King Saud University
advertisement

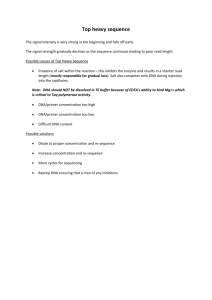
المملكة العربية السعودية وزارة التعليم العالي جامعة الملك سعود عمادة البحث العلمي مركز بحوث........... نموذج طلب دعم مشروع بحثي للدراسات العليا عنوان البحث : تأثير الديكسرازوكسان على عدم االستقرار الكروموسومي المستحث بواسطة االتوبوسيد فى الفئران اسم الطالب أو الطالبة والقسم :أالء أحمد العنتيت كلية الصيدلة قسم علم األدوية اسم المشرف :الدكتور صبري محمد عطية الميزانية المقترحة :سبعين ألف لاير ملخص البحث مشكلة البحث :ان معالجة السرطان في السنوات األخيرة اصبحت تعتمد بشكل أساسي على السمية الخلوية للعالج الكيمياوي .وبما أن استخدام األدوية المتفاعلة مع انزيمات توبوأيزومرازمن النوع الثاني أثبتت فعاليتها في تحسين حياة مرضى السرطان فقد شاع استخدامها كثيرا بالرغم من وجود دراسات عديدة أثبتت بأن هذه األدوية تسبب طفرة في الخاليا والتي تتطور الى سرطان من نوع ثاني أو ممكن ان تصبح مقاومة لعالج الدواء او ظهور نسل غير طبيعي أهمية البحث :لذلك من المهم ان نحدد تطور وخطورة تلك الطفرات في الخاليا بسبب استخدام هذه االدوية وبأعتبارنا لالستخدام الشائع لدواء االتوبوسيد في عالج السرطان وقدرة دواء الديكسرازوكسان على تحسين فعالية العالج مع االتوبوسيد .هذا قد حفزنا لنبحث بأمكانية الديكسرازوكسان في تحسين عدم االستقرار الكرومسوي المحدث باالتوبوسيد في الخاليا الطبيعية للفئران .وذلك ممكن أن يسمح لنا بزيادة الجرعات لمرضى السرطان بشكل امن وقتل أكثر للخاليا السرطانية مع حماية الخاليا الغير خبثة من االثار الجانبية لعقار االتوبوسيد. أهداف البحث :تحديد امكانية الديكسرزوكسان بحماية الخاليا الطبيعية من تأثير األتوبوسيد على عدم االستقرار الجيني فيها وذلك بقياس -1طفرة الكروموسونات -2تكون النوية في خاليا نخاع العظام -3حيوية االنقسام في طور الميتا والنترفاس -4عامل األكسدة – 5موت الخاليا المنظم ()apoptosis منهج البحث تحديد الطفرة على شكل و عدد الكروموسومات باستخدام المجهر الضوئي ,تكون النوية في خاليا نخاع العظام باستخدام المجهر الضوئي ,تحديد عامل االكسدة باستخدام جهاز سبكتروفوتوميتر ,قياس موت الخاليا باستخدام جهاز الفلوسيتوميتر King Saud University College of Pharmacy Department of Pharmacology INFLUENCE OF DEXRAZOXANE ON ETOPOSIDEINDUCED CHROMOSOMAL INSTABILITY IN MICE تأثير الديكسرازوكسان على عدم االستقرار الكروموسومي المستحث بواسطة االتوبوسيد فى الفئران Master Research Proposal Submitted to the Department of Pharmacology By Alaa A. Al-Anteet أالء أحمد العنتيت B. Pharm (2004) 1429 (H) 2008 (G) 1 1. Introduction 1.1. Topoisomerases inhibitors Topoisomerase II is an essential enzyme which alters DNA topology by transiently creating and resealing DNA double strand breaks to enable the passage of one DNA strand through another [1]. DNA topoisomerase II is a target for a number of clinically useful anti-tumour agents, in part because it is essential for cell survival. To date, there are two general classes of topoisomerase II inhibitors that interfere with enzyme catalysis at distinct points of the enzyme reaction. DNA topoisomerase II inhibitors, such as etoposide, amsacrine and doxorubicin stabilize cleaved DNAtopoisomerase II complexes. In contrast to the complex-stabilizing topoisomerase II inhibitors, merbarone and the bisdioxopiperazines (such as dexrazoxane) block the catalytic activity of the enzyme [1, 2, 3]. Specifically, the bisdioxopiperazines have been reported to stabilize topoisomerase II in a closed-clamp configuration around the DNA, whereas agents such as merbarone have been implicated recently in blocking the topoisomerase II-mediated DNA cleavage reaction. Because these drugs do not stabilize DNA-topoisomerase II complexes (i.e., they do not induce DNA strand breaks), they are termed “catalytic inhibitors” of topoisomerase II [2]. 1.2. Topoisomerase II inhibitors induce chromosomal instability In fact, after application of topoisomerase II poisons, damage to DNA may result as DNA fragmentation, chromosomal breaks, and micronucleus formation causing chromosomal instability, and may lead to mutagenesis, carcinogenesis, or finally to apoptotic cell death [4, 5] [Fig. 1]. Follow-up studies of patients who received topoisomerase II inhibitors therapy revealed an increased incidence of acute myeloid leukaemia characterized by site-specific rearrangements in the mixed multiple leukaemia gene on chromosome 11q23 [6]. In addition, a significant increase in the frequency of aneuploid sperm during the first 18 months following initiation of topoisomerase II poisons-including regimen was reported [7]. In animals, topoisomerase II poisons are somatic and germ-cell mutagens capable of inducing both numerical and structural chromosome aberrations [8-14]. Such events may have important consequences in cancer chemotherapy. Firstly, mutations induced in somatic cells may lead to the development of secondary tumours from cells that were not originally neoplastic. Secondly, induced somatic mutations may lead to drug resistance, limiting 2 further therapeutic response. Thirdly, mutations induced in germ cells may be transmitted to the progeny and pose a genetic hazard to future generations. The majority of the literature has described catalytic inhibitors which produce low levels of topoisomerase II-mediated DNA cleavage as having only modest or even no clastogenic activity [15, 16]. In contrast, in a few studies measuring chromosomal alterations, merbarone has been reported to produce significant genotoxic effects both in vivo and in vitro [17, 18]. Additionally, in a few studies measuring chromosomal damage, dexrazoxane has been reported to produce significant genotoxic effects in vitro [18, 19]. However, to our knowledge, the in vivo genotoxic effects of dexrazoxane have never been reported. Catalytic Inhibitors Topoisomerase Poisons Normal Cell Growth Dexrazoxane High Low Etoposide Abnormal Growth Chromosomal instability Cell Death Mitotic failure and apoptosis Figure 2. DNA topoisomerase II: an essential enzyme and cellular toxins [5]. 1.3. Dexrazoxane Dexrazoxane was originally developed as an anti-tumour agent. However, dexrazoxane now is clinically used to reduce doxorubicin-induced cardiotoxicity [20]. Since dexrazoxane is effective in inhibiting doxorubicin’s ability to damage cardiac cells, there are concerns that the drug may, as a protective agent, diminish the effectiveness of various chemotherapeutics. There is some clinical and in vitro data supporting this concern. Hasinoff et al. [21] demonstrated that if Chinese hamster ovary cells are exposed to dexrazoxane in vitro prior to the administration of doxorubicin, a significant antagonism of the anti-tumour activity occurs. Alternatively, they showed that if dexrazoxane is administered simultaneously with or after doxorubicin, significant additive growth inhibitory effects occur [21]. Additionally, Holm et al. [22] reported that dexrazoxane rescued healthy mice from lethal doses of etoposide. Using an L1210 intracranial inoculation model in mice, Holm and his colleagues have shown that the 3 LD10 of etoposide in mice increased 3.6-fold when used together with non-toxic dexrazoxane doses. Also, there was a significant increase in lifespan of mice treated with etoposide and dexrazoxane as compared to etoposide alone. They concluded that tumour cells in the brain were reached by cytotoxic levels of etoposide, whereas normal tissues in the periphery were protected by dexrazoxane. This is because the lipophilic drug etoposide passes the blood-brain barrier to a much greater extent than the hydrophilic drug dexrazoxane. Moreover, combining etoposide and dexrazoxane synergizes with radiotherapy and improves survival in mice with central nervous system tumours [23]. The improved survival from radiotherapy following dexrazoxane and etoposide is difficult to be explained, however, a pharmacokinetics based explanation is attractive. The prolonged co-exposure of the cerebral tumour to etoposide and low concentrations of dexrazoxane enhance the outcome from radiotherapy whereas, extracerebrally, the much higher dexrazoxane concentration counteracts the toxic myelosuppression effects [24]. 1.4. Mechanisms of antimutagens Antimutagens are compounds capable of lowering the frequency of mutations. They have diverse mechanisms of action, such as activating cellular systems which intercept and detoxify mutagens, decreasing genotoxic agent uptake and transport, stimulating DNA damage repair, and/or elimination of heavily damaged cells via apoptosis [25]. 2. Hypothesis: The hypothesis of providing protection against chromosomal instability in nontumour tissues will represent a promising approach of attacking the unwanted toxicity from conventional cytotoxic chemotherapy, this will allow the safe use of increased drug doses for the benefit of future cancer patients. 3. Rational of the Investigation: Considering the widespread use of etoposide in clinical oncology and the ability of dexrazoxane to improve the therapeutic outcome from etoposide prompt the investigation of whether dexrazoxane in combination with etoposide can ameliorate etoposide-induced chromosomal instability in mice normal tissues. 4 3. Research Objectives: The objectives of the current investigation are: 3.1. To determine whether dexrazoxane can protect against chromosomal instability induced by etoposide in mice genotoxically-damaged cells by mitotic chromosomal aberrations, micronuclei formations and mitotic activity at both metaphase and interphase stages. 3.2. The possible mechanisms underlying this amelioration will be assessed by oxidative damage and apoptosis. 4. Materials and Methods: 4.1. Animals: Experiments will be performed with male Swiss albino mice (SWR) aged 6-10 weeks and weighing 25-30 g. Animals will be obtained from the Experimental Animal Care Center, King Saud University and will be maintained on a 12 h light/dark cycle with mouse standard pellet food and water ad libitum. All experiments on animals will be carried out according to the Guidelines of the Animal Care and Use Committee, King Saud University, Kingdom of Saudi Arabia. 4.2. Chemicals: Etoposide and dexrazoxane will be obtained from the Developmental Therapeutics Program, National Cancer Institute, Bethesda, MD, USA. Etoposide will be dissolved in 10% DMSO and dexrazoxane will be dissolved in 0.9% NaCl. All other chemicals and reagents will be of analytical grade. 4.3. Experimental protocol: Animals will be randomly assigned into 16 groups of 10 mice each, as follows: Group 1: mice will serve as a control group and will be intraperitoneally (i.p.) injected with 10% DMSO in 0.9% NaCl. Group 2: mice will be i.p. injected with 40 mg/kg cyclophosphamide as a positive control mutagen. Groups 3-6: mice will be i.p. injected with etoposide in 4 doses (0.5, 1, 10 or 20 mg/kg). Groups 7-8: mice will be i.p. injected with dexrazoxane in 2 doses (125 or 250 mg/kg). 5 Groups 9-12: mice will be i.p. injected with 125 mg/kg dexrazoxane 30 min before etoposide 0.5, 1, 10 or 20 mg/kg treatment. Group 13-16: mice will be i.p. injected with 250 mg/kg dexrazoxane 30 min before etoposide 0.5, 1, 10 or 20 mg/kg treatment. 10% DMSO have previously been shown to be non-mutagen in mice [9, 10]. The doses of etoposide were selected on the basis of its effectiveness in inducing mutations in mice [8-14] and the selected doses are within the dose range used for human chemotherapy [26]. Doses of 125 and 250 mg/kg dexrazoxane have previously been shown to be the optimal protective doses against etoposide-induced myelosuppression and weight loss toxicities in mice and is corresponding to a clinically relevant dose in humans of 375 mg/m2 [24]. All drugs will be administered within 1 h following preparation. The animals will be sacrificed by cervical dislocation 24 h after administration of etoposide to estimate the following parameters; 1. Bone marrow mitotic chromosomal aberrations, micronuclei formations and mitotic activity: will be performed according to the modified techniques of Adler [27]. 2. Oxidative damage: will be assessed by measuring the reduced glutathione level according to the protocol described by Tietze [28]. 3. Apoptosis: it will be measured by using annexin V detection kit according to the methods of Vermes et al. [29]. 4.4. Statistical Analysis: Significant differences of mean percentage between individual treatment groups and solvent control or between the two treatment groups (etoposide alone or etoposide plus dexrazoxane) will be determined on an animal to animal basis by the non-parametric Mann-Whitney U-test and ChiSquare test [30]. Differences between groups will assessed by one way analysis of variance using the GraphPad InStat software package for Windows. Results will be considered significantly different if the p value is 0.05. 6 5. References: [1] J. C. Wang. DNA topoisomerases. Annu. Rev. Biochem. 65, 635-92 (1996). [2] T. Andoh, R. Ishida. Catalytic inhibitors of DNA topoisomerase II. Biochim. Biophys. Acta. 1400(1-3), 155-71 (1998). [3] A. K. Larsen, A. E. Escargueil, A. Skladanowski. Catalytic topoisomerase II inhibitors in cancer therapy. Pharmacol. Ther. 99(2), 167-81 (2003). [4] R. E. Smith. Risk for the development of treatment-related acute myelocytic leukemia and myelodysplastic syndrome among patients with breast cancer: review of the literature and the National Surgical Adjuvant Breast and Bowel Project experience. Clin. Breast Cancer 4(4), 273-9 (2003). [5] S. M. Attia. Mutagenicity of some topoisomerase II-interactive agents. S. P. J. 16(1), 1-24 (2008). [6] C. A. Felix. Leukemias related to treatment with DNA topoisomerase II inhibitors. Med. Pediatr. Oncol. 36(5), 525-35 (2001). [7] P. De Mas, M. Daudin, M. C. Vincent, G. Bourrouillou, P. Calvas, R. Mieusset, L. Bujan. Increased aneuploidy in spermatozoa from testicular tumour patients after chemotherapy with cisplatin, etoposide and bleomycin. Hum. Reprod. 16, 1204-8 (2001). [8] F. Marchetti, F. S. Pearson, J. B. Bishop, A. J. Wyrobek. Etoposide induces chromosomal abnormalities in mouse spermatocytes and stem cell spermatogonia. Hum. Reprod. 21(4), 888-95 (2006). [9] S. M. Attia, T. E. Schmid, O. A. Badary, F. M. Hamada, I.-D. Adler. Molecular cytogenetic analysis in mouse sperm of chemically induced aneuploidy: studies with topoisomerase II inhibitors. Mutat. Res. 520, 1-13 (2002). [10] S. M. Attia, U. Kliesch, G. Schriever-Schwemmer, O. A. Badary, F. M. Hamada, I.-D. Adler. Etoposide and merbarone are clastogenic and aneugenic in the mouse bone marrow micronucleus test complemented by fluorescence in situ hybridization with the mouse minor satellite DNA probe. Environ. Mol. Mutagen. 41, 99-103 (2003). [11] S. M. Attia, O. A. Badary, F. M. Hamada, M. H. de Angelis, I.-D. Adler. The chemotherapeutic agents nocodazole and amsacrine cause meiotic delay and non-disjunction in spermatocytes of mice. Mutat. Res. 651, 105-13 (2008). [12] S. D. Turner, S. W. Wijnhoven, H. Tinwell, L. S. Lashford, J. A. Rafferty, J. Ashby, H. Vrieling, L. J. Fairbairn. Assays to predict the genotoxicity of the 7 chromosomal mutagen etoposide-focussing on the best assay. Mutat. Res. 493, 139-47 (2001). [13] R. C. Choudhury, A. K. Palo, P. Sahu. Cytogenetic risk assessment of etoposide from mouse bone marrow. J. Appl. Toxicol. 24(2), 115-22 (2004). [14] K. Agarwal, A. Mukherjee, S. Sen. Etoposide (VP-16): cytogenetic studies in mice. Environ. Mol. Mutagen. 23(3), 190-3 (1994). [15] M. Chen, W. T. Beck. Differences in inhibition of chromosome separation and G2 arrest by DNA topoisomerase II inhibitors merbarone and VM-26. Cancer Res. 55, 1509-16 (1995). [16] F. H. Drake, G. A. Hofmann, S. M. Mong, J. O. Bartus, R. P. Hertzberg, R. K. Johnson, M. R. Mattern, C. K. Mirabelli. In vitro and intracellular inhibition of topoisomerase II by the antitumor agent merbarone. Cancer Res. 49(10), 257883 (1989). [17] M. Kallio, J. Lähdetie. Effects of the DNA topoisomerase II inhibitor merbarone in male mouse meiotic divisions in vivo: cell cycle arrest and induction of aneuploidy. Environ. Mol. Mutagen. 29, 16-27 (1997). [18] G. Boos, H. Stopper. Genotoxicity of several clinically used topoisomerase II inhibitors. Toxicol Lett. 116(1-2), 7-16 (2000). [19] L. Wang, D. A. Eastmond. Catalytic inhibitors of topoisomerase II are DNAdamaging agents: induction of chromosomal damage by merbarone and ICRF187. Environ. Mol. Mutagen. 39(4), 348-56 (2002). [20] S. M. Swain, F. S. Whaley, M. C. Gerber, S. Weisberg, M. York, D. Spicer, et al. Cardioprotection with dexrazoxane for doxorubicin containing therapy in advanced breast cancer. J. Clin. Oncol. 15, 1318-32 (1997). [21] B. B. Hasinoff, J. C. Yalowich, Y. Ling, J. L. Buss. The effect of dexrazoxane (ICRF-187) on doxorubicin- and daunorubicin-mediated growth inhibition of Chinese hamster ovary cells. Anticancer Drugs. 7(5), 558-67 (1996). [22] B. Holm, P. B. Jensen, M. Sehested. ICRF-187 rescue in etoposide treatment in vivo. A model targeting high dose topoisomerase II poisons to CNS tumors. Cancer Chemother. Pharmacol. 38, 203-9 (1996). [23] K. F. Hofland, A. V. Thougaard, M. Dejligbjerg, L. H. Jensen, P. E. G. Kristjansen, P. Rengtved, M. Sehested, and P. B. Jensen. Combining Etoposide and Dexrazoxane Synergizes with Radiotherapy and Improves Survival in Mice with Central Nervous System Tumors. Clin. Cancer Res. 11(18), 6722-9 (2005). 8 [24] K. F. Hofland, A. V. Thougaard, M. Sehested, P. B. Jensen. Dexrazoxane protects against myelosuppression from the DNA cleavage-enhancing drugs etoposide and daunorubicin but not doxorubicin. Clin. Cancer Res. 11(10), 3915-24 (2005). [25] S. DeFlora. Mechanisms of inhibitors of mutagenesis and carcinogenesis. Mutat. Res. 402, 151-8 (1998). [26] L. H. Einhorn. Testicular cancer: an oncological success story. Clin Cancer Res. 3, 2630-2 (1997). [27] I.-D. Adler. Cytogenetic tests in mammals. Mutagenicity Testing: A Practical Approach. S. Venitt, J. M. Parry, (ed.). Oxford, IRI. pp. 275-306 (1984). [28] F. Tietze. Enzymatic method for quantitative determination of nanogram amounts of total and oxidized glutathione: application to mammalian blood and other tissues. Anal. Biochem. 27, 502 (1969). [29] I. Vermes, C. Haanen, H. Steffens-Nakken, C. Reutelingsperger. A novel assay for apoptosis. Flow cytometric detection of phosphatidylserine expression on early apoptotic cells using fluorescein labelled Annexin V. J. Immunol. Methods 184, 39-51 (1995). [30] L. Sachs. Angewante Statistik, Auflage. Vol. 6, Springer, Berlin. 230-8 (1984). 9