disorders
Neurotransmitters, genetics, and psychosocial stressors all seem to play a part in mood disorders.
The same depressed patient may have variable clinical symptoms from one major depressive episode to another. Despite this
variability, major depression may have the same underlying cause. The variable presentations may be due to differing patterns in
neurotransmitter abnormalities. Deficiencies in serotonin, norepinephrine, dopamine, GABA, and peptide neurotransmitters
(somastatin, thyroid-related hormones, and brain derived neurotrophic factors) have all been hypothesized as contributing to
depression. Over activity in other neurotransmitters including substance P, and acetylcholine, and elevated serum cortisol (with lack
of diurnal variation) has also been proposed to contribute to depression.
Although no specific genes that affect neurotransmitters or hormones have been identified, both depression and bipolar disorder are
clearly inheritable. The first degree relatives of a patient with recurrent major depression have a 1.5 – 3 times higher risk of depression
themselves as compared to the general population. 27% of children with one parent with a mood disorder will develop a mood
disorder themselves, and that increases to 50 – 75% if both parents are affected. First degree relatives of patients with bipolar disorder
have an estimated 12% lifetime prevalence of bipolar disorder, which is 10 times higher than the general population (Cutler, J.
Charon, R. 1999). Genetic predisposition is not enough to result in a patient with a mood disorder, however. Identical twins have
incomplete concordance in regards to depression. Depression also occurs in patients with no family history of mood disorders, which
may infer that they have another acquired biological deficiency such as a viral insult, genetic or perinatal insult, or vascular brain
disease.
Psychosocial stressors in combination with a genetic predisposition have been postulated to alter the size of neurons, neuronal
function, repair capabilities, and production of new neurons. Elevated cortisol in some depressed patients may reduce hippocampus
volume, especially if their depression has not been treated in some time. Brain imagery has also noted some altered structures, which
suggest some changes in neurocircuitry. Psychosocial theories suggest that experiences of “loss” in certain vulnerable individuals may
cause depression, either through trauma, parental loss, loss of love from others, or loss of self-esteem.
Page 5 of 50
“On the Threshold of Eternity / At Eternity’s Gate / Old Man in Sorrow” - Vincent van Gogh
V. Diagnosing Mood
Disorders
A. Screening for
Depression
B. Major
Depressive
Episode
C. Approaches To
The Clinical
Interview
D. Depressive
Spectrum
LINK: Vincent van Gogh (Wikipedia: http://en.wikipedia.org/wiki/Vincent_van_Gogh)
Screening for Depression
The primary care physician’s most powerful screening tool for depression is patient observation and active listening skills. Most
depressed patients do not realize they are depressed – and this is especially true in elderly patients. A physician should consider that a
patient may have depression in the setting of unexplained physical symptoms or complaints. The higher the number of somatic
complaints that a patient has, the higher the risk that they may have a mood disorder. Other clues may be a patient with persistent
worries or concerns about medical illness, complaints that do not respond to typical interventions, or complaints outright of anxiety or
panic attacks. Patients with substance abuse issues may also suffer from a mood disorder. A careful history of present illness, past
medical history, social and family history, and review of systems may yield more important information for making the diagnosis.
The primary care physician should ask open-ended questions of the patient about normal patterns as well as variations to determine
baseline function and mood. Mood is a range of emotions that a person feels over a period of time, while affect is how a person
Page 6 of 50
E.
F.
G.
H.
I.
J.
K.
L.
M.
N.
Disorders: The
Depressed
Mood
Algorithm
Mood disorder
due to a general
medical
condition
Substanceinduced
depression
Dysthymic
Disorder
Bereavement
Adjustment
disorder with
depressed mood
Seasonal
affective
disorders
Postpartum
depression
Pseudodementia
Manic and
Hypomanic
Symptoms and
Bipolar
Disorders
Suicidal
Patients –
students to
identify
displays his or her mood. The presence of a mood disorder may affect a person’s concentration, attention, motivation, interest, and
sleep, as well as energy level, hunger and satiety levels, sexual pleasure, and pain sensation. These patients also frequently lose
interest and lose pleasure (anhedonia) in things, people, or activities that they used to enjoy. Interruption in personal relationships with
others can be a side effect due to increasing anger and conflicts, lower frustration tolerance, or from apathy and lack of enthusiastic
feelings towards other people. Patients with depression may become emotionally constricted and lose their emotional flexibility.
Depression can impair cognitive function. Cognitive dysfunction is common and patients may state that when they watch television
they lose the point of the story; they read the same page of a book over and over again without comprehension; or lose the point of
conversations with other people. A depressed patient’s memories may amount to more of selective recall, and normal perceptions may
become distorted. Severe cognitive impairment due to depression is known as pseudodementia, and may be seen in elder populations
or patients with central nervous disorders.
Psychomotor activity is usually decreased in depressed patients. Psychomotor retardation is present when thoughts, motor movements,
or speech are slowed down. Psychomotor agitation can also occur and is present when patients experience unintentional and
purposeless movements – such as unstoppable crying, pacing around a room, or hand-wringing. Frequently patients may complain of
insomnia. In addition to having difficulty falling asleep, depressed patients typically wake up in the middle of the night or early in the
morning with feelings of sadness, anxiety, or thoughts of dread or doom. They may also sleep excessively or stay most of the day in
bed.
Depressed patients may also have self-worth that goes through turbulent fluctuations. For depressed patients, past events may be
viewed with extreme guilt and self criticism, and feelings of worthlessness. Patients may view themselves and their world as hopeless.
Suicidal ideation or a history of suicidal attempts from the patient should be assessed. Asking depressed patients about recent
bereavement is also important to note.
A past medical history of prior episodes of depression is a very important question because you may be observing a relapsing episode.
In addition, the physician should inquire about a previous history of bipolar disorder because inappropriate treatment with an
antidepressant-therapy alone in these patients may precipitate a manic episode. It is also important to inquire about a family history of
depression or bipolar disorder.
When to think about screening adults for depression
Personal previous history of depression or bipolar disorder
First-degree biologic relative with history of depression or bipolar disorders
Patients with chronic diseases
Obesity
Chronic pain (e.g., backache, headache)
Impoverished home environment
Page 7 of 50
Financial strain
Experiencing major life changes
Pregnant or postpartum
Socially isolated
Multiple vague and unexplained symptoms (e.g., gastrointestinal, cardiovascular,
neurological)
Fatigue or sleep disturbance
Substance abuse (e.g., alcohol or drugs)
Loss of interest in sexual activity
Elderly age
Adapted from Sharp, LK, Lipsky MS. “Screening for depression across the lifespan: a review of measures for use in primary care
settings.” American Family Physician. 2002; 66: 1001-1008
Question 2) Which are the current recommendations of United States Preventive Screening Task Force for screening adults for
depression in primary care settings?
a)
b)
c)
d)
e)
No recommendation for or against routine screening for depression in primary care settings
Screen only adults with positive risk factors for major depression, such as those with a positive family history or chronic pain
Screen in all primary care practices because it is highly effective
Screen only when the primary care practice has a psychiatrist on staff
Screen only when systems are in place to ensure adequate treatment and follow up
The correct answer is e. The United States Preventive Screening Task Force recommends “screening adults for depression in
clinical practices that have systems in place to assure accurate diagnosis, effective treatment, and follow up” (USPSTF, 2006).
The system in place to assure follow up and monitoring can be the primary care physician, their primary care colleagues, or
properly trained staff such as nurses. Access to mental health services, outside the practice, is important should referrals be
necessary for complicated cases (e.g., psychiatrists, therapists, emergency departments, etc.). The USPSTF recommends that
clinicians provide depression screening to eligible patients because of fair evidence that screening improves important health
outcomes and concludes that benefits outweigh harms. The existing literature suggests that screening tests perform reasonably
well in adolescents and that treatments are effective, but the clinical impact of routine depression screening has not been studied
in pediatric populations in primary care settings. (Source: United States Preventive Screening Task Force. Screening for
depression: Recommendations and rationale. November 2006 Recommendations. http://epss.ahrq.gov/PDA/index.jsp)
There are many formal screening tools available such as the Zung Self-Assessment Depression Scale, Beck Depression Inventory,
General Health Questionnaire (GHQ), Center for Epidemiologic Study Depression Scale (CES-D), and the Patient Health
Questionaire-2 (PHQ-2). The USPSTF does not recommend one screening test over another and the interval for screening that is
Page 8 of 50
considered optimal is unknown. Recurrent screening in patients with a history of depression, unexplained somatic symptoms,
substance abuse, chronic pain, or co-morbid psychological conditions may be the most useful. Any screening test that is positive
requires a full diagnostic interview that uses standard diagnostic criteria, Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) to determine the presence of major depressive disorder and/or dysthymia.
The Patient Health Questionnaire - 2 (PHQ-2) is a validated primary care tool for depression screening, and is favored because of
the relative ease of using a two question tool and because the USPSTF believes that with current available evidence it is as effective as
longer screening tools.
Patient Health Questionnaire – 2 (PHQ-2)
Screen for depression by asking the following 2 questions:
Over the past 2 weeks, have you been bothered by:
little interest or pleasure in doing things?
feeling down, depressed, or hopeless?
A “no” response to both questions is a negative screen.
A “yes” response to either question OR if the physician is still concerned about depression,
then the physician should ask more thorough assessment questions using
the Patient Health Questionnaire – 9 (PHQ-9).
The Patient Health Questionnaire – 9 (PHQ-9) is a nine item questionnaire that can be completed by the patient before or during a
primary care office visit. It is available in several languages. The PHQ-9 can reliably detect and quantify the severity of depression
using the DSM-IV criteria for major depressive episode. The PHQ – 9 was created by Dr. Robert Spitzer, et al. at Columbia
University and is copyright protected by Pfizer Inc. The PHQ – 9 is also useful for patient follow up visits to assess symptom
management. Instructions on the use of the PHQ – 9 is available on the PDF files below:
LINK: PDF of PHQ – 9 (English)
LINK: PDF of PHQ – 9 (Spanish)
Major Depressive Disorder
Summary of DSM-IV Criteria for Major Depressive Episode
If depressed mood or loss of interest or pleasure persists for more than at least a two-week
period, consider the diagnosis of major depressive episode. The diagnostic criteria are
summarized below:
Page 9 of 50
A. At least five of the following symptoms have been present during the same two-week
period, nearly every day, and represent a change from previous functioning. At least
one of the symptoms must be either (1) depressed mood or (2) loss of interest or
pleasure:
1) Depressed mood (or alternatively can be irritable mood in children and
adolescents)
2) Marked diminished interest or pleasure in all, or almost all, activities
3) Significant weight loss or weight gain when not dieting
4) Insomnia or hypersomnia
5) Psychomotor retardation or agitation
6) Fatigue or loss of energy
7) Feelings of worthlessness or excessive or inappropriate guilt
8) Diminished ability to think or concentrate
9) Recurrent thoughts of death, recurrent suicidal ideation without a specific
plan, or a suicide attempt or specific plan for committing suicide
B. Symptoms are not accounted for by a mood disorder due to a general medical
condition, a substance-induced mood disorder, or bereavement (normal reaction to the
death of a loved one).
C. Symptoms are not better accounted for by a psychotic disorder (e.g. schizoaffective
disorder).
A well-known mnemonic that is commonly used to remember the DSM-IV criteria is SIGECAPS:
Sleep
Interest (anhedonia)
Guilt
Energy
Concentration
Appetite
Psychomotor
Suicidality
A major depressive episode can be associated with special features: melancholic, psychotic, or atypical.
Patients with melancholic features will report nearly total anhedonia. Depressed patients with melancholia must have three of the
Page 10 of 50
following symptoms: diurnal variation (depression worse in the morning); pervasive and irremediable depressed mood; marked
psychomotor retardation or agitation; significant weight loss or anorexia; excessive or inappropriate guilt; and early morning
awakening. Depressed patients with melancholic features have the best response to pharmacotherapy.
Depressed patients that have psychotic features such as hallucinations and delusions are at very high risk for suicide even if they deny
suicidal ideation. These patients should be sent for hospitalization immediately and should be under the care of a psychiatrist.
Patients with atypical features have milder depressed symptoms. Depressed patients with atypical features must experience mood
reactivity as well as two of the following: leaden paralysis (enormous effort to walk or exert); hypersomnia; rejection hypersensitivity
(even when the patient is not acutely depressed); overeating or weight gain. These patients respond less to tricyclic antidepressants.
Approaches to Interviewing Patients with Suspected Depression
Depressed patients may feel so helpless, hopeless, indecisive, or lacking in energy that physicians may need to take a more active role
to engage the patient or to show their interest or concern. Again in major depression, the more common complaint is anhedonia and
not depressed mood. Quiet listening and empathy are important approaches physicians can use with patients. A caring and
nonjudgmental tone is critical to allay patient fears of the stigma of depression. Introducing the topic of depression with an
educational statement first and then asking the patient for their response may help the patient not feel judged (example – “Patients
who have had a heart attack sometimes get depressed or down after the event. Has this been happening to you recently?”). Making a
statement instead of a question may allow the patient to have permission to be depressed and to know that you are willing and open to
discussing the issue without judgment (example – “It sounds like you have been pretty down recently.”).
Physicians may want to excuse depression symptoms in patients by attributing them to stressors or complications of life. Patients with
increasing financial stress, work difficulties, and relationship problems should raise further possibility of major depression.
These patients may be unduly critical of themselves but may also be critical of others including their doctors. It is important to
recognize when they evoke frustration or anger in you so that you can avoid negative countertransference and avoid directing anger
back at the patient.
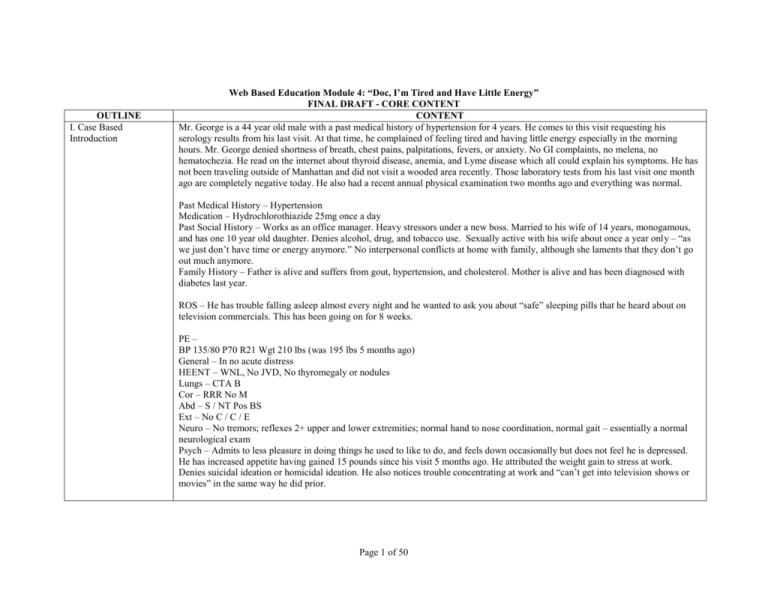
Depressive Spectrum Disorders: The Depressed Mood Algorithm
Major depressive episode is just one of several depressive spectrum disorders. In addition, depression may be associated with chronic
medical illnesses. The following “depressed mood algorithm” can be used in primary care settings to assist in making the differential
diagnosis.
Depressed Mood Algorithm
Page 11 of 50
NO
NO
If NO,
Are the symptoms
due to a stressor?
Is a general medical
condition directly
responsible for the
symptoms?
YES
Mood disorder
due to a general
medical
condition
Is a substance directly
responsible for the
symptoms?
YES
Substanceinduced disorder
Is the depressed mood
or anhedonia present
for at least 2 weeks?
If YES,
Are associated
symptoms present?
YES
Adjustment disorder with depressed
mood
If YES,
Are they best
explained by
bereavement?
NO
Depressive disorder not otherwise
specified or no disorder
If NO,
Has the depressed mood or
anhedonia and milder
associated symptoms been
present for at least 2 years?
NO
Major depressive disorder
YES
Bereavement
YES
Dysthymic disorder
Adapted with permission from “Depression” Janis Cutler MD and Rita Charon, MD. Primary Care Psychiatry and Behavioral
Page 12 of 50
Medicine: Brief Office Treatment and Management Pathways. Edited by RE Feinstein, AA Brewer. Springer Publishing Co., New
York, NY. 1999
Depression Due To General Medical Conditions
Alterations in mood may be related to underlying medical conditions. Depression may be associated with other chronic medical
diseases such as cancer, stroke, heart disease, endocrine disorders, neurological diseases, epilepsy, gastrointestinal diseases,
rheumatologic diseases, and severe anemia. This depression is independent of the psychological impact of the stress of the illness, and
is patho-physiologically related to the underlying condition.
Medical Conditions Associated With Increased Incidence of Depression
Cardiac disease
Ischemic disease, Myocardial infarction
Heart failure
Cancer
Brain cancer
Pancreatic cancer
Endocrine disorders
Hyperthyroidism
Hypothyroidism
Diabetes
Parathyroid dysfunction
Cushing’s disease
Gastrointestinal disorders
Inflammatory bowel disease
Irritable bowel syndrome
Hepatic encephalopathy
Cirrhosis
Neurologic disease
Stroke
Chronic headache
Dementias
Traumatic brain injury
Multiple sclerosis
Parkinson’s disease
Epilepsy
Pulmonary disease
Sleep apnea
Reactive airway disease
Rheumatologic disease
Lupus
Rheumatoid arthritis
Chronic fatigue syndrome
Fibromyalgia
Page 13 of 50
Metabolic disease
Renal failure
Electrolyte disturbances
HIV disease
Syphilis
Hepatitis
Lyme disease
Severe anemia
Infectious disease
Hematologic disorder
Identification of co-morbid disease or conditions is important in patients with depression. Primary care physicians should consider
initial lab testing such as thyroid-stimulating hormone, complete blood count, and chemistry panel. The findings of the complete
history and physical examination may clarify the need for further testing for other diseases or syndromes.
Depression Impacting Existing Medical Illness
Patients who suffer from diabetes, ischemic heart disease, stroke, or lung disorders and who have concurrent depression have poorer
outcomes than those without depression. Depressed patients, in general, have a higher risk of death from heart disease, respiratory
disorders, stroke, accidents, and suicide.
Question 3) Depression may affect the management of general medical illness. Which of the following statement is false?
a)
Patients with depression may exhibit maladaptive interpersonal behaviors which can make collaboration with physicians
more challenging
b) Patients with depression have higher rates of adverse health-risk behaviors when compared to non-depressed patients
c) Patients with aversive symptoms such as pain are at an increased risk for developing depressive disorders
d) The presence of a chronic medical illness is the most prevalent risk factor for the development of depression
e) The importance of screening, diagnosing, and treating depression after a myocardial infarction has been well documented
The correct answer is d. The presence of a chronic medical illness alone is not the most prevalent risk factor for developing
depression. Depressed patients have higher rates of adverse health risk behaviors which may lead to higher risk of death from
heart disease, respiratory disorders, stroke, accidents, and suicide. Chronic pain is known to be a risk factor for developing
depression. Depressed patients may express maladaptive interpersonal behaviors such as anger or non-adherence which may
cause some conflict with their medical providers. Screening, diagnosing, and treating depression after a myocardial infarction has
been found to be of benefit in these patients.
Substance-induced depression
Depression may be induced by substances ingested for recreation or mood alteration or from their withdrawal. These substances
Page 14 of 50
include alcohol, hypnotics, sedatives, opiates, marijuana, amphetamines, cocaine, and other designer drugs (e.g., ketamine, ecstasy).
Prescription drugs used for medical treatment can also cause mood disturbances such as blood pressure medication (e.g., reserpine,
propanolol), anticholinergics, steroids, oral contraceptives, psychotropic medications, and antineoplastic drugs.
Dysthymic disorder
Dysthymic disorder is a chronic form of depression. The signs and symptoms are milder but can cause much distress and dysfunction.
The patient must have at least a two year history of complaints occurring on over half the days to make the diagnosis. It is important
to distinguish dysthymic disorder from major depression because dysthymic disorder is more chronic and unremitting, and less
responsive to pharmacotherapy. Family and friends may experience people with dysthymic disorders to be chronic complainers or
pessimists.
Summary of DSM-IV Criteria for Dysthymic Disorder
A. Depressed mood for most of the day, for more days than not, as indicated either by
subjective account or observation by others, for at least two years. Note: In children and
adolescents, mood can be irritable and duration must be at least one year.
B. Presence, while depressed, of two (or more) of the following:
1) Poor appetite or overeating
2) Insomnia or hypersomnia
3) Low energy or fatigue
4) Low self-esteem
5) Poor concentration or difficulty making decisions
6) Feelings of hopelessness
C. During the two year period (one year for children and adolescents) of the disturbance, the
person has never been without the symptoms in criteria A or B for more than two-months
at a time.
D. No major depressive episode has been present during the first two years of the
disturbance (one year for children and adolescents); i.e, the disturbance is not better
accounted for by chronic major depressive disorder, or major depressive disorder in patial
remission.
E. There has never been a manic episode, a mixed episode, or a hypomanic episode, and
criteria have never been met for cyclothymic disorder.
F. The disturbance does not occur exclusively during the course of a chronic psychotic
disorder, such as schizophrenia, or delusional disorder.
G. The symptoms are not due to the direct physiological effects of a substance (e.g. a drug of
abuse, a medication) or general medical condition (e.g., hypothyroidism).
H. The symptoms cause clinically significant distress or impairment in social, occupational,
Page 15 of 50
or other important areas of functioning.
Bereavement
Bereavement is a normal reaction to the loss of a loved one. It is accompanied by insomnia, sadness, weight loss, decreased appetite.
Symptoms resolve normally within 2 months and do not require psychotherapy or pharmacotherapy. When symptoms persist beyond
2 months, the possibility of a diagnosis of major depression exists. Pathologic symptoms include thoughts of death beyond the wish to
be with the lost loved one, excessive guilt, an overwhelming new sense of worthlessness, severe psychomotor retardation,
hallucinations (other than transiently hearing the voice or seeing the image of the loved one), or the inability to perform usual tasks
and obligations.
Adjustment disorder with depressed mood
Adjustment disorder with depressed mood is diagnosed when the patient has depressive symptoms or complaints within 3 months of
an identifiable psychosocial stressor. Stressors may include academic failure, job loss, or divorce. The stressor causes depressed
symptoms that do not meet the criteria for major depression or dysthymic disorder. The treatment of choice is psychotherapy over
pharmacologic therapy.
Seasonal affective disorders
Major depressive episodes that have a seasonal pattern, particularly with the start of fall or winter, or when natural daylight decreases,
are considered seasonal affective disorders. The diagnosis can not be made if there is a clear psychosocial stressor related to the
change in season. These patients respond to standard antidepressants and psychotherapy, in addition to light therapy.
Depression in pregnancy and postpartum depression
Question 4) You have a 28 year old woman who is in her third trimester of pregnancy. She has been diagnosed with severe
depression and is under the care of a psychiatrist. She wants to discuss with you the risk of taking antidepressants during the rest of
her pregnancy. Which of one of the following statements is true?
a)
If she takes an SSRI (selective serotonin reuptake inhibitor), her newborn has a small risk of developing a transient
withdrawal syndrome that may consist of inconsolable crying, irritability, tachypnea, thermal instability, and poor muscle
tone.
b) If she takes an SSRI (selective serotonin reuptake inhibitor), her newborn has a small risk of developing a permanent
serotonin syndrome that may consist of inconsolable crying, irritability, tachypnea, thermal instability, and poor muscle tone.
c) If she takes an SSRI, her newborn will likely be larger than a newborn delivered by a mother not taking antidepressants.
Page 16 of 50
d) Tricyclic antidepressants have teratogenic effects.
e) She should stop any antidepressant a few weeks prior to her due date to prevent neonatal withdrawal syndrome.
The correct answer is a. Selective serotonin reuptake inhibitors are the agents of choice. Selective serotonin reuptake inhibitors
and tricyclic antidepressants appear to have no teratogenic effects. There is also a small but significant risk of “withdrawal
syndrome” in the newborn if serotonergic antidepressants are taken during the third trimester. This “withdrawal syndrome”
consists of irritability, inconsolable crying, tachypnea, thermal instability, and poor muscle tone but is usually mild and transient.
More recently, a case-control study reported a possible association between SSRI use in late pregnancy and persistent pulmonary
hypertension in the offspring.
Although depression in pregnancy and postpartum depression is beyond the scope of this web module, it is important for primary care
physicians to be aware of screening these patients for timely intervention.
Medical management of depressed patients during pregnancy usually stirs discomfort in physicians because of fear of teratogenic
effects in the fetus. Adverse effects of not treating this population are well documented, as well as the safety profiles of commonly
prescribed psychiatric medications. Selective serotonin reuptake inhibitors are the agents of choice. Fluoxetine and tricyclic
antidepressants appear to have no teratogenic effects, and new data shows similar safety profiles for other selective serotonin reuptake
inhibitors. The mood stabilizers (e.g., dilantin, valproic acid, carbamazepine) appear to be teratogenic. The decisions regarding the use
of psychiatric medications should be individualized. The most important factor is usually the patient’s level of functioning in the past
when she was not taking medications. There is a small but significant risk of “withdrawal syndrome” in the newborn if serotonergic
antidepressants are taken during the third trimester. This “withdrawal syndrome” consists of irritability, inconsolable crying,
tachypnea, thermal instability, and poor muscle tone but is usually mild and transient. Overall, pregnant patients, once identified with
depression, should be under the care of a psychiatrist and an obstetrician or family physician with experience in high risk obstetrics.
Psychotherapy has also been found to be useful in these women.
Postpartum depression typically occurs within one month of delivering a baby. Normal “baby blues” can begin 24 hours after delivery
and last up to 10 days. Postpartum depression is not different from a major depressive episode, but the primary care physician or
obstetrician should recognize the symptoms as immediate interventions can have positive outcomes for the mother and baby. One
important challenge is that the onset of postpartum depression frequently occurs before the patient is seen for a routine six-week
postpartum visit. The risk-benefit decision about whether to start antidepressants in a breastfeeding woman is based on the severity of
the depression and the need for pharmacotherapy, rather than any known risks to the infant.
More information on treatment of depression in pregnancy, postpartum women, and breastfeeding woman can be found in this web
module’s library.
LINK: Ward, R. Zamorski, M. “Benefits and Risks of Psychiatric Medications in Pregnancy” Am Fam Physician. 2002;66:62936,639.
Page 17 of 50
LINK TO RESOURCE FOR PATIENTS AND DOCTORS ON PREGNANCY AND DEPRESSION: www.womensmentalhealth.org
Depression in the Elderly and Pseudodementia
QUESTION 5) Which one of the following statements is true about depression in the elderly?
a) Physicians are more likely to diagnose depression correctly in the elderly than in younger people.
b) Depression in the elderly is less important than in younger patients because depression is a normal part of the aging process.
c) Patients who are elderly when their first depressive episode occurs have a relatively high likelihood of developing recurring
chronic depression.
d) Risk factors for depression in elderly persons include a history of depression, chronic medical illness, male sex, being single
or divorced, brain disease, alcohol abuse, use of certain medications, and stressful life events.
e) The long term prognosis for the elderly suffering from depression is poor even with treatment.
The correct answer is c. As in younger populations, depression in the elderly is often not diagnosed and not treated by
physicians. A popular misconception by patients, families, and physicians is that depression is a normal part of the aging process.
Risk factors for depression in elderly persons include a history of depression, chronic medical illness, female sex, being single or
divorced, brain disease, alcohol abuse, use of certain medications, and stressful life events. Patients who are elderly when their
first depressive episode occurs have a relatively high likelihood of developing recurring chronic depression. With proper
diagnosis and management, depression in the elderly is treatable and has a good prognosis. (Source: Birrer, RB, Vemuri SP.
Depression in later life: A diagnostic and therapeutic challenge. Am Fam Physician 2004; 69 (10): 2375-2382)
Depression in the elderly is not part of the normal aging process. This common misconception may lead elderly patients, or their
families, not to seek appropriate help. It can also lead physicians to miss the diagnosis of depression in the elderly and leave it
untreated. A common complaint in elderly patients is not depression but insomnia, anorexia, and fatigue. Treatment with
antidepressants, especially selective serotonin reuptake inhibitors can be useful. Patients who are elderly when they have their first
episode of depression have a relatively higher likelihood of developing chronic and recurring depression. The prognosis for recovery
is equal in young and old patients, although remission may take longer to achieve in older patients.
Pseudodementia, associated with severe depression, can be easily mistaken for dementia, especially in the elderly or persons with
underlying neurological disease (e.g., strokes, etc). The symptoms of pseudodementia include marked psychological distress, inability
to concentrate or complete daily tasks, and marked cognitive dysfunction. Differentiating between dementia and pseudodementia is
important. Typically, patients suffering from pseudodementia will exhibit profound concern about their impaired cognitive function,
in contrast with patients with a diagnosis of dementia, who may tend to minimize their disability. In addition to pharmacotherapy,
electroconvulsive therapy may be warranted in patients with pseudodementia.
Page 18 of 50
All patients with depression of all ages, including the elderly, should have a mini-mental status examination at baseline. Patients
successfully treated of their major depression will see their pseudodementia and cognitive dysfunction improve.
Reproduced with permission from Birrer, R., Vemuri, S. “Depression in Later Life: A Diagnostic and Therapeutic Challenge.”
American Family Physician. 2004;69:2375-82.
More information on depression in the elderly is available in this web module’s library.
LINK TO: Birrer, RB, Vemuri SP. Depression in later life: A diagnostic and therapeutic challenge. Am Fam Physician 2004; 69 (10):
2375-2382
Manic and Hypomanic Symptoms: Bipolar Disorder
Page 19 of 50
Question 6) You are evaluating a 35 year old male in your primary care practice. He has a history of depression and occasional panic
attacks. His previous physicians treated his panic symptoms with selective serotonin reuptake inhibitors (SSRIs) approved for panic
disorders but the medications made him more restless, agitated, and unable to sleep. Upon further questioning, you discover he has
been having symptoms with impairing depressive episodes and anxiety since late childhood. His father was hospitalized with a manic
episode on one occasion. Upon further exploration, which one of the following would be most specific for confirming the diagnosis of
bipolar disorder?
a)
b)
c)
d)
e)
His brother has a confirmed diagnosis of bipolar I disorder
His sister has a confirmed diagnosis of bipolar II disorder
The patient has symptomatic improvement on lithium
His mother’s mania improved with lithium
The patient has had a hypomanic episode
The correct answer is e. The risk of having bipolar disorder is higher in persons with first degree relatives with bipolar disorder.
Incidental improvement of symptoms with lithium may also provide clues. Of all these findings, the most specific to the diagnosis
is the patient having a hypomanic episode himself. (Source: American Psychiatric Association: Diagnostic and Statistical Manual
of Mental Disorders, ed 4 text revision, American Association, 2000. Washington DC)
A major depressive episode can appear as a unipolar disorder, but all primary care physicians should be aware that this presentation
may be part of an underlying bipolar disorder. Primary care physicians who diagnose and treat patients with depression should
carefully assess patients for a history or current complaint of manic and hypomanic symptoms. Misdiagnosis of a bipolar disorder
patient presenting with major depressive symptoms can lead to mistreatment with antidepressants alone, which may precipitate a
manic episode. A manic mood is characterized by irritability or abnormal euphoria. Hypomania can be seen as a lesser degree of
mania that lasts for a shorter duration. Hypomanic patients usually can continue with their normal life routines and don’t require
hospitalization. A patient with a “mixed state” has to technically satisfy all the criteria of a major depressive disorder and mania at the
same time. DSM-IV criteria for mania and hypomania can be found on the next table. Patients with bipolar disorder should be referred
for collaborative care with a psychiatrist.
Summary of DSM-IV Criteria for Manic Episode
A. A distinct period of abnormally and persistently elevated, expansive, or irritable
mood, lasting 1 week (or any duration if hospitalization is necessary).
B. During the period of the mood disturbance, three (or more) of the following
symptoms have persisted (four if the mood is only irritable) and have been present
to a significant degree:
1) Inflated self-esteem or grandiosity
2) Decreased need for sleep (e.g., feels rested after only 3 hours of sleep)
3) More talkative than usual or pressure to keep talking
Page 20 of 50
4) Flight of ideas or subjective experience that thoughts are racing
5) Distractibility (i.e., attention too easily drawn to unimportant or irrelevant
external stimuli)
6) Increase in goal-directed activity (either socially, at work or school, or
sexually) or psychomotor agitation
7) Excessive involvement in pleasurable activities that have a high potential
for painful consequences (e.g., engaging in unrestrained buying sprees,
sexual indiscretions, or foolish business investments)
C. The symptoms do not meet the criteria for a Mixed Episode.
D. The mood disturbance is sufficiently severe to cause marked impairment in
occupational functioning or in usual social activities or relationships with others, or
to necessitate hospitalization to prevent harm to self or others, or there are psychotic
features.
E. The symptoms are not due to the direct physiological effects of a substance (e.g., a
drug of abuse, a medication, or other treatment) or a general medical condition (e.g.
hyperthyroidism).
Note: Manic-like episodes that are clearly caused by somatic antidepressant treatment
(e.g. medication, electroconvulsive therapy, light therapy) should not count toward the
diagnosis of Bipolar I Disorder.
Summary of DSM-IV Criteria for Hypomanic Episode
A. A distinct period of persistently elevated, expansive, or irritable mood, lasting
throughout at least 4 days, that is clearly different from the usual non-depressed mood.
B. During the period of mood disturbance, three (or more) of the following symptoms have
persisted (four if the mood is only irritable) and have been present to a significant
degree:
1) Inflated self-esteem or grandiosity
2) Decreased need for sleep (e.g., feels rested after only 3 hours of sleep)
3) More talkative than usual or pressure to keep talking
4) Flight of ideas or subjective experience that thoughts are racing
5) Distractibility (i.e., attention too easily drawn to unimportant or irrelevant
external stimuli)
6) Increase in goal-directed activity (either socially, at work or school, or
sexually) or psychomotor agitation
7) Excessive involvement in pleasurable activities that have a high potential
for painful consequences (e.g., engaging in unrestrained buying sprees,
sexual indiscretions, or foolish business investments)
C. The episode is associated with an unequivocal change in functioning that is
Page 21 of 50
uncharacteristic of the person when not symptomatic.
D. The disturbance in mood and the change in functioning are observable by others.
E. The episode is not severe enough to cause marked impairment in social or occupational
functioning, or to necessitate hospitalization, and there are no psychotic features.
F. The symptoms are not due to the direct physiological effects of a substance (e.g., a
drug of abuse, a medication, or other treatment) or a general medical condition (e.g.
hyperthyroidism).
Note: Manic-like episodes that are clearly caused by somatic antidepressant treatment (e.g.
medication, electroconvulsive therapy, light therapy) should not count toward the diagnosis
of Bipolar II Disorder.
Assessing The Risk of Suicide
“The Scream” – Edvard Munch
LINK: Edvard Munch (Wikipedia: http://en.wikipedia.org/wiki/Edvard_Munch)
Page 22 of 50
Patients with depression may be at increased risk for suicide (Kahn, 1999. NYCDOH, 2006, Mann, 2005). Any patient that has a
positive screening for depression should be evaluated for suicide risk. Asking about suicidal thoughts can save the patient’s life.
Contrary to many physicians’ fear, asking about suicidal plans or ideation does not make patients more prone to commit suicide.
Patients are usually relieved that they have been asked about their feelings and thoughts. Asking about suicidal ideation or plans
conveys your interest in their well-being.
Questions in Assessing Suicidal Risk
Current thoughts of harming or killing self
Current plans to harming or killing self
Prior suicide attempts (critical indicator of future suicide risk)
Family history of mood disorder, alcoholism, or suicide
Actions or threats of violence to others
Access to firearms
Male
Elderly
Significant comorbid anxiety or psychotic symptoms and active substance abuse
Poor social support system or living alone
Recent loss or separation
Hopelessness
Preparatory acts (e.g., putting affairs in order, suicide notes, giving away personal
belongings)
Physicians can initiate the topic of suicidal ideation with questions about the patient’s feelings about life.
“Did you ever wish you could go to sleep and never wake up?”
“Have you ever felt life was not worth living?”
Depending on the response, more specific questions about suicidal ideation can be asked.
“Do you ever feel others would be better off without you?”
“Are you having thoughts about killing yourself?”
“Have you thought about killing or hurting others?”
If suicidal ideation is elicited, physicians should ask patients if they have a suicidal plan (e.g., how, when, where). A patient that is
actively thinking about suicide and has a plan for suicide constitutes a medical emergency. This is especially true in patients with
previous suicide attempts. 911 should be called for safe transport to the nearest emergency room for psychiatric care. Prediction of
which patients with suicidal ideation will attempt or commit suicide is very poor.
Page 23 of 50
The Institute of Mental Health has made recommendations for physicians who are assisting potentially suicidal patients. It is
important to monitor your own reactions to a suicidal patient. Stay calm and don’t appear threatened so that the patient feels secure
and maintains the doctor-patient dialogue. Listen attentively so that the patient feels validated about their distress and is not ignored.
Avoid judgmental statements. Emphasize that suicidal feelings worsen with stress, but is a treatable condition. Also highlight that
suicide causes family members and friends great pain that lasts for years. Make it clear to the patient that he or she will have input into
their treatment along with you and the psychiatric team as part of a partnership.
Question 7) Outpatients at risk for suicide should not receive large supplies of antidepressants in case of overdose. Which one of the
following statements is true about antidepressants and suicide?
a) Fluoxetine has been shown to lead to more suicide attempts in adolescents than use of placebo.
b) Norepinephrine reuptake inhibitors (NRIs) are less like than selective serotonin reuptake inhibitors (SSRIs) to be associated
with suicidal thoughts in adolescents.
c) Tricyclic antidepressants (TCAs) are more lethal in overdose than SSRIs.
d) Suicide rates are higher with TCAs than with SSRIs.
The correct answer is c. Tricyclic antidepressants are more lethal in overdose over selective serotonin reuptake inhibitors. The
risk of suicide in all patients who are recovering from major depression may transiently increase during initial treatment, but
whether antidepressants possibly cause increased suicide risk is extremely controversial. Increased energy to act on suicidal
ideation is only one of the possible explanations currently under consideration. Monitoring patients closely during treatment is
paramount and is part of “psychiatric treatment”. Fluoxetine is the only antidepressant found to be effective in children and
adolescents, but close surveillance for suicidal ideation or plans is again warranted. The average risk of suicide in general was 4%
with antidepressants and 2% on placebo. (Sources: Jick SS, Dean AD, Jick H. Antidepressants and suicide. BMJ 1995; 310
(6974): 215-218; Simon GE. How can we know whether antidepressants increase suicide risk? Am J Psychiatry 163:1861-1863,
2006.)
A link to a recent article on whether antidepressants increase suicide risk and the advent of “black box” warnings is available in
the library.
VI. Treatment
Recommendations for
Major Depressive
Disorder
LINK: Simon GE: How can we know whether antidepressants increase suicide risk? Am J Psychiatry 163:1861-1863, 2006.
Treatment Recommendations for Major Depressive Disorder
Successful treatment of major depressive disorder starts with a thorough assessment of the patient. As discussed previously and based
on recommendations of the American Psychiatric Association, healing begins with “psychiatric management” of the patient, followed
by three phases of treatment. This may be done by the primary care physician, and / or psychotherapist, and / or psychiatrist
depending on the history, complexity, and degree of severity of the depression. The following recommendations are for Major
Page 24 of 50
Depressive Disorder, and although no existing scientific literature has been established – it may apply to other syndromes such as
dysthymic disorder.
Psychiatric Management
1.
Perform a diagnostic evaluation to determine if the diagnosis of depression is warranted or if other psychiatric or medical
conditions exist.
History of present illness and current symptoms
Psychiatric history (e.g., symptoms of mania, previous history of psychiatric treatment, response to previous
psychiatric treatments)
General medical history
History of substance abuse disorders
Personal history (e.g. psychological development, response to major life events and transitions)
Social history
Occupational history
Family history
Medication review
A review of systems
A physical examination
A mental status examination
Diagnostic studies as indicated (e.g., TSH, CBC, Basic Chemistry Profile)
2.
Evaluate for the safety of the patient and of others. This evaluation is crucial.
Presence of suicidal or homicidal ideation or plans
Access to a means for suicide and the lethality of the means (e.g. access to handguns)
Presence of psychotic symptoms (e.g. command hallucinations or delusions)
Severe anxiety
Concurrent alcohol or substance use
History of previous attempts
Family history of suicide
Recent exposure to another person who committed suicide
3.
Evaluate functional impairment by assessing:
Interpersonal relationships
Work
Page 25 of 50
Living conditions
Health and medical related needs
4.
Determine a treatment setting. This can vary from ambulatory settings with a primary care provider only, ambulatory settings
with a primary care provider in conjunction with a psychiatrist, day programs, to involuntary psychiatric hospitalization.
Criteria for involuntary hospitalization are usually set by local jurisdictions. Patients should be treated in the setting that is
the safest and is the most effective. The setting should be reassessed at follow up visits. The following situations require
referral to psychiatrist:
Suicide risk
Bipolar disorder or manic episode
Psychotic symptoms
Severe decrease in level of functioning (e.g., unable to care for self)
Recurrent depression
Chronic depression
Depression that is refractory to treatment
Cardiac disease that requires tricyclic antidepressants treatment (contraindication)
Need for electroconvulsive therapy (ECT)
Lack of available support system
Any diagnostic or treatment questions
5.
Establish and maintain a therapeutic alliance. Major depression is a chronic disease and it requires that the patient actively
engages and adheres to long periods of treatment. Symptoms of major depressive disorder (e.g., poor motivation, cognitive
dysfunction, pessimism, etc.), side effects of medications, and misunderstandings between the physician and patient can be
major obstacles to adherence.
Pay attention to concerns patients and their families.
The physician should be aware of any transference or countertransference issues with the patient (e.g., frustration or
anger from or toward the patient, etc.).
6.
Continue to monitor the patient’s psychiatric status and safety. With treatment, some symptoms may improve while others
emerge.
Significant changes in psychiatric status or emergence of new symptoms requires diagnostic and management
reassessment.
7.
Provide patient education and, if appropriate, to the patient’s family. Effective education will allow patients to make
informed decisions about their treatment and improve adherence.
Emphasize that major depression is a “real” illness and not a moral defect.
Page 26 of 50
Effective treatment is available and necessary.
Discuss anticipated side effects of treatments.
Education of family and friends is important
Support groups are available for patients and their families
8.
Enhance treatment adherence.
It is critical for the physician to monitor the patient closely especially as they begin to feel better as the patient may
start to focus on the side effects of treatment rather than the benefits.
The patient should be encouraged to verbalize any concerns or issues.
Review with the patient when and how often to take their medication.
Explain that beneficial effects may take 2 – 4 weeks to be noticed.
Explain the need to continue taking the medication even after the patient feels better.
Remind the patient the need to consult with a physician before stopping medication.
Explain to the patient how to access you, a colleague, or the health care team in case a question or problem arises.
Consider issues of polypharmacy especially in elderly patients.
Consider the financial impact of medications on patients.
Encourage the family to help in the process of adherence.
9.
Work with the patient to address early signs of relapse.
Exacerbations and relapse are common in major depressive disorder, and patients and families should be educated
on this point.
A review of signs and symptoms of relapse with the patient is critical as the next episode may contain different
depressive characteristics.
Emphasize the need to seek early treatment and intervention if symptoms arise to prevent a full-blown exacerbation.
The three phases of treatment of major depression
Treatment consists of three phases:
1.
2.
3.
Acute Phase – Remission is induced (minimum 6 – 8 weeks in duration).
Continuation Phase – Remission is preserved and relapse prevented (usually 16 – 20 weeks in duration).
Maintenance Phase – Susceptible patients are protected against recurrence or relapse of subsequent major depressive
episodes (duration varies with frequency and severity of previous episodes).
Remission and relapse have been defined by the American Psychiatric Association. Remission is the return to the patient’s baseline
level of symptom severity and functioning. Remission should not be confused with significant but incomplete improvement. Relapse
Page 27 of 50
is the re-emergence of significant depressive symptoms or dysfunction after remission has been achieved.
Acute phase treatment
The goal of acute phase treatment is to induce remission and typically lasts a minimum 6 – 8 weeks in duration.
For patients with mild to moderate depression, the initial treatment modalities may include pharmacotherapy alone, psychotherapy
alone, or the combination of medical management and psychotherapy. As stated prior, psychiatric management must be integrated
into treatment regardless of the initial approach.
Antidepressant medications
Antidepressant medications can be used as initial treatment modality by patients with mild or moderate depression. Clinical features
that may suggest that antidepressant medication is preferred over other modalities are a positive response to prior antidepressant
treatment, significant sleep and appetite disturbance, severity of symptoms, or anticipation by the physician that maintenance therapy
will be needed. Patient preference for antidepressant medication alone should be taken into consideration. Most primary care
physicians can medically manage these patients in their practices as long as they continue to monitor the patient’s symptoms closely.
The frequency of monitoring in the acute phase of pharmacotherapy is from once a week to multiple times a week.
Psychotherapy
Psychotherapy alone may be considered as initial treatment modality for patients with mild to moderate depressive disorder. Clinical
features that suggests the use of psychotherapy over other modalities are the presence of psychosocial stressors, interpersonal
difficulties, intrapsychic conflict, and any axis II comorbidities (personality disorders as per DSM-IV). In addition, patient preference
for psychotherapy alone should be taken into consideration, as well as a woman’s desire to get pregnant, be pregnant, or to breastfeed.
Most primary care physicians will refer these patients to a professional psychotherapist for management. The frequency of monitoring
in the acute phase of psychotherapy is from once a week to multiple times a week.
Combination antidepressant medication and psychotherapy
The combination of antidepressant medication and psychotherapy may be the initial treatment approach for patients with moderate
depression in the presence of psychosocial stressors, interpersonal difficulties, intrapsychic conflict, and any axis II comorbidities.
Combination therapy may also be appropriate for patients with only partial remission on one type of treatment, or with a history of
poor adherence to treatment. Most primary care physicians can medically manage these patients while referring them to a professional
psychotherapist for co-management.
Initial acute phase treatment approaches for patients with severe depressive symptoms
Page 28 of 50
Antidepressant medications alone can be used as initial treatment modality by patients with severe depression. There is insufficient
evidence that psychotherapy alone is effective for patients with severe depression. The combination of antidepressant medication and
psychotherapy may be the initial treatment approach for patients for patients with severe depression in the presence of psychosocial
stressors, interpersonal difficulties, intrapsychic conflict, and any axis II comorbidities. Patients with depression and psychotic
symptoms, catatonia, or severe impairment may be considered for combination therapy with antidepressants, antipsychotics, and / or
electroconvulsive therapy (ECT). Patient with severe depression are usually referred for care under a psychiatrist.
Assessing an adequate response in the acute phase with mild to moderate depression
Although the goal of acute phase treatment is to return patients to their functional and symptomatic baseline, it is common for patients
to have a substantial but incomplete response to acute phase treatment. Structured tools that measure depression severity and
functional status may be used for follow up assessment (e.g., PHQ- 9, Beck Depression Inventory, etc.). It is important to not
conclude treatment for these patients at this phase as it may be associated with poor functional outcomes. The degree of an “adequate
response” to treatment of depression has been loosely defined: non-response is the decrease in baseline symptoms of 25% or less;
partial response is a 26 – 49% decrease in baseline symptoms; partial remission is 50% or greater decrease in baseline symptoms with
residual symptoms; and remission is the complete absence of symptoms). When patients have not fully responded at this phase, the
most important first step is increasing the dose.
Overall, if after the initial 4 – 8 weeks there is not a moderate improvement in baseline symptoms in the acute phase, then a
reassessment of the diagnosis, medication regimen and / or psychotherapy, adherence, substance or alcohol use is in order. Increasing
the treatment dose is the first step to be considered. If 4 – 8 weeks after the increase of treatment dose there is not a moderate
improvement in symptoms, another review should occur. Other treatment options should then be considered in consultation with a
psychiatric specialist.
Question 8) From our initial opening clinical case, Mr. George is a 44 year old male who you found to have major depression.
Administration of a standard depression questionnaire (such as the PHQ – 9) found his depression to be of moderate severity. You
started him on antidepressants. You see him 8 weeks later after starting the antidepressant medication and his appetite is back, he is
sleeping well, and concentrating better at home and at work. He still feels tired but denies feeling depressed. He still has not assumed
his normal social activities. You re-administer the same standard depression questionnaire, and conclude that he has achieved partial
remission. Reassessment has found no issues with substance abuse or adherence issues with his medications. After this initial
reassessment, which one of the following is the most appropriate first step in treatment options?
a)
b)
c)
d)
Maintain the current dosage of medication and see him back in 4 to 8 weeks.
Increase the dose of the medication and see him back in 4 to 8 weeks.
Change the medication.
Recommend adjunct psychotherapy.
Page 29 of 50
e)
Consult with a psychiatrist.
The correct answer is b. In the acute phase of treatment, if after 4 – 8 weeks there is not a moderate improvement in baseline
symptoms in the acute phase, then a reassessment of the diagnosis, medication regimen and / or psychotherapy, adherence,
substance or alcohol use is in order. The first step is increasing the dose of the medication since he achieved only partial
remission at the initial dose. If after another 4 – 8 weeks, Mr. George is not improved, consideration can be given to again
increasing the dose of the medication, changing to a different medication, or begin adjunct psychotherapy. If 4 – 8 weeks after the
change in treatment there is not a moderate improvement in symptoms, another review should occur. Other treatment options
should then be considered in consultation with a psychiatric specialist – or at any time the primary care physician feels
improvement is not optimal. (Source: Working Group on Major Depressive Disorders. Practice Guidelines for the Treatment of
Patients With Major Depressive Disorder. American Psychiatric Association. 2000. Washington D.C.)
Continuation Phase Treatment
Patients who have been treated with antidepressant medications in the acute phase should be maintained with this regimen to prevent
relapse. This “continuation phase” should last for 16 – 20 weeks after remission. “Psychiatric management” should continue in this
phase. The American Psychiatric Association recommends the medication doses used in the acute phase be maintained in the
continuation phase. There is increasing data to support the continued use of specific effective psychotherapy in this phase. The use of
ECT in this phase has not been well researched. The frequency of visits in the continuation phase may vary. Stable patients may be
seen once every 2 – 3 months. Patients in active psychotherapy may be seen several times a week.
Patients who remain stable throughout the continuation phase, and who are not candidates for the maintenance phase (e.g., recurrent
relapsing chronic depression, etc.), can be considered candidates for discontinuation of treatment.
QUESTION 9) A 35 year old female returns for a follow visit after you have successfully treated her first episode of uncomplicated
major depression. After 6 weeks of treatment with an antidepressant, all of her depressive symptoms have resolved. Based on the
evidence, the total length of treatment with antidepressants should be at a minimum:
a)
b)
c)
d)
e)
3 months
6 months
9 months
12 months
Indefinite
The correct answer is b. Based on the treatment recommendations of the American Psychiatric Association, this uncomplicated
patient with her first major depressive episode would have had an initial six weeks of antidepressant treatment. This six week
period in the acute phase of treatment has apparently induced complete remission of symptoms. The evidence would recommend
Page 30 of 50
another 16 – 20 weeks of continuation phase treatment. The minimum total length of acute and continuation phase treatment for
this patient would be about 6 months. (Source: Working Group on Major Depressive Disorders. Practice Guidelines for the
Treatment of Patients With Major Depressive Disorder. American Psychiatric Association. 2000. Washington D.C.)
Maintenance Phase Treatment
Between 50 – 85% of patients with a single major depressive episode will have another episode. Maintenance phase treatment is
designed to prevent recurrence. Issues to consider in using maintenance phase treatment are severity of episodes (e.g., suicidal
ideation or attempts, psychotic symptoms, functional impairment); risk of recurrence (e.g., residual symptoms between episodes,
number of recurrent episodes); comorbid conditions; side effects experienced with continuous treatment; or patient preference.
The same treatment that was effective in the acute and continuation phase should be continued in the maintenance phase. The doses of
medication in the previous phases are usually maintained. The type of psychotherapy employed dictates the frequency of visits in the
maintenance phase (e.g., cognitive behavioral therapy and interpersonal therapy decrease to once a month, while psychodynamic
psychotherapy maintains the same previous frequency). Combination therapy (psychotherapy and pharmacotherapy) may be
beneficial for some patients although it is not well studied. Patients with recurrent moderate or severe depressive episodes who don’t
respond well to pharmacotherapy may be candidates for periodic ECT. Frequency of visits in the maintenance phase can vary as in the
continuation phase.
The length of maintenance treatment that is optimal is unknown. Factors that may influence this period may be frequency and severity
of recurrent episodes, persistence of symptoms after a period of recovery, tolerability of treatment, and patient preference. Some
patients may require indefinite maintenance treatment.
Question 10) For which one of the following patients is a trial of discontinuation of antidepressant medication appropriate?
a)
A 30 year old male with is his first lifetime episode of major depression who is now asymptomatic after taking his
medication for 3 months.
b) A 50 year old female with depression and an anxiety disorder with her fourth episode of major depression, which has taken 6
months of medication and is now asymptomatic.
c) A 40 year old male with is third lifetime episode of major depression who has taken medication for 12 months and is now
asymptomatic.
d) A 40 year old female with her first lifetime episode of major depression who is now asymptomatic after taking 12 months of
medication
The correct answer is d. The 40 year old male and 50 year old female with recurrent episodes of major depression may benefit
from longer or indefinite treatment. The 30 year old male with his first episode and who is now asymptomatic after 3 months of
medication has not completed the recommended length of continuation phase treatment. The 40 year old female with her first
Page 31 of 50
lifetime episode of major depression who is now asymptomatic after taking 12 months of medication is the only possible
candidate for a trial of discontinuation but still needs monitoring and education on relapse. (Source: Working Group on Major
Depressive Disorders. Practice Guidelines for the Treatment of Patients With Major Depressive Disorder. American Psychiatric
Association. 2000. Washington D.C.)
Discontinuation of active treatment
VII. Medical
Management of
Depression
The factors to discontinue treatment are based on the same considerations in deciding on using maintenance phase therapy: frequency
and severity of recurrent episodes, dysthymic symptoms between episodes, the presence of other psychiatric disorders, the presence of
chronic general medical disorders, or patient preference. If maintenance pharmacotherapy is discontinued, it is recommended to taper
the medication over several weeks. Slow tapering may allow the physician to detect emerging symptoms and restore the medical
management to full therapeutic doses. Discontinuation syndromes (e.g., mood disturbances, sleep, energy, and appetite) can appear
much like relapses but are in fact due to lack of tapering of medications. Patients on short acting agents are more prone to
discontinuation syndromes and should be tapered over longer periods of time. Signs and symptoms of relapse should again be
reviewed with the patient once discontinuation of treatment has occurred.
First line choices of antidepressant drugs
QUESTION 11) Which one of the following statements is true regarding the effectiveness of antidepressants agents for treating
major depression?
a)
b)
c)
d)
e)
Selective serotonin reuptake inhibitors (SSRIs) are the most effective class of antidepressants.
Tricyclic antidepressants (TCAs) are the most effective class of antidepressants.
Serotonin-norepinephrine reuptake inhibitors are the most effective class of antidepressants.
Monoamine oxidase inhibitors (MAOIs) are the most effective class of antidepressants.
All classes of antidepressants are equally as effective.
The correct answer is e. Although there may be specific class considerations for use of one medication over another for a
particular patient, all classes of antidepressants are equally effective. (Source: Mann, JJ., “The Medical Management of
Depression” New England Journal of Medicine. 2005 Oct 27;353(17):1819-34.; and Working Group on Major Depressive
Disorders. Practice Guidelines for the Treatment of Patients With Major Depressive Disorder. American Psychiatric Association.
2000. Washington D.C.)
Antidepressant medications’ effectiveness is generally comparable across classes and within classes of medications. The medications
differ in side effect profiles, drug-drug interactions, and cost. The history of a positive response to a particular drug for an individual
or a family member, as well as patient preferences, should also be taken into account. Most psychiatrists agree that an SSRI should be
the first line choice. The dual action reuptake inhibitors venlafaxine and bupropion are generally regarded as second line agents.
Tricyclics and other mixed or dual action inhibitors are third line, and MAOI’s (monoamine oxidase inhibitors) are usually
Page 32 of 50
medications of last resort for patients who have not responded to other medications, due to their low tolerability, dietary restrictions,
and drug-drug interactions. Most primary care physicians would prefer that a psychiatrist manage patients requiring MAOI’s.
The recommended starting dose of antidepressants is illustrated in the table below from Mann JJ., “The Medical Management of
Depression” New England Journal of Medicine. 2005 Oct 27;353(17):1819-34. Titration of the drug to therapeutic levels is done over
the initial weeks of treatment. The rate of titration may depend on the patient’s age, the development of side effects, and comorbid
conditions. In the geriatric population, the starting dose is usually half the recommended starting dose for other adults.
Classification, Doses, Safety, Side Effects of Antidepressants
Page 33 of 50
Page 34 of 50
Table reproduced with permission from the Massachusetts Medical Society. Taken from Mann, JJ., “The Medical Management of
Depression” New England Journal of Medicine. 2005 Oct 27;353(17):1819-34. Copyright © 2005 Massachusetts Medical Society. All
rights reserved.
As stated prior, the patient should be monitored over time for improvement, exacerbation of depression, suicidal feelings, side effects,
and adherence. All antidepressants may induce a manic episode in patients susceptible to bipolar disorder. The frequency of
monitoring can vary from once a week to multiple times a week. Monitoring can be done via face-to-face visits, telephone contact via
the physician and patient, or the patient and nursing staff. This can be a challenge in clinical practice, but there are novel approaches
for improving systems for monitoring depressed patients in primary care settings (available in the library of this module).
Page 35 of 50
LINK: Oxman, T., et al. “A Three-Component Model for Reengineering Systems for the Treatment of Depression in Primary Care.”
Psychosomatics 2002; 43:441-450.
Antidepressant Medications
Most antidepressant agents amplify norepinephrine or serotonin signaling by inhibiting their reuptake at the synaptic cleft.
Selective serotonin reuptake inhibitors (SSRIs)
Clinical trials have found little difference in efficacy and tolerability amongst the various SSRIs. SSRIs tend to be well tolerated as
compared with other classes of antidepressants. The half life of all of the SSRIs is long enough to allow for once a day dosing, which
improves patient adherence. Of note, fluoxetine is the only antidepressant found to be effective in controlled trials treating depressed
children and adolescents. SSRIs have fewer cardiovascular effects than tricyclic antidepressants.
Tricyclic antidepressants (TCAs) and Norepinephrine reuptake inhibitors (NRIs)
TCAs and NRIs are older classes of antidepressants. They may be more effective in severe depression or depression with melancholic
features. They may also be more effective than SSRIs for depression that has predominant physical symptoms or pain. TCAs and
NRIs tend to have cardiac conduction effects and thus they are not the drug of choice in patients with cardiovascular conditions,
particularly conduction defects. They are also contraindicated in people with benign prostatic hypertrophy, urinary retention, and
closed angle glaucoma.
Dual action antidepressants
Venlafaxine, milnacipran, duloxetine are serotonin-norepinephrine reuptake inhibitors. They block monoamine transporters much
more selectively than the TCAs and NRIs and thus have less cardiac-conduction effects. Venlafaxine has been shown to be more
effective than SSRIs or TCAs through higher rates of remission in severe depression. Duloxetine is as effective as the SSRI
paroxetine. Both duloxetine and paroxetine are also effective in treating chronic pain and diabetic neuropathy.
Bupropion inhibits norepinephrine and dopamine, but not serotonin, reuptake. It has similar efficacy to TCAs and SSRIs, but has less
diarrhea, nausea, somnolescence, and sexual side effects than SSRIs. Bupropion also can be used as an adjunct in smoking cessation
(although some health insurance companies will pay for buproprion as an antidepressant but not as a smoking cessation medication).
Monoamine oxidase inhibitors (MAOIs)
MAOIs nonselectively block Mao A and B isoenzymes, and have similar efficacy to TCAs. Again, MAOIs are not considered first
line choice due to the side effect profile, drug-drug interactions, and the need to adhere to a low tyramine diet to prevent a
Page 36 of 50
hypertensive crisis. Under the care of a psychiatrist, MAOIs may be more effective than TCAs for atypical depression which is
characterized by extreme fatigue, sensitivity to rejection, or troubled relationships.
Newer antidepressant therapies
Nefazodone blocks 5-HT serotonin receptors thus enhancing serotonin in synaptic clefts. It has an efficacy similar to SSRIs, and tends
to be sedating.
Mirtazapine blocks alpha 2 – adrenergic receptors, specific serotonin receptors, and histamine receptors to enhance norepinephrine in
the synaptic cleft. It is as effective as SSRIs and TCAs. Mirtazapine tends to be quite sedating and to cause significant weight gain.
Considerations before switching antidepressants
As mentioned prior, patients getting the same dose of an antidepressant and not achieving a response should consider having their
antidepressant dose increased before changing the medication altogether. Before the medication is switched, the primary care
physician should reassess the diagnosis; consider increasing the antidepressant dose; assess the patient for adherence; consider
alcoholism or substance-abuse; and re-evaluate for coexisting medical conditions and use of non-psychiatric drugs that may contribute
to treatment failure.
It is generally recommended that patients who don’t have a response to an SSRI should be switched to an antidepressant in another
class. Similarly, if a dual action antidepressant has been used first, a switch to an SSRI should be considered. For patients with a
partial response to one antidepressant, a second antidepressant from another class can be added for augmentation.
Adjunct medications
There are other medications that are used in conjunction with antidepressants to augment their effects. Mood stabilizers, such as
lithium can prevent manic and depressive episodes in bipolar patients. Lithium can also be an effective augmenting agent in patients
who don’t have an effective response to antidepressants alone. Antipsychotic medications can be added to antidepressants to treat
depression with psychotic features.
Anxiety: Antidepressants and Anxiolytics
In major depression with comorbid anxiety or panic disorder (15 – 30% of cases), depression and anxiety symptoms resolve with
antidepressant treatment. SSRIs and TCAs may initially worsen the anxiety. This can be avoided by starting at lower doses and
titrating up more slowly.
Benzodiazepines are used as an adjuvant in 30 - 60% of cases of depression with anxiety or insomnia. Benzodiazepines improve
Page 37 of 50
VIII. Psychotherapeutic
Management of
Depression
antidepressant response, but can cause sedation, memory loss, and dependence and withdrawal syndromes. Benzodiazepines should be
used on a limited basis to avoid dependency; avoided in those with a history of alcohol or drug abuse; and be used with extreme
caution in geriatric populations who don’t metabolize the drugs well and can cause increased cognitive dysfunction, falls, and death.
In general, benzodiazepines should not be used as the primary pharmacologic agent in any patient with major depression and anxiety
disorders.
Psychotherapeutic Management of Depression
Psychotherapy may be a first line therapy choice for mild depression particularly when associated with psychosocial stress,
interpersonal problems, or with concurrent developmental or personality disorders. Psychotherapy in mild to moderate depression is
most effective in the acute phase, and in preventing relapse during continuation phase treatment. Psychotherapy is not appropriate
alone for severe depression, psychosis, and bipolar disorder. For more severe depression, psychotherapy may be appropriate in
combination with the use of medications. The most effective forms of psychotherapy are those with structured and brief approaches
such as cognitive behavioral therapy, interpersonal therapy, and certain problem solving therapies. Regardless of the psychotherapy
initiated, “psychiatric management” must be integrated at the same time. Primary care physicians should be aware of the different
psychotherapy approaches so that they can understand what their patients are undergoing and what goals they are trying to achieve.
Studies indicate that the use of cognitive therapy modalities is most effective (Rupke, 2006); Cognitive behavioral therapy (CBT) is
most frequently cited in studies as highly effective in treating depression. However, interpersonal psychotherapy and problem
oriented psychotherapy have also been considered as desirable and cost effective when compared to more traditional models of
psychotherapy.
Cognitive Behavioral Therapy (CBT)
CBT targets thoughts and behaviors that need to be changed. Based on the premise that behaviors have their roots in thoughts, this
approach assumes that depression is rooted in pessimistic thoughts and excessive self-criticism. The goal of the therapy is to
recognize what triggers certain thoughts and behaviors and to alter your routines through direction and action. Learning to substitute
healthy thoughts for negative thoughts will improve a person’s mood, self-concept, behavior and physical state. Behavior change is
the primary goal with internal change as a byproduct. Initially, in treating depression, behavioral principles are used to overcome a
patient’s inertia and to reinforce positive activities. An important part of CBT for depression is scheduling pleasurable activities,
especially with others, that usually give positive reinforcement. Other CBT techniques include graded tasks and homework
assignments as well as acting out difficult behavioral situations. Emphasis is on the present rather than on the past. The combination
of CBT and antidepressants has been shown to effectively manage severe or chronic depression and for adolescents with depression.
CBT has been shown to reduce relapse rates and effectively manage residual symptoms.
LINK TO LIBRARY ARTICLE: “Cognitive Therapy” AAFP
Interpersonal Therapy (IPT)
Page 38 of 50
Based on the belief that depression is caused by problems in important interpersonal relationships, this approach focuses on teaching
about the connection between interpersonal problems and depression. Depression is viewed as arising out of conflict or loss in
interpersonal relationships. A key feature is the compiling of an interpersonal inventory that lists and examines all the patient’s
relationships. In this approach the number of sessions is generally limited over a period of several months. Treatment is divided into
three stages: assessment, practice and termination, with emphasis on relapse prevention skills and techniques. Focus is on present
events rather than past history and on learning ways to improve important relationships in the present and to have more positive
interactions. Patients are taught not only to identify but to deliberately tolerate feelings. According to this model, as relationships
improve, so should the patient’s mood. The model incorporates psychoeducation; is “medication friendly”; and agrees with a medical
model of depression. Unlike CBT, IPT does not involve formal homework or rely on extensive paperwork, although patients are
encouraged to develop skills and experiment between sessions. IPT is particularly useful for patients who find psychodynamic
approaches mystifying, and has been modified for use with adolescents.
Problem Solving Therapy (PST)
IX. Other Therapies
Problem solving therapy is a brief, focused form of cognitive therapy that focuses on the problems a person is currently facing and on
helping to find solutions to these problems. Based on studies that have demonstrated links between poor problem solving abilities
and the etiology and maintenance of psychological disorders, this approach is often used in the treatment of depression. Problem
focused methods involve changing the situation itself, whereas emotion-focused strategies involve changing one’s reaction to the
situation. Problem solving strategies work well in addressing and solving problems encountered in everyday situations where a
change in behavior can have positive results. Individuals are taught to identify, discover and invent effective responses for specific
problematic situations. The goal is to provide clients with a set of tools on how to effectively manage life’s stress in order to decrease
distress, enhance sense of control, and improve quality of life. Interventions include didactic explanations, training exercises, practice
opportunities, and homework to practice between sessions. PST sessions are often conducted in groups as well as individual sessions.
It is often less expensive than other forms of treatment and can easily be performed by health care professionals. PST has been shown
to be effective in treating depression in adults of all ages and is thought to be particularly effective in treatment of older adults.
Other Therapeutic Options
Combination of medications and psychotherapy
There are very few clinical trials to guide with a specific selection of the optimal combination of antidepressants and psychotherapy.
The same considerations in selecting monotherapy of antidepressants or psychotherapy apply. Monitoring with the same frequency for
side effects, efficacy, adherence, and safety are the same in combination as when either therapy is given alone. If after 4 – 8 weeks
there is not a moderate improvement in baseline symptoms, then a reassessment of the diagnosis, medication regimen, adherence,
substance or alcohol use is in order. Change in treatment can be considered. If 4 – 8 weeks after the change in treatment there is not a
moderate improvement in symptoms, another review should occur. Other treatment options should be considered in consultation with
a psychiatric specialist if the patient fails to respond.
Page 39 of 50
Electroconvulsive therapy (ECT)
ECT is exclusively available through an experienced psychiatric specialist. Remission rates with ECT are around 60 – 80 percent in
severe major depressive disorder (UK ECT Review Group, Lancet 2003), and the maximum response is usually 3 weeks after
treatment. ECT is the first line treatment when there is severe depression with psychotic features, psychomotor retardation, or
resistance to medications. Suicidal patients and pregnant patients may also have rapid benefits from ECT. ECT consists of 6 – 12
treatments (2 to 3 times a week). Because the relapse rate after ECT is more than 50 percent, most psychiatrist start prophylactic
treatment with antidepressants and adjuvant medications such as lithium. Postictal confusion, retrograde and anterograde memory
impairment usually improves in a few days.
St. John’s wort
QUESTION 12) A 35 year old male who is HIV positive, takes antiretroviral medications, and lives with severe major depression has
achieved remission of his depression on his SSRI but complains of lack of sexual libido. He read some information about St. John’s
wort and asks if it would be appropriate to treat his depression. Which one of the following statements is appropriate advice to this
patient:
a)
b)
c)
d)
e)
St. John’s wort is more effective than placebo in patients with severe major depression.
St. John’s wort is not effective for treatment of major depression.
St. John’s wort is safe for use in people taking HIV antiretroviral medications.
St. John’s wort is safe and effective in combination with SSRIs and TCAs.
St. John’s wort is safe and effective in combination with MAOIs.
The correct answer is b. St. John’s wort is a plant product commonly used to treat depression. Although two dozen trials have
Page 40 of 50
been conducted on the use of St. John’s wort in depression, most have had significant flaws in design and do not enable
meaningful interpretation. The results of a randomized, double-blind, placebo-controlled clinical trial conducted between
November 1998 and January 2000 in 11 academic medical centers in the United States with 200 participants found that St. John’s
wort was not effective in the treatment of major depression (Sources: Shelton RC, Keller M, Gelenberg A, et al. Effectiveness of
St. John’s wort in major depression: a randomized controlled trial. JAMA. 2001 (15); 285: 1978-1986). Information on
combination of St. John’s wort and SSRIs and TCAs is unknown. St. John’s wort and combination of MAOIs is contraindicated.
(Working Group on Major Depressive Disorders. Practice Guidelines for the Treatment of Patients With Major Depressive
Disorder. American Psychiatric Association. 2000. Washington D.C.) St. John’s wort is not a drug and thus is not regulated by
the FDA, thus there is a lack of standardized preparations. Patients living with HIV / AIDS and on antiretroviral treatment should
be made aware that St. John’s wort is contraindicated because it lowers the serum levels of their antiretroviral cocktail.
ST JOHNS WORT LINK PDF: National Center for Complementary and Alternative Medicine. Herbs At A Glance: St. John’s Wort.
National Center for Complementary and Alternative Medicine Web site. National Institutes of Health. Accessed at
http://nccam.nih.gov/health/stjohnswort
LINK: : Shelton RC, Keller M, Gelenberg A, et al. Effectiveness of St. John’s wort in major depression: a randomized controlled trial.
JAMA. 2001 (15);285: 1978-1986
X. Living With
Depression
Living With Depression
The Personal Experience
Page 41 of 50
“Self Portrait” – Frida Kahlo
LINK: Frida Kahlo (Wikipedia: http://en.wikipedia.org/wiki/Frida_Kahlo)
Patients living with depression have enormous obstacles to overcome. Recognizing in oneself the symptoms and signs of depression
can be difficult. People who suffer from depression describe the experience as a feeling of isolation, a feeling of being cut off from the
people around them, almost of being “emotionally underwater”, of losing interest in physical contact and in sexual relationships, and
of excessive worry. They may lack any energy in getting out of bed or to leave home. They may become emotionally distant and not
talk to others. They may blame themselves for a moral defect for persistently feeling down. Although some may become aware their
feelings are not normal, they may not want to seek help due to fear of stigma or fear of institutionalization. Cultural and social factors
may make it even more difficult to seek help. In some cultures, it is not appropriate to discuss feeling depressed or may be seen as an
“imaginary disease”. Men may feel that being depressed is a sign of weakness, and because discussing feelings is not “masculine” –
may make males feel even more isolated. Depression is an agonizing experience.
Page 42 of 50
HANDOUTS for SPECIAL POPULATIONS
Mens Guide
Womens Guide
Latino Americans
Asian Americans
African Americans
Native Americans
VIDEO CLIP OF CBS CORRESPONDANT FROM BACKPACK FULL OF BRICKS
With treatment and education, persons with depression can have functional and meaningful lives. It requires ongoing personal
acknowledgement of the illness, and surveillance and recognition of signs. It requires the support of family and friends. A
compassionate and vigilant primary care physician should also be part of depression monitoring and support.
The Effect On Families
The effect and impact on family, friends, and coworkers of a person who suffers from depression can be tremendous. Their families
and friends may not recognize depressive symptoms, or dismiss the signs as either a normal reaction to life events, or ascribe the
symptoms as the person being “difficult” or “moody”. Some friends and families may stop socializing with a depressed loved one
because the experience can be difficult or frustrating. They may begin to resent the depressed person. Even when depression is
evident, families and friends may believe that a person can just “stop” being depressed, or that the person with depression is “acting
out” at them. Others may think that they may be the sole solution to solving their loved one’s depression (e.g., “Maybe if I do things
differently? Maybe if I can kid them out of their depression? Maybe if we went on vacations more often?”), or may suffer tremendous
guilt about the situation. It can be difficult for families to accept the illness. Some families become socially isolated over secrecy over
their loved one’s condition. Families and friends benefit by learning about the illness of depression, and understanding what is not in
their control and how they can be supportive. Support groups for friends and families of those living with depression also exist.
Family and friends also have to find time to take care of themselves. Primary care physicians can be very effective in education and
providing support to family and friends.
VIDEO CLIP OF FAMILY EXPERIENCE FROM BACKPACK FULL OF BRICKS
Patient and Family Education Resources
LINK
http://www.familyaware.org/
Page 43 of 50
Wellness Guide for Patients With Depression and Their Friends and Families PDF
The Arts and Depression
The arts have long explored the experience of living with depression and its’ effects on others. Film, plays, books, and art can provide
us with window into the world of a person coping with chronic depression and associated mental health illnesses. A physician can
learn much empathy and compassion for these persons thorough these powerful artistic expressions.
Film
“Ordinary People” (1980)
Director: Robert Redford
LINK: http://www.imdb.com/title/tt0081283/
“Pollock” (2000)
Director: Ed Harris
LINK: http://www.imdb.com/title/tt0183659/
“The Snake Pit” (1948)
Director: Anatole Litvak
LINK: http://www.imdb.com/title/tt0040806/
“Sophie's Choice” (1982)
Director: Alan Pakula
LINK: http://www.imdb.com/title/tt0084707/
“Reality Bites” (1994)
Director: Ben Stiler
LINK: http://www.imdb.com/title/tt0110950/
“Wild Strawberries” (1957)
Director: Ingmar Bergman
LINK: http://www.imdb.com/title/tt0050986/
Plays
“Monster in A Box” (1992) – LINK TO VIDEO CLIP FROM BACKPACK FULL OF BRICKS
Page 44 of 50
“Gray’s Anatomy” (1994)
Playwright: Spalding Gray
“Proof” (2001)
Playwright: David Auburn
“4.48 Psychosis” (1999)
Playwright: Sarah Kane
Books
“The Bell Jar” (1963)
Author: Sylvia Plath
“The Sorrows of Young Werther” (1774)
Author: Johann Wolfgang von Goethe
“Unholy Ghost: Writers on Depression” (2002)
Edited by: Nell Casey
“Girl Interrupted” (1994)
Author: Susanna Kaysen
“One True Thing” (2006)
Author: Anna Quindlen
Arts
XI. Conclusion
“On the Threshold of Eternity / At Eternity’s Gate / Old Man in Sorrow” - Vincent Van Gogh
“The Scream” – Edvard Munch
“Self Portrait” – Frida Kahlo
Summary
Depression is one of the most common conditions in primary care, but is often unrecognized, undiagnosed, and untreated. Depression
has a high rate of morbidity and mortality when left untreated. Most patients suffering from depression do not complain of feeling
depressed, but rather anhedonia or vague unexplained symptoms. All physicians should remain alert to effectively screen for
depression in their patients. There are several screening tools for depression that are effective and feasible in primary care settings. An
Page 45 of 50
appropriate history, physical, initial basic lab evaluation, and mental status examination can assist the physician in diagnosing the
patient with the correct depressive spectrum disorder (including bipolar disorder). Primary care physicians should carefully assess
depressed patients for suicide. Depression in the elderly is not part of the normal aging process. Patients who are elderly when they
have their first episode of depression have a relatively higher likelihood of developing chronic and recurring depression. The
prognosis for recovery is equal in young and old patients, although remission may take longer to achieve in older patients. Elderly
patients usually start antidepressants at lower doses than their younger counterparts.
Most primary care physician can successfully treat uncomplicated mild or moderate forms of major depression in their settings with
careful psychiatric management (e.g., close monitoring of symptoms, side effects, etc.); maintaining a therapeutic alliance with their
patient; pharmacotherapy (acute, continuation, and maintenance phases); and / or referral for psychotherapy. The following situations
require referral to psychiatrist: suicide risk, bipolar disorder or a manic episode, psychotic symptoms, severe decrease in level of
functioning, recurrent depression and chronic depression, depression that is refractory to treatment, cardiac disease that requires
tricyclic antidepressants treatment, need for electroconvulsive therapy (ECT), lack of available support system, and any diagnostic or
treatment questions.
Antidepressant medications’ effectiveness is generally comparable across classes and within classes of medications. The medications
differ in side effect profiles, drug-drug interactions, and cost. The history of a positive response to a particular drug for an individual
or a family member, as well as patient preferences, should also be taken into account. Most psychiatrists agree that an SSRI should be
the first line choice. The dual action reuptake inhibitors venlafaxine and bupropion are generally regarded as second line agents.
Tricyclics and other mixed or dual action inhibitors are third line, and MAOI’s (monoamine oxidase inhibitors) are usually
medications of last resort for patients who have not responded to other medications, due to their low tolerability, dietary restrictions,
and drug-drug interactions. Most primary care physicians would prefer that a psychiatrist manage patients requiring MAOI’s.
Psychotherapy may be a first line therapy choice for mild depression particularly when associated with psychosocial stress,
interpersonal problems, or with concurrent developmental or personality disorders. Psychotherapy in mild to moderate depression is
most effective in the acute phase, and in preventing relapse during continuation phase treatment. Psychotherapy is not appropriate
alone for severe depression, psychosis, and bipolar disorders. For more severe depression, psychotherapy may be appropriate in
combination with the use of medications. The most effective forms of psychotherapy are those with structured and brief approaches
such as cognitive behavioral therapy, interpersonal therapy, and certain problem solving therapies. Regardless of the psychotherapy
initiated, “psychiatric management” must be integrated at the same time.
Patients, who live with depression, and their family and friends, have enormous challenges to overcome. Primary care physicians can
provide compassionate care, important education, psychiatric monitoring, social support, reassurance, and advocacy for these patients
and their loved ones.
XII. Bibliography
Link To Survey Monkey Feedback and Content Questions
Bibliography
Page 46 of 50
Ables, A. et al. “Antidepressants: Updates on New Agents and Indications” Am Fam Physician. 2003; 67:547-54.
American Broadcasting Company. “Depression: A Backpack Full of Bricks”. March 9, 2004. Films For Humanities and Sciences.
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, ed 4 text revision, American Association,
2000. Washington DC
Birrer, RB, Vemuri SP. Depression in later life: A diagnostic and therapeutic challenge. Am Fam Physician 2004; 69 (10): 2375-2382
Cutler, J. Charon, R. “Depression” from Primary Care Psychiatry and Behavioral Medicine: Brief Office Treatment and Management
Pathways. Edited by RE Feinstein, AA Brewer. Springer Publishing Co., New York, NY. 1999
Dietrich, A., et al. “Re-engineering systems for the treatment of depression in primary care: cluster randomized controlled trial.” BMJ
2004;329
Gaynes, B., et al. “Screening for Suicide Risk in Adults: A Summary of the Evidence for the U.S. Preventive Services Task Force”
Ann Intern Med. 2004; 140:822-835.
Jick SS, Dean AD, Jick H. Antidepressants and suicide. BMJ 1995; 310 (6974): 215-218.)
Kahn, David. “Mood Disorders”. Psychiatry, edited by JL Cutler, ER Marcus. WB Saunders, Philadelphia, PA. 1999
Lewis-Fernandez, R. et al., “Depression in US Hispanics: Diagnostic and Management Considerations in Family Practice” J Am
Board Fam Pract 2005;18: 282–96.
Mann, JJ., “The Medical Management of Depression” New England Journal of Medicine. 2005 Oct 27;353(17):1819-34
Morris, Jane, “Interpersonal psychotherapy – a trainee’s ABC?” in Psychiatric Bulleting (2002), 26, 26-28.
National Center for Complementary and Alternative Medicine. St. John’s Wort and the Treatment of Depression. National Center for
Complementary and Alternative Medicine Web site. Accessed at http://nccam.nih.gov/health/stjohnswort on June 30, 2005.
New York City Department of Health and Mental Hygiene. “Detecting and Treating Depression in Adults.” City Health Information.
25 (1): 1-8.
Nezu, Arthur, et al., “Managing Stress through Problem Solving” in STRESS NEWS, Vol. 13 No.3, July
Page 47 of 50
Oxman, T., et al. “A Three-Component Model for Reengineering Systems for the Treatment of Depression in Primary Care.”
Psychosomatics 2002; 43:441-450.
Reid, Cary M., Ph.D., M.D., “Determining the Feasibility of a Cognitive-Behavioral Therapy for the Treatment of Co-Occurring
Chronic Back Pain and Depression Among Persons Ages 60 Years and Above” Aetna INteliHealth: Depression July 12, 2005
(www.intelihealth.com)
Remick, R. “Diagnosis and management of depression in primary care: a clinical update and review.” CMAJ 2002;167(11):1253-60
Rost. K., et al. “Managing Depression as a Chronic Disease; a randomized trial of ongoing treatment in primary care.” BMJ October
2002; 325
Rupke, Stuart, et al., “Cognitive Therapy for Depression” Am Fam Physician, 2006: 73, 83-86
Sharp, LK, Lipsky MS. “Screening for depression across the lifespan: a review of measures for use in primary care settings.”
American Family Physician. 2002; 66: 1001-1008
Shearer, S., et al. “Excessive Worry.” Am Fam Physician 2006;73:1049-56, 1057-8.
Shelton RC, Keller M, Gelenberg A, et al. “Effectiveness of St. John’s wort in major depression: a randomized controlled trial.”
JAMA. 2001 (15);285: 1978-1986
Simon GE., “How can we know whether antidepressants increase suicide risk?” Am J Psychiatry 163:1861-1863, 2006.
The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990
and projected to 2020. Vol. 1 Cambridge, Mass.: Harvard University Press, 1996.
Thimbault, J., et al. “Efficient Identification of Adults with Depression and Dementia.” Am Fam Physician 2004;70:1101-10.
UK ECT Review Group, Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and metaanalysis. Lancet 2003; 361: 799-808.
United States Preventive Screening Task Force. Screening for depression: Recommendations and rationale. November 2006
Recommendations. http://epss.ahrq.gov/PDA/index.jsp
Ward, R. Zamorski, M. “Benefits and Risks of Psychiatric Medications in Pregnancy” Am Fam Physician. 2002;66:629-36,639.
Page 48 of 50
Working Group on Major Depressive Disorders. Practice Guidelines for the Treatment of Patients With Major Depressive Disorder.
American Psychiatric Association. 2000. Washington D.C.
Credits
Written and Created by Pablo Joo MD
Center for Family Medicine – New York Presbyterian / Columbia University College of Physicians and Surgeons
Director of Predoctoral Education
Contributing Writer: “Psychotherapeutic Management of Depression” segment
Cathie Vourkas, ACSW
Behavioral Scientist, Center for Family Medicine
New York Presbyterian / Family Medicine Residency Program
Contributing Writer: “First line choices of antidepressant drugs” segment
Janis Cutler, MD, Dept. of Psychiatry
New York Presbyterian / Columbia University College of Physicians and Surgeons
Creative Direction and Production
Michelle V. Hall
Columbia Center for New Media, Teaching and Learning – Columbia University
Medical Education Curriculum and Research Contributor
Sharon K. Krackov, Ed.D
Center for Education Research and Evaluation – Columbia University Medical Center
Contributing Editors
Janis Cutler, MD, Dept. of Psychiatry
New York Presbyterian / Columbia University College of Physicians and Surgeons
Edgar Figueroa MD, MPH, Family Medicine
Director of Student Health Services
Weill Medical College of Cornell University
Columbia P&S Primary Care Clerkship Co-Directors
Primary Care Clerkship Co-directors
Rebecca Kurth MD – Department of Medicine
Page 49 of 50
Pablo Joo MD – Center for Family Medicine
New York Presbyterian / Columbia University College of Physicians and Surgeons
This Columbia P&S Primary Care Clerkship Web Education Module was made possible by a generous grant the Columbia University
Primary Care Education and Research Gift Fund.
Page 50 of 50